
Mobile App and Website for Major Depression Monitoring
Àngela Nebot, Francisco Mugica and Luca Abdollahi
Soft Computing Group, Technical University of Catalonia, Jordi Girona Salgado 1-3, Barcelona, Spain
Keywords: Major Depression, Remote Intelligent Monitoring, Mobile Phone Application, Website, Android.
Abstract: One of the challenges for the patients diagnosed with major depression is not to experience relapse or
reoccurrence which are very common characteristics of major depression. Providing constant monitoring of
these patients during their daily life for the first year of their depression can have a significant impact on
preventing these patients to experience reoccurrence and relapse. In this paper we describe an intelligent
remote monitoring system that is in the process of development and present the new research done centered
on the interaction between the system and the actors involved, i.e. patients, psychiatrists and primary care
physicians. This interaction is done through an android application for mobile telephones and a Website.
The specification and design of the information requested and submitted to system actors through both
platforms is performed by the communication module, which is also described in this research.
1 INTRODUCTION
Depression is a common mental disorder that
according to World Health Organization is affecting
121 million people worldwide (WHO, 2012).
Compared with other medical diagnoses, depression
is very common. It is twice as frequent in women
comparing to men and it can begin at any age, but its
average age of onset is in the middle of the 20s.
Lifetime prevalence estimates for major depressive
disorder in the community range from 15% to 17%,
one year prevalence range from 6% to 7% (Ebmeier
et al., 2006). A crucial aspect of the epidemiology of
major depression is the increased mortality
associated with this condition. A recent meta-
analysis of 25 studies with 1.3 to 16 years´ follow-
up of over 100,000 individual reported an overall
relative risk of dying between 1.58 and 2.07
compared with people who are not depressed.
According to studies, a sixth of people in the
community will have major depressive disorder
during their lifetime (Ebmeier et al., 2006).
Major depression is traditionally considered a
treatable mental disorder. Nevertheless up to 50% of
such patients may not have a satisfactory response in
spite of adequate trials of antidepressant drugs
(Fava, 2003). Even if they respond to medication
still there is a high risk of relapse or recurrence.
Naturalistic studies have found that most patients
will eventually experience either a relapse (another
depressive episode within 6 months after response)
or recurrence (another depressive episode after 6
month elapsed) if followed for a long enough period
without sustained treatment. After 15 years, almost
90% of the patients could be expected to become
depressed again after experiencing an acute
depressive episode (Nierenberg et al., 2003). One
widely accepted method for preventing relapse or
recurrence is long-term pharmacotherapy.
Depression is ranked as third among disorders that
cause global disease, with all the concomitant
economic costs to society and will rank as first in
high-income countries by 2030 (Waraich et al.,
2004). Even beyond the assessment of global and
national costs, the personal cost of depression is
enormous. Half of the people suffering a first
episode of depression will develop chronic or
recurrent disorder and spent more than 20% of their
life in a depression condition (Cuijpers et al., 2012).
On the other hand due to the large epidemic
character of major depression it becomes impossible
that psychiatrists can carry out a continuous
supervision of the patient in the short time during the
healing process and a long term observation after the
full recovery.
Moreover, once diagnosed and prescribed by a
psychiatrist, the follow-up of patients is usually done
by primary care physicians, which give follow-up
appointments to the patients every 3 months to
analyze their evolution and make changes in the
medication if required.
605
Nebot À., Mugica F. and Abdollahi L..
Mobile App and Website for Major Depression Monitoring.
DOI: 10.5220/0004621606050612
In Proceedings of the 3rd International Conference on Simulation and Modeling Methodologies, Technologies and Applications (HA-2013), pages
605-612
ISBN: 978-989-8565-69-3
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)
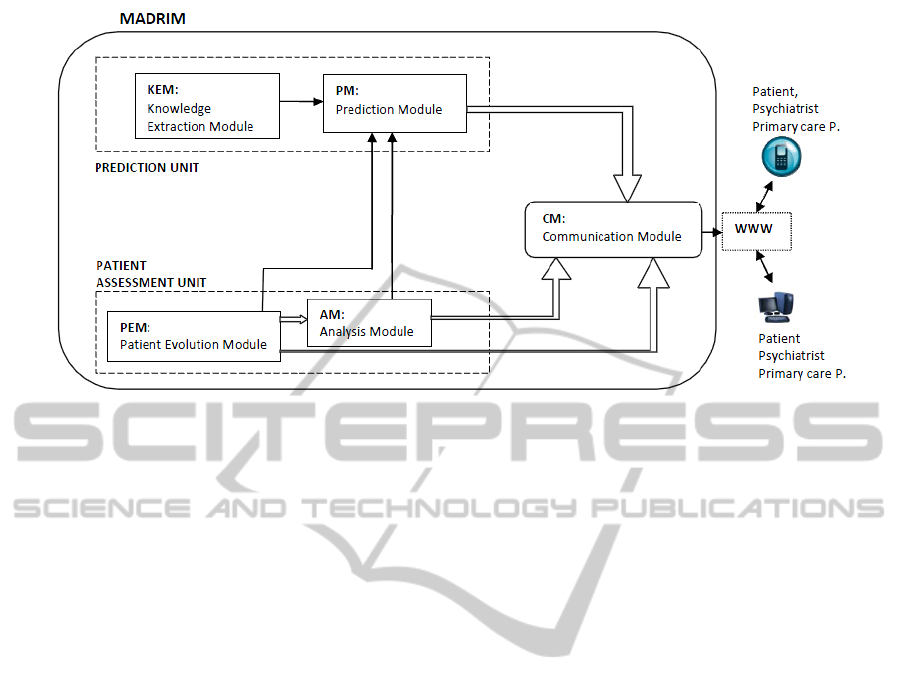
Figure 1: Architecture of the MADRIM remote intelligent monitoring and prediction system.
Therefore, in the major depression disorder there is a
clear gap of supervision and continuous attention to
the patients, when in reality this type of patient
needs greater oversight in order to ensure, as much
as possible, to take the pills.
Automatic monitoring is a tool which can prove
vital to mitigate these problems and give greater
attention to the patient. In addition, advances in
telecommunication and sensors technologies make
the task of developing ubiquitous monitoring
feasible and of great usefulness. Moreover, the
widespread use of mobile phones and computers
make continuous remote follow-up of the patient
completely feasible and practical.
Our recent work is focused on the development
of an intelligent remote monitoring and prediction
system, called MADRIM, for MAjor Depression
Remote Intelligent Monitor, to help physicians in the
process of supervision and give continuous attention
to the patients. We think that a monitoring system
that provides clear and concise information to both
patients and physicians, keeps them informed of the
evolution of patients in a short term basis and alerts
them in the case of necessity is a valuable
contribution if the goal is to offer monitoring to a
massive number of patients. Moreover, predictions
of the evolution of the patient in the near future and
prediction of relapse and reoccurrence would be of
great interest to psychiatrist if included in the
system.
This paper is centered on the part of this system
that interacts with the actors, which are patients,
psychiatrists and primary care physicians. A mobile
App and Website are developed and presented in
this research allowing the continuous interaction
with all the actors involved in the intelligent remote
monitoring system, each one with its specific role.
The first part of the paper presents the whole
intelligent monitor architecture and describes shortly
the developments already performed. The second
part of the paper presents the new developments
centered on the interaction between the system and
the actors involved in the major depression disease.
Finally the conclusions are presented and the future
work is outlined.
2 INTELLIGENT REMOTE
MONITORING SYSTEM
The architecture of MADRIM is presented in Fig. 1.
MADRIM is composed of two units: the patient
assessment unit and the prediction unit.
The goal of the patient assessment unit is to
follow the evolution of the patient during his/her
recovery in order to understand its behavior and
provide support to patients, psychiatrist and primary
care physicians. The prediction module has the goal
of going a step further and forecast the evolution of
the patients some time in advance taking into
account the patient assessment at this time and the
knowledge obtained from data mining of registered
major depression data.
The patient assessment unit is already developed
and it is based on rule-based models derived from
experience and expert knowledge (Mugica et al.,
2012). The prediction unit is still being developed
and it is based on knowledge extracted from real
data by means of the Fuzzy Inductive Reasoning
SIMULTECH2013-3rdInternationalConferenceonSimulationandModelingMethodologies,Technologiesand
Applications
606

(FIR) data mining technique (Escobet et al., 2008).
MADRIM is implemented in java.
The communication module has the function of
transmitting the results of the patient assessment unit
and the prediction unit to those actors involved in
the healing process, i.e. psychiatrists, physicians and
patient. To this end the interaction with the patient,
psychiatrist and primary care physicians is done by
means of a Website and a mobile App under android
platform.
2.1 Patient Assessment Unit
The idea behind the patient assessment unit is to
develop a multi-factor monitor that allows following
the evolution of the patient during his/her recovery
in order to understand its behavior and also to
provide support that helps to preventing the relapse
of depression. It receives the following information
(input data): the clinical data of the patient (personal
information and clinical history); patient’s mood and
life events that are obtained from patient’s responses
to specific questionnaires (e.g. PHQ-9, Brugha, etc.)
and physiological data streaming from sensors as for
example weight, sleep and movement. Although the
patient assessment module is designed in a generic
form, i.e. it works with any of the available
psychiatric questionnaires, in the description
presented here the PHQ-9, Brugha and M.I.N.I
questionnaires are used to describe the design and
development of the different modules and to validate
its functioning. The PHQ-9 is a depression
assessment tool, which scores each of the 9
diagnostic criteria of mental disorders. The
questionnaire is designed to assess the patient’s
mood over the last 2 weeks (The Macarthur, 2013).
It is important to notice that the PHQ-9 is an
extensively used questionnaire that has been
validated in several studies and that is useful not
only for major depression diagnosis but also for
patient’s evaluation. It has also been proved that this
kind of questionnaires can also be applied through
the telephone obtaining reliable results (Pinto-Meza
et al., 2009). The Brugha questionnaire is a self-
report questionnaire that examines the incidence of
12 categories of negative life events over the
previous 6 months (Brugha et al., 1985). The
questionnaire assesses life stressors involving
moderate or long-term threat such as illness or
injury, death of a close friend or relative,
unemployment, financial loss and loss of important
relationships. The use of this questionnaire in our
system is not to support the initial diagnosis, but to
help to understand certain variations in patient
evolution that would be inexplicable without this
information.
The Mini-International Neuropsychiatric
Interview (M.I.N.I.) is a short structured diagnostic
interview, developed jointly by psychiatrists and
clinicians in the United States and Europe, designed
to meet the need for a short but accurate structured
psychiatric interview for multi-center clinical trials
and epidemiology studies and to be used as a first
step in outcome tracking in non research clinical
settings (Sheehan et al., 1997). Although it has
several modules, in this research we only use the
suicidal risk questionnaire, in order to detect suicidal
intentions. In the case that the question 9 of the
PHQ-9 takes its highest value, more information is
needed to distinguish between thoughts of death
(relatively common in patients with depression, that
do not necessarily imply thoughts of suicide) and the
real thoughts of suicide. In this case the M.I.N.I
questionnaire is presented to the patient in order to
get more information related to the suicidal risk.
The patient assessment unit is composed of the
Patient Evolution Module (PEM), inspired on a
qualitative reasoning and the Analysis Module
(AM), based on expert knowledge and pattern
recognition models.
The PEM allows tracing the progress of the
patients in a short time basis (15 days) in order to
characterize their re-establishment to the mental
health pattern. The PEM is centered on the overall
rate of PHQ-9 questionnaire that is responded by the
patients every two weeks.
The AM receives the short-term patient evolution
status, which is the output of the PEM. From this
knowledge and together with the input data
described before, it defines a framework for
assessing both the process of healing and the
patient's risk/hazard level for each stage of
treatment. The word risk is used here in the sense of
defining the level of patient’s enhancement, so it has
nothing to do with the risk of not taking the pills.
The AM is designed as a rule base model that
processes a set of heterogeneous information related
to the patient with the goal of monitoring and
assessing the process of healing of the patient. Once
diagnosed and prescribed by a psychiatrist, the
follow-up of patients is usually done by primary care
physicians. The objective of the system is to provide
expert information to both physicians and patients
that allow them to know the effectiveness of the
prescribed treatment, at any time. From this point of
view the results of the analysis module must be
quickly and easily interpretable. The set of
heterogeneous information that the analysis module
MobileAppandWebsiteforMajorDepressionMonitoring
607

requires during the reasoning process is the
following:
evolution of the patient state (i.e. the inferred rules
obtained by PEM),
incidence of new major stressful life events (e.g.
Brugha questionnaire change),
significant variations in the physiological data (e.g.
sleep, weight and movement sensors),
preexistence of alarms in the past weeks,
number of weeks passed from the beginning of
medication,
clinical history of patients regarding to prior
suicide attempt or prior recurrence or relapse,
continuous high risk response to persistent suicidal
thoughts (i.e. question 9 of PHQ9 questionnaire
and section C of the MINI international
neuropsychiatric interview).
The rule system of the AM processes this set of
inputs in order to establish the patient treatment
efficiency. AM produces two levels of conclusions.
At one side, it provides a classification that in a very
synthetic way warns if the treatment progresses
successfully, if the evolution is not satisfactory or if
the treatment is failing or if it has a high risk of
failure. On the other side, it stores information about
the rules that have been shot in the reasoning process
and that allow to explain the above classification.
The AM is robust because it is able to deal with
incomplete data, i.e. the patient is not answering the
questionnaires temporally, the system could not save
the data that was generated, etc. In these cases the
analysis module is still capable of performing the
classification and reasoning process.
2.2 Prediction Unit
This unit is composed of the Knowledge Extraction
Module (KEM) and the Prediction Module (PM).
The KEM has as main goal extracting knowledge
from real data that will be used for predicting
patient’s future behavior, especially possible
reoccurrences or relapses. The process starts from
data steaming form the patients. The data available
for real patients are usually: personal data (i.e. age,
gender, marital status, number of children, is
working now?, level of studies, etc.), clinical data
(i.e. previous diagnosis of major depression, has or
not other diseases such are asthma, cancer,
hypertension, neurological, lung, etc., the patient
smokes or drinks), questionnaires (i.e. PHQ9,
Hamilton, SCID depression, SCSR, etc.), treatment
received (i.e. type of antidepressant, frequency and
doses, type of anxiolytic, frequency and doses, type
of hypnotic, frequency and doses, etc.), treatment
effects (i.e. is the patient taking the medication?, has
the patient side effects? which ones?, etc.). These
data is usually registered at the beginning of the
treatment, when the patient is diagnosed, and after 3
and 6 months of the treatment.
The Fuzzy Inductive Reasoning (FIR)
methodology is then used to perform variable
selection and to determine a prediction model that
defines the causal and temporal relations between
the relevant variables and a set of rules. With these
kind of data it usually happens that the quality of the
models obtained are not as good as desired, i.e. the
entropy associated to the model is high. That is why
we think that argumentation can be an interesting
solution. The idea behind working with learning
examples accompanied by arguments is to come up
with machine learning techniques more efficient
through mechanisms of argumentation (Bratko and
Mozina, 2004); (Bratko et al., 2006). The usual task
of machine learning from examples is: given a set of
examples find a theory that is consistent with the
examples. In the case of argument based machine
learning, given a set of examples and supporting
arguments for some of the examples the idea is to
find a theory that explains the examples using given
arguments. The motivation for using arguments in
learning is twofold, 1) arguments impose constrains
over the space of possible hypotheses, thus reducing
search complexity and 2) a model conclusion should
make more sense to an expert as it has to be
consistent with given arguments. It is also important
to take into account that the knowledge that experts
have is usually implicit and they find it extremely
difficult to elicit in the form of a set of rules.
However, experts can rather easy discuss a certain
case, instead of giving a general theory. The experts
should give arguments to some specific examples for
all possible outcomes. The arguments are then given
to an argumentation engine that can use these,
possible contradictive, arguments to make
predictions for new examples. The prediction unit is
now under development, and it is expected to have it
working properly in the near future.
3 INTERACTION
WITH SYSTEM’S ACTORS
The interaction with system’s actors involves two
main tasks. The first one is the specification and
design of the information that should be gathered
from the patients and that the system should offer to
the stockholders. The communication module (CM)
is the responsible for this task. The second one
SIMULTECH2013-3rdInternationalConferenceonSimulationandModelingMethodologies,Technologiesand
Applications
608

corresponds to the physical means by which the
stakeholders have access to the monitoring process.
In this case a mobile App and a Website. In this
section both crucial developments are described in
detail.
3.1 Communication Module
The CM is the responsible to sort out the risk data
that is derived from the AM and to provide the
adequate information to the different actors involved
in the treatment process, i.e. patient, primary care
physicians and psychiatrists.
While the patient needs positive encouragement
messages to continue with the treatment, the primary
care physician requires a tool to observe if the
patient is progressing adequately. This tool should
present the information in an intuitive way that does
not require too much time of interpretation. If the
patient does not have a good progress, the primary
care practitioner redirects the patient to the
psychiatric unit. The CM is designed so as to
provide, on the one hand, synthesized visual
information and, on the other hand, relevant and
detailed information of the AM reasoning or analysis
process. The first information is very helpful to the
doctor and the patient, while the second is essential
to facilitate psychiatrist decision making.
Every two weeks the information of the patient is
actualized and a short term analysis of the state of
the patient is performed by the AM. The results of
the analysis are sent to the communication module,
which prepares the appropriate messages and alarms
to the involved actors.
The CM provides four hierarchies of
communication: semaphore, alerts, reports and
alarms. The highest level of the hierarchy, i.e. the
semaphore, is visible for all the actors involved in
the system in each time instant. A green light means
that the patient is progressing adequately saying to
the physicians that no action is needed. A yellow
light represents an alert. This means that the patient
is doing well but that there is the possibility that in
the near future the progress of the patient suffers a
recess. Therefore, the patient should be closely
observed by the virtual assistant and/or the primary
care physician. An example of yellow light could be
when the PEM gives as output that the patient is
improving quickly but a terrible life event, captured
by the Brugha questionnaire, has occurred recently.
In this case the AM concludes that a yellow light is
the adequate alert level and sends this information
plus the reasoning performed by the model to the
CM. Finally a red light represents an alarm. An
alarm means that the patient is not doing well and
that physicians need to take actions, i.e. have a
personal interview with the patient to asses him/her
more deeply, change the medication, increase the
dosage, etc. The format of the following hierarchical
levels, i.e. alerts, reports and alarms are presented as
a set of text messages that explain the reasoning
process carried out by the AM but with different
language, priority and detail depending on the level
and type of the actor to whom is sent. The different
messages to a particular actor can be inhibited or
activated depending on the system requirements
specified by psychiatrists and primary care
physician. Alerts are activated each time the patient
is responding to the questionnaires. Associated to
the light color, the alerts show synthetically
important information that must be present to
interpret the light properly and, are specific to each
actor in the system. Reports explain in an extensive
and detailed way the inference performed by the rule
base system defined in the AM, adapting the set of
messages to each recipient. The reports are available
upon request. Alarms inform of critical states that
require taking specific actions and are transmitted by
means of rapid ways like sms, e-mails, etc.
3.2 App and Website
In this research two platforms have been designed to
allow the interaction with the patients and the
doctors, i.e. an android mobile application (App) and
a Website. The idea is that the actors can use the
platform that is available to them at each time.
The architecture of the interaction between
MADRIM and system actors is synthesized in Fig.
2. Both platforms cooperate with a web server that
has implemented the MADRIM reasoning process
described in Fig 1. The MADRIM App and Website
interact, previous actor identification, with the
patient, the primary care physician or the
psychiatrist. The application is responsible of
capturing the data of the different questionnaires
administered to patients. These data is used by
MADRIM reasoning process as described in the
previous sections and a conclusion of the evolution
of the patient is obtained. This evolution is display
through a graphical semaphore representation and a
set of alerts in the form of messages, to the actors
that has requested it. If required the system sends
also reports and alarms to psychiatrists or primary
care physicians.
Both the App and the Website have an
identification functionality, since each actor has
different functionalities and the interaction with the
MobileAppandWebsiteforMajorDepressionMonitoring
609

Figure 2: Architecture of the interaction between MADRIM and system actors.
system differ from one actor to another. Moreover,
both use a secure shell protocol that allows having
access to patient’s data in a secure manner.
The MADRIM main functionalities available for
each actor are summarized next.
3.2.1 The Patient
There are three main functionalities for the patient in
both platforms (App and Website). The first one
allows the definition of the virtual assistant profile.
The second one allows the patient’s data acquisition,
i.e. presents to the patient the different
questionnaires that should answer. The third
functionality presents the evolution of the patient
graphically and gives the right messages to the
patient at all times.
With respect the virtual assistant profile
functionality, the patient can personalize a specific
profile for his/her virtual assistant, i.e. can choose a
face for the assistant, different colours for the App
or Website and chose between different languages.
With respect patient’s data acquisition, the most
relevant actions involved in this functionality are:
Presentation of the PHQ-9 questionnaire to the
patient in a user-friendly manner every two weeks
and acquisition of the patient responses.
If the patient answered PHQ-9 question #9:
Thoughts that you would be better off dead, or of
hurting yourself, with a value of 3 (maximum
value), then the M.I.N.I. suicidal risk questionnaire
is presented to the patient. Patient responses are
then saved.
The system asks to the patient if he/she has had a
critical event in the last month. If the answer is yes
then the system presents the Brugha questionnaire
to the patient in a user-friendly manner and
acquires his/her responses
Presentation of additional questions to the patient
related to the treatment effects, i.e. is the patient
taking the medication?, has the patient side
effects? are they supportable? Patient responses are
then saved.
There are a number of logistical issues that the
mobile App must manage and resolve to make the
platform dynamic and flexible to the patient’s
timing, when presenting the different questionnaires.
For example, how the mobile App should act
when the patient is not answering the questionnaires
on time? Different action protocols have been
PATIENT
PSYCHIATRIST
PRIMARYCARE
PHYSICIAN
PATIENT
Patient’sEvolution
Display:semaphore
andalerts.Sends
reportsandalarmsif
required.
Webserver
MADRIMAppandWebsite
DataBase
Patient’sData
Acquisition:
PHQ‐9,Brugha,
suicidalrisk,
treatmenteffects
Interne
t
Patient’sData
Patient’sEvolution:
semaphore,alarms,
re
p
ortsandalerts
MADRIM
reasoning
p
rocess
SIMULTECH2013-3rdInternationalConferenceonSimulationandModelingMethodologies,Technologiesand
Applications
610
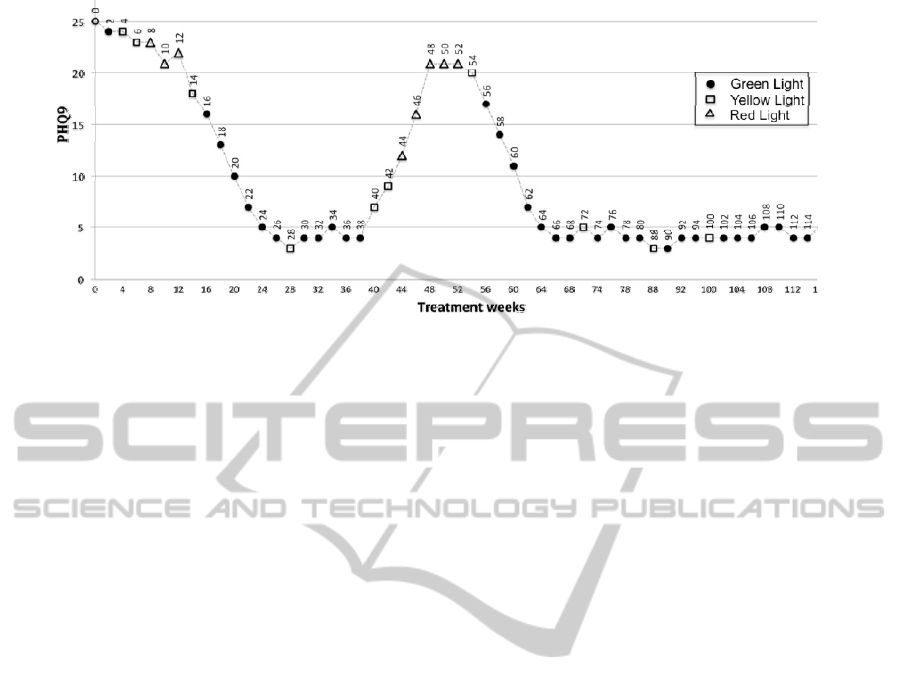
Figure 3: Graphical representation of the evolution of a patient during treatment at home. The symbols represents the
different lights of the semaphore (a black dote corresponds to a green light, a square to a yellow light and a triangle to a red
light), and the numbers near the symbols are the accumulated weeks of treatment.
defined to deal with each of the possible adverse
situations derived from the patient interaction.
For instance, in the case that the patient is not
answering the PHQ9 every two weeks the App
detects that the patient did not respond the
questionnaire the day fifteen and since then, each
day sends a recall SMS message indicating in a
friendly manner that she/he needs to respond the
questionnaire in order that he/she can see graphically
its own evolution and that the doctors can follow
also his/her recovery. Each day the message is a
little different getting less polite day by day. If the
patient does not answer the questionnaire the next
time he/she should respond (i.e. a month has been
passed since the last PHQ-9 data registered), then
the App sends an alarm message to the primary care
physician alerting of a possible reoccurrence of the
depression. The doctor decides if it is necessary to
get in contact with the patient to find out what is
going on. Notice that the Website cannot manage
this kind of situations because cannot get in contact
with the patient if he/she does not decide to enter to
the Website.
With respect the presentation of the patient’s
evolution functionality, the main actions involved
are:
Presentation of the evolution of the patient in a
graphical manner. Fig. 3 shows an example of this
kind of representation. The graph shows the value
of the PHQ-9 questionnaire every two weeks
(when the patient answers the questionnaire). It is
represented by using a semaphore light, i.e. green,
yellow or red, as explained in detail in the
communication module section.
Display messages to the patient. When the patient
positions the cursor over one of the lights of the
graph, the messages associated with the patient's
situation at that moment in time are displayed in
the bottom of the graph. In that way, the patient
can check the messages associated to their
evolution each time he/she answers the
questionnaires and, also, the messages of the past
PHQ-9 values. For example, if the patient is
currently at week 24 and selects the green dot
shown in the graph for this week (see Fig. 3), the
following message is displayed in the bottom of
the graph: Congratulations, depressive state
overcome. Do not leave the medication! If the
patient is now in the week 50 the message that
appears is: Worsening rapidly; Get help, go
immediately to your doctor.
In addition to the previous mentioned messages, the
system sends support citations to the patient
depending on his/her current disease situation. For
example if the patient is progressing adequately but
slowly the following citation is presented: Have
patience with all things, but chiefly have
patience with yourself. Do not lose courage in
considering your own imperfections but
instantly set about remedying them -- every
day begin the task anew.
3.2.2 The Primary Care Physician
and the Psychiatrist
The primary care physicians and the psychiatrist
have available (in both platforms: App and Website)
the evolution of the patient functionality, explained
before.
As in the case of the patients, this functionality
presents graphically (using a semaphore) how is the
patient doing with the treatment. This way the doctor
MobileAppandWebsiteforMajorDepressionMonitoring
611

can analyze the evolution of the patient in a glance.
Specific messages for the doctors are also
displayed at the bottom of the graph. Following the
same example described for the patient in the
previous section, at week 24 the message for the
doctors is: Improves adequately; Remission, whereas
at week 50 the message is: Worsening rapidly;
Relapse. In the last case, a relapse alarm is also sent
to the psychiatrist. In this way the doctor knows that
the patient has had a relapse without accessing the
application MADRIM and can act quickly
accordingly.
4 CONCLUSIONS
Our current research is focused on the development
of an intelligent remote monitor (MADRIM), which
helps physicians in the process of supervision and
gives continuous attention to patients that suffer
from major depression. A monitoring system that
provides complete information of the evolution of
patients in a glance, keeps both patients and
physicians continuously informed and alarm them in
the case of necessity is a valuable contribution when
the goal is to monitor a massive number of major
depression patients.
The research presented in this paper is centered
on the part of this system that interacts with the
actors, which are patients, psychiatrists and primary
care physicians. A mobile App and a Website are
developed and presented in this research. These
tools allow the patient’s data acquisition and the
presentation of the evolution of the patient in a
friendly and intuitive manner. These tools have been
developed paying great attention to the specific
characteristics of patients that suffer from major
depression and analyzing every interaction with
these patients in a very precise way.
REFERENCES
Bratko, I. & Mozina, M. (2004). Argumentation and
Machine learning. Chapter 5 of Theoretical framework for
argumentation, ASPIC project, deliverable D2.1.
Bratko, I., Mozina, M. & Zabkar, J. (2006). Argument-
Based Machine Learning. Lecture Notes in Artificial
Intelligence, 4203, 11-17.
Brugha, T., Bebbington, P., Tennant, C., Hurry, J. (1985).
The List of Threatening Experiences: a subset of 12
live event categories with considerable long-term
contextual threat. Psychological Medicine, 15, 189–
194.
Cuijpers P., Beekman A. F., Reynolds, C. F. (2012).
Preventing depression global priority. JAMA, 307(10),
1033-1034.
Ebmeier, K. P., Donaghey, C., Steele, J. D. (2006). Recent
developments and current controversies in depression,
Lancet, 367(9505), 153-67.
Escobet, A., Nebot, A., Cellier, F. E. (2008). Visual-FIR:
A tool for model identification and prediction of
dynamical complex systems, Simulation Practice and
Theory, 16, 76-92.
Fava, M. (2003). Diagnosis and definition of treatment-
resistant depression. Biological Psychiatry, 53, 649–
659.
Mugica, F., Nebot, A., Bagherpour, S., Serrano-Blanco,
A.,
Baladón, L. (2012). MADRIM: A major
depression remote intelligent monitor. In Proceedings
of the WCCI’12: IEEE World Congress on
Computational Intelligence (FUZZ-IEEE), Brisbane,
10-15 June.
Nierenberg, A. A., Petersen, T. J., Alpert, J. E. (2003).
Prevention of Relapse and Recurrence in Depression:
The Role of Long-Term Pharmacotherapy and
Psychotherapy. J Clin Psychiatry, 64, 13-7
Pinto-Meza, A., Suárez, D., Caseras, X., Haro, J. M.,
Serrano-Blanco, A., Torrubia, R. (2009). Evaluación
telefónica de los sistemas de activación e inhibición
conductual, Revista de psiquiatría y salud mental,
2(2), 66-71.
Sheehan, D. V., Lecrubier, Y., Harnett-Sheehan, K.,
Janavs, J.,Weiller, E., Bonora, L. I., Keskiner, A.,
Schinka, J., Knapp, E., Sheehan, M. F., Dunbar, G. C.
(1997). Reliability and Validity of the MINI
International Neuropsychiatric Interview (MINI):
According to the SCID-P. European Psychiatry, 12,
232-241.
The Macarthur initiative on dperession and primary care
(2013): http://www.depression-primarycare.org/
clinicians/ toolkits/materials/forms/phq9/
Waraich P., Goldner E. M., Somers J. M., Hsu L. (2004).
Prevalence and incidence studies of mood disorder: a
systematic review of the literature. Can J Psychiatry.,
49(2), 124-138.
WHO: Depression (2012). From http://www.who.int/
topics/depression/en/
SIMULTECH2013-3rdInternationalConferenceonSimulationandModelingMethodologies,Technologiesand
Applications
612
