
Comparative Study of Medical-grade and Off-the-Person ECG Systems
Carlos Carreiras
1
, Andr
´
e Lourenc¸o
1,2
, Hugo Pl
´
acido da Silva
1
and Ana Fred
1
1
Instituto de Telecomunicac¸
˜
oes, Av. Rovisco Pais 1, Lisboa, Portugal
2
Instituto Superior de Engenharia de Lisboa, R. Cons. Em
´
ıdio Navarro 1, Lisboa, Portugal
Keywords:
Pervasive Electrocardiology, Off-the-Person ECG Sensor, Morphological Analysis.
Abstract:
Simplified, off-the-person electrocardiogram (ECG) sensor designs enable the introduction into everyday life
of continuous, and pervasive ECG acquisition paradigms. This significantly augments the potential of ap-
plications such as remote health monitoring, emotion assessment, and ECG biometrics, among others. We
accomplish this by reducing the number of contact points to just two, making use of a groundless setting. Ad-
ditionally, acquisition is made at the hand palms or fingers through dry electrodes. In this paper, we describe
such a system, comparing it against a standard 12-lead, medical-grade ECG system. Our analysis is based
on the morphological similarity between individual heartbeat waveforms, as well as the general similarity be-
tween the synchronized time series. We show that the ECG signal acquired at the hands with our sensor is
highly correlated with lead I from the standard system.
1 INTRODUCTION
The measurement and recording of the electrical ac-
tivity of the heart, commonly known as the electro-
cardiogram (ECG), has come a long way since its
introduction at the end of the 19th century. The
first systematic study of the electrical activity of the
human heart was performed by Augustus Waller in
1887 (Besterman and Creese, 1979). He used a Lipp-
mann capillary electrometer to measure the electri-
cal potential between two surface electrodes placed
on the front and back of the chest. This device con-
sisted of a capillary tube partially filled with mercury
and a solution of sulfuric acid. The electrodes were
connected to either side of the tube; when an electric
pulse arrives, the surface tension of the mercury is al-
tered, allowing it to climb up a small distance in the
capillary tube. Weller combined the use of the Lipp-
mann electrometer with a light source, allowing him
to project the oscillations of the mercury in the capil-
lary onto a photographic plate; the plate moved with
the help of a toy train, producing a real-time recording
of the heartbeat.
A few years later, Willem Einthoven used a string
galvanometer to significantly advance the knowledge
about the electrical activity of the heart, naming
the various deflections of the ECG (P, Q, R, S, T,
and later U), standardizing the use of three limb
leads (Einthoven’s Triangle), and correlating numer-
ous electrocardiographic features with cardiovascular
disorders (Barold, 2003). The string galvanometer
consisted of a long conductive filament; when sub-
jected to a strong magnetic field, the fialment oscil-
lates in proportion to the current traveling through it.
This movement is then amplified and projected onto a
moving photographic plate.
Fast forward to the present, the ECG has become a
perfectly established and mainstream technique, pro-
viding vital information for the diagnosis and preven-
tion of a wide array of cardiovascular disorders (Drew
et al., 2004; Chung, 1996). Clinical practice relies
mainly on the widespread short-term (< 1 minute)
12-lead ECG for diagnosis, and, in selected cases,
on Holter monitors (∼ 24 hour assessment). Nev-
ertheless, the outreach of ECG data acquisition and
processing can still be significantly improved upon,
in the context of a pervasive healthcare framework,
with off-the-person ECG sensor designs. The goal
of off-the-person approaches is not to replace exist-
ing data acquisition procedures, but to enhance and
complement current practices with a simplified sen-
sor setup that can be introduced, transparently to the
subject, in multiple aspects of his everyday life. This
enables a more comprehensive assessment of cardio-
vascular function, contributing to the development
of preventive behaviors and methodologies. Also, it
opens the door to many potential applications, such as
continuous monitoring, non-intrusive emotion assess-
115
Carreiras C., Lourenço A., Plácido da Silva H. and Fred A..
Comparative Study of Medical-grade and Off-the-Person ECG Systems.
DOI: 10.5220/0004675501150120
In Proceedings of the International Congress on Cardiovascular Technologies (IWoPE-2013), pages 115-120
ISBN: 978-989-8565-78-5
Copyright
c
2013 SCITEPRESS (Science and Technology Publications, Lda.)
ment (Haag et al., 2004; Medina, 2009) and ECG bio-
metrics (Lourenc¸o et al., 2011; Odinaka et al., 2012),
among others.
In previous work by our team, we have proposed
a simplified, off-the-person ECG sensor design tar-
geted at data acquisition in a pervasive framework
(Silva et al., 2011). In this paper, we compare the
performance of this sensor against a medical-grade
12-lead standard ECG device, assessing the morpho-
logical and structural differences between both sig-
nals. The remainder of this paper is organized as fol-
lows: Section 2 provides an overview of our off-the-
person sensor design, highlighting the main technical
options, and details the acquisition setup; Section 3
describes the signal processing techniques employed,
and the similarity measures used to compare the sig-
nals under study; finally, Section 4 outlines the main
conclusions.
2 EXPERIMENTAL SETUP
With the goal of designing a non-intrusive, pervasive
ECG sensor, we have been focusing our work on min-
imizing the number of electrical contact points with
the subject’s body, and eliminating the need for any
gel or conductive paste in the electrode-skin inter-
face. In this section, we present the general design
guidelines adopted for the development of our off-the-
person sensor, as well as the description of the signal
acquisition setup used for the comparison of our sen-
sor with a medical-grade ECG system.
2.1 Off-the-Person Sensor
Targeting the context of pervasive ECG acquisition,
our sensor design uses only two dry electrodes, be-
ing based on the classical voltage potential differen-
tial principle. In particular, the sensor does not re-
quire the placement of a ground electrode, which is
replaced by a reference voltage produced by the cir-
cuit (commonly known as a virtual ground).
According to the literature (Webster, 2009), typi-
cal physiological ECG signals range from 0.5 to 4 mV
in amplitude, with a spectral content between 0.01
and 250 Hz. These small amplitudes require the use
of high-quality, low-noise instrumentation and oper-
ational amplifiers, with high common-mode rejection
at the input. The global gain of our system is set at
2000. However, given the use of dry electrodes and a
groundless setting, our system is more prone to high-
frequency noise. Therefore, the sensor incorporates a
band-pass filter with a passing band between 0.5 and
40Hz, simultaneously reducing the effect of the low-
frequency respiratory modulation, as well as the pow-
erline and high-frequency noise.
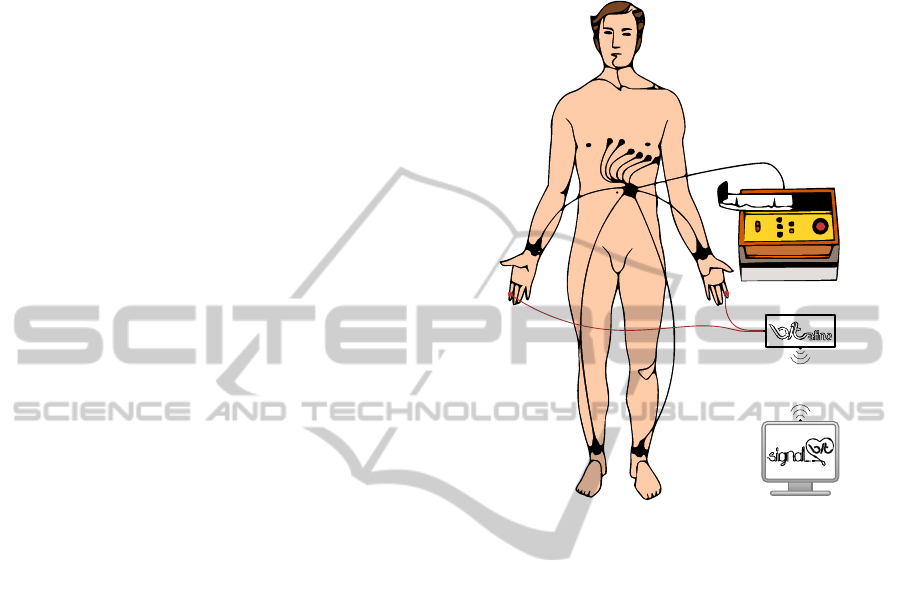
Figure 1: Schematic representation of the classical 12-
lead ECG placement system, along with the placement of
our off-the-person sensor approach, with the dry electrodes
placed at the hands (drawings not to scale).
Figure 1 illustrates the typical 12-lead ECG sys-
tem, as well as the placement of our off-the-person
sensor, using two dry electrodes placed at the hands.
Our ECG sensor is integrated into a broader signal ac-
quisition hardware framework, the BITalino platform
(Guerreiro et al., 2013), which wirelessly transmits
the acquired ECG signal to a computing device. Note
that, although our sensor was specifically designed
for 1-lead measurements at the hand palms or fingers
with virtual ground, it can also be used with a ground
electrode, being capable of emulating any of the bipo-
lar ECG leads (the Einthoven leads: I, II and III).
2.2 Acquisition and Preprocessing
We conducted experimental tests involving 11 vol-
unteers (5 females and 6 males) in which simul-
taneous recordings were performed using a Philips
PageWriter Trim series ECG device (hereinafter re-
ferred to as Philips), and our off-the-person sensor
design (hereinafter referred to as BITalino) with data
acquisition performed using the SignalBIT platform
(Alves et al., 2013). The acquisitions were made on
two sessions, separated by ∼ 1.5 months, but three of
CARDIOTECHNIX2013-InternationalCongressonCardiovascularTechnologies
116
the subjects only partook in one of the sessions (sub-
jects S1, S3 and S6).
The Philips equipment was used in the standard
12-lead configuration (I-III, V1-V6, aVF, aVL, aVR),
as shown in Figure 1, with conductive gel applied to
each of the electrodes, which were placed on the sub-
jects by an experienced technician. It acquires sig-
nal data at 500 Hz, with 16 bit resolution, and storage
is made in a proprietary file format. Our sensor was
used in the virtual ground setting with dry Ag/AgCl
electrodes, and the subjects were told to hold the elec-
trodes at the hands. The BITalino device acquires sig-
nal data at 1000 Hz, with 10 bit resolution, and stor-
age is made in the open StorageBIT file format (Car-
reiras et al., 2013a). Given the fact that the Philips
system records only 10 seconds of data for each run,
we acquired three sequential runs, thus amounting to
30 seconds of data per subject per session.
The main application of our sensor has been to
ECG biometrics (Lourenc¸o et al., 2011; Silva et al.,
2013; Carreiras et al., 2013b), reason for which both
signals were filtered with a Finite Impulse Response
(FIR) bandpass filter with a Hamming window of
300ms, and cutoff frequencies of 5 − 20Hz. These
parameters were determined to be appropriate for this
specific application (Lourenc¸o et al., 2012).
Additionally, for the comparison measures we em-
ploy in this paper, it is necessary to have both signals
with the same sample rate. Therefore, and given the
characteristics of the filter just described, we down-
sampled the BITalino signal by a factor of 2, making
it match the 500 Hz sampling rate of the Philips de-
vice.
3 COMPARATIVE STUDY
We base our comparative study of the BITalino sen-
sor and the Philips system on two major approaches:
morphological and synchronized analyses. While the
first approach focuses on the shape similarity between
individual heartbeat waveforms, the second focuses
on analyzing the correlation between the signals after
a synchronization step, i.e. the correction of the time
delay between the two independent data acquisition
systems.
3.1 Morphological Analysis
In this paper, morphological analysis is understood to
be the comparison of the shape similarity between in-
dividual heartbeat waveforms, as measured by a spec-
ified metric. This requires the use of a QRS detection
algorithm, which enables the segmentation and ex-
traction of the individual heartbeat waveforms from
the ECG time series. For that purpose, we used the
modified Engzee algorithm described in (Lourenc¸o
et al., 2012), which identifies the positions of the R
peaks in the ECG. We then extract the signal seg-
ment corresponding to 200ms before and 400 ms after
each R peak, amounting to a total of 600ms, which
corresponds to the RR interval with a heart rate of
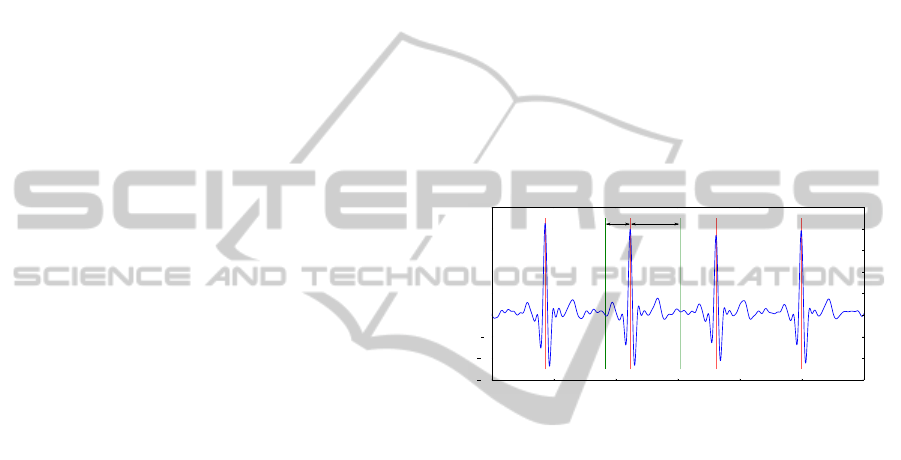
100bpm (see Figure 2). We applied this segmenta-
tion algorithm to the signals from both devices, col-
lecting, from each subject, all the identified heartbeat
waveforms across both sessions. Note that in the case
of the Philips device, segmentation was performed us-
ing the signal from lead I, using it as reference for the
other leads, i.e. the positions of the R peaks found
using lead I were used to extract the individual heart-
beats from the other leads.
10 .0 10 .5 11 .0
11 .5
12 .0 12 .5 13 .0
Tim e (s)
15 0
10 0
50
0
50
10 0
15 0
20 0
25 0
Am p lit u d e
200 ms 400 ms
Figure 2: Example of the segmentation and heartbeat wave-
form extraction procedure; the positions of the R peaks are
plotted in red vertical lines; the limits of one of the heart-
beats are shown in green.
Figure 3 shows the heartbeat waveforms obtained
for one of the subjects, comparing the BITalino heart-
beats with each of the leads from the Philips system.
We can observe that the most visually similar Philips
lead to the BITalino heartbeats is lead I, as intended
by the design of the sensor described in the previous
section, with an almost complete overlap between the
two. It is also possible to distinguish two groups of
heartbeats in the Figure, identifiable, for example, by
looking at the T waves. This is due to the fact that
the Figure shows the heartbeats from both acquisition
sessions, for which the subject happened to have dif-
ferent resting heart rates. As it is known (Simoons
and Hugenholtz, 1975), the heart rate influences the
relative position of the ECG waves, in particular the
T wave.
For the quantitative analysis, given the use of dif-
ferent electrode types and gains between the Philips
and BITalino devices, we adopted the cosine distance
as similarity metric (Equation 1), which is bounded
between 0 and 1, respectively representing complete
similarity (vectors with same orientation) and com-
plete dissimilarity (vectors at π/2).
ComparativeStudyofMedical-gradeandOff-the-PersonECGSystems
117
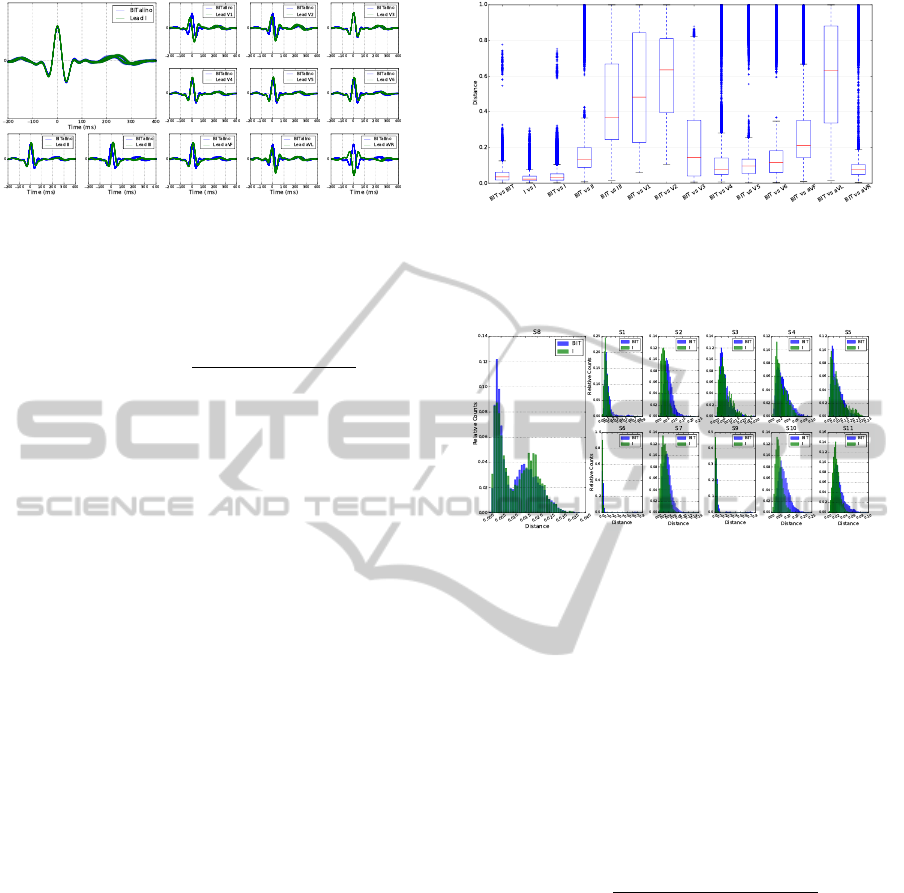
Figure 3: Segmented heartbeat waveforms obtained for sub-
ject S8 with both devices; the BITalino heartbeats are repro-
duced in each plot, comparing them with each of the leads
from the Philips system.
D
cos
(x
i
,x
j
) = 1 −
∑
N
k=1
x
i
[k]x
j
[k]
∑
N
k=1
x
2
i
[k]
∑
N
k=1
x
2
j
[k]
(1)
We use this metric to compare, for each subject,
the distance of the segmented heartbeat waveforms:
a) within the BITalino sensor (BIT vs BIT); b) within
lead I of the Philips system (I vs I); and c) of
the BITalino device against the segmented heartbeat
waveforms of each of the Philips leads (BIT vs X).
Figure 4 shows the boxplots describing the general
distribution characteristics, across all subjects, of the
cosine distances obtained for each of the previously
mentioned items. We can see that the most simi-
lar Philips lead to the BITalino sensor is lead I, as it
presents the lowest median and narrowest Interquar-
tile Range (IQR) of the compared leads. Additionally,
these values are the most similar to the ones obtained
in the BIT vs BIT and the I vs I cases. This reinforces,
with quantitative information, the conclusion drawn
earlier when comparing the heartbeat waveforms of
one of the subjects. Also of note is the fact that the
BIT vs BIT distribution appears to have a wider IQR
when compared to that of the I vs I case, as well as
two distinct groups of outliers. This suggests that the
BITalino sensor is somewhat more sensitive to noise.
To better analyze this question, we also show in Fig-
ure 5 the histograms of these two distributions, for
all subjects. Indeed, the BITalino sensor produces
distributions with higher means, with a slower decay
as the distance increases. In two specific cases (sub-
jects S6 and S9), the BITalino system originates some
heartbeats with high dissimilarity to the others, aris-
ing from the existence of spurious, noisy heartbeats
for these subjects (e.g. resulting from motion arti-
facts). Again, note that the two distribution modes
observable in subject S8 result from different resting
heart rates between the acquisition sessions.
Figure 4: Boxplots, across all subjects, of the cosine dis-
tance of the BITalino heartbeats against the heartbeats of
each of the Philips leads; the whiskers extend to the lowest
and highest data points still within 1.5 times the Interquar-
tile Range; crosses represent outliers.
Figure 5: Histograms, for all subjects, of the cosine dis-
tance between the BITalino heartbeats (BIT), and between
the heartbeats from lead I of the Philips system (I).
3.2 Synchronized Analysis
The synchronized analysis corresponds to the com-
parison of the two ECG sensor systems after the sig-
nals have been aligned in the time domain. We ac-
complish this by first normalizing the DC offset and
amplitude of the signals, as shown in Equation 2,
where the original signal x[k] is subtracted of its mean
µ, and divided by the total amplitude variation.
x
norm
[k] =
x[k] − µ
max
k
{
x[k]
}
− min
k
{
x[k]
}
(2)
We then aligned the signals between corresponding
BITalino and Philips runs by computing the time
delay for which the cross-correlation between them
(Equation 3) is maximum. Note that we use the lead I
from the Philips system to determine the delay, given
that we demonstrated in the previous section that this
derivation is the same as the one used by the BITalino
sensor.
d
∗
= argmax
d∈Z
+∞
∑
k=−∞
x[k] y[k + d] (3)
Figure 6 shows an example of the synchronized
signals for one of the acquisition runs, where we can
observe that there is an almost exact match between
CARDIOTECHNIX2013-InternationalCongressonCardiovascularTechnologies
118
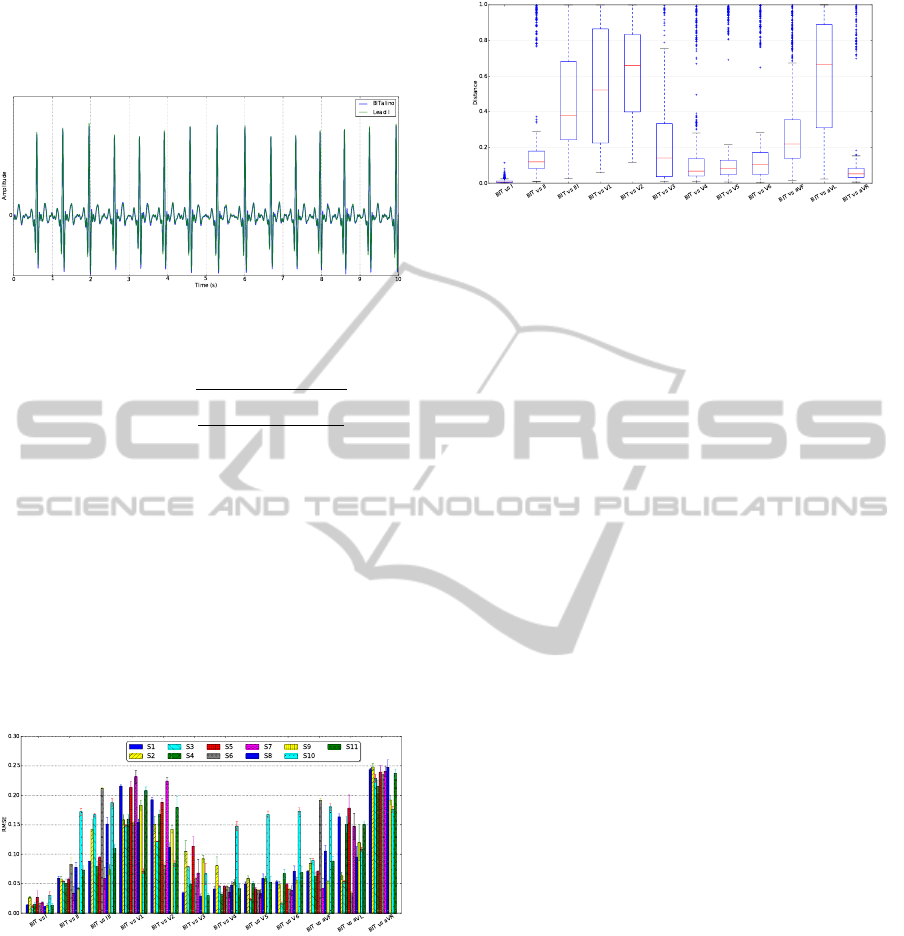
the two signals. This is further validated by comput-
ing the Root Mean Square Error (RMSE), as defined
in Equation 4.
Figure 6: Synchronized BITalino and Philips lead I signals
(subject S8); normalization using Equation 2.
RMSE(x,y) =
s
∑
N
k=1
(x[k] − y[k])
2
N
(4)
Figure 7 shows, for each subject, the averaged
(across all runs) RMSE between the synchronized
BITalino signal and each of the Philips leads. We can
see that the error to lead I is indeed small, although we
lack a reference with which to formulate stronger con-
clusions. It is also interesting to note that subject S10
exhibits a different pattern to that of the other subjects
of the RMSE across the various leads. This arises due
to the subject having a rotation of the heart axis, re-
sulting in different projections onto the typical ECG
derivations.
Figure 7: Root Mean Square Error between the BITalino
and Philips lead I synchronized signals, for all subjects; val-
ues are the averages across all runs.
Finally, we use the cosine distance to compare
the individual heartbeats of the synchronized signals,
computing the distance between each BITalino heart-
beat waveform and the corresponding aligned Philips
heartbeat waveform. We show the results in Figure 8,
where we can observe that the comparison against
lead I exhibits a very small variability, and a median
close to zero. This allows us to conclude that the
BITalino and the Philips lead I signals are highly cor-
related.
Figure 8: Boxplots, across all subjects, of the cosine dis-
tance of the synchronized BITalino heartbeats against the
heartbeats of each of the Philips leads; the whiskers extend
to the lowest and highest data points still within 1.5 times
the Interquartile Range; crosses represent outliers.
4 CONCLUSIONS
In this paper we described a simplified ECG sensor
design targeted at pervasive, off-the-person acquisi-
tion, comparing it with a standard 12-lead, medical-
grade ECG system. Our analysis was based on the
morphological similarities between individual heart-
beat waveforms, and also on the general similarity be-
tween the synchronized time series.
The main conclusion of this paper is that the ECG
signal acquired at the hands with our sensor is most
similar to lead I from the standard system, showing a
high degree of correlation between them. This result
strongly encourages us to further investigate the off-
the-person acquisition paradigm, especially for ECG
biometrics. In this particular case, it is important,
in order to develop a practical system, to have ECG
acquisition setups that are non-intrusive and seam-
lessly integrate into everyday objects. In the future,
we would like to compare the recognition accuracy
of an ECG biometric system using our off-the-person
sensor design, against the standard 12-lead ECG sys-
tem.
ACKNOWLEDGEMENTS
This work was partially funded by Fundac¸
˜
ao para a
Ci
ˆ
encia e Tecnologia (FCT) under grants PTDC/EEI-
SII/2312/2012, SFRH/BD/65248/2009 and SFRH/PR
OTEC/49512/2009, whose support the authors grate-
fully acknowledge.
REFERENCES
Alves, A. P., Silva, H., Lourenc¸o, A., and Fred, A. (2013).
SignalBIT A web-based platform for real-time biosig-
ComparativeStudyofMedical-gradeandOff-the-PersonECGSystems
119

nal visualization and recording. In Proc. of the 10th
SIGMAP.
Barold, S. S. (2003). Willem Einthoven and the birth
of clinical electrocardiography a hundred years ago.
Cardiac electrophysiology review, 7(1):99–104.
Besterman, E. and Creese, R. (1979). Waller–pioneer of
electrocardiography. Brit. Heart J., 42(1):61.
Carreiras, C., da Silva, H. P., Lourenc¸o, A., and Fred, A.
L. N. (2013a). StorageBIT: A Metadata-aware, Exten-
sible, Semantic, and Hierarchical Database for Biosig-
nals. In Proc. of the 6th HEALTHINF.
Carreiras, C., Lourenc¸o, A., Silva, H., and Fred, A. L. N.
(2013b). A Unifying Approach to ECG Biometric
Recognition Using the Wavelet Transform. In Proc.
of the 10th ICIAR.
Chung, E. K. (1996). Pocket guide to ECG diagnosis.
Blackwell Science.
Drew, B. J., Califf, R. M., Funk, M., Kaufman, E. S., Kru-
coff, M. W., Laks, M. M., Macfarlane, P. W., Sommar-
gren, C., Swiryn, S., and Van Hare, G. F. (2004). Prac-
tice standards for electrocardiographic monitoring in
hospital settings. Circulation, 110(17):2721–2746.
Guerreiro, J., Martins, R., Silva, H., Lourenc¸o, A., and Fred,
A. L. N. (2013). BITalino: A Multimodal Platform
for Physiological Computing. In Proc. of the 10th
ICINCO.
Haag, A., Goronzy, S., Schaich, P., and Williams, J. (2004).
Emotion recognition using bio-sensors: First steps to-
wards an automatic system. In Aff. Dial. Syst., pages
36–48. Springer.
Lourenc¸o, A., Silva, H., and Fred, A. (2011). Unveiling
the biometric potential of Finger-Based ECG signals.
Computational Intelligence and Neuroscience, 2011.
Lourenc¸o, A., Silva, H., Leite, P., Lourenc¸o, R., and Fred,
A. (2012). Real time electrocardiogram segmentation
for finger based ECG biometric. In Proc. of the 5th
BIOSIGNALS, pages 49–54.
Lourenc¸o, A., Silva, H., and Fred, A. L. N. (2012). ECG-
based biometrics: A real time classification approach.
In Proc. of the IEEE MLSP Workshop.
Medina, L. (2009). Identification of stress states from ECG
signals using unsupervised learning methods. Mas-
ter’s thesis, Universidade T
´
ecnica de Lisboa, Instituto
Superior T
´
ecnico.
Odinaka, I., Lai, P.-H., Kaplan, A., O’Sullivan, J., Sirevaag,
E., and Rohrbaugh, J. (2012). ECG biometric recogni-
tion: A comparative analysis. IEEE Trans. Inf. Foren-
sics Security, 7(6):1812 –1824.
Silva, H., Lourenc¸o, A., Lourenc¸o, R., Leite, P., Coutinho,
D., and Fred, A. (2011). Study and evaluation of a sin-
gle differential sensor design based on electro-textile
electrodes for ECG biometrics applications. In Proc.
IEEE Sensors Conf.
Silva, H., Lourenc¸o, A., Canento, F., and Fred, A. (2013).
ECG Biometrics: Principles and Applications. In
Proc. of the 6th BIOSIGNALS.
Simoons, M. and Hugenholtz, P. (1975). Gradual changes
of ECG waveform during and after exercise in normal
subjects. Circulation, 52(4):570–577.
Webster, J. G. (2009). Medical Instrumentation Application
and Design. Wiley, 4th edition.
CARDIOTECHNIX2013-InternationalCongressonCardiovascularTechnologies
120
