
An Ontological Map for Meaningful Use of Healthcare Information
Systems (MUHIS)
Arkalgud Ramaprasad
1, 2
, Thant Syn
1
and Mohanraj Thirumalai
2
1
School of Business Administration, University of Miami, 5250 University Drive, Coral Gables, FL, U.S.A.
2
College of Business Administration, University of Illinois at Chicago, 601 S Morgan Street, Chicago, IL, U.S.A.
Keywords: Ontology, Meaningful Use, Healthcare Information Systems, Electronic Health Records.
Abstract: An ontological map of meaningful use of healthcare information systems (MUHIS) is the visualization of its
requirements and practices using an ontology. We map (a) the Stages 1and 2 meaningful use requirements
set by the Centers for Medicaid & Medicare Services (CMS) for Electronic Health Records (EHR), and (b)
the current literature on meaningful use, to derive the ontological map of the requirements and practices
respectively. The map is fragmented and incomplete. The results will focus attention on the gaps (a) in the
requirements, (b) in practices, and (c) between requirements and practices, and highlight the bright, light,
blank, and blind spots in MUHIS. These gaps should be (a) bridged if they are important, (b) ignored if they
are unimportant, or (c) reconsidered if they have been overlooked. Feedback based on incremental
ontological maps over time will help to continuously improve MUHIS.
1 INTRODUCTION
Meaningful Use of Healthcare Information Systems
(MUHIS) is a work-in-progress at the national level
in the USA and other countries(Dermer and Morgan,
2010, Ke et al., 2012, Kim and Kim, 2012, Varroud-
Vial, 2011), at the local level in many states and
cities, and at the enterprise level in many hospitals,
physician practices, and other healthcare providers.
Its requirements and practices are evolving in
tandem, and along different paths depending on the
initial conditions, incentives, and the environment. It
is seen as an instrument for addressing the national
(USA, for example) concerns about the cost, quality,
and safety of healthcare. Consequently, there is a
constant pressure to continuously and rapidly
improve MUHIS. To catalyze the evolution, the
Centers for Medicaid & Medicare Services (CMS) in
the USA has set Stages 1 and 2 meaningful use
requirements for Electronic Health Records (EHR)
(Centers for Medicare & Medicaid Services). The
requirements specify the outcomes, associated
objectives, and corresponding measures. There are
incentives for meeting the objectives. Fulfilling the
requirements will be necessary but not sufficient for
harnessing the full potential of MUHIS; it has far
greater potential than envisioned in the present
requirements. The requirements and MUHIS have to
evolve quickly in tandem to meet the rapidly
increasing global demands on healthcare. It would
be a challenge to make the MUHIS ‘elephant’ dance.
MUHIS is a large, complex, and ill-structured
problem. It is a ‘wicked’ problem (Churchman,
1967). We have to manage its ‘wickedness’ through
feedback and learning to help it evolve rapidly. To
do so, we have to (a) abstract from the diverse, often
contradictory, and heterogeneous requirements and
practices of MUHIS, and (b) apply it to the
reformulation of requirements and practices
(Ramaprasad, 1979, Ramaprasad, 1983,
Ramaprasad, 1987). We need a clear framework
and method for abstraction and application
(Ramaprasad, 1987, Ramaprasad and Mitroff, 1984)
to avoid replaying the proverbial story of the five
blind men each of whom imagined an elephant as a
rock, an arrow, a fan, a rope, and a tree trunk after
touching its body, tusk, ear, tail, and leg,
respectively (Börner et al., 2003, Ramaprasad et al.,
2009). A wise man settles their argument about the
ontic nature of the elephant by piecing together the
picture for them. Fortuitously, the wise man in the
story could see and recognize the elephant; without
him the blind men’s argument would likely have
continued ad infinitum. Analogously we need wise
men and women who can see and recognize the ‘big
16
Ramaprasad A., Syn T. and Thirumalai M..
An Ontological Map for Meaningful Use of Healthcare Information Systems (MUHIS).
DOI: 10.5220/0004734500160026
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2014), pages 16-26
ISBN: 978-989-758-010-9
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

picture’ of MUHIS. The framework should guide the
abstraction, inform the application, and structure the
visualization of the MUHIS. It should thus help (a)
to limit the fragmentation of the requirements and
practices, (b) to make the system greater than the
sum of its parts, and (c) to evolve MUHIS
systemically and systematically. The framework
itself should be adaptable to the evolution of
requirements and practices through scaling,
extension, reduction, refinement, and magnification
of its components.
In the following, we will present an ontology
(Ramaprasad et al., 2009) for MUHIS and discuss a
method of mapping it using the framework. Thus,
we will present a map of the “knowledge structure”
(Zhang et al., 2012) of requirements and practices of
MUHIS as an ontological map. The ontological map
represents a “virtual knowledge
landscape” (Scharnhorst, 2001, p. 505) based on
textual empirical data about the requirements and
practices. It will help visually recognize the
coherence and lack of it in the cumulative domain
knowledge, and therefore help correct the lacuna
when appropriate (Hoeffner and Smiraglia, 2013,
Noar and Zimmerman, 2005). Thus, it will provide
“support for navigating the knowledge
landscape.” (Kazimierczak et al., 2012, p. 1) Further,
“[i]ncrementally computed information landscapes
are an effective means to visualize longitudinal
changes in large document repositories…" (Syed et
al., 2012, p. 352) such as the requirements and
practices of MUHIS. It will aid the continuous
improvement of MUHIS.
First, we will describe an ontology of MUHIS.
We will explain the conceptual foundations of the
framework and its bases in MUHIS requirements
and practice. We will also discuss the face, content
(Brennan et al., 2011), semantic (Kotis and Vouros,
2006), and systemic validity (Horn and Lee, 1989)
of the framework.
Second, we will describe the method for
mapping the requirements specifications and
practice literature onto the ontology and explain the
mapping process. We will discuss the reliability and
validity of the mapping. We will demonstrate the
visualization of the ontological map from the
mapped data based on the map.
Third, we will describe the gaps within
requirements, within practice, and between
requirements and practice using the ontological map.
We will discuss the importance of these gaps and
their implications for future requirements
specifications and practice.
Fourth, and last, we will describe how the
method can be used to develop incremental maps
(Syed et al., 2012) over time to generate feedback
and facilitate learning in the evolution of MUHIS.
We expect that continuous assessment and
improvement of MUHIS using the proposed method
will eventually lead to the realization of the guiding
vision.
2 ONTOLOGY OF MUHIS
Ontologies “… provide a shared and common
understanding of a domain that can be
communicated between people and heterogeneous
and widely spread application systems.” (Fensel,
2003, p.1) They “… make it possible to understand,
analyze, exchange or share knowledge of a specific
domain and therefore they are becoming popular in
various communities. However, ontologies can be
very complex and therefore visualizations can
support users to understand the ontology easier.
Moreover, graphical representations make
ontologies with their structure more manageable. For
an effective visualization, it is necessary to consider
the domain for which the ontology is developed and
its users with their needs and expectations.”
(Kriglstein and Wallner, 2013, p. 123)
Ontology is the study of being in contrast to
epistemology which is the study of knowing. Its
focus is on objects, their categories, and the
relationships between them. Ontologies represent the
conceptualization of a domain (Gruber, 2008); they
organize the terminologies and taxonomies of a
domain. An ontology is an “explicit specification of
a conceptualization.” (Gruber, 1995, p. 908) It is
used to systematize the description of a complex
system (Cimino, 2006). “Our acceptance of an
ontology is… similar in principle to our acceptance
of a scientific theory, say a system of physics; we
adopt, at least insofar as we are reasonable, the
simplest conceptual scheme into which the
disordered fragments of raw experience can be fitted
and arranged.” (Quine, 1961, p. 16)
There are potentially many ways of representing
a domain ranging from a natural-language narrative
to a formal mathematical formulation (when
possible). The ontology is a structured natural-
language representation, more formal than a
narrative but less formal than a mathematical
formulation. It is particularly suited for ‘wicked’
problems such as MUHIS. It is easy to understand
and apply the ontology.
The ontology for MUHIS is shown in Figure 1.
It encapsulates the logic of MUHIS. It has been
AnOntologicalMapforMeaningfulUseofHealthcareInformationSystems(MUHIS)
17

Figure 1: Ontology for Meaningful Use of Healthcare Information Systems (MUHIS).
formulated manually by the authors from the
meaningful use outcomes, objectives, and measures
(Centers for Medicare & Medicaid Services) and
their knowledge of the structure and functions of an
information systems. There is no computerized
method for extracting such an ontology (a) at this
level of granularity, (b) which is parsimonious (fits a
letter size page with legible font), and (c) has high
semantic validity (Kotis and Vouros, 2006) (each
combination is a natural English sentence as
explained below). During the formulation two of the
authors iterated between abstraction of the
framework from and its application(Ramaprasad and
Mitroff, 1984) to the requirements until the model
(a) was logically complete, and (b) covered all the
objectives, requirements, and criteria. It is similar to
the process described by Ramaprasad & Mitroff
(1984) and Ramaprasad (1987) for the formulation
of strategic problems.
The ontology has five columns representing the
five dimensions of MUHIS; two of the dimensions
together comprise the Health Information Systems.
Each dimension is defined by a one- or two-level
taxonomy. The dimensions are linked by
words/phrases interleaved between the respective
columns. The columns are ordered left to right such
that the concatenation of a word from each column
with the interleaved words/phrases results in a
meaningful natural English sentence. Four such
concatenated sentences are shown, with examples, at
the bottom of Figure 1. In the following we will
discuss the dimensions, the taxonomies, and the
concatenations in greater detail.
Management Structure Function Stakeholders Outcome
Analysis [of] Technology [for] Acquisition Recipients Efficiency
Specification Hardware Analysis Patients Quality
Design Software Interpretation Families Safety
Implementation Networks Application Population Disparities
Maintenance Processes Distribution Providers
Assessment Policies Physicians
Personnel Nurses
Pharmacists
Payers
Employers
Insurers
Regulators
Government
Examples:dataminingspecialists
HealthcareInformationSystems
[ofinformationby/to]
[tomeaningfullymanage]
1.Specificationoftechnologyforanalysisofinformationbyproviderstomeaningfullymanage
costofhealthcare.
Examples:electronichealthrecordssoftware,dataminingsoftware
2.Designofprocessesforacquisitionofinformationbypatientstomeaningfullymanagequalityof
healthcare.
FourIllustrativecomponentsofmeaningfuluseofHISfrom3360(6x4x5x7x4)level‐
1components:
Examples:accesstoonlinelabresults,formationofsocialnetworks
3.Implementationofpoliciesforapplicationofinformationbygovernmenttomeaningfully
managedisparitiesinhealthcare.
Examples:wellnesseducationpolicies,Medicaidreimbursementpolicies
[of/inhealthcare]
4.Implementation(deployment)ofpersonnelforinterpretationofinformationbyinsurersto
meaningfullymanagesafetyofhealthcare.
HEALTHINF2014-InternationalConferenceonHealthInformatics
18

2.1 Dimensions of the Ontology
The rightmost column is ‘Outcome’ and it lists the
four critical healthcare outcomes which need to be
meaningfully managed using HIS. They are
efficiency, quality, and safety of healthcare and
disparities in healthcare – a Core and Menu Set
outcome (Centers for Medicare & Medicaid
Services). There are many other Core and Menu Set
outcomes. We interpret them as means to the four
outcomes in the ontology. For example, consider the
Core outcome to ‘Engage patients and families in
their healthcare’. In the ontology patients and
families are stakeholders in achieving the desired
healthcare outcomes using the Health Information
System. Similarly, consider the Menu Set outcome
to ‘Improve population and public health’ – the
Population is a stakeholder receiving healthcare to
achieve the desired outcomes. We have been able to
relate all the present Stages 1 and 2 outcomes to the
four outcomes. In the future, additional outcomes or
subcategories of outcomes can be added, or some of
the outcomes deleted for application to a particular
context.
The second column from the right (Stakeholders)
is a taxonomy of stakeholders in HIS. They are the
recipients of healthcare (patients, families, and the
population as a whole), the providers of healthcare
(physicians, nurses, and pharmacists), payers for
healthcare, employers of recipients, insurers of
recipients, regulators of healthcare, and the
government. The categories of stakeholders are not
mutually exclusive – an entity may have multiple
roles. For example, a recipient may also be a payer,
and a self-insured employer may also be the insurer.
The categories may not also be exhaustive – they
may need to be extended or reduced. The present
taxonomy is a generic, parsimonious list of
stakeholders whose interests and roles in
meaningfully managing the healthcare outcomes
need to be considered.
The third and fourth columns (Structure,
Function) from the right are the common structural
and functional components of an information
system. They have been adapted to the CMS
terminology (Centers for Medicare & Medicaid
Services). The structural components of HIS are the
technology (hardware, software, and networks),
processes, policies, and personnel. The functional
components are acquisition, analysis, interpretation,
application, and distribution of information.
The leftmost column (Management) lists the
functions necessary to manage HIS to assure their
meaningful use. These are common functions in the
analysis, design, and assessment of any information
system. They are analysis, specification, design,
implementation, maintenance, and assessment; they
have been derived from the HealthIT terminology
(HealthIT.gov).
2.2 Illustrative Components
Each concatenation of words/phrases across the
framework is a potential component of MUHIS.
There are 3360 (6x4x5x7x4) level-1 and 7920
(6x6x5x11x4) level-2 components. We will focus
our discussion on the level-1 components and
subsume within them the details of the second level.
Four level-1 components are listed at the bottom of
Figure 1 with an example for each; they are
discussed below.
First, consider ‘Specification of technology for
analysis of information by providers to meaningfully
manage cost of healthcare.’ This could include
specification of cost-effective electronic health
records software to provide the type of clinical
decision support required by CMS for meaningful
use. It could also include data mining software to be
used by a large regional Health Maintenance
Organization (HMO) to determine the most
efficacious drugs for a commonly occurring chronic
condition.
Second, consider ‘Design of processes for
acquisition of information by patients to
meaningfully manage quality of healthcare.’ It could
include design of processes for online access of lab
results (required by CMS in Stages 1 and 2), or
processes to foster formation of social networks of
cancer patients to acquire information from each
other and form support groups.
Third, consider ‘Implementation of policies for
application of information by government to
meaningfully manage disparities in healthcare.’ It
could include policies to transmit health data to
government agencies, wellness education policies
for those living in the ‘food deserts’, and
reimbursement policies which help counter the
imbalance due to socio-economic status.
Fourth, and last, consider ‘Implementation
(deployment) of personnel for interpretation of
information by insurers to meaningfully manage
safety of healthcare.’ It could entail deployment of
data mining specialists to discover early warnings
about new potentially unsafe drugs.
Further, as shown in the examples, each
component may be instantiated in multiple ways.
The many instantiations constitute the MUHIS. We
note that some components may not be instantiated
AnOntologicalMapforMeaningfulUseofHealthcareInformationSystems(MUHIS)
19

at all in a given context. For example, without health
insurance the fourth illustrative component above
may be irrelevant. In general, the absence of
instantiation may reflect either an error of omission
(blind spot) or an irrelevant component (blank spot)
in that context.
2.3 Validity of the Ontology
In assessing the validity of the framework we note
that it is an ontology not the ontology for MUHIS;
we recognize that there can be other equally valid
frameworks. Each framework can be a lens to study
the domain; each lens can offer different insights
about the domain. Given that the MUHIS problem is
complex and ill-structured, ‘wicked’ (Churchman,
1967), a singular ontology is unlikely. We offer a
framework and its associated insights. It derives its
validity from its (a) logical construction, (b)
comprehensiveness, (c) interpretability, and (d)
completeness.
First, the logic of the MUHIS ontology’s
dimensions can be deconstructed as follows:
Meaningful Use of Healthcare Information
Systems = Meaningful Use + Healthcare
Information Systems
Meaningful Use = Management +
Stakeholders + Outcome
Healthcare Information Systems = Structure
+ Function
Thus, the dimensions comprehensively cover the
connotation of MUHIS. They can be easily
interpreted by a user.
Second, the categories of the taxonomy for each
dimension are logical and generally accepted in the
respective disciplines. Moreover, should a category
or subcategory be missing from a taxonomy, it can
be easily added. By the same token, a redundant
category or subcategory can be easily removed.
These corrections of potential errors of omission and
commission will not invalidate the rest of the
framework. Thus, the taxonomies of the dimensions
are comprehensive and interpretable.
Third, the ordering of the dimensions fits the
rules of English grammar – thus rendering the
concatenations in natural English and making them
meaningful and hence interpretable. Further, all the
components (concatenations) encapsulated in the
framework taken together provide a complete,
closed description of MUHIS.
Fourth, and last, the parsimonious representation
of the ontology provides a panoptic view of MUHIS
which can be analyzed with minimal cognitive
strain. A user can conveniently and meaningfully
explore its dimensions, elements, and components at
different levels of granularity.
Thus, we believe that the framework’s face
validity (Brennan et al., 2011), content validity
(Brennan et al., 2011), systemic validity (Horn and
Lee, 1989), and semantic validity (Kotis and
Vouros, 2006) are high. It parsimoniously
encapsulates the complexities of the system; it
makes the MUHIS ‘elephant’ known and visible and
hence can be used to map MUHIS systemically and
systematically. It is a simple, powerful tool to
synthesize and visualize the MUHIS knowledge
domain, to analyze the accumulation of knowledge
over time, and visualize its trajectory. It provides a
holistic approach to visualize the map and guide the
progress of a domain, for example, to answer the
question: How can we continuously improve
MUHIS? We explore these possibilities in the
following.
3 METHOD
3.1 Mapping MUHIS Requirements
We mapped all the Stages 1 and 2 requirements onto
the ontology through consensus mapping. The
requirements were obtained from the CMS website
(Centers for Medicare & Medicaid Services). Each
objective was mapped individually, considering it in
the context of the associated outcome and measures.
The total number of objectives mapped = 51. All the
objectives were first mapped by one author,
reviewed and modified by the other, and the
discrepancies between the two discussed and
resolved in the final mapping. The mapping does not
distinguish between the core and menu objectives,
and those for eligible professionals, eligible
hospitals, and CAHs (Critical Access Hospitals). We
provide two examples of mapping in the following.
Consider the Stage 1 core objective of
“Implement drug-drug and drug-allergy interaction
checks.” It is one of a set of objectives with the
stated outcome of “Improving quality, safety,
efficiency, and reducing health disparities.” We
mapped the objective for quality, safety, and
efficiency outcomes but not for disparities; we could
not see a direct link from the discussion of the
objective and its measures to managing disparities.
We mapped it to the ontology as: “Implementation
of technology/processes for application of
information by providers to meaningfully manage
efficiency/quality/safety.” We note that the objective
HEALTHINF2014-InternationalConferenceonHealthInformatics
20
corresponds to six components of the ontology, not
just one.
Consider the Stage 2 core objective of “Provide
patients the ability to view online, download and
transmit their health information within four
business days of the information being available to
the EP.” Although the stated outcome of the
objective is “Patient Electronic Access”, we inferred
the ultimate outcome to be primarily quality. It could
be efficiency and safety too, but we did not find
sufficient evidence to justify them. We mapped the
objective to the ontology as: “Implementation of
technology for distribution of information by/to
recipients/providers to meaningfully manage
quality.” Again, we note that the objective
corresponds to two components of the ontology.
Mapping the meaningful use objectives was
straightforward in most cases. It required little
interpretation except in the mapping the outcomes of
a few objectives as illustrated above. The mapping
was recorded on an Excel spreadsheet using one row
per objective and a column per element of the
ontology. All but 2 of the 51 objectives were
mapped to all the five dimensions of the framework
for a total of 65 full and 10 partial components.
3.2 Mapping MUHIS Practice
We mapped all the articles indexed in PubMed that
contain the term "Meaningful Use" in the
title/abstract and belong to the following MeSH
major topics: "Medical Informatics", "Medical
Records Systems, Computerized", "Electronic
Prescribing", and "Computer Communication
Networks". In addition, we also included articles
specifically designated to MeSH major topic
"Meaningful Use". The combined result was filtered
by date (2009 – March 1, 2013) as well as the
availability of abstract. We obtained a total of 200
articles. Of these, 43 were announcements,
editorials, etc. and 7 were non-US. They were
excluded from the study. The remaining 150 articles
were mapped by the authors onto the ontology based
on their titles and abstracts. Each article was mapped
by one author and validated by the other.
Differences in mapping between the two were
resolved through discussion. As with the
requirements an article could be coded (a) on all or
some of the dimensions, and (b) into a single or
multiple components of the framework. Of the 150
articles, 63 were coded on all the dimensions and 87
on a subset, for a total of 214 components and 1964
partial components. All the data were maintained
and mapped on spreadsheets (Google Docs and
Excel).
4 RESULTS
4.1 Ontological Map of MUHIS
Requirements
The ontological map of MUHIS requirements is
shown in Figure 2. The elements correspond to the
first level of the ontology. The number in
parenthesis adjacent to each element is the frequency
Figure 2: Ontological map of Stages 1 and 2 meaningful use requirements.
4
Management Structure Function Stakeholders Outcome
Analysis (0) Technology (49) Acquisition (21) Recipients (22) Efficiency (39)
Specification (0) Processes (44) Analysis (0) Providers (51) Quality (44)
Design (0) Policies (10) Interpretation (0) Payers (0) Safety (28)
Implementation (44) Personnel (0) Application (9) Employers (0) Disparities (9)
Maintenance (7) Distribution (28) Insurers (0)
Assessment (0) Regulators (0)
Government (7)
Healthcare Information System
[of]
[for]
[of information by/to]
[to meaningfully manage]
[of healthcare]
AnOntologicalMapforMeaningfulUseofHealthcareInformationSystems(MUHIS)
21
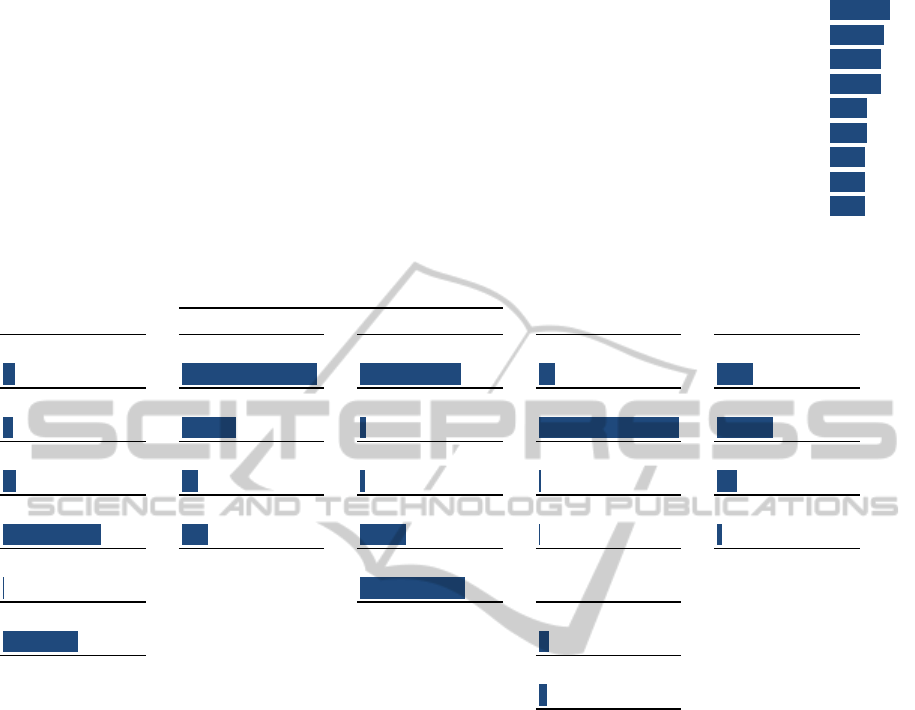
Figure 3: Partial histogram of Stages 1 and 2 meaningful use requirements.
Figure 4: Ontological map of meaningful use practice.
of its occurrence in the set of objectives. The bar
below the element is proportional to the frequency
using the total number of objectives (51) as the
denominator. The profile is very similar for Stages 1
and 2 requirements and hence they are not shown
separately. The total frequency for elements in a
column may exceed the total number of CMS
objectives due to one to many mapping of objectives
to components as illustrated and explained earlier.
The mosaic of the MUHIS requirements as a
whole is evident from the ontological map. It has
many bright spots (high frequency elements), light
spots (low frequency elements), and blank/blind
spots (no frequency elements). The no frequency
elements may be ‘blank’ by choice or ‘blind’ by
oversight – it cannot be resolved based on the data.
The mosaic may be summarized in a complex
sentence with higher frequency elements in bold and
decreasing frequency left to right as follows:
Implementation/ maintenance of
technology/ processes/ policies for
distribution/ acquisition/ application of
information by/to providers/recipients/
government to meaningfully manage
quality/efficiency/safety/disparities of
healthcare.
The partial histogram of Stages 1 and 2
meaningful use requirements shown in Figure 3
highlights the most common components of the
requirements using the structured construction of the
ontology – the bright spots. On the left is the
synthetic requirement based on the ontology, and on
the right the total frequency of its occurrence and a
proportional bar. As we have noted earlier, a CMS
requirement may be deconstructed into multiple
synthetic requirements. The full histogram (not
shown due to space constraint) portrays the bright,
light, and blank/blind spots at the component level,
in contrast to the element level visualization in the
ontological map.
Implementation of Technology for Distribution of information by/to Providers to meaningfully manage Quality of/in healthcare 19
Implementation of Processes for Distribution of information by/to Providers to meaningfully manage Quality of/in healthcare 17
Implementation of Technology for Distribution of information by/to Providers to meaningfully manage Efficiency of/in healthcare 16
Implementation of Processes for Distribution of information by/to Providers to meaningfully manage Efficiency of/in healthcare 16
Implementation of Technology for Acquisition of information by/to Providers to meaningfully manage Efficiency of/in healthcare 12
Implementation of Technology for Acquisition of information by/to Providers to meaningfully manage Quality of/in healthcare 12
Implementation of Technology for Distribution of information by/to Providers to meaningfully manage Safety of/in healthcare 11
Implementation of Processes for Acquisition of information by/to Providers to meaningfully manage Efficiency of/in healthcare 11
Implementation of Processes for Acquisition of information by/to Providers to meaningfully manage Quality of/in healthcare 11
Management Structure Function Stakeholders Outcome
Analysis (10) Technology (119) Acquisition (89) Recipients (15) Efficiency (32)
Specification (9) Processes (49) Analysis (6) Providers (124) Quality (50)
Design (11) Policies (15) Interpretation (5) Payers (2) Safety (18)
Implementation (87) Personnel (24) Application (41) Employers (1) Disparities (5)
Maintenance (1) Distribution (92) Insurers (0)
Assessment (66) Regulators (9)
Government (8)
[of]
[for]
[of information by/to]
[to meaningfully manage]
Healthcare Information Systems
[of/in healthcare]
HEALTHINF2014-InternationalConferenceonHealthInformatics
22

Figure 5: Partial histogram of meaningful use practice.
4.2 Ontological Map of MUHIS
Practice
The ontological map of MUHIS practice mirrors that
of the requirements, as one would expect, but with
the following significant exceptions: (a) in
Management there is a greater emphasis on
Assessment and virtually no emphasis on
Maintenance in practice; (b) in Structure, there is
less emphasis on Processes and slightly more
emphasis on Personnel in practice; and (c) among
Stake holders there is less emphasis on Recipients in
practice. The Function and the Outcome profiles of
the requirements and practice are similar.
The mosaic of the MUHIS practice as a whole is
evident from the ontological map. As with the map
of requirements it has many bright spots, light spots,
and blank/blind spots. The mosaic may be
summarized in a complex sentence with higher
frequency elements in bold and decreasing
frequency left to right as follows:
Implementation/ assessment/ design/
analysis/ specification/ maintenance of
technology/ processes/ personnel/ policies
for distribution/ acquisition/ application/
analysis/ interpretation of information by/to
providers/ recipients/ government/
regulators/ payers/ insurers to meaningfully
manage quality/efficiency/safety/disparities
of healthcare.
The partial histogram of meaningful use practice
shown in Figure 5 highlights the bright spots using
the synthetic components of the ontology. Its
construction is similar to Figure 3.
5 DISCUSSION
Words matter. The formulation of a problem can be
inclusive or restrictive, depending on the choice of
words and their connotations. We have formulated
meaningful use inclusively in the MUHIS ontology
(Figure 1). The Management dimension includes all
the major steps of a system development cycle; the
primary components of the Structure and Function
of a Health Information System are incorporated;
and so are all the key Stakeholders and Outcomes.
Meaningful use should be ‘meaningful’ for all the
stakeholders for all the key ‘uses’ (outcomes). The
inclusive formulation makes the MUHIS ‘elephant’
fully visible – doing so can diminish the costs of
fragmentation and drive the benefits of integration.
CMS has formulated meaningful use narrowly in
its Stages 1 and 2 requirements, as shown in the
ontological map in Figure 2. The narrow formulation
may be driven by its mission – their primary site for
MUHIS is ‘HealthIT.gov’ not ‘HealthIS.gov’,
emphasizing technology not the system. It may be
motivated by the strategy for implementation – to
start where there may be greatest leverage and to
proceed in stages. It may also be determined by their
decisions about their role. They may see motivating
recipients and providers as their role but not
motivating payers and employers. Similarly, they
may see motivating implementation as part of their
role but not analysis, specification, and design – the
latter could be the EMR vendors’ role. Last, the
similarity of Stages 1 and 2 maps suggest a
continuity of focus. We cannot adduce the reasons
for the map shown in Figure 2 and its continuity but
we can assert that the Stages 1 and 2 requirements
by themselves are unlikely to result in MUHIS in its
panoptic connotation expressed in the ontology. The
narrow formulation is likely to be suboptimal if not
dysfunctional.
Consider the Stage 1 objective: ‘Implement drug-
drug and drug-allergy interaction checks’. These
checks will directly affect the Quality and Safety
(Crosson et al., 2012, Rahmner et al., 2012, Spina et
al., 2011) Outcomes of healthcare (Classen et al.,
2011). Their effectiveness will depend upon the
providers’ response to the alerts issued based on the
Assessment of Technology for Acquisition of information by/to Providers to meaningfully manage Quality of/in healthcare 20
Assessment of Technology for Distribution of information by/to Providers to meaningfully manage Quality of/in healthcare 20
Implementation of Technology for Distribution of information by/to Providers to meaningfully manage Quality of/in healthcare 20
Implementation of Technology for Acquisition of information by/to Providers to meaningfully manage Quality of/in healthcare 18
Implementation of Technology for Distribution of information by/to Providers to meaningfully manage Efficiency of/in healthcare 18
Implementation of Technology for Acquisition of information by/to Providers to meaningfully manage Efficiency of/in healthcare 17
Implementation of Technology for Acquisition of information by/to Providers to meaningfully manage Safety of/in healthcare 14
Implementation of Technology for Distribution of information by/to Providers to meaningfully manage Safety of/in healthcare 14
Assessment of Technology for Acquisition of information by/to Providers to meaningfully manage Efficiency of/in healthcare 13
Assessment of Technology for Distribution of information by/to Providers to meaningfully manage Efficiency of/in healthcare 13
AnOntologicalMapforMeaningfulUseofHealthcareInformationSystems(MUHIS)
23

checks. Recent Assessment shows that more than
90% of the alerts are overridden due to alert fatigue
(Smithburger et al., 2011, Phansalkar et al., 2012b,
Crosson et al., 2012), information overload (Callen
et al., 2011), poor user interface Design (Seidling et
al., 2011, Gaikwad et al., 2007, Rahmner et al.,
2012), poor Specification of the critical interactions
(Gaikwad et al., 2007), and inadequate Analysis
(Phansalkar et al., 2012a, Takarabe et al., 2011) of
the interactions. It will be necessary to include most
of the blank elements in the map of Stages 1 and 2
(Figure 2) to improve the effectiveness of the
checks. First, it would be necessary to Assess
(Saverno et al., 2011, Warholak et al., 2011) the
current system to provide feedback (Smithburger et
al., 2011) for Analysis (Phansalkar et al., 2012a,
Takarabe et al., 2011), Specification, and Design of
the system. Second, the Assessment could be done
internally by a provider, locally, or by a conference
of all the Stakeholders (Phansalkar et al., 2012b,
Phansalkar et al., 2012a, Hines et al., 2012). Third,
any Assessment and feedback will entail extensive
Analysis (Phansalkar et al., 2012a, Takarabe et al.,
2011) and Interpretation (Dhabali et al., 2012) of
empirical data (Haueis et al., 2011). Thus, the
success of a large number of components
encapsulated in the ontology will be essential for
effectively implementing the ‘drug-drug and drug-
allergy interaction checks’. In absence of a
systematic systemic (Saverno et al., 2011)
perspective, the checks may be implemented but
they may be meaningless, especially if they are
overridden constantly (Yu et al., 2011).
6 CONCLUSIONS
The ontological maps and histograms provide clear
visualizations of the gaps within each and between
them. Some of these gaps definitely need to be
bridged, as in the case of decision support for drug-
drug and drug-allergy interactions. The policy
makers and practitioners have to assess the
importance of the other gaps and change
requirements and practices to bridge them. This
process of feedback and change has to be ongoing
for continuous improvement of MUHIS. Ontological
maps such as the ones presented in this paper can
provide the foundations for visualizing the domain,
monitoring the incremental changes, and making it
complete and integrated.
In summary, we present an ontological meta-
analysis and synthesis of MUHIS requirements and
practice (Ramaprasad and Syn, 2013). It highlights
the domain’s bright spots which are heavily
emphasized, the light spots which are lightly
emphasized, the blank spots which are not
emphasized, and the blind spots which have been
overlooked. It also highlights the biases and
asymmetries in MUHIS requirements and practice;
they can be realigned to make them stronger and
more effective.
As we have emphasized earlier our ontology is
one lens through which one can study MUHIS.
There can be other equally valid frameworks. Each
lens will likely yield a different map and thus
different insights into the bright, light, and
blank/blind spots. Each of these sets of insights will
be a product of observing the phenomenon
systematically through a systemic framework, of a
different way of making the ‘elephant’ visible.
Reconciling these differences, in addition to
changing the map of each will advance knowledge
of MUHIS and can set the research/practice agenda
for the domain.
The ontology is extensible and reducible, and
hence the method is adaptable to the developments
in MUHIS. Should a new Function or Stakeholder of
MUHIS emerge in the future, they can be added to
the framework. Or, should a new subcategory of
Providers becomes a key Stakeholder, the
framework can be extended to accommodate the
change. By the same token, if a category becomes
irrelevant, it could be eliminated from consideration.
The extensibility and reducibility will also help trace
the evolution of the constructs in and the logic of
MUHIS.
Last, but not the least, visualization is key to
making sense of and interpreting ‘big text data’ like
the emerging requirements and practice of MUHIS.
The ontology provides an easy and intuitively
understandable vehicle for visualization. Note, for
example, the ontological maps can be used to study
the evolution of MUHIS over time by creating maps
for different cross-sections of time. It can also be
used to study the map at different levels of
granularity using more refined/coarsened
taxonomies. These are works in progress. Feedback
based on incremental ontological maps will help to
continuously improve MUHIS. With the current
ontological map of MUHIS requirements and
practice it is unlikely that the full vision of
meaningful use will be realized – they have to
evolve a lot.
The evolution has to balance the emphasis on the
categories, dimensions, and components of the
ontology. It has to balance the bright, light, blank,
and blind spots. Following are three examples:
HEALTHINF2014-InternationalConferenceonHealthInformatics
24

The emphasis on the Stakeholders has to be
balanced. All the stakeholders, individually and in
interaction with each other, collectively affect the
outcome.
With the increasing role of ‘big data’ and data
mining in healthcare the low emphasis on Analysis
and Interpretation will likely have to increased
significantly
Meaningful Use is itself a dynamic concept which
will evolve with time. MUHIS too has to be
equally dynamic. To do so the emphasis on
Analysis, Specification, Design, and Maintenance
(in Management) will have to be increased
considerably.
The ontological map can guide the evolution.
REFERENCES
Börner, K., Chen, C. & Boyack, K. W. 2003. Visualizing
knowledge domains. Annual Review of Information
Science and Technology, 37, 179-255.
Brennan, L., Voros, J. & Brady, E. 2011. Paradigms at
play and implications for validity in social marketing
research. Journal of Social Marketing, 1, 3-3.
Callen, J. L., Westbrook, J. I., Georgiou, A. & Li, J. 2011.
Failure to Follow-Up Test Results for Ambulatory
Patients: A Systematic Review. Journal of General
Internal Medicine, 27, 1334-1348.
Centers for Medicare & Medicaid Services. Meaningful
Use (Online). Available: https://www.cms.gov/
Regulations-and-Guidance/
Legislation/EHRIncentivePrograms/Meaningful_Use.
html.
Churchman, C. W. 1967. Wicked Problems. Management
Science, 14, B-141.
Cimino, J. J. 2006. In defense of the Desiderata. Journal
of Biomedical Informatics, 39, 299-306.
Classen, D. C., Phansalkar, S. & Bates, D. W. 2011.
Critical drug-drug interactions for use in electronic
health records systems with computerized physician
order entry: review of leading approaches. Journal of
Patient Safety, 7, 61-65.
Crosson, J. C., Schueth, A. J., Isaacson, N. & Bell, D. S.
2012. Early adopters of electronic prescribing struggle
to make meaningful use of formulary checks and
medication history documentation. The Journal of the
American Board of Family Medicine, 25, 24-32.
Dermer, M. & Morgan, M. 2010. Certification of primary
care electronic medical records: lessons learned from
Canada. J Healthc Inf Manag, 24, 49-55.
Dhabali, A. A. H., Awang, R. & Zyoud, S. H. 2012.
Clinically important drug–drug interactions in primary
care. Journal of clinical pharmacy and therapeutics.
Fensel, D. 2003. Ontologies: A Silver Bullet for
Knowledge Management and Electronic Commerce,
Springer.
Gaikwad, R., Sketris, I., Shepherd, M. & Duffy, J. 2007.
Evaluation of accuracy of drug interaction alerts
triggered by two electronic medical record systems in
primary healthcare. Health informatics journal, 13,
163-177.
Gruber, T. R. 1995. Toward Principles for the Design of
Ontologies Used for Knowledge Sharing.
International Journal Human-Computer Studies, 43,
907-928.
Gruber, T. R. 2008. Ontology. In: LIU, L. & OZSU, M. T.
(eds.) Encyclopedia of Database Systems. Springer-
Verlag.
Haueis, P., Greil, W., Huber, M., Grohmann, R., Kullak-
Ublick, G. A. & Russmann, S. 2011. Evaluation of
drug interactions in a large sample of psychiatric
inpatients: a data interface for mass analysis with
clinical decision support software. Clinical
Pharmacology & Therapeutics, 90, 588-596.
HealthIT.gov. Available: http://www.healthit.gov/
providers-professionals.
Hines, L. E., Malone, D. C. & Murphy, J. E. 2012.
Recommendations for Generating, Evaluating, and
Implementing DrugDrug Interaction Evidence.
Pharmacotherapy: The Journal of Human
Pharmacology and Drug Therapy, 32, 304-313.
Hoeffner, L. & Smiraglia, R. 2013. Visualizing Domain
Coherence: Social Informatics as a Case Study.
Advances In Classification Research Online, 23, 49-
51.
Horn, B. R. & Lee, I. H. Toward integrated
interdisciplinary information and communication
sciences: a general systems perspective. Proceedings
of the Hawaii International Conference on System
Sciences, 1989 Hawaii. IEEE, 244-255 vol. 4.
Kazimierczak, K. A., Skea, Z. C., Dixon-Woods, M.,
Entwistle, V. A., Feldman-Stewart, D., N'Dow, J. M.
O. & MacLennan, S. J. 2012. Provision of cancer
information as a “support for navigating the
knowledge landscape”: Findings from a critical
interpretive literature synthesis. European Journal of
Oncology Nursing, 1-10.
Ke, W. C., Hsieh, Y. C., Chen, Y. C., Lin, E. T. & Chiu,
H. W. 2012. Trend analysis and future development of
Taiwan electronic medical records. Stud Health
Technol Inform, 180, 1230-2.
Kim, H. & Kim, S. 2012. Legislation direction for
implementation of health information exchange in
Korea. Asia Pac J Public Health, 24, 880-6.
Kotis, K. & Vouros, G. 2006. Human-centered ontology
engineering: The HCOME methodology. Knowledge
and Information Systems, 10, 109-131.
Kriglstein, S. & Wallner, G. 2013. Human Centered
Design in Practice: A Case Study with the Ontology
Visualization Tool Knoocks. In: CSURKA, G.,
KRAUS, M., MESTETSKIY, L., RICHARD, P. &
BRAZ, J. (eds.) Computer Vision, Imaging and
Computer Graphics. Theory and Applications.
Springer Berlin Heidelberg.
Noar, S. M. & Zimmerman, R. S. 2005. Health Behavior
Theory and cumulative knowledge regarding health
behaviors: are we moving in the right direction?
AnOntologicalMapforMeaningfulUseofHealthcareInformationSystems(MUHIS)
25

Health Education Research, 20, 275-290.
Phansalkar, S., Desai, A. A., Bell, D., Yoshida, E., Doole,
J., Czochanski, M., Middleton, B. & Bates, D. W.
2012a. High-priority drug–drug interactions for use in
electronic health records. Journal of the American
Medical Informatics Association, 19, 735-743.
Phansalkar, S., van der Sijs, H., Tucker, A. D., Desai, A.
A., Bell, D. S., Teich, J. M., Middleton, B. & Bates, D.
W. 2012b. Drug–drug interactions that should be non-
interruptive in order to reduce alert fatigue in
electronic health records. Journal of the American
Medical Informatics Association.
Quine, W. V. O. 1961. From a Logical Point of View,
Boston, MA, USA, Harvard University Press.
Rahmner, P. B., Eiermann, B., Korkmaz, S., Gustafsson,
L. L., Gruvén, M., Maxwell, S., Eichle, H.-G. & Vég,
A. 2012. Physicians' reported needs of drug
information at point of care in Sweden. British Journal
of Clinical Pharmacology, 73, 115-125.
Ramaprasad, A. 1979. Role of Feedback in
Organizational-Change - Review and Redefinition.
Cybernetica, 22, 105-113.
Ramaprasad, A. 1983. On the Definition of Feedback.
Behavioral Science, 28, 4-13.
Ramaprasad, A. 1987. Cognitive Process as a Basis for
MIS and DSS Design. Management Science, 33, 139-
148.
Ramaprasad, A. & Mitroff, I. I. 1984. On Formulating
Strategic Problems. Academy of Management Review,
9, 597-605.
Ramaprasad, A. & Syn, T. 2013. Ontological Meta-
Analysis and Synthesis. Proceedings of the Nineteenth
Americas Conference on Information Systems,
Chicago, Illinois, August 15-17, 2013.
Ramaprasad, A., Valenta, A. L. & Brooks, I. 2009.
Clinical and Translational Science Informatics:
Translating Information to Transform Health Care. In:
AZEVEDO, L. & LONDRAL, A. R. (eds.)
Proceedings of HEALTHINF 2009 – Second
International Conference on Health Informatics.
Porto, Portugal: INSTICC Press.
Saverno, K. R., Hines, L. E., Warholak, T. L., Grizzle, A.
J., Babits, L., Clark, C., Taylor, A. M. & Malone, D.
C. 2011. Ability of pharmacy clinical decision-support
software to alert users about clinically important drug–
drug interactions. Journal of the American Medical
Informatics Association, 18, 32-37.
Scharnhorst, A. 2001. Constructing Knowledge
Landscapes Within the Framework of Geometrically
Oriented Evolutionary Theories. In: MATHIES, M.,
MALCHOW, H. & KRIZ, J. (eds.) Inegrative Systems
Approaches to Natural Social Dynamics.
http://www.virtualknowledgestudio.nl/staff/andrea-
scharnhorst/documents/constructing- knowledge-
landscapes.pdf: Springer.
Seidling, H. M., Phansalkar, S., Seger, D. L., Paterno, M.
D., Shaykevich, S., Haefeli, W. E. & Bates, D. W.
2011. Factors influencing alert acceptance: a novel
approach for predicting the success of clinical decision
support. Journal of the American Medical Informatics
Association, 18, 479-484.
Smithburger, P. L., Buckley, M. S., Bejian, S.,
Burenheide, K. & Kane-Gill, S. L. 2011. A critical
evaluation of clinical decision support for the
detection of drug-drug interactions. Expert Opinion on
Drug Safety, 10, 871-882.
Spina, J. R., Glassman, P. A., Simon, B., Lanto, A., Lee,
M., Cunningham, F. & Good, C. B. 2011. Potential
Safety Gaps in Order Entry and Automated Drug
Alerts: A Nationwide Survey of VA Physician Self-
Reported Practices With Computerized Order Entry.
Medical Care, 49, 904-910.
Syed, K., Kröll, M., Sabol, V., Scharl, A., Gindl, S.,
Granitzer, M. & Weichselbraun, A. 2012. Dynamic
Topography Information Landscapes–An Incremental
Approach to Visual Knowledge Discovery. Data
Warehousing and Knowledge Discovery, 352-363.
Takarabe, M., Shigemizu, D., Kotera, M., Goto, S. &
Kanehisa, M. 2011. Network-Based Analysis and
Characterization of Adverse Drug–Drug Interactions.
Journal of chemical information and modeling, 51,
2977-2985.
Varroud-Vial, M. 2011. Improving diabetes management
with electronic medical records. Diabetes Metab, 37
Suppl 4, S48-52.
Warholak, T. L., Hines, L. E., Saverno, K. R., Grizzle, A.
J. & Malone, D. C. 2011. Assessment tool for
pharmacy drug–drug interaction software. Journal of
the American Pharmacists Association, 51, 418-424.
Yu, D. T., Seger, D. L., Lasser, K. E., Karson, A. S.,
Fiskio, J. M., Seger, A. C. & Bates, D. W. 2011.
Impact of implementing alerts about medication
blackbox warnings in electronic health records.
Pharmacoepidemiology and drug safety, 20, 192-202.
Zhang, J., Xie, J., Hou, W., Tu, X., Xu, J., Song, F.,
Wang, Z. & Lu, Z. 2012. Mapping the Knowledge
Structure of Research on Patient Adherence:
Knowledge Domain Visualization Based Co-Word
Analysis and Social Network Analysis. PLoS ONE, 7.
HEALTHINF2014-InternationalConferenceonHealthInformatics
26
