
Utilizing a Mobile Electrode (PEN) for Functional Electrical
Stimulation (FES) to Treat Facial Paralysis Caused by a Brain Injury
A Case Study
Fabiana S. B. Perez¹, Adson Ferreira da Rocha¹, Karla de Castro Cardoso²,
Hellen Orlando Veloso² and Inez Janaina de Lima Amaral³
¹School of Medicine, University of Brasília, Brasília, DF, Brazil
²State University of Goiás, Anapolis, GO, Brazil
³Catholic University of Goiás, Goiania, GO, Brazil
Keywords: Electrical Stimulation, Facial Paralysis, Pen-shaped Mobile Electrode, Brain Injury.
Abstract: This research is a case study that evaluated the therapeutic efficacy of Functional Electrical Stimulation
(FES) associated with the method of Proprioceptive Neuromuscular Facilitation (PNF) in a patient with
central facial paralysis caused by brain damage resulting from brain anoxia. The treatment involved the
application of Orofacial Regulation Therapy, associated with physical therapy using a pen-shaped electrode
whith an FES current. The treatment was administered for a period of one year and involved two weekly 15
minute sessions. The stimuli were performed with modulated current at a frequency of 60 hertz, pulse width
of 300 miliseconds, rise of four (4) seconds, decay of four (4) seconds, time ON of one (1) second, time
OFF of five (5) seconds, in trapezoidal pulses (forming a mini cycle of 14 seconds with 30 pulses) at an
intensity level measured according to the patient’s sensitivity, associated with the PNF method. The mobile
pen-shaped electrode was positioned at precise points on the paralyzed muscles of the face, and the fixed-
electrode was positioned on the Deltoid muscle. There was satisfactory rehabilitation of muscles in the left
hemiface and acquired improvement in the oral consumption of the bolus. The symmetry of the face was
also enhanced, along with facial expressions and connotation measuring four (4) on the Chevalier scale.
1 INTRODUCTION
Facial paralysis can cause an individual to lose one
form of non-verbal communication. Non-verbal
communication is significant when oral expression
can no longer be used to transmit information to a
recipient (Calais et al., 2005).
Facial expressions can be utilized to more
accurately demonstrate the feelings of an individual
and sometimes transmit more information than
actual verbal communication. An individual with
facial paralysis often feels insecure and embarrassed
about these changes, which often results in isolation.
This can also cause a family to feel alienated
because of a member’s communication difficulties
and even an inability to feed normally in some cases
(Lima, 2001).
Central Facial Paralysis (CFP) or supranuclear
palsy consists of lesions on the pyramidal motor
neurons of the frontal cortex (responsible for
voluntary movements), that manifest on the
ipsilateral (upper face) and contralateral (top and
bottom) of the facial motor nucleus (Lazarini et al.,
2002). Thus, involuntary movements or emotion can
be preserved. It is usually caused by vascular
lesions, tumors, degenerative or inflammatory
processes and can be accompanied by other
neurological manifestations including hemiplegia
and dysarthria (Bento et al., 1998); (Esborrat, 2000);
(Testa and Antunes, 2000); (Chevalier et al., 1987).
Facial paralysis consists of two phases: flaccid
and sequel. The flaccid phase is characterized by
sagging muscles while at rest and reduced muscle
activity during movement. During this phase there is
potential for regeneration and normal mobility can
return. In the sequel phase, aberrant reinnervation of
the facial nerve can occur and symptoms including
synkinesis (involuntary movements), motor skills
paralysis and contractures may be exhibited (Goffi -
Gomez, 1999); (Moran and Neely, 1996).
269
S. B. Perez F., Ferreira da Rocha A., de Castro Cardoso K., Orlando Veloso H. and Janaina de Lima Amaral I..
Utilizing a Mobile Electrode (PEN) for Functional Electrical Stimulation (FES) to Treat Facial Paralysis Caused by a Brain Injury - A Case Study.
DOI: 10.5220/0004252002690272
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2013), pages 269-272
ISBN: 978-989-8565-34-1
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

The Kabat Method or Proprioceptive
Neuromuscular Facilitation (PNF) assists in the
rehabilitation process of an individual’s physical
condition by requiring a learning of motor skills,
improving flexibility and range of motion, increased
muscle strength and coordination. PNF exercises
combine diagonal movements, based on a deep
anatomical study, with the biomechanical and
neurophysiological. These exercises resemble the
functional movements of daily life and can be used
in the treatment of facial paralysis (Alencar et al.,
2011). This method is more efficient when
associated with electrical stimulation.
FES (Functional Electrical Stimulation) enables
a selective repeat afferent input of the central
nervous system which activates not only the targeted
location, but also the reflex mechanisms of the
muscle. These are very important for the
reorganization of motor activity and movements that
are impaired due to the injury of the upper motor
neurons. Furthermore, FES produces a general
increase in the potential that the electric current will
reach the balance of excitatory and inhibitory pulses,
stimulating the disabled motoneurons while the
patient has the opportunity to consciously
experience the “normal movement”. Thus with
repetition, the patient may relearn movement and
modulate their tonus. (Perez, 2011).
The smaller the diameter of the electrode, the
more concentrated the electrical charge becomes,
thus requiring a lower dose of current to achieve the
same result as a larger electrode in relation to
muscular contraction (Agne, 2004).
The movable electrode used for facial
stimulation had a pen shape and was smaller in
diameter than others electrodes. These features
promoted a deeper and more intense stimulation of
the muscle fiber utilizing a lower intensity current
than required by other conventional electrodes
(Perez, 2011).
According to Roberts (1997), physical therapy
uses myotherapy, and in some cases, electrical
stimulation with the aim of recovering facial
symmetry. Speech therapy uses this practice to
achieve facial symmetry and adequate stomatognatic
functions (chewing, sucking and swallowing), in
addition to improving verbal communication as a
whole.
2 MATERIAL AND METHODS
This research is a case study of a patient with left-
sided facial paralysis who was treated with the pen-
shaped electrode, utilizing FES current therapy
associated with the PND Method and Orofacial
Regulation Treatment.
Patient VLN, now deceased, was a Caucasian
female. At age 31 she suffered anoxia after
exogenous poisoning (ingestion of poison as a result
of depression). She was discovered 24 hours after
the incident and was unconscious. The patient
suffered cardiac arrest and fell into a comatose state.
Patient VLN was initially diagnosed with brain
damage from anoxia and remained on a
tracheostomy for 18 days and a gastrostomy for a
month.
Three years after the incident the patient was
admitted to the Center for Integrated Rehabilitation
and Stimulation (CEREI) in Goiânia-Goiás, Brasil,
to undergo a multidisciplinary rehabilitation
program. During the physiotherapeutic examination
the patient appeared apathetic, lacking initiative and
spontaneous verbal fluency. During a neurological
examination, we observed impaired expressive
language and language comprehension
as only
preserved for simple orders. She exhibited spastic
rigidity ranked degree five on the Ashworth Scale,
as well as spastic tetraplegia, hyperreflexia,
preserved sensation, facial paralysis and
opisthotonos. During the evaluation of facial
movements it was possible to identify facial
asymmetry and spastic facial palsy was only visible
as an eye twitch (a sign noted on Chevalier’s Scale).
Patient VLN also lacked the ability to contract the
following muscles: occipitofrontal,corrugator
supercilii, orbicularis oculi, transverse nose, risorius
and the orbicularis oris of the left hemiface. She also
had synkinesis and unintelligible vocalization.
The speech therapy evaluation uncovered left-
sided facial hemiparesis (falling oral rhyme and
difficulty in labial sealing), a decrease in the tone
and mobility of the organs that compose the
orofacial complex (COF), as well as the presence of
mild drooling from the left side of the mouth. When
food was administered orally (in both a liquid and
paste form), difficulty was observed during the
swallowing cycle. Patient VLN’s tongue thrust
forward during swallowing and signs of laryngeal
penetration were noted (gagging and coughing after
swallowing).
Patient VNL was referred to undergo both
physical and speech-language therapy twice a week
for a year without interruption. Therapy sessions
BIODEVICES2013-InternationalConferenceonBiomedicalElectronicsandDevices
270
utilizing FES associated with the PNF Method lasted
for 15 minutes. The apparatus that was used was the
Electro Scientific ORION – Quark/ Br (featuring
TENS and FES functions) with two channels. For
this case, the channel was coupled with two types of
electrodes while in the FES program. A synchronous
current in a trapezoidal shape was generated by the
apparatus through both a pen-shaped mobile
electrode (which identified the precise musculature
in the face) and a fixed electrode in the deltoid
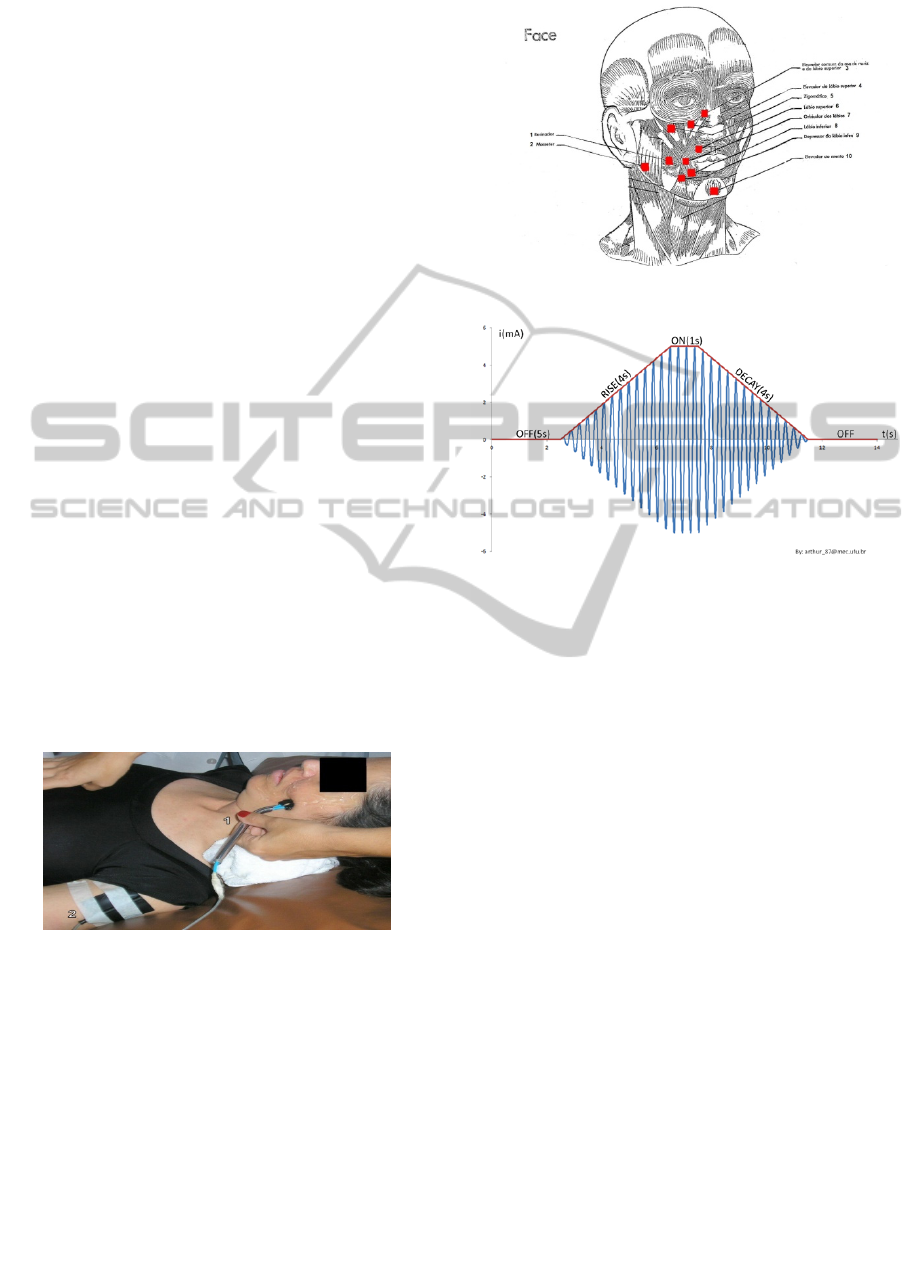
muscle (Figure 1). Ten facial motor points were
stimulated, noted in Figure 2. The stimuli were
performed with modulated current at a frequency of
60 hertz, pulse width of 300 miliseconds, rise of four
(4) seconds, decay of four (4) seconds, time ON of
one (1) second, time OFF of five (5) seconds, in
trapezoidal pulses (forming a mini cycle of 14
seconds with 30 pulses) (figure 3). The intensity of
the treatment was measured in accordance with the
sensitivity of the patient, based on the gestural
communication. The total cycle was 140 seconds,
therefore each point was stimulated for six mini-
cycles. During the “off” time the pen position was
changed along with the movement of PNF.
The following muscles were stimulated: 1 –
Buccinator, 2 – Masseter, 3 – Levator anguli oris, 4
– Levator labii superioris, 5 - Zygomaticus, 6 –
Levator anguli oris, 7 – Orbicularis oris, 8-
Depressor labii inferioris, 9 – Depressos anguli oris
and 10 – Mentalis. Following on FES session, we
performed tactile and gustatory intra and extra oral
stimulation.
Figure 1: (1) Is the mobile electrode- (2) is the electrode
fixed to the Deltoid.
3 RESULTS AND DISCUSSION
In this case study, we used a combination of
traditional ideas and contemporary concepts of
functionality. Upon the conclusion of the treatment,
a satisfactory rehabilitation in the muscles of the left
hemiface was achieved. Patient VLN acquired the
ability to communicate by meaningfully
unsystematic vocalizations and an improvement in
Figure 2: Points of the face that were stimulated.
Figure 3: Graphic of the FES current.
the oral consumption of the food bolus. She also
gained facial symmetry and expressions, along with
vast connotation abilities ranked level four on
Chevalier’s scale (motion made broadly,
synchronously and symmetrically to one side).
The assumption is made that electric stimulation
in facial paralysis can interfere with neural
regeneration after facial nerve injury, but there are
few studies about its effectiveness. Due to the small
size and proximity of the muscles in the face, it
becomes difficult to isolate contractions, causing
massive movements that generate abnormal motor
skill patterns (Rodrigues, 1997). In our study, the
goal of electric stimulation was to return the
movement (muscle contraction) of the facial
muscles. The pen-shaped electrod developed by
Perez (2011) differentiates itself from other devices
by modulating the intensity of the stimulus in order
to visualize muscle contraction instead of only
relying on motor sensitivity. Another benefit is that
the smaller diameter of the electrode is capable of
stimulating an isolated muscle mass, as opposed to
an entire cluster of muscles. The aim of the
myofunctional exercises is to accelerate the return of
movement and muscle function to the facial
muscles, thus preventing atrophy of these muscles,
which would hinder their recovery (Goffi-Gomez,
1999). The use of electric current therapy for muscle
UtilizingaMobileElectrode(PEN)forFunctionalElectricalStimulation(FES)toTreatFacialParalysisCausedbyaBrain
Injury-ACaseStudy
271

strengthening, the aid of the pen-shaped electrode
and myofunctional therapy increases and enhances
the effectiveness of exercise. These combined
techniques are effective treatments for the
rehabilitation of CFP.
4 CONCLUSIONS
The treatment of facial paralysis with electrical
stimulation is a long-lasting process that requires
dedication on the part of the individual and family
(caregivers).
FES provides a selective repetitive afferent input
to the central nervous system which not only
activates the targeted location, but also the reflex
mechanisms of muscles. This process reorganizes
the motor activities and movements that are
impaired. FES leads to a general increase in the
potential that electric currents will reach the balance
of excitatory and inhibitory pulses, thus stimulating
disabled motoneurons while the patient has the
opportunity to consciously experience the “normal
movement.” As a result, through repetition, the
patient can relearn movement. (Perez, 2011)
Electrical stimulation, the type of electrode used
and the method of exercises associated with PND
seem to be important factors that enhance training
by increasing the balance of the COF structures and
their functions. Ultimately, this results in an
improvement in the quality of life of patients and
families, and supports an increasing acceptance of
the treatment.
The combination of both physical and speech
therapy is essential to the effectiveness of the
method and an improvement in the technique.
REFERENCES
Agne, J. E. Electro-thermotherapy Theory and Practice.
2nd ed. Santa Maria: Orium, 2004, 346 p.
Alencar, R. F. et al. Proprioceptive Neuromuscular
Facilitation mat in the reacquisition of functions in
spinal cord injury. Journal Neuroscience, v. 19, n. 3,
p. 512-518, 2011.
Bento, R. F.; Miniti, A.; Marone, S. A. M. Treaty of
Otology. New York: Edusp, 1998
Calais, L. L.; Gomez, M. V. S. G.; Bento, R. F.;
Comerlatti, L. R. Avaliação funcional da mímica na
paralisia facial central por acidente cerebrovascular.
Pró- Fono Revista de Atualização Científica, Barueri
(SP), v. 17, n. 2, p. 213-222, maio-ago. 2005.
Chevalier, A. M. et al. Evaluation of motor function in
the face of the central and peripheral lesions. IN:
Lacote, M., Chevalier, AM, Miranda, A.; Bleton, JP;
Stévenin, P. Clinical evaluation of muscle function.
Manole, 13-24,1987.
Comitê de Motricidade Oral – SBFa. Motricidade Oral –
Como atuam os especialistas. Pulso Editorial. São
José dos Campos, 2004.
Esborrat, L. M. Facial paralysis (Part I). Chiron, v. 31, n.
1, p. 18-35, 2000.
Goffi-Gomez, M.V.S. -The contribution of speech therapy
in facial paralysis in head and neck cancer. In:
Kowalski, LP, DIB, LL, Ikeda, MK & ADDE, C.,
Reg-prevention, diagnosis and treatment of oral
cancer. New York: frontis, 523-8, 1999.
Lazarini, P. R.; Fernández, A. M. F.; Brasileiro,V. S. B.;
Custódio, S. E. V. Peripheral facial palsy by
impairment of the brainstem - the purpose of a clinical
case. Journal of Otolaryngology, v. 68, n. 1, p. 140-
144, 2002.
Lima, C. M. O.; Atuação Fonoaudiológica na Paralisia
Facial. Monografia de Conclusão de Especialização
em Motricidade Oral Hospitalar. CEFAC. Londrina.
2001.
Morales, R. C.: Terapia de Regulação Orofacial. Edições
Científicas Memnon. São Paulo, 1999.
Moran, C. J. & Neely, J. G. - Patterns of facial nerve
synkinesis. Laryngoscope, 106, 1491-6, 1996.
Perez, F. S. B. . Comparative study between a fixed
electrode and movable electrode (pen) in strengthening
perineal. Brasilia, 2011. 35 p. Thesis (Master of
Medical Sciences) - Faculty of Medicine, UNB.
Rodrigues, R. R. The Speech Therapy and Physical
Therapy in Peripheral Facial Paralysis, New York,
1997. 25 p. Monograph - Centre of Specialization in
Clinical Speech Pathology.
Tessitore, A.; Regulação Orofacial: Sua importância no
equilíbrio das funções estomatognáticas. Anais do 16º.
Conclave Internacional de Campinas, ACDC.
Mar/Abr, 2005, São Paulo.
Testa, J. R. G.; Antunes, M. L. Facial palsy: diagnosis and
treatment. Compact, v. 1, n. 4, p. 5 15, 2000.
BIODEVICES2013-InternationalConferenceonBiomedicalElectronicsandDevices
272
