
Paradigm Shifts in Health Informatics
Luca Dan Serbanati
1
and Serban Radu
2
1
Dept. of Engineering Taught in Foreign Languages, Politehnica University, Spl. Independentei 313, Bucharest, Romania
2
Dept. of Computer Science, Politehnica University, Spl. Independentei 313, Bucharest, Romania
Keywords: Paradigm Shift, Business Modelling, Digital Ecosystem, Multi-agent System, Virtual Health Record.
Abstract: There are many reasons to reflect upon the importance of paradigms in healthcare, their explicit use in
health system restructuring and the possibility to anticipate the health field evolution with paradigms. For
instance, it is known that an improving or restructuring strategy is needed to adapt health systems to major
changes in the way of thinking or doing that occurred in the recent years in the health sector and the society.
Such changes are often characterized as paradigm shifts where a paradigm is intended as a reference model
of fundamental value widely accepted in a particular sector of activity. The paper claims that an explicit use
of paradigms can speed up the restructuring process in healthcare. Some paradigms recently transferred
from business modelling and engineering to healthcare could be more helpful if explicitly used in health
system restructuring. Two recent paradigms in software engineering that will be found particularly useful to
health informatics are also introduced.
1 INTRODUCTION
It's a fact that in many countries, in the presence of
considerable demographic changes, national health
systems have achieved over many years high cost
levels that potentially continue to rise. These costs
are not accompanied by corresponding effectiveness
and efficiency in provided services. Moreover, the
services offered are characterized by on the whole
modest levels of quality, especially in the perception
of citizens who are the main contributors to the
system. In such a situation any business should settle
upon a restructuring of its organization and
processes that involves redeployment of functions,
assets, and risks between associated organizations,
but also conversion of business processes.
In fact, the governments of these countries are
pursuing a restructuring strategy of national health
systems to adapt them to new needs and epoch-
making changes that occurred in the recent years in
the society and the world. Such major changes in the
way of thinking about something or do something
are often described as a paradigm shift.
A paradigm is a reference model of fundamental
value widely accepted in a particular area that could
be a current of thought or a sector of manufacturing
activity. A paradigm emphasizes relationships
between some fundamental concepts that shape the
thinking in that area. It is derived from a specific
way of thinking, communicating and viewing the
world, based on a specific system of values which
leads to a specific representation of the world. A
paradigm is thus an expression of a comprehensive
belief system or world view that guides research and
practice in a field. It works at the subconscious level
and moves tacit knowledge by a series of implicit or
explicit assumptions that synthesize a set of
experiences, beliefs and values, and influence how
an individual perceives an area of the real world or
reacts to this perception. At the same time, a
paradigm may be used as a benchmark to assess
methods or conceptual tools that are related to the
paradigm goal or idea.
The aspect we are interested with in this paper is
how to use paradigms for transferring knowledge
across domains. Let consider the following example.
When restructuring occurs for health systems a
local health organization or a regional health system
can be viewed as a small or, respectively, large
industrial company and restructuring measures in the
health sector can be the same or very similar to the
measures that typically take place in companies with
the purpose of making them more profitable, or
better organized for their current needs. But one
wonders: the knowledge gained in engineering
companies may be transferred in health as paradigms
256
Serbanati L. and Radu S..
Paradigm Shifts in Health Informatics.
DOI: 10.5220/0004328102560262
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2013), pages 256-262
ISBN: 978-989-8565-37-2
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)
to improve, innovate, or even re-engineer the
healthcare system and its subsystems?
To answer this question a review was carried out
of various paradigms that were invoked in the last
years as panacea for many problems in healthcare
activities. An analysis of their motivation in
healthcare as well as of their possible origin in
similar paradigms of other activity sectors was
carried out. First, brief presentations of emerging
paradigms in healthcare are given in the next
section. Paradigms from other human activity
sectors that were transferred to health are presented
in the followings sections of the paper.
This paper regains an idea from (
Serbanati, 1992)
in accordance with which the explicit use of
paradigms in modelling and designing software
systems can significantly improve the quality of both
the development process and the final product. A
similar idea we find in the use of design patterns and
architectural styles in software engineering,
observing that in the case of paradigms the initial
model is more general and highly abstract.
Advances in information technology (IT)
brought the seeds for a new sector in healthcare: "e-
health" based on an IT-supported care practice. Thus
it is natural that many paradigms in e-health are
echoes of paradigms in systems and software
engineering that we use to restructure businesses and
for software development. Their presentation could
help us to understand how we can use them to
restructure health systems in the view of challenges
currently facing health care delivery systems.
Because a paradigm moves much specific
knowledge that synthesizes experiences, beliefs and
values, we claim that any paradigm transfer from
engineering to healthcare represents an enrichment
of the knowledge in the health domain and provides
it with new approaches to its problems.
Generally speaking, transfer of paradigms from a
domain to another involves organization, creation
and distribution of knowledge, and ensures its
availability for future users. The new paradigms are
related not only with theories and "common sense",
but mainly with the current trends in healthcare. The
transfer may affect either the way of interpreting
phenomena in health or the models and patterns
accepted by the medical academic and scientific
community to analyze these phenomena.
2 PARADIGM-ORIENTED
MODELING AND DESIGN
It is worthy to note that paradigms usually
emphasize only few aspects of the reality of
reference: those concerning our interest for a limited
understanding of existing situations in the real world
or those that are sufficient for us to initiate the
design of new artefacts.
Our claim is that a paradigm may guide research
and practice in different areas of human endeavour.
It can be used as a structuring schema in both
teaching and model-driven design processes.
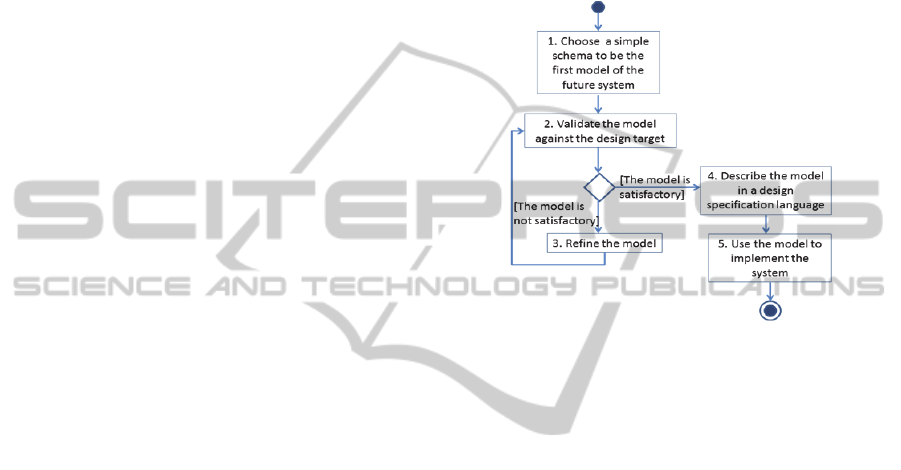
Figure 1: The paradigm-based design process.
According to (Serbanati, 1992) a paradigm-based
design process goes through 5 steps (Figure 1):
1. An appropriate initial schema is
identified/chosen. The schema is an intuitive,
summarized structure, a kind of primary, very
simple model that features the main elements of the
system to be designed. Such an initial schema has a
very general, often fuzzy specification and requires
our intuition for its full understanding. It may be a
paradigm or a meta-model with a paradigmatic
function that originates from our basic knowledge of
the reality where the system to be modeled will
evolve, and experience in approaching this reality. In
the following steps models of the target system will
be iteratively built from this initial schema.
2. Models are continually validated against the
target during the system construction. The cycle
ends when a model that satisfactorily represents the
target’s properties and behavior is obtained.
3. The current model is refined, by bringing new
ideas, practice or technology elements, in order to
match the validation criteria.
4. Once validated, the model is described in a
suitable design specification language.
5. The final model is used for the system’s detailed
design and implementation.
ParadigmShiftsinHealthInformatics
257

3 PARADIGMS IN HEALTH
A business model is an abstract model that
summarizes the way we observe and understand
things and events that belong to the reality of the
business
we want to study or engineer. It describes
the logic of how an individual, group or organization
creates and disseminates economic, social or other
forms of value. A business model may also express a
meaningful view of an existing business or a future
one and building the model is an integral part of the
enterprise’s strategy. Consequently, any business
change should be model-based. This is why to
restructure health systems as business organizations
a model-based approach is needed. To transfer
know-how from the corporate business restructuring
to the restructuring of organizations and activities in
the healthcare system some paradigms of business
modelling can be usefully transferred, eventually
with some changes of connotation, in healthcare.
Business models can be defined and
conceptualized according to various paradigms that
often appear us like some very synthetic models or
meta-models. Examples can be the REA model
initially coined for accounting (McCarthy, 1982) and
successively extended to enterprise information
systems (Geerts, 2000), and Zachman’s framework
(Zachman, 2008).
Let consider two paradigms the authors used to
model various health-related environments.
Figure 2 shows a schema for modelling the
business in software companies that was proposed in
(Serbanati, 1992). It is an example of high-level
meta-model acting as paradigm. It emphasizes the
main components of business processes and their
relationships, while other business aspects such as
business functions or organization are ignored.
Figure 2: A business meta-model (Serbanati, 1992).
According to this paradigm any business model
should specify the business main activities and
entities that support these activities. The entities play
some well-defined, proactive or passive roles in
business: agent, object or resource, and tool.
Activities are transformations that get outputs from
some inputs in order to meet a pre-defined objective.
They are carried out by agents who act upon
business objects with the aid of tools, as extensions
of human capabilities, to produce outcomes
consisting of business objects, too. For each
component in the meta-model (Serbanati, 1992)
proposes a paradigm that can be used by the analyst
to approach entities in the real world she/he wishes
to model: the multifaceted object for (business)
objects, the processor for agents and tools, and the
process for activities. Such a paradigm may be used
as initial model in a model-driven process as Figure
1 shows.
The meta-model in Figure 2 was successfully
applied for modelling important healthcare activities
as business processes: medical care in (Grifoni,
1995); (Grifoni, 1996) and (Luzi, 1997), home
recovery in (Luzi, 1996), and clinical trials in (Fazi,
2004) and (Serbanati, 2005).
HL7 (Health Level Seven) is a standardization
organization involved in development of standards
of healthcare informatics interoperability
(http://www.hl7.org, n.d.). HL7 version 3 introduces
HL7 Development Framework (HDF), an object-
oriented development methodology for continuously
evolving message specifications that assure semantic
interoperability between healthcare applications.
The cornerstone of the HDF methodology is the
Reference Information Model (RMI), a UML class
diagram that specifies the healthcare concepts which
must be documented and/or communicated as
messages within a specific clinical or administrative
context, and their semantic and syntactic
connections.
From the RIM HDF first derives domain-specific
information models that are then transformed
through a series of rule-based refinement processes
to yield a static model of the information content of
messages to be exchanged by the healthcare
applications belonging to the domain.
Figure 3: The RIM HL7 V3 meta-model.
Any clinical and administrative concept in RIM
is derived from one of six core classes that compose
the HL7 meta-model (Figure 3). This meta-model
HEALTHINF2013-InternationalConferenceonHealthInformatics
258

forms a kind of high-level, abstract grammar for
making statements about the delivery of medical
care.
In the meta-model Act represents actions and
events that make up health services. Entity
represents physical things or beings. Role is a model
of socially expected behaviour of an entity. RoleLink
represents relationships between two individual roles
played by entities. ActRelationship represents the
ability of two acts of relating with each other.
Participation instances indicate contexts for an act
in terms such as: who performed it, for whom it was
done, where it was done, etc.
It has become evident in recent years that HDF
encompasses not only HL7 standard message
specifications but may include standards resulting
from analysis of new electronic health record
architectures and requirements. (Serbanati, 2011)
introduces an extension of the HDF scope for
designing a virtual healthcare record in the Lumir
system. Lumir is a software platform that enables
semantic interoperability in collaboration of
caregivers who assist the same patient.
The Lumir experience convinced us that the RIM
meta-model might be widely used to model any
business. We consider it a true paradigm that helps
us not only for specification of messages between
healthcare applications but also for modelling any
business system in any other sector of activity that
involves entities playing roles and participating in
acts. By transferring the HL7 approach to business
systems we can model any business as a framework
where some real-world entities exist and some
intentional actions (called acts) are performed.
Many paradigms are arising in healthcare to
respond to huge challenges and mark epochal
changes in the domain. They are focused on cost
control as "pay for performance", the quality of
services as "personalized medicine", “medical
home” and "evidence-based medicine", or the
citizens’ perception of the quality and efficiency of
the health system as "patient care-centric” and
"patient empowerment" paradigms.
All these paradigms require radical changes of
mentality and extensive revisions of health
organizations. Our claim is that the explicit use of
paradigms in healthcare can substantially change the
landscape of health, provided that a "cultural"
evolution to happen and that they penetrate the
doctors’ mindset and medical practice. A major shift
in attitude will take place when care providers will
realize that the critical element in work the ability to
exchange ideas, information and knowledge in a
collaborative environment and recognize the value
in empowering their patients to collaborate.
4 PARADIGMS IN E-HEALTH
The carrier of many recent changes in healthcare are
the advances in IT, particularly in computer
networks, technological solutions for managing and
sharing the patient’s clinical history, and web
technologies. IT has made possible the development
of some new paradigms in health informatics.
Today, it is a fact that to assess the quality and
effectiveness of their services, healthcare systems
are relying on information systems. Progress in IT
has opened the door to the restructuring of the health
sector, stimulating the emergence of new paradigms,
some of them acquired from IT itself.
The evolution that IT pursued in health initiated
from the needs of system innovation essentially
focused on goals of "efficiency" and only later it
joined the responsibility of re-construction of the
relationships between caregivers and with their
patients. The result was e-health, a new, not only
technological, but also scientific field in the
intersection of medical informatics, public health
and business. It is the key field that facilitated
transfer of paradigms from systems and software
engineering to healthcare. (Eysenbach, 2001)
“Interconnecting health” is a central paradigm in
e-health. It focuses on approaches, challenges, and
solutions affecting the ability to connect health
organizations and systems, and the role of IT as an
enabler in achieving this connectivity. Collaboration
between all stakeholders is a key element to creating
new health systems, more efficient in easily
conversion of knowledge on the health of citizens in
therapies that benefit the health. The growth in
importance of electronic health records in the last
two decades marked a technological but also
"cultural" shift:
1. EMR (Electronic Medical Record), a
computerized medical record created and used in an
organization that delivers care, such as a hospital or
physician's office.
2. EHR (Electronic Health Record), an evolving
concept defined as a systematic collection of digital
information about individual patients’ health thanks
to all contributions of information that GPs,
hospitals, and laboratories caring them supply with.
(Contenti, 2010)
3. PHR (Personal Health Record), an electronic
health record that grants patients access through the
web to a wide range of health information sources,
ParadigmShiftsinHealthInformatics
259

best medical practices and health knowledge and
where health data related to the care is entered by
the patient himself/herself.
4. VHR (Virtual Health Record) is a Web 2.0
evolution of the EHR concept with a more
emphasized vocation towards collaboration,
coordination and integration. (Contenti, 2010) and
(Serbanati, 2011) introduce VHR as an internet
resource that provides healthcare applications with a
comprehensive and authoritative representation of
the current health state, medical history and ongoing
treatments of any subscribing citizen. This
information is stored in a longitudinal, distributed
repository and highly structured according to various
criteria: clinical contacts, episodes of care, health
issues, care providers, medical equipment,
organizations, individual and territorial jurisdictions.
VHR provides more than a comprehensive, uniform,
and consistent data source: with its proactive
behaviour it is a trusted partner for the caregivers
who jointly support integrated and patient-centric
care processes in a Regional Health Information
Organization (RHIO). VHR can support the care
workflow and evidence-based decisions, quality
management, and reporting.
We observe that the evolution “Interconnecting
health” was a continuous broadening of the horizon
of interoperability in health from EMR to RHIO,
that is an extension to an ever larger community of
the opportunity to share and communicate
information using collaboration of healthcare
applications running on heterogeneous platforms.
5 NEW PARADIGMS IN HEALTH
INFORMATICS
Current advances in systems and software
engineering give us a glimpse of the next generation
of information systems supporting healthcare. While
current efforts in e-health are focused on the
development of information systems based on
service-oriented architectures, in the near future a
shift will be towards integration of healthcare
information systems (HISs) in multi agent systems
(MAS). In the long run when more and more
heterogeneous health applications will be highly
integrated in national and regional HISs a new
paradigm, the digital health ecosystem (DHE), could
be used to model them. A DHE consists of virtual
entities, information and knowledge sources, and
applications that adapt to local needs will be created.
An intelligent agent is a software component
with autonomous behaviour similar to human agents.
It has the following characteristics: autonomy,
sociality, pro-activity, mobility, and reactivity.
Agent-based health applications require a
population of agents knowing health ontologies and
working together in an MAS to solve problems on
behalf of patients, organizations, professionals, or
even of the agents themselves. The MAS paradigm
could be used to model, design and implement
software platforms that integrate software
applications in healthcare systems. Such an approach
has many advantages over a traditional approach.
An agent-based paradigm is a more natural way
to represent many situations that often occur in
medical settings, such as: absence of a
comprehensive control system, limited or
insufficient resources for a care provider to solve a
given problem, and geographical distribution of the
needed information and knowledge. On the other
hand, in health systems we can identify many
recurrent features common to MASs: delegation of
responsibility, re-allocation of tasks, need to
consider a large variety of user concerns and
problems, planning the collaborative work , think
and work in open spaces, etc. Moreover:
1. Agents related to each other can be easily put
together in an organized community to efficiently
coordinate and perform operations of recovery,
analysis and integration of information originating
from geographically distributed sources.
2. Interoperability of legacy systems in health
systems are facilitated by the MAS approach.
3. A network of interconnected agents better model
distribution of computing resources and capacity in
the existing health system.
In the case of “agentification” of a regional health
system, all stakeholders (care providers,
professionals, patients and their relatives) must be
represented as agents in the system. We called
“avatar” such an agent. It presents itself to other
agents with the role of the stakeholder it represents.
An avatar is characterized by a stressed pro-
activeness acting with own initiatives on behalf of
an individual. Other virtual entities in the system
may represent real organizations but also virtual,
temporary, ad-hoc created organizations as teams of
professionals involved in the patient’s care process.
For instance, the avatar representing the patient
should present itself as a manager of the patient’s
VHR and respond to queries regarding its content,
interact with other agents to update the VHR, and
interact with the patient to monitor her/his health
state, notify her/him about relevant events and
update its own information on the patient’s concerns
HEALTHINF2013-InternationalConferenceonHealthInformatics
260

and the context where the patient is currently found.
To “agentify” an HIS, additional agents are
needed to provide services to avatars, interact with
medical devices and other applications, supervise
execution of care plans, play the role of mediators,
or negotiate access permissions to a central authority
that provides proper authentication and authorization
management. (Vasilateanu, 2011)
A natural ecosystem is a biological community
of interacting organisms plus their physical
environment. Correspondingly, a health ecosystem
can be defined as a network consisting of a
multitude of health service suppliers and consumers,
and healthcare organizations and institutions, all of
them supported by HISs. Organisms of the health
ecosystem are care suppliers and consumers and the
environment is composed of their shared resources.
Digital business ecosystem is a self-organising
digital infrastructure aimed at creating a digital
environment for networked organisations that
supports the cooperation, the knowledge sharing, the
development of open and adaptive technologies and
evolutionary business models. (Nachira, 2007),
(www.digital-ecosystems.org/, n.d.).
(Serbanati et al., 2011) introduces the digital
health ecosystem (DHE) as an IT infrastructure
designed to support activities in the health
ecosystem. Figure 4 shows the relationship between
the health ecosystem and its DHE. The synergy of
the two ecosystem is based on a continuous osmosis
of information and knowledge flows between them:
avatars gradually acquire digital representations of
real world entities, clinical documents, and
knowledge from the health ecosystem and deliver
processed information in the real world.
DHE is composed of a hierarchically organized
network of local digital ecosystems that mirror the
organizations in the real world and preserve their
identity and own knowledge.
Figure 4: Health ecosystem and its digital ecosystem
(Serbanati et al., 2011).
The DHE infrastructure becomes a resource in
the health ecosystem, that manages virtual entities
and avatars. It allows them to share digital resources
and interact with each other on behalf of
organizations and individuals in the real world. The
infrastructure also implements self-generation
mechanisms that enables DHE to include more
functions of knowledge interpretation and to gain
more high-level services, in other words to become
more intelligent and provide more support for the
health ecosystem.
5 CONCLUSIONS
This paper aims to open a discussion on the role of
paradigms in our reasoning and proposes the use of
innovative paradigm-based solutions in one or
another field of activity. A paradigm better captures
the nature of the differences between different
approaches to solve a problem.
There are many reasons to reflect upon the
importance of paradigms in healthcare, their explicit
use in restructuring health systems and possibility to
anticipate the health field evolution with paradigms.
Explicit use of paradigm shifts shows how better
control knowledge transfers between science fields.
In particular, paradigm shifts in health informatics
are good go-betweens in transferring knowledge to
and from healthcare.
ACKNOWLEDGEMENTS
This work was supported by the project ERRIC No.
264207, FP7-REGPOT-2010-1.
REFERENCES
Contenti, M. at al., 2010. The Region-Wide EHR-s in
Basilicata: the Lumir System. In C. Safran et al. (eds),
Studies in Health Technology and Informatics, v.160,
pag. 327 – 331, IOS Press.
Eysenbach, G., 2001. What is eHealth? J Med Internet
Res;3(2):e20.
Fazi, P. et al., 2004. Toward a model of clinical trials. In
Procs. ISBMDA’04, pag.299-312.
Geerts, L. G., McCarthy, E. W., 2000. The ontological
foundation of REA enterprise information systems.
Working paper, Michigan State University.
Grifoni, P. et al., 1995. Modeling the management of
protocols as the kernel of a healthcare information
system. In Medinfo ’95, pag. 502-5.
ParadigmShiftsinHealthInformatics
261

Grifoni, P. et al., 1996. Towards an information system
architecture of healthcare units. In ER'96, Berlin.
Health Level Seven International, n.d. HL7 version 3,
www.hl7.org .
Luzi, D. et al, 1997. Extending the standard architecture
for healthcare units: the guideline server. In J. Dudeck
et al. (Eds.), New technologies in hospital information
systems. pp 95-101, IOS Press.
Luzi, D. et al, 1996. The virtual hospitalization, towards
an information-organization system architecture. In J.
Brender et al. (Eds.) Medical Informatics Europe '96,
vol. 34, pp. 710-714, IOS Press.
McCarthy, E. W., 1982. The REA accounting model: A
generalized framework for accounting systems in a
shared data environment. The Accounting Review, pag.
554–78.
Nachira, F. et al., 2007. Digital Business Ecosystems,
www.digital-ecosystems.org/book/Section0.pdf .
Serbanati, L. D., 1992. Integrating tools for software
development, Yourdon Computing Series, Prentice
Hall.
Serbanati, L. D. et al., 2005. Modelling medical research
processes to set up a clinical trial management system.
In Cunningham P., Cunningham M. (eds) Innovation
and the Knowledge Economy. Issues, Applications,
Case studies, pag. 904-11, IOS Press.
Serbanati, L. D., Ricci, F., Mercurio, G., Vasilateanu, A.,
2011. Steps towards a digital health ecosystem.
Journal of Biomedical Informatics, Vol. 44, Issue 4.
Vasilateanu, A., 2011. An agent oriented architecture for
supporting the digital health ecosystem, PhD Thesis,
Politehnica University of Bucharest.
Zachman, J. A., 2008. The Zachman Framework: The
official concise definition, Zachman International,
zachman.com/about-the-zachman-framework .
www.digital-ecosystems.org
HEALTHINF2013-InternationalConferenceonHealthInformatics
262
