
An Empirical Comparison of DEA and SFA Method to Measure
Hospital Units’ Efficiency
George Katharakis
1
, Maria Katharaki
2
and Theofanis Katostaras
1
1
Faculty of Nursing, National and Kapodistrian University of Athens, 23 Papadiamantopoulou Str., Athens, Greece
2
Department of Economic Sciences, National and Kapodistrian University of Athens, 8 Pesmazoglou Str., Athens, Greece
Keywords: Efficiency, Data Envelopment Analysis (DEA), Stochastic Frontier Analysis (SFA), Bootstrap Analysis,
Translog Form, OR in Health.
Abstract: Although frontier techniques have been used to measure healthcare efficiency, their utility in decision
making process is limited by both methodological questions concerning their application. The present paper
aims to examine the data envelopment analysis (DEA) and stochastic frontier analysis (SFA) results in order
to facilitate a common understanding about the adequacy of these methods. A two-stage bootstrap DEA
method and the Translog formula of the SFA were performed. Multi-inputs and multi-outputs were used in
both of the approaches assuming two scenarios either including environmental variables or not. Thirty-two
Greek public hospital units constitute the sample. The main output of the analysis was that the efficiency
scores increased with the incorporation of environmental variables. Moreover, environmental variables
being hospital status and geographical position were found significantly correlating with inefficiency, while
patient mobility was not found strongly correlating. DEA and SFA were found to yield divergent efficiency
estimates due to the nature of the environmental variables and the measurement error. The analysis
concludes that there is a need for careful attention by stakeholders since the nature of the data and its
availability influence the measurement of the efficiency and thus it is necessary to be specific when
choosing the mathematical form.
1 INTRODUCTION
1.1 Background
Governments all over the world face the difficult
task of managing the complexities of controlling
healthcare costs while at the same time ensuring that
patients receive not only a high quality of care, but
also that this care is delivered as efficiently as
possible (Katharaki, 2008). As a result, payers and
purchasers have begun to use frontier efficiency
measurement techniques in order to measure the
performance of the healthcare sector with the aim of
supporting their decisions on healthcare units’
performance. More commonly used techniques are
data envelopment analysis (DEA) and stochastic
frontier analysis (SFA) which employ quite distinct
methodologies for frontier estimation and efficiency
measurement, each with associated strengths and
weaknesses. Specifically, “…non-statistical
approaches such as DEA have the disadvantage of
assuming no statistical noise, but have the advantage
of being non-parametric and requiring few
assumptions about the underlying technology. SFA
models on the other hand have the attraction of
allowing for statistical noise, but have the
disadvantage of requiring strong assumptions as to
the form of the frontier” (Jacobs, 2001, p.3). DEA is
favored where measurement error is unlikely to pose
much of a threat and where the assumptions of
neoclassical production theory are in question.
Conversely, SFA should have the advantage in
coping with severe measurement error and where
simple functional forms provide a close match to the
properties of the underlying production technology.
Gong and Sickles (1992) report findings along
similar lines so that “...as mis-specification of
functional form becomes more serious, DEA’s
appeal (vis-à-vis SFA) becomes more compelling”
(p.259).
Hospital units evaluations have to date been
carried out using mostly DEA-based methodologies.
During the last twenty years, non-parametric and
parametric methods have been increasingly
94
Katharakis G., Katharaki M. and Katostaras T..
An Empirical Comparison of DEA and SFA Method to Measure Hospital Units’ Efficiency.
DOI: 10.5220/0004274502420251
In Proceedings of the 2nd International Conference on Operations Research and Enterprise Systems (ICORES-2013), pages 242-251
ISBN: 978-989-8565-40-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)

employed to measure and analyze the productive
performance of healthcare services. The healthcare
sector is a unique area of application, and one in
which the measurement of efficiency has burgeoned
over the past few years. Mortimer (2002)
highlighted the need for parallel application of
competing methods for frontier estimation and
efficiency measurement.
Thereby, in the efficiency analysis literature
there has been considerable interest in reconciling
SFA and DEA (Mutter et al., 2011). Both studies of
Chirikos and Sear (2000) and Jacobs (2001) that
compared SFA and DEA methods found divergent
estimations between the results. Linna (1998)
examined cost efficiency of Finish hospitals and
found that SFA and DEA generated similar results.
The last 5 years Desaia et al., (2005), Assaf and
Matawie (2008), Lee et al., (2009) share the same
prospect that neither DEA nor SFA can be regarded
as clearly dominant. Likewise, more recent studies,
Nedelea and Fannin (2012), Ippoliti and Falavigna
(2012) suggest that SFA and DEA approaches along
with other techniques are viable alternatives for
analyzing the impact of environmental variables and
dynamic effects on hospital cost efficiency,
generating similar but more consistent results in
empirical application to the efficiency analysis of
healthcare units. Moreover, the majority of the
researchers agree on the need of being aware of
using both DEA and SFA methods, along with
determining the sources of productivity factors by
regressing the efficiency scores against a set of
environmental variables.
1.2 Aim and Scope
Under this context, an empirical application of both
two-stage bootstrap DEA approach of Simar and
Wilson (2007) and SFA with the Translog functional
form (SFA
translog
) on a sample of Greek public
hospital units has been conducted in order to analyze
cost efficiency estimations comparatively. Based on
the fact that SFA is mostly used in literature under
one input and many outputs or the opposite (Bryce,
Engberg and Wholey, 2000; Chirikos and Sear,
2000; Giuffrida and Gravelle, 2001; Jacobs, 2001;
Ondrich and Ruggiero, 2001; Assaf and Matawie,
2008; Lee et al., 2009), in this paper, multi-inputs
and multi-outputs are used in both of the approaches
assuming two scenarios, either including
environmental variables or not. Thus, the analysis is
focused on discussing the results derived by the
models’ applications.
Therefore, the main purpose of our study is to
examine the “behavior” of the two-stage bootstrap
DEA approach and SFA
translog
, and how the two
methods can be used to make valid inferences about
the effects of environmental variables on estimated
cost efficiency. Nevertheless, the present study aims
to highlight the importance of the information
derived with regard to the functional forms of the
DEA and SFA method and therefore what should be
taken into account when applying them in a larger
sample of health units. Hospital managers and
policymakers can become more effective decision
makers by understanding the relationships between
efficiency and these environmental variables.
2 LITERATURE SURVEY
Many researchers have applied methods in order to
evaluate hospital efficiency, such as Data
Envelopment Analysis (DEA) and Stochastic
Frontier Analysis (SFA). These frontier methods use
an efficient frontier to identify the efficiency of
hospital units relative to a reference set of healthcare
units. DEA is a non-parametric approach that uses
mathematical programming to identify the efficient
frontier. SFA is a parametric approach that
hypothesizes a functional form and uses the data to
econometrically estimate the parameters of that
function using the entire set of DMU’s. However,
the two methods differ in some key theoretical
aspects. DEA measures efficiency relative to a
nonparametric estimate of an unobserved true
frontier, conditional on observed data (Simar and
Wilson, 2007). On the other hand, SFA requires the
specification of a functional form for the frontier,
and assumptions about the distributions of the
random error and inefficiency error terms, which
might be very restrictive (Newhouse, 1994).
In their systematic literature review regarding the
investigation of the results derived from at least one
pair-wise comparison of the DEA/SFA methods,
Katharakis and Katostaras (2012) highlighted that
both approaches of DEA and SFA were found to
yield divergent efficiency estimates due to many
factors such as statistical noise and inputs and
outputs definition, as well as data availability.
Nevertheless, different modeling approaches have
advantages and disadvantages and the choice of the
most appropriate estimation method should depend
on the type of organizations under investigation, the
perspective taken and the quality of the available
data as Hollingsworth (2008) also highlights. The
issue of testing whether an environmental variable
has a significant influence on the production process
AnEmpiricalComparisonofDEAandSFAMethodtoMeasureHospitalUnits'Efficiency
95

and any resulting efficiency estimates has been also
reviewed. Jacobs (2001) note that the literature
provides several different recommendations on how
to handle such variables. Katharakis & Katostaras
(2012) points out that researchers, besides the
combination of models to measure efficiency,
introduce environmental variables in the analysis,
aiming at better understanding the relationship of
these factors to efficiency and thus at better decision
making.
The most commonly used SFA method is the
Cobb-Douglas functional form and Quadratic
formula or Translog formula, using one input or one
output most of the time, along with existing
environmental factors which are analyzed
separately. DEA has the advantage that it is able to
manage complex production environments with
multiple inputs and outputs, but as a non-statistical
method it does not produce the usual diagnostic
tools with which to judge the goodness-of-fit of the
model specifications. While SFA can discriminate
between efficient units, DEA has a limited ability to
do this, although both techniques can discriminate
between inefficient hospitals (Jacobs, 2001).
Considering the above and the purpose of the study,
the choice of multi-inputs and multi-outputs was
adopted for the SFA Translog formula, indicating
the innovation suggested by this paper.
3 MATERIAL AND METHODS
3.1 Sample Synthesis and Variables
Definition
Following Katharaki (2008) research work, both
DEA and SFA model was applied on the sample of
32 Obstetrical and Gynecological (O&G) units
located in five of the ten geographical Greek NHS
regions. Below, hospital units are referred to by
number (N1–N32), for confidentiality reasons. The
evaluation is focused on DEA and SFA methods that
allow initial comparisons to be made and some early
conclusions to be reached. Based mainly on the data
fit to the model, the following are used in this study
as inputs:
number of beds (KL);
number of medical personnel (PR);
total expenditure for the provision of care (SD).
Regarding the selected inputs, hospital size and
capacity were measured by the number of beds.
Most studies exclude the number of physicians
because independent contractors exist who may
admit patients. For the purpose of the current study,
it is important to include them as an input since wide
discrepancies exist between the numbers of
specialized physicians in different regions of the
country which largely determine the volume of the
O-G services that a hospital can perform (Katharaki,
2008). The input “total expenditure”, refers to the
grand total expenditure and not to the individual
resource component costs (doctors’ salaries, nurses’
salaries, etc.). The introduction of “operating
expenses” into the set of inputs aims at an estimate
of the degree of utilization of the financial resources
in relation to the "services" produced.
It should be mentioned that quantitative
expression of factors determining services provided
by healthcare units display significant difficulties
referring to both the factors’ identification and their
functional relationship to the health product.
According to this the "health product" of healthcare
units is expressed through:
the number of female patients treated (NOS);
the number of outpatient examinations (EIA);
the number of lab tests (ERG).
The use of the number of O&G lab tests and
patient days as outputs of the study was selected in
order to become criteria for efficiency assessment of
units as proxy factors of the degree of resource
utilization. These criteria have been utilized in a
plethora of related studies (Chilingerian and
Sherman, 2004).
In this analysis, the environmental variables in
order to analyze the efficiency are the same for both
the stochastic frontier model and the second stage
truncated regression of DEA model. For the
specification of environmental variables, we
followed Rosko and Mutter (2011) along with
Nedelea and Fannin (2012). The primary variable of
interest is Geographical Position (GP) dummy (one
if the hospital is an urban and zero if it a rural one)
which is used to test whether rural O&Gs are more
or less cost efficient than non-rural hospitals. Two
more dummy variables that define the reputation of
the hospital, indicated by:
Hospital Status (HS) (one with high status,
referring to tertiary and university hospitals and
zero with lower status, referring to secondary and
non-university hospitals) and
Patient Mobility (PM) to seek healthcare services
in well-known hospitals (one referring to
hospitals that accept patients from other
geographical regions and zero otherwise)
are included to control the internal pressure
associated with efficiency estimation. The HS
variable was introduced to our analysis based on the
fact that it explains the organizations’ structure.
ICORES2013-InternationalConferenceonOperationsResearchandEnterpriseSystems
96

Following Assaf and Matawie (2008), and Chen,
Hwang and Shao (2005) the status of the hospital
depends on the position of the hospital (university
hospital or not), the experience of the doctors and
the technological infrastructure of the hospital.
Moreover, the PM is a variable which gives the
patients’ mobility to well-known tertiary hospitals
for their better treatment. PM variable has also been
used by Ippoliti and Falavigna (2012) who argue
that patient mobility may be due to a previous
personal experience or to remarks by someone closer
to the patient and that the perception mechanism is
linked to reputation. In this study the classification
of each hospital of the sample regarding PM was
based on Katharaki (2008) research work who
describes the mobility of patients through regions in
order to seek healthcare services.
3.2 Data Analysis
The empirical research was conducted using two
scenarios: the application of DEA and SFA model
either with environmental variables or without them.
The programming language R environment version
2.15 was used for the data analysis, along with the
software package FEAR 1.15 of Wilson (2010) and
the software package FRONTIER 4.1 of Coelli
(2007).
The SFA Translog and the DEA CRS approaches
were used to conduct the empirical analysis of the
first scenario which was not investigated the
environmental effect on inefficiency. With regard to
the method used, DEA, a method originating from
Farrell’s 1957) seminal work, popularized by
Charnes, Cooper and Rhodes (1978) and Banker,
Charnes and Cooper (1984), provides a non-
parametric alternative to parametric frontier
production function analysis. This non-parametric
method allows the calculation of technical efficiency
measured that can be either input or output oriented
(Charnes, Cooper and Rhodes, 1978; Charnes and
Cooper, 1985; Cooper, et al., 2004; Katharaki,
2008). To estimate the efficiency of the Greek public
units used in the sample, the CCR (Charnes, Cooper
and Rhodes) input oriented model was used (1978).
With the help of input and output variables, the cost-
minimizing input vector for each hospital is
calculated using linear programming (Nedelea and
Fannin, 2012). Next, cost efficiency is measured as
the ratio of minimum cost to observed cost and takes
a value between 0 and 1, where a value of 1
indicates a cost efficient hospital (Coelli
et al., 2005).
Regarding SFA, this parametric method was
based on the quantitative economy theory.
According to Farrell (1957) theory of efficiency
measurement, Aigner et al., (1997) and Meeusen and
van den Broeck (1977) independently constructed an
error structure of stochastic frontier analysis to
measure productive efficiency of firm.
SFA is a
parametric approach, and is suited to measure
efficiencies of stochastic industry for input/output
information. To complete the model estimation, it is
important to specify and use the suitable functional
form. Translog and Cobb-Douglas cost functions are
the most well known formulas for research,
especially in evaluating the efficiency of units.
Translog function is very commonly used. It is a
generalization of the Cobb-Douglas function and it’s
a flexible functional form providing a second order
approximation. Cobb-Douglas and Translog
functions are linear in parameters and can be
estimated using least squares methods. For the
purpose of our empirical research the Translog
function has been used since we had multi-inputs
and multi-outputs of the O&G units. In this paper,
we use the Translog form (formula embedded in the
package frontier 4.1 for multi-inputs and outputs)
with three inputs and three outputs provided in the
following equation (equation 1), respectively:
∗
∗
(1)
where
= the variables of the outputs (NOS= Patients
hospitalized, EIA=Patients examined in outpatient
clinics, ERG=Lab tests) for the i
th
healthcare unit at
time t
= Beds for the i
th
healthcare unit at time t
= Total expenditures (€) for the i
th
healthcare
unit at time t
= Medical personnel for the i
th
healthcare
unit at time t
V
= Random error
= Non-negative random variable (or technical
inefficiency)
Data analysis of the second scenario was based
on the two-stage bootstrap DEA method and the
Translog formula of the SFA including the
explanatory variables that have been defined (see
section 3.1). The differences between the SFA and
the DEA approaches are that the SFA requires
AnEmpiricalComparisonofDEAandSFAMethodtoMeasureHospitalUnits'Efficiency
97

functional forms on the production frontier, and
assumes that firms may deviate from the production
frontier not only due to technical inefficiency but
also from measurement errors, statistical noise or
other non-systematic influences (Admassie,
Matambalya, 2002). For this purpose, in the formula
of the SFA Translog frontier, the second non-
negative random variables
which are assumed to
be independently and identically distributed normal
random variables as truncations at zero with
δ
means and variances
(
~0,
) are
known as the technical inefficiency effects and in
our model was formed under the environmental
factors, which were earlier defined. Thus equation 2
represents the inefficiency effects model and is the
following for the second scenario:
= σ
0
+ σ
1
+ σ
2
+ σ
3
+
(2)
where
= dummy variable of geographical position
(0, 1) for the i
th
healthcare unit at time t
= dummy variable of hospital status (0, 1)
for the i
th
healthcare unit at time t
= dummy variable of moving patient (0, 1)
for the i
th
healthcare unit at time t
=Random error (
~0,
)
This research focus on how the environmental
variables influence hospital cost efficiency. From the
first stage of the DEA approach the efficiency scores
are estimated, then regressed in the second stage by
the three environmental variables in order to
investigate if the hospital inefficiency is changed by
these explanatory variables.The second stage of the
two-stage DEA model is conducted by regressing
environmental variables on the healthcare units’
CRS technical inefficiency scores which are
predicted from the first step of the two-stage DEA
model. The units’ technical inefficiency scores are
used as the dependent variable. The set of
environmental variables are used as independent
variables for the two-stage DEA model. The
estimated inefficiency scores are normally bounded
between zero and one. Applying the method of
truncated regression with such a dependent variable
that its values are bounded between zero and one
will lead to biased and inconsistent estimators, since
the truncated method is likely to predict inefficiency
scores which are greater than one (Coelli et al.,
2005). A disadvantage of DEA is that it has no
statistical properties. Simar and Wilson (2007) have
recently addressed this problem and showed that it is
possible to obtain statistical properties for DEA via
the use of the ‘‘bootstrap’’ approach. The bootstrap
approach can also be extended to account for the
impact of environmental variables on efficiency.
These variables are viewed as possibly affecting the
production process but not under the control of
managers. Determining how these variables
influence efficiency is thus essential for deriving
performance improvement strategies. The procedure
used in this study follows that of Simar and Wilson
(2007). A comprehensive discussion of the bootstrap
procedure and its advantages are also provided in
Simar and Wilson (2007).
Both of these approaches have been popular the
last years among researchers in order to explain
valid inferences about the impact of environmental
variables on hospital cost efficiency. What is clear
from the existing literature is that none of the
existing papers (to our knowledge) have adopted the
bootstrapped DEA procedure comparing it with an
SFA model for multi-inputs and multi-outputs.
4 RESULTS
Table 1 shows summary of efficiency scores (per
unit and per geographical area) estimated by both
DEA CRS, DEA bootstrap and SFA Translog model
under the two scenarios of the analysis, with and
without determinants. Efficiency intervals in two
methods DEA and SFA are respectively between
zero and one. Moreover with regard to the first
scenario, the DEA CRS mean efficiency score was
81.56% while the mean efficiency estimated using
SFA
Eq1
was 85.07%. Note the increased score of
approximately 120% for the SFA
Eq1
estimation of
units N9, N16, and N29, something that can be
explained by the structure of the hospital
organization since they have a small amount of
O&G beds and of which the two are regional
hospitals.
From table 1 it is derived that the efficiency
scores obtained from DEA CRS and SFA
Eq1
without
determinants differ, which is consistent with
Chirikos and Sear (2000). The Spearman's Rank
Correlation between the mean of efficiencies
calculated in different methods was then estimated.
The results are listed in Table 2; as it is seen there is
no significant correlation in the different methods.
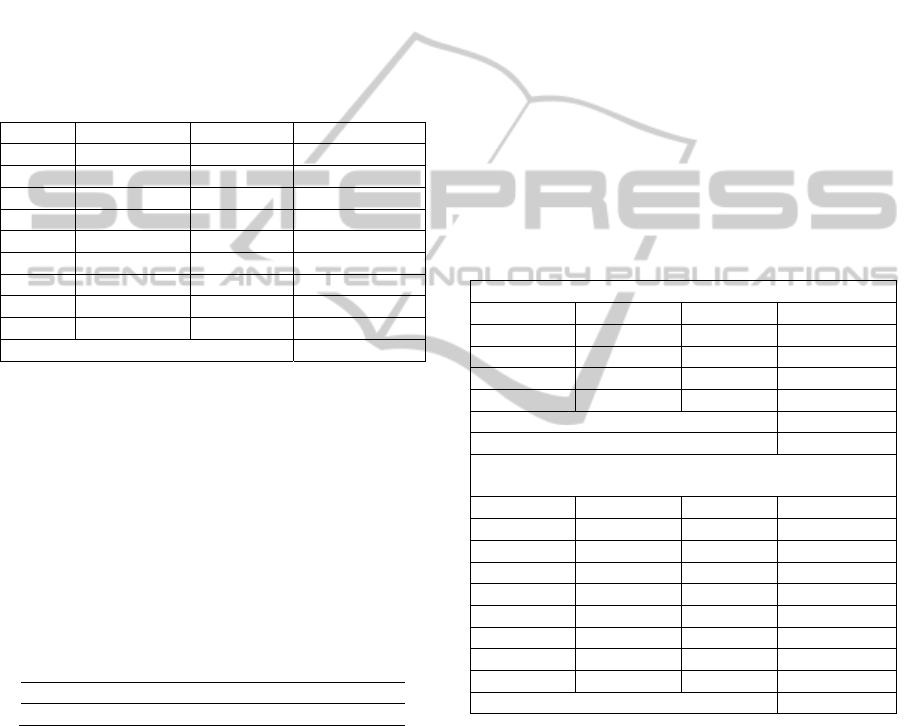
Subsequently, results of the Maximum
Likelihood Estimation of equation 1 of the SFA
Translog model are provided in Table 3. All
variables of the stochastic frontier regression proved
significant.
ICORES2013-InternationalConferenceonOperationsResearchandEnterpriseSystems
98
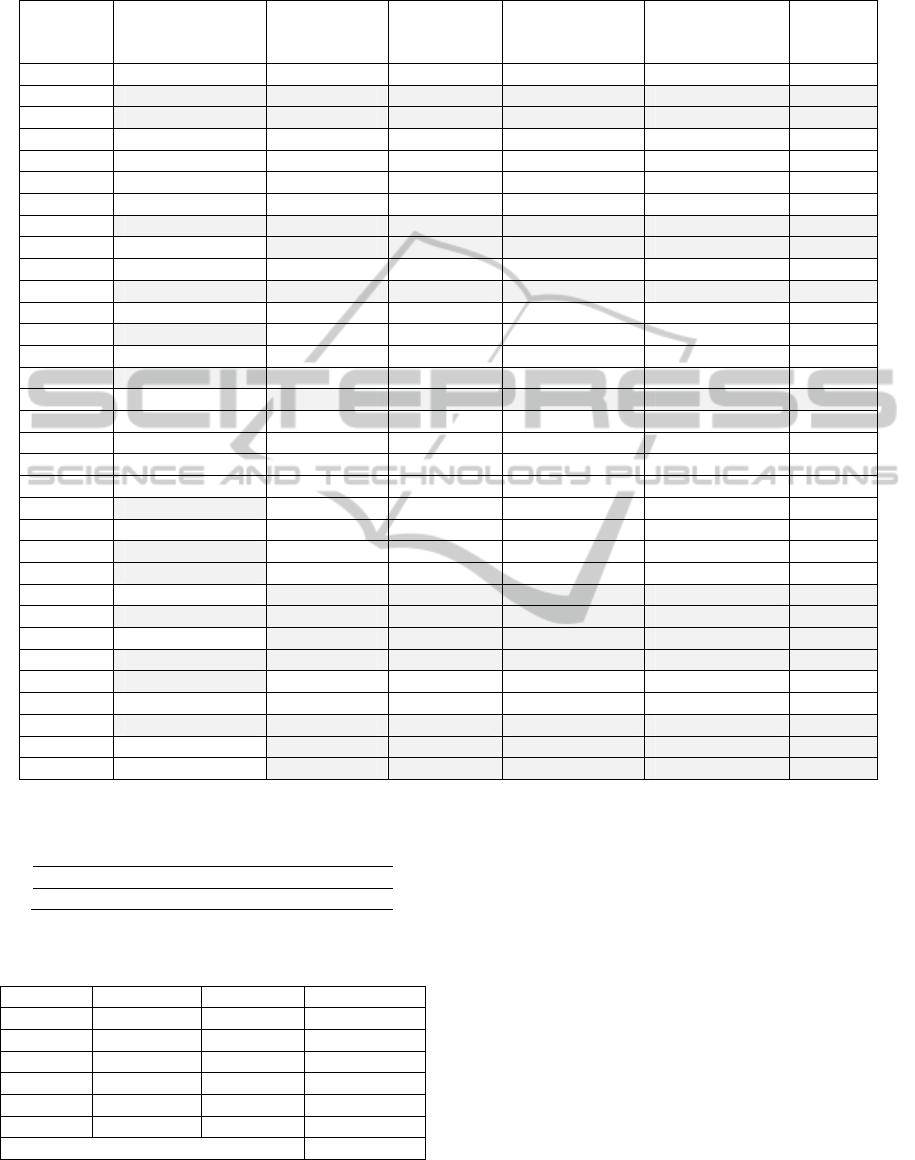
Table 1: The efficiency score of the units of the sample using DEA and SFA model under the two scenarios.
Hospital
units
DEA CRS
efficiency score
SFA
efficiency
score (Eq
1
)
% change
DEA bootstrap
efficiency score
(bias corrected)
SFA efficiency
score (Eq
1+2
)
%
change
N1 0.9512 0.76038 -20.06% 0.7716 0.8917 15.57%
N2 1.0000 0.96840 -3.16% 0.8096 0.9762 20.58%
N3 1.0000 0.93015 -6.99% 0.8108 0.9621 18.66%
N4 0.7196 0.88657 23.20% 0.6199 0.9452 52.48%
N5 0.7794 0.72841 -6.54% 0.6922 0.8027 15.96%
N6 0.5038 0.52935 5.07% 0.4327 0.9456 118.53%
N7 0.5916 0.75046 26.85% 0.5093 0.6842 34.34%
N8 1.0000 0.90595 -9.41% 0.8145 0.9596 17.81%
N9 0.4162 0.91890 120.78% 0.3701 0.8966 142.26%
N10 0.8463 0.66225 -21.75% 0.7516 0.7293 -2.97%
N11 1.0000 0.98596 -1.40% 0.8482 0.9810 15.66%
N12 0.8891 0.82467 -7.25% 0.8034 0.8810 9.66%
N13 1.0000 0.71870 -28.13% 0.8078 0.8244 2.05%
N14 0.4777 0.87582 83.34% 0.4167 0.9336 124.05%
N15 1.0000 0.79965 -20.04% 0.8691 0.8669 -0.25%
N16 0.4337 0.96563 122.65% 0.3552 0.9322 162.44%
N17 0.6852 0.86720 26.56% 0.5947 0.9693 62.99%
N18 0.6603 0.84691 28.26% 0.5840 0.8745 49.74%
N19 0.7634 0.83798 9.77% 0.6597 0.8867 34.41%
N20 0.8084 0.67411 -16.61% 0.7135 0.7988 11.96%
N21 1.0000 0.83900 -16.10% 0.8458 0.9071 7.25%
N22 0.6024 0.73069 21.30% 0.4965 0.8009 61.31%
N23 1.0000 0.97582 -2.42% 0.8572 0.9843 14.83%
N24 1.0000 0.95069 -4.93% 0.8223 0.8961 8.97%
N25 0.9818 0.87170 -11.21% 0.8705 0.9164 5.27%
N26 1.0000 0.96252 -3.75% 0.8669 0.9730 12.24%
N27 0.9096 0.97093 6.74% 0.8232 0.9854 19.70%
N28 1.0000 0.92440 -7.56% 0.8318 0.8966 7.79%
N29 0.4348 0.89203 105.16% 0.3572 0.9201 157.59%
N30 0.8590 0.87164 1.47% 0.7764 0.8572 10.41%
N31 1.0000 0.87509 -12.49% 0.8369 0.8857 5.83%
N32 0.6343 0.97526 53.75% 0.5392 0.9669 79.32%
Mean 0.8156 0.8507 4.30% 0.6945 0.8924 28.49%
Table 2: DEA CRS vs. SFAEq1 Spearman's Rank
Correlations rho.
coefficient = 0.241759
p-value = 0.1825 >0.05
Note: coefficient was insignificant at 0.05% level.
Table 3: SFA Results without determinants.
Coefficient Std. Error t value
Intercept -4.5136e+03 9.8655e-01 -4575.185***
LogKL -3.5771e+02 9.5342e-01 -375.191 ***
LogSD 3.4379e+03 9.0588e-01 3795.058 ***
LogPR -1.6328e+02 9.4125e-01 -173.477 ***
σ
2
4.5061e-02 3.7098e-03 12.146 ***
γ 9.9025e-01 4.5601e-02 21.715 ***
Log Likelihood function 23.2629
Note: ***denotes significance at 1% level, **significance at 5%
level, *significance at 10% level
Provided that DEA models incorporate only
discretionary inputs and the fact that environmental
factors that may influence efficiency are not taken
into consideration in the analysis, scenario 2 was
introduced and under the null hypothesis of positive
effect of the environmental variables GP, HS and
PM on inefficiency, SFA Translog under equation 1
and 2 was performed. In other words, GP, HS and
PM dummies were included into the SFA Translog
model as shifted variables or else variables that
explain the inefficiency level. Table 1 summarizes
the estimated efficiency scores that are likely to
substantially increase, while Table 4 outlines the
significance of the introduced variables of the MSE
estimation of SFA
Eq(1+2)
. In particular, the two
environmental variables GP and HS found to explain
inefficiency as significant. This is also derived from
AnEmpiricalComparisonofDEAandSFAMethodtoMeasureHospitalUnits'Efficiency
99
Ippoliti and Falavigna (2012) and Chen, Hwang and
Shao (2005).
Moreover, the coefficients of the KL and PR
variables found to be negatively correlating with
inefficiency before and after the explanatory
variables introduction (Table 3 & 4). According to
Chen, Hwang and Shao (2005) hospitals with a large
bed size, experience a lower inefficiency score. On
the other hand, the variable SD was found to be
significantly correlating with inefficiency in both
scenarios. This finding is in line with Katharaki
(2008) results, indicating the need for more rational
utilization of economic resources.
Table 4: SFA Results with determinants.
Coefficient Std. Error t value
Intercept -4.7798e+03 9.8891e-01 -4833.3560***
LogKL -3.7874e+02 9.6128e-01 -393.9903***
LogSD 3.4567e+03 9.2055e-01 3755.0573***
LogPR -1.5535e+02 9.4804e-01 -163.8625***
GP -7.9177e-01 1.8268e-01 -4.3341***
HS 6.9518e-01 1.4319e-01 4.8551***
MP 2.2101e-01 1.1332e-01 1.9504
σ
2
1.9973e-02 1.0085e-02 1.9805*
γ 9.6286e-01 3.4351e-01 2.8030**
Log Likelihood function 32.87449
Note: ***denotes significance at 1% level, **significance at 5%
level, *significance at 10% level
Following Simar and Wilson (2007), a DEA
bootstrap was conducted. The results are also
presented in Table 1. The Spearman's Rank
Correlation between the mean of efficiencies scores
of DEA bootstrap and SFA
Eq1+2
were also calculated.
The results are listed in Table 5; as it is seen, there is
still no significant correlation in the different
methods.
Table 5: Boootsrap DEA CRS vs. SFAEq
1+2
Spearman's
Rank Correlations rho.
coefficient = 0.21004
p-value = 0.2475>0.05
Note: coefficient was insignificant at 0.05% level.
Considering that the most common approach in
testing the impact of environmental variables on
efficiency involves the use of two-stage analysis,
where according to McDonald (2009) ‘‘Stage 1 is
used to use nonparametric DEA to calculate the
efficiency with which output is produced from
physical inputs. Stage 2, on the other hand, uses
regression to relate efficiency scores to factors seen
to influence’’ (p. 792), and that Simar and Wilson
(2007) have recently criticized this approach, and
suggested instead of a bootstrap approach in which it
is possible to improve the accuracy of the regression
estimates, we regressed the derived bias corrected
bootstrap efficiency scores on the environmental
variables GP, HS and PM (following the
methodology presented in section 3.2). Note that
2000 bootstrap replications (B=2000) was used,
following Simar and Wilson (1999) who highlighted
the adequate coverage of the confidence intervals by
choosing the appropriate number of replications.
At the last step of our analysis, the effect of
determinants on inefficiency was estimated through
the model of the truncated regression. Results of the
Maximum Likelihood Estimation for the parameters
on DEA CRS initial scores and on the bias corrected
bootstrap scores are provided in Table 6. Comparing
the results with those from the SFA method (Table 3
and 4) all variables proved significant and likely
similar. The estimated coefficients and standard
errors for the models are also presented in Table 6.
Table 6: Estimated effects of environmental variables in
both approaches.
DEA results without the effect of determinants
Coefficient Std. Error t value
Intercept 0.6604 0.05347 12.352 ***
KL -0.0001643 0.002434 -0.007
SD 2.467e-07 8.526e-08 2.893**
PR -0.01773 0.006159 -2.880**
Log Likelihood function 13.694348
Two- stage DEA results with determinants after
bootstrap
Coefficient Std. Error t value
Intercept 0.5664788 .0458635 12.35***
KL -0.000144 .0018592 -0.08
SD 2.23e-07 6.72e-08 3.31**
PR -0.0170342 .0052943 -3.22**
GP -0.3272004 .1759237 -3.86***
HS 0.2450065 .1442114 3.70***
MP 0.1418569 .1156827 1.23
Log Likelihood function 18.57163
Note: ***denotes significance at 1% level, **significance at 5%
level, *significance at 10% level
Furthermore, Table 6 outlines the positive and
highly significant coefficient of GP, and negative
and highly significant coefficient of HS dummy,
suggesting that the geographical position of a
healthcare unit, as well as the hospital status of the
unit influence their performance.
5 DISCUSSION
This paper has proposed a framework to measure the
ICORES2013-InternationalConferenceonOperationsResearchandEnterpriseSystems
100

efficiency of hospital units, aiming to examine the
adequacy of two different methods that are
commonly used in literature. Both DEA and SFA
approaches are efficiency frontier analysis, and
provide a suitable way of approaching the
measurement of hospital efficiency. Hospitals are
aimed to minimize inputs and operating efficiently.
Under this context, this paper applies the two
methods to evaluate the efficiency of 32 hospital
units. In particular, a two-stage bootstrap DEA
method and the Translog formula of the SFA were
performed. Multi-inputs and multi-outputs were
used in both of the approaches assuming two
scenarios either including environmental variables or
not.
The main output of the analysis was that the
efficiency scores increased with the incorporation of
environmental variables in the SFA model and
decreased when bootstrap is applied. Specifically,
the analysis shows that the average efficiency scores
of SFA
Eq1
model is the highest (0.85), followed by
DEA
CCR
model (0.81), while the SFA
Eq(1+2)
model
increased (0.89) when environmental variables were
taken into consideration. This result is in line with
Prochazkova (2011), and Nedelea and Fannin
(2012). In addition, when applying the bootstrap
approach and regressing the bias corrected
estimations on the same environmental variables, the
average score decreases to 0.69. Considering the
bootstrapped results, none of the healthcare units
appear to be close to full efficiency and even the
rankings are not preserved. This confirms previous
results from Simar and Wilson (1998; 1999) who
argued that traditional DEA models tend sometimes
to present firms as efficient, when they are actually
not. Consistent to Cordero, Pedraja and Santin
(2009) who outlines that one stage approach
overestimates efficiency especially in the small
sample due to the loss of discrimination power in
DEA after including additional variables (non-
discretionary inputs), the above finding could be
further justified from the small sample of our
analysis.
Moreover, the significant correlation of
environmental variables GP and HS with the
inefficiency are in line with the findings of Ippoliti
and Falavigna (2012) and Chen et al., (2005),
indicating that future research would include a more
detailed study of organizational factors (Minvielle et
al., 2005; Minvielle et al., 2008). In addition, the
present study provides valuable information
regarding deployment of medical staff and beds and
the utilization of financial resources. SFA results
indicate the need for measures taken regarding the
more rational utilization of economic resources.
With regard to the methodology used, a large
number of efficiency analysis studies use SFA with
cross-sectional data. However, the cross-sectional
stochastic frontier model has been shown to have
some limitations. First, in cross-sectional stochastic
frontier models, firm-specific efficiency is
unidentified and researchers typically estimate
expectations of efficiency conditional on a
composite residual. Second, cross-sectional
stochastic frontier models require specific
distributional assumptions for each error component
in order to estimate efficiency.
Alternatively, one can use the two-stage
approach along the line of Simar and Wilson (2007)
with cross-sectional data. From the results, it is
clearly that the DEA and SFA approach have many
advantages and disadvantages as well. Both
techniques constitute two alternatives solutions for
analyzing the effects of the environmental variables
on hospital efficiency. It is shown that similar and
consistent results have been obtained in our
empirical application from the two methods
considering the efficiency analysis of O&G units.
6 CONCLUSIONS
Different methods have been utilized for adjusting
efficiency scores to control the environmental
factors (Cooper, Seiford and Zhu, 2004). The
purpose of our work was to reach a wide variety of
stakeholders, each of which faces different pressures
and values in the selection and application of
efficiency measures. Moreover, this paper is
intended to create a common understanding among
these stakeholders about the adequacy of tools to
measure healthcare efficiency. Given the limitations
of frontier techniques, it may be that they are best
employed in tandem, when possible, and if different
methods suggest similar directions for results then
the validity of such findings is enhanced. Since the
healthcare industry is one area where efficiency
measurement may have a direct policy impact, a
cautious approach is necessary. The use of models
with restrictions placed upon the weight given to
variables, in order to reflect underlying production
models or policy values, is also an interesting area
requiring further research to justify the use of such
restrictions. The quality of data available for use
may also be a problem to be addressed.
Notwithstanding the caveats mentioned earlier
regarding making comparisons across studies, and
AnEmpiricalComparisonofDEAandSFAMethodtoMeasureHospitalUnits'Efficiency
101

that perhaps work needs to be undertaken to think of
ways of making efficiency studies comparable, these
findings may have important policy implications for
the organizational structure of healthcare delivery.
Besides that, the paper has a number of other
limitations. The panel has been restricted to one year
of observations in an unbalanced form with a small
sample of the healthcare units. According to Coelli
et al. (2005) SFA models should be applied in much
bigger samples. Furthermore, focusing solely on the
improvement of the overall inefficiency, a policy
maker or a manager may opt to alter a specific
decision variable. It is thus necessary to carefully
address issues regarding improving the managerial
decision-making process through quantitative
analysis.
To sum up, careful attention should be paid to
the purpose of the analysis and to how results are to
be used. In particular, if they are to be used to
influence economic behavior - for example in the
form of setting targets, or identifying candidates for
inspection - then the potential costs of making
incorrect inferences should be recognized. The
results of this analysis should not serve as a
background for immediate policy responses. It rather
points out special circumstances and provides
motivation for further research. At the same time, it
is fully acknowledged that economic analysis of
Greek hospitals is not telling the whole story. It
should be supplemented by surveys of satisfaction
with the quality of care or surveys of patient criteria
for choosing the hospital unit, and thus include
quality of care, other managerial factors and even
clinical research and political change, as exogenous
variable factors, in order for the analysis to provide
an overall picture.
ACKNOWLEDGEMENTS
The current paper constitutes part of the thesis titled
‘‘Evaluating Efficiency of Health Care Units with
Stochastic Frontier Analysis” that has been co-
financed by the European Union (European Social
Fund – ESF) and Greek national funds through the
Operational Program "Education and Lifelong
Learning" of the National Strategic Reference
Framework (NSRF) - Research Funding Program:
“Heracleitus II. Investing in knowledge society
through the European Social Fund”.
REFERENCES
Aigner, D., Lovell, C., Schmidt, P., Formulation and
estimation of stochastic frontier production functions.
Journal of Econometrics, 6, pp. 21–37.
Admassie, A., Matambalya, F., 2002. Technical Efficiency
in Small and Medium Scale Enterprises: Evidences
from a Survey of Enterprises in Tanzania - Easter
Africa. Eastern Africa Social Science Research
Review, 17(2), pp. 1-29.
Assaf, A., Matawie, K., 2008. Cost efficiency modeling in
healthcare food service operations. International
Journal of Hospitality Management, 27(4), pp. 604–
613.
Banker, R., Charnes, A., Cooper, W.W., 1984. Some
Models for Estimating Technical and Scale
Inefficiencies in Data Envelopment Analysis.
Management Science, 30, pp. 1078-1092.
Bryce, C., Engberg, J., Wholey, D., 2000. Comparing the
Agreement among Alternative Models in Evaluating
Hmo Efficiency. Health Service Journal, 35(2), pp.
509-528.
Charnes, A., Cooper, W.W., 1985. Preface to topics in
Data Envelopment Analysis. Annals of Operations
Research, 2, pp. 59-94.
Charnes, A., Cooper, W.W., Rhodes, E., 1978. Measuring
the efficiency of decision-making units. European
Journal of Operational Research, 2, pp. 429–44.
Chen, A., Hwang, Y., Shao, B., 2005. Measurement and
sources of overall and input inefficiencies: Evidences
and implications in hospital services. European
Journal of Operational Research, 161, pp. 447-468.
Chilingerian, J. A., Sherman, H. D., 2004. Health care
applications. From Hospitals to Physicians, from
productive efficiency to quality frontiers. In: Cooper
WW, Seiford LM, Zhu J, editors. Handbook on data
envelopment analysis. Boston/London: Kluwern
Academic Publisher.
Chirikos, T., Sear, A., 2000. Measuring hospital
efficiency: a comparison of two approaches. Health
Services Research, 34(6), pp. 1389-1408.
Coelli, T., 2007. A guide to FRONTIER version 4.1: A
computer program for stochastic frontier production
and cost function estimation. CEPA Working Paper
96/07, Department of Econometrics, University of
New England, Armidale, Australia.
Coelli, T., Rao, D., O’Donnell, C., Battese, G., 2005. An
introduction to efficiency and productivity analysis,
New York: Springer 2nd edition.
Cooper, W. W., Seiford, M., Zhu, J., 2004. Handbook on
Data Envelopment Analysis, Boston: Kluwer
Academic Publisher.
Cordero, J., Pedraja, F., Santin, D., 2009. Alternative
approaches to include exogenous variables in DEA
measures: A comparison using Monte Carlo.
Computers and Operations Research, 36, pp. 2699-
2706.
Desaia, A., Ratick, S., Schinnar, A., 2005. Data
envelopment analysis with stochastic variations in
ICORES2013-InternationalConferenceonOperationsResearchandEnterpriseSystems
102

data. Socio-Economic Planning Science, 39, pp. 147–
164.
Farrell, M., 1957. The measurement of productive
efficiency. Journal of the Royal Statistical Society,
120(3), pp. 253-281.
Giuffrida, A., Gravelle, H., 2001. Measuring performance
in primary care: Econometric analysis and DEA.
Applied Economics, 33(2), pp. 163-175.
Gong, B., Sickles, R., 1992. Finite sample evidence on the
performance of stochastic frontiers and data
envelopment analysis using panel data. Journal of
Econometrics, 51, pp. 259-284.
Hollingsworth, B., 2008. The measurement of efficiency
and productivity of health care delivery. Health
Economics, 17(10), pp. 1107–1128.
Ippoliti, R., Falavigna, G., 2012. Efficiency of the medical
care industry: Evidence from the Italian regional
system. European Journal of Operational Research,
217, pp. 643-652.
Jacobs, R., 2001. Alternative methods to examine hospital
efficiency: Data Envelopment Analysis and Stochastic
Frontier Analysis. Health Care Management Science,
4, pp. 103-115.
Katharaki, M., 2008. Approaching the management of
hospital units with an operation research technique:
The Case of thirty two Greek Obstetric and
Gynaecology Public Units. Health Policy, 85(1),
pp.19-31.
Katharakis, G., Katostaras, T., 2012. SFA vs. DEA for
measuring healthcare efficiency: A systematic review.
Health Policy, (under review).
Lee, R., Bott, M., Gajewski, B., Taunton, R., 2009.
Modelling Efficiency at the Process Level: An
Examination of the Care Planning Process in Nursing
Homes. Health Services Research, 44(1), pp. 15–32.
Linna, M., 1998. Measuring hospital cost efficiency with
panel data models. Health Economics, 7, pp. 415-427.
McDonald, J., 2009. Using least squares and tobit in
second stage DEA analyses. European Journal of
Operational Research, 197, pp. 792–8.
Meeusen, W., Van den Broeck, J., 1977. Efficiency
estimation from Cobb-Douglas production function
with composed error. International Economic Review,
18, pp. 435-444.
Minvielle, E., Dervaux, B., Retbi, A., Aegerter, Ph.,
Boumendil, A., Guincestre, M., Tenaillon, A., Guidet,
B., 2005. Culture, Organizations, and Management in
Intensive Care: Construction and Validation of
Multidimensional Questionnaire. Journal of Critical
Care, 20(2), pp. 126-38.
Minvielle, E., Phillipe, A., Dervaux, B., 2008. Assessing
Organizational Performance in Intensive Care Units: A
French Experience. Journal of Critical Care, 23, pp.
236-44.
Mortimer, D., 2002. A Systematic Review of Direct DEA
vs SFA/DFA Comparisons, Working Paper 136,
Centre for Health and Evaluation, Australia.
Mutter, L., Rosko, D., Greene, H., Wilson, W., 2011.
Translating frontiers into practice: taking the next
steps toward improving hospital efficiency. Medical
Care Research and Review, 68(1), pp. 35-195.
Nedelea, C., Fannin, J., 2012. Efficiency Analysis of Rural
Hospitals: Parametric and Semi-parametric
Approaches. In Southern Agricultural Economics
Association Annual Meeting, 4-7 February 2005,
Birmingham, Alabama.
Newhouse, J., 1994. Frontier estimation: how useful a tool
for health economics? Journal of Health Economics,
13, pp. 317-322.
Ondrich, J., Ruggiero, J., 2001. Efficiency measurement in
the stochastic frontier model. European Journal of
Operational Research, 129, pp. 434-442.
Prochazkova, J., 2011. Efficiency of Hospitals in the Czech
Republic: DEA & SFA Applications. Ph.D. Faculty of
Social Sciences, Institute of Economic Studies,
Charles University in Prague.
Rosko, D., Mutter, L., 2011. What have we learned from
the application of stochastic frontier analysis to U.S.
hospitals? Medical Care Research and Review, 68(1),
pp. 75-100.
Simar, L., Wilson, P., 1998. Sensitivity analysis of
efficiency scores: How to bootstrap in nonparametric
frontier models. Management Science. 44, pp. 49–61.
Simar, L., Wilson, P., 1999. Estimating and bootstrapping
Malmquist indices. European Journal of Operational
Research, 115, pp. 459–471.
Simar, L., Wilson, P., 2000a. A General methodology for
bootstrapping in non-parametric frontier models.
Journal of Applied Statistics, 27, pp. 779–802.
Simar, L., Wilson, P., 2000b. Statistical inference in
nonparametric frontier models: The state of the art.
Journal of Productivity Analysis, 13, pp. 49–78.
Simar, L., Wilson, P., 2007. Estimation and inference in
two-stage, semi-parametric models of production
processes. Journal of Econometrics, 136, pp. 31-64.
Wilson, P., 2010. FEAR 1.15 User’s Guide. Available at:
<http://www.clemson.edu/economics/faculty/wilson/S
oftware/FEAR/FEAR-1.15/fear-user-guide.pdf>
[Accessed 25 July 2012].
AnEmpiricalComparisonofDEAandSFAMethodtoMeasureHospitalUnits'Efficiency
103
