
The Present and Future of Dynamic e-Health Interoperability in
Switzerland
Results of an Online Questionnaire
Visara Urovi and Michael I. Schumacher
Institute of Business and Information Systems, University of Applied Sciences of Western Switzerland, Sierre, Switzerland
Keywords:
e-Health, Semantic Interoperability, Dynamic EHR Echange, IHE, Interoperability Standards.
Abstract:
The research in the medical health care systems is shifting towards solutions that enable dynamic data ex-
change. To achieve this shift, interoperable solutions have been proposed by initiatives such as the integrating
Healthcare Enterprise (IHE). IHE focuses on defining interoperable solution by specifying recommendations
that foster standard based integration between healthcare systems. Using the results of an online questionnaire,
in this work we study the current use of standards in the health care systems of Switzerland. The question-
naire identifies four dynamic data exchange scenarios that enhance the interoperability and the integration
between different healthcare systems. The novelty of this work is that the identified scenarios are currently
not addressed by the IHE recommendations and, they can improve the current interoperability solutions. The
questionnaire confirms that those scenarios are useful and we suggest some technical solutions that may help
to achieve them.
1 INTRODUCTION
Electronic Health Records (EHRs) are electronic col-
lections of health information about patients (Gunter
and Terry, 2005). EHRs are easy to transfer and, if
linked to best-practice guidelines, they can support
care decisions (Grimson et al., 2000). Many of the
current EHR systems operate in a closed environ-
ment where patient’s EHRs can be dynamically ex-
changed only within the health organisation that cre-
ates them. As the focus of health care delivery shifts
from specialist centers to community settings (Kalra,
2006), new approaches are focusing on the integra-
tion of such records across the institutional bound-
aries (Wozak et al., 2008).
The health industry is recognizing the impor-
tance of dynamic exchange of EHRs by adopting in-
teroperability standards and by seeking integrations
with external platforms. In particular, the Integrat-
ing the Healthcare Enterprise (IHE)
1
is an initia-
tive that specifies guidelines on how healthcare pro-
viding systems can integrate and communicate more
effectively. IHE enjoys high acceptance due to its
practical complement to existing standards such as
HL7 CDA
2
. The IHE consortium specifies various
1
www.ihe.net
2
HL7 CDA is a standard supporting message-based in-
IHE Integration Profiles which define solutions to
specific problems. The Integration Profiles are con-
stantly checked against practical experiences and are
continuously adapted (Wozak et al., 2008). Despite
this, IHE lacks features to handle dynamic scenar-
ios where caregivers can dynamically connect and ex-
change data (IHE, 2008), and mechanisms on how pa-
tient’s data are found and exchanged are yet to be de-
fined.
Using an online questionnaire, this paper dis-
cusses the gap between the interoperability standards
and what healthcare system solutions are currently
missing in order to support the dynamic data ex-
change. The questionnaire confirms that there is a
gap between the use of interoperability standards and
the current ability to dynamically connect and share
patient data at a cross community level. The partici-
pants recognized as very important for health systems
to rely on interoperability standards and found useful
to have more dynamic scenarios for EHR exchange.
The paper is organized as follows. Section 2 intro-
duces the current standards and semantic dictionaries
defined in health care systems. Section 3 discusses
the focus of the survey, the recruiting of participants
and the design of the online questionnaire used for the
study. Section 4 illustrates the results of the question-
formation exchange of medical data www.hl7.org
244
Urovi V. and I. Schumacher M..
The Present and Future of Dynamic e-Health Interoperability in Switzerland - Results of an Online Questionnaire.
DOI: 10.5220/0004748902440249
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2014), pages 244-249
ISBN: 978-989-758-010-9
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)
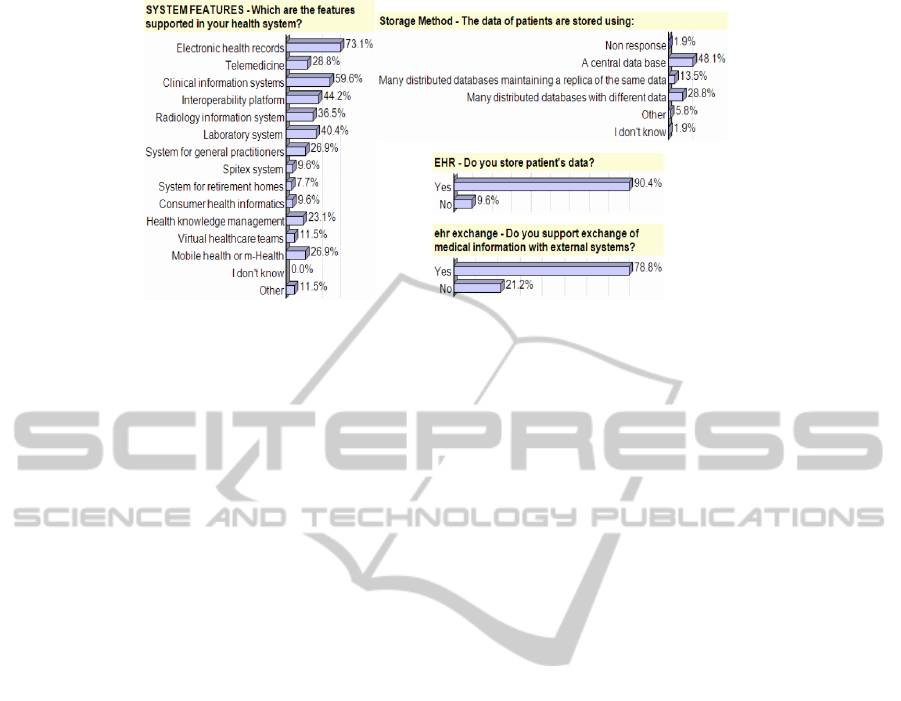
Figure 1: The characteristics of the represented systems.
naire. Section 5 discusses how future technical solu-
tions may drive interoperability in healthcare systems.
Finally, Section 6 summarizes this work.
2 SEMANTIC
INTEROPERABILITY
Semantic interoperability in a medical context means
that medical data are exchanged and processed in dis-
tributed systems by unambiguously sharing the mean-
ing of the document content (Reinhold et al., 2011).
Standard models for EHR exchange play a funda-
mental role for achieving semantic interoperability.
Among the standardisations efforts, the most adopted
nowadays have become HL7 (Dolin et al., 2001) and
OpenEHR (Garde et al., 2007), for structuring the
health data, IHE for defining the architectural as-
pects of EHR exchange, and SNOMED CT (Stearns
et al., 2001), LOINC (McDonald et al., 2003) and
MEDICINE (Goltra, 1997) as code based systems for
the medical terminology.
HL7 is a standard supporting message-based ex-
change of medical data. The most adopted HL7
standard is the HL7-Clinical Document Architecture
(HL7-CDA). HL7-CDA specifies the syntax and sup-
plies a framework for specifying the full semantics of
a clinical document. The focus of HL7 is in the mes-
sage exchange and not in the organization of the EHR,
thus this standard alone is not enough to achieve in-
teroperability. OpenEHR is standard that describes
the management, storage, retrieval and exchange of
EHR. Like HL7, OpenEHR proposes a set of models
for clinical data with the difference that the reference
model is based on building blocks and its underlying
modeling style is strictly object oriented, thus, solv-
ing several limitations of the message based exchange
model proposed by HL7-CDA. Healthcare terminolo-
gies such as SNOMED CT, LOINC and MEDICINE
define universal code names and identifiers to medi-
cal terminology. Their purpose is to associate codes to
medical terminology so that, if everyone was to share
them, it would be possible to share and automatically
understand the health data, such as the one exchanged
in HL7 messages.
The IHE Integration profiles are becoming the
glue to these standardization efforts. They com-
plement these standards with concrete recommen-
dations on how to achieve interoperability in terms
of how to construct the messages that enable data
to be exchanged and what are the actors that in-
volved in these interactions. There are many IHE
profiles that address interoperability between health
care systems. We focus on the ones that propose solu-
tions for EHR exchange (denoted as XC*), namely
Cross-Enterprise Document Sharing (XDS), Cross-
Community Access (XCA), Cross-Community Pa-
tient Discovery (XCPD) and Cross-Community Fetch
(XCF).
The XDS (IHE, 2011) profile defines how health
enterprises can inter-operate to share patient-relevant
documents by working as one health community with
the same set of policies, patient identifications and
security mechanisms. Since XDS does not resolve
document sharing among multiple communities, the
XCA profile specifies how medical data held by other
communities can be queried and retrieved. XCA as-
sumes that communities have pre-established agree-
ments, knowledge of one another and have ways to
know the correct patient identifiers in different com-
munities (IHE, 2008). XCPD locates communities
which hold patient’s relevant health data and trans-
lates patient’s identifiers across communities. XCPD
does not automate the discovery of communities and
it still requires communities to have pre-established
agreements for exchanging the documents. Finally
XCF defines a single transaction to retrieve a small
number of documents (ideally one). XCF requires
document properties to be known prior to the doc-
ThePresentandFutureofDynamice-HealthInteroperabilityinSwitzerland-ResultsofanOnlineQuestionnaire
245

Figure 2: Standard’s use and importance. Figure 3: The use and importance of semantic dictionaries in EHR exchange.
ument retrieval. Other IHE profiles support cross-
community data exchange by providing: security
(Audit Trial and Node Authentication); privacy (Ba-
sic Patient Privacy Concent); mapping of user identi-
fications (Cross-Enterprise User Assertion); point-to-
point e-mail notification of updates (Notification of
Document Availability); and a consistent time (Con-
sistent Time). Not all of these profiles are manda-
tory to integrate in the healthcare systems that sup-
port cross-community document exchange, however
they provide important technical solutions for secure
interoperability at a cross-community level.
3 METHOD
Our study focuses on the use of interoperability solu-
tions in Switzerland. The health system in Switzer-
land is a combination of public (i.e. hospitals) and
private systems (i.e. private clinics) and health condi-
tions can be treated in any of the competent healthcare
providers. The Swiss Government has recently rec-
ommended the adoption of IHE profiles to achieve in-
teroperability. The first pilot deployments have been
released, such as the eToile project (Geissbuhler et al.,
2004) in Geneva and Infomed (Michelet et al., 2011)
in Valais. The objective of the questionnaire was to
find out the current state and the future directions with
regards to the dynamic EHR exchange.
The survey was based on an online questionnaire
which was sent to the Swiss eHealth summit
3
, a
leading event for ICT in medicine and healthcare for
Switzerland, with around 200 experts interested in
ways technology can improve medicine and health-
care in general.
Fifty two participants took part on the survey. The
3
http://www.ehealthsummit.ch/
majority of the participants (28.8%) were holding an
IT role, followed by 15.4% and 13.5% respectively
holding Chief Technology Officer, or Chief Execu-
tive Officer roles. These roles are very important for
our questionnaire as they can best answer the tech-
nical and strategical aspects of the represented sys-
tems. It also suggests to us that we met our target
audience for having relevant results within the scope
of the questionnaire. We asked the participants about
their represented system, the use of standards and how
interoperable their systems is. Figure 1 summarizes
the features of the systems represented by the partic-
ipants. The majority were systems dealing with EHR
and with clinical information (73.1% and 59.6% re-
spectively). Also, 44.2% of the participants said that
their represented system solution provides a solution
to interoprerability. Storage of EHR accounted for
90.4% with 78.2% also supporting EHR exchange.
The storage of EHR was mostly done within a cen-
tral database (49%). The results described in Section
4 are based on what the participant said about these
types of systems.
In order to specify future directions in terms of
healthcare interoperability, we defined four scenarios
that were drawn from an analysis of the state of the
art, with specific focus into what is currently missing
in the IHE interoperability solutions. The scenarios
were described as follows:
• Scenario 1: A patient is treated in the hospital A,
rather than the hospital B of its residence area.
The system of hospital A can find the patient’s
data in the system of hospital B without prior in-
tegration between the two.
• Scenario 2: A patient is treated in the hospital A,
rather than the hospital B of its residence area.
Hospital A creates new health records on the pa-
tient. The Hospital A, upon patient’s consent,
HEALTHINF2014-InternationalConferenceonHealthInformatics
246
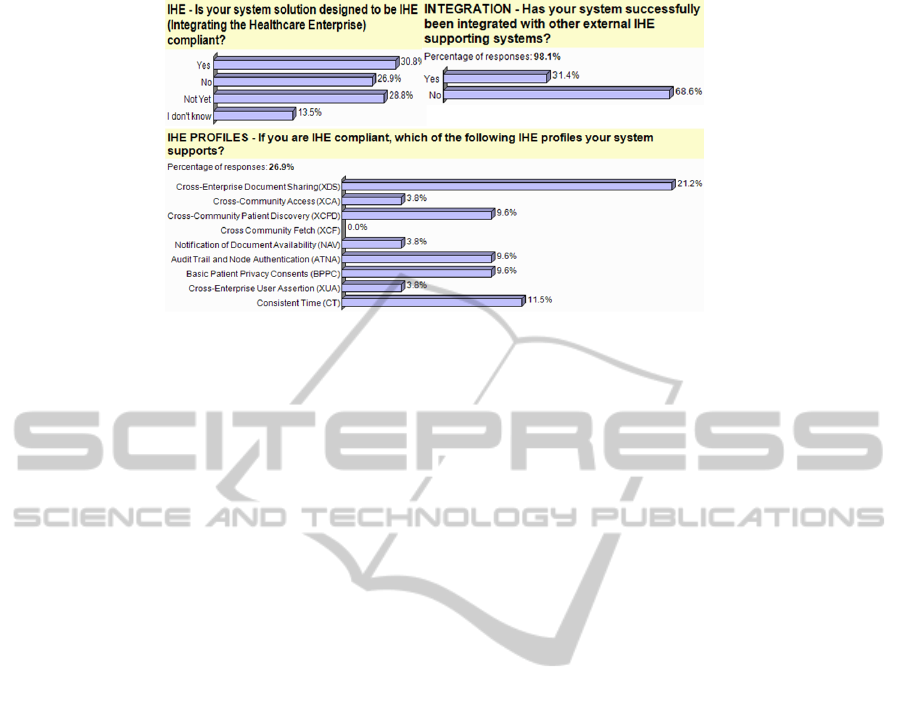
Figure 4: The use of IHE Interoperability Standards.
automatically updates the system B about these
records.
• Scenario 3: A patient is treated in the hospital
A. This patient has chosen that all the updates
concerning his health should be sent to hospital
B. The Hospital B collects all the updates on the
health of its patients.
• Scenario 4: A Hospital B receives health updates
on one of its patients. This patient has agreed that
his general doctor should receive these updates as
well. Hospital B, upon patient’s consent, automat-
ically propagates updates on patients to subscrib-
ing clinics.
4 RESULTS
4.1 Interoperability in Swiss Healthcare
Systems
We asked what are the general trends towards interop-
erability? We focused on three factors that combined
are known to foster integration within heterogenous
health platforms, namely the use of standards, the use
of semantic dictionaries and the use of IHE profiles
for standard system architectures. We were interested
to know the acceptance level of the existing standards.
For this reason, we asked what standards were used to
store patient data. Figure 2 shows that 63.5% agreed
that standards are important for interoperability with
other systems and, the most used standard for stor-
ing patient related data was HL7 (53.8%). The use of
HL7 standard is highly recommended in the current
IHE profiles. The result shows that the adoption of
IHE interoperability solutions is possible.
In order to measure the extend to which semantic
dictionaries are used in today’s Swiss healthcare set-
tings we asked the participants if, in their represented
systems: i) semantic dictionaries were used to de-
scribe data, ii) if the reason for their use was to enable
interoperability and iii) if the participants believed
that using the semantic dictionaries fosters record ex-
change. Figure 3 shows the results to these three ques-
tions. The majority of the participants (46.2%) did not
recognize the use of semantic data to be needed in de-
scribing patient health records or messages. This may
be due to the fact that most of the data exchanged with
external systems still requires human intervention and
automated data exchange has a long way to go. The
26.9% and 23.1% of users did respectively strongly
agreed and agreed that the use of semantic dictionar-
ies in their system was made to enable interoperabil-
ity with external systems. Additionally, 40.4% and
36.5% respectively strongly agreed or agreed that se-
mantic dictionaries, if used to describe EHRs, foster
their exchange.
In order to find out to what level the existing IHE
interoperability solutions are integrated in the current
health care systems, we asked if the represented sys-
tems were IHE compliant. Participants were given the
possibility to express interest in using IHE in the fu-
ture by answering ”Not Yet”. We considered that the
IHE adoption is quite new with respect to the digi-
talization of the EHR and that these systems may, in
the future, adapt to interoperate with other healthcare
systems. We also asked what specific IHE profiles
were supported and if they had been integrated with
other external IHE compliant systems. Figure 4 sum-
marizes the results which show that i) the use of IHE
accounted for 30.8%, however, another 28.8% indi-
cated an intention of using them, ii) In Switzerland,
the IHE profiles that support EHR exchange are be-
ing adopted. XDS is the most used (21.2%) because
it supports document exchange at the health organiza-
tion level. iii) 30.8% of the participants said that there
had been successful integration(s) with other external
IHE supporting system(s).
ThePresentandFutureofDynamice-HealthInteroperabilityinSwitzerland-ResultsofanOnlineQuestionnaire
247
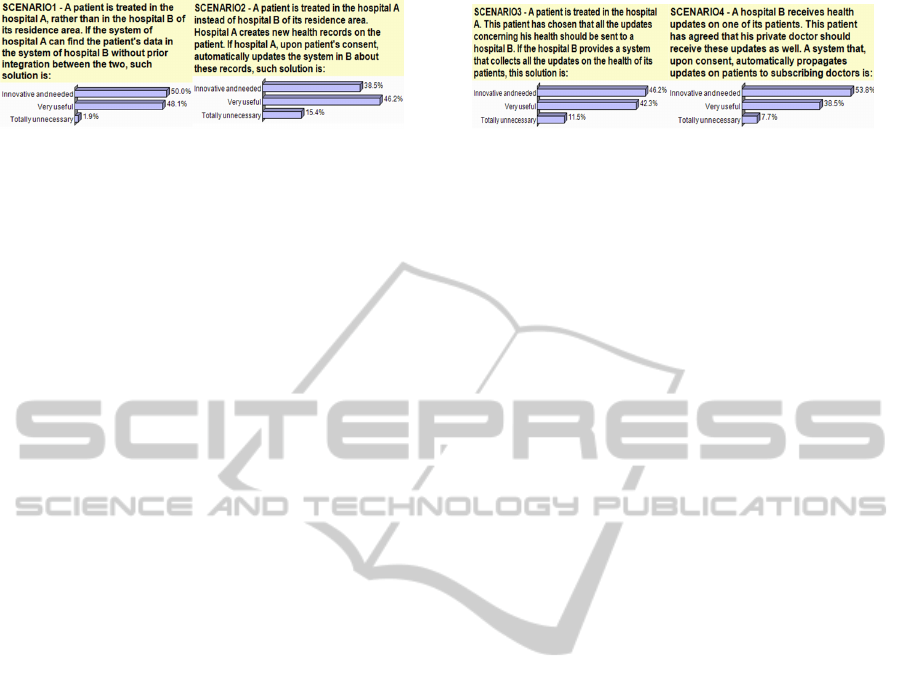
Figure 5: The results for Scenario 1 and 2. Figure 6: The results for Scenario 3 and 4.
4.2 Future Interoperability Scenarios
In order to find out what are the trends with respect to
interoperability solutions in health care systems, we
asked the participants to determine if the scenarios
presented in Section 3 were innovative, very useful
or unnecessary. Only one response was possible. A
distinction between innovative and useful was done
in order to determine if the scenarios were novel for
the participants as opposed to a useful feature which
already may exist in some systems.
Figure 5 and 6 show that all the scenarios are well
received with an average of 84.7-98.1% of partici-
pants finding the four scenarios either innovative or
very useful. The first scenario was the most impor-
tant feature with 50% finding the scenario innovative,
48.1% very useful and 1.9% finding it as unnecessary.
This result confirms that being able to dynamically
view data of patients held in other healthcare settings
is very beneficial.
5 DISCUSSION
The results of the questionnaire show that there is a
need to exchange data in more dynamic settings. The
realization of the four proposed scenarios requires
health communities to adopt standard approaches and
enable solutions for sharing their EHR in open and
dynamic settings. Some attempts in this direction
have already been done. The epSOS project pro-
vides cross-border health-services to patients seek-
ing healthcare in different countries from their own.
In Switzerland, e-Toile project proposes an universal
information exchange service for e-Health that cov-
ers a geographic area (Geneva). SemHealthCoord
project defines an architecture that enhances the cur-
rent IHE profiles with more dynamic EHR exchange
solution (Urovi et al., 2013). Presenting these works
is out of the scope of this paper, but it suffices to say
that all of those recent works rely on IHE profiles for
the data exchange. It is also worth noting that, for the
achievement of the four scenarios, ethical, legal and
security aspects must be investigated as much as the
challenges of the technical solution.
From a technical viewpoint, in addition to provid-
ing integration through use of standards, the results
suggest two key components that are important for
designing interoperable healthcare system solutions:
(a) dynamicity and (b) scalability. A dynamic solu-
tion supports EHR exchange with functions for find-
ing EHRs of patients independently from the system
that creates and stores them while a scalable solution
is needed to optimize the time and effort to find and
exchange EHRs.
A dynamic model for EHR exchange requires so-
lutions that address the semantic interoperability be-
tween heterogeneous healthcare systems. By provid-
ing semantic descriptions of the data held in other
health oganisations, it is possible to facilitate the in-
terpretation and sharing of the health data (Hendler,
2001). The semantic interoperability enables local
processing of the shared data; and it is also a prereq-
uisite for intelligent decision support and care plan-
ning (Schloeffel et al., 2006). In this context, the
agent technology brings advantages to interoperabil-
ity of the health care solutions such as high adapt-
ability in front of changes, distributed management
of sources and remote access to patient data (Isern
et al., 2010). In fact, agent-based systems can perform
distributed communication and reason with semantic
knowledge, thus enabling EHR sharing between such
heterogeneous systems. Finally, to support the dy-
namics of the scenarios here defined, common coordi-
nation models are needed in order to decouple the in-
teractions within different health organizations (Urovi
et al., 2013).
Scalability on a dynamic network of health com-
munities can be achieved by overlaying a Peer to Peer
(P2P) network (Androutsellis-Theotokis and Spinel-
lis, 2004) to link the heterogeneous health organi-
sation’s systems as peers (Kilic et al., 2010). The
P2P allows communities to interact on top of existing
network configurations without a central dependency.
With the right P2P network configurations, the time
to answer queries can be logarithmic with a growing
number of peers (Androutsellis-Theotokis and Spinel-
lis, 2004). The use of P2P technology in health care
settings is a novel concept (Guo et al., 2011) and it
requires security and privacy considerations. There
are many factors to consider, from sharing confiden-
tial information in a secure manner, to guaranteeing
the proper use of the EHRs. All these aspects require
HEALTHINF2014-InternationalConferenceonHealthInformatics
248

the security to be focal point to the design of such so-
lutions because it will determine if these frameworks
will, in the future, have a practical value.
6 CONCLUSIONS
We presented a study of the current situation and of
the future directions in dynamic interoperable solu-
tions for healthcare systems. We focused on the re-
sults of an online questionnaire collected from the
participants of the Swiss eHealth summit. The re-
sults showed a general trend towards the use of IHE
and HL7 which is a good indicator of solutions that
can support integration with other systems. The re-
sults also suggested that the future interoperability
will require more dynamic and open solutions to-
wards record exchange. Finally we discussed some
technical solutions that can make the difference to-
wards supporting these future scenarios. As part of
our future work, we plan to further investigate the im-
plications of the four proposed scenarios. The techni-
cal solution is only one aspect of realising these sce-
narios. We plan to study what are the practical, legal
and ethical aspects that may prevent institutions to go
towards more dynamic settings and how to overcome
them. Including issues of depersonalization and min-
imization of data and the way these can be integrated
in cross-institutional IHE settings.
ACKNOWLEDGEMENTS
This work was funded by the Switzerland FNS grant
nr. 200021 135386 / 1.
REFERENCES
Androutsellis-Theotokis, S. and Spinellis, D. (2004). A sur-
vey of Peer-to-Peer content distribution technologies.
ACM Comput. Surv., 36(4):335–371.
Dolin, R. H., Alschuler, L., Beebe, C., Biron, P. V., Boyer,
S. L., Essin, D., Kimber, E., Lincoln, T., and Matti-
son, J. E. (2001). The HL7 Clinical Document Archi-
tecture. Journal of the American Medical Informatics
Association, 8(6):552–569.
Garde, S., Knaup, P., Hovenga, E., and Heard, S.
(2007). Towards semantic interoperability for elec-
tronic health records–domain knowledge governance
for open ehr archetypes. Methods of information in
medicine, 46(3):332–343.
Geissbuhler, A., Spahni, S., Assimacopoulos, A., Raetzo,
M., and Gobet, G. (2004). Design of a patient-
centered, multi-institutional healthcare information
network using Peer-to-Peer communication in a
highly distributed architecture. Medinfo, 11(Pt
2):1048–52.
Goltra, P. S. (1997). MEDCIN: a new nomenclature for
clinical medicine. Springer.
Grimson, J., Grimson, W., and Hasselbring, W. (2000). The
SI challenge in health care. Commun. ACM, 43:48–55.
Gunter, D. T. and Terry, P. N. (2005). The emergence of
national electronic health record architectures in the
united states and australia: Models, costs, and ques-
tions. J Med Internet Res, 7(1):e3.
Guo, Y., Hu, Y., Afzal, J., and Bai, G. (2011). Using
P2P technology to achieve eHealth interoperability. In
Service Systems and Service Management (ICSSSM),
pages 1 –5.
Hendler, J. (2001). Agents and the Semantic Web. IEEE
Intelligent Systems, 16:30–37.
IHE (2008). White paper: Cross community infor-
mation exchange. http://www.ihe.net/ Techni-
cal Framework/upload/IHE ITI TF White Paper
Cross Community 2008-11-07.pdf.
IHE (2011). Technical framework integration profiles vol 1.
http://www.ihe.net.
Isern, D., Snchez, D., and Moreno, A. (2010). Agents ap-
plied in health care: A review. International Journal
of Medical Informatics, 79(3):145 – 166.
Kalra, D. (2006). Electronic health record standards. vol-
ume 45, pages 136–144. Methods Inf Med.
Kilic, O., Dogac, A., and Eichelberg, M. (2010). Provid-
ing interoperability of ehealth communities through
peer-to-peer networks. Information Technology in
Biomedicine, IEEE Transactions on, 14(3):846–853.
McDonald, C. J., Huff, S. M., Suico, J. G., Hill, G.,
Leavelle, D., Aller, R., Forrey, A., Mercer, K., De-
Moor, G., Hook, J., et al. (2003). LOINC, a universal
standard for identifying laboratory observations: a 5-
year update. Clinical chemistry, 49(4):624–633.
Michelet, C., Fragnire, F., and Gnaegi, A. (2011). Infomed,
dossier patient partag en Valais. Journal of Swiss
Medical Informatics, 72.
Reinhold, S., Henning, M., Dominik, A. and Patrick, R.
2011. e-Heallth Semantic and Content for Switzerland
Schloeffel, P., Beale, T., Hayworth, G., Heard, S., and
Leslie, H. (2006). The relationship between cen 1360
6, hl7 and openehr. HIC and HINZ Proceedings, 24.
Stearns, M. Q., Price, C., Spackman, K. A., and Wang, A. Y.
(2001). SNOMED clinical terms: overview of the de-
velopment process and project status. In Proceedings
of the AMIA Symposium, page 662. American Medical
Informatics Association.
Urovi, V., Olivieri, A., Bromuri, S., Fornara, N., and
Schumacher, M. (2013). A P2P Agent Coordination
Framework for IHE based Cross-Community Health
Record Exchange. In ACM 28th Symposioum on Ap-
plied Computing, page to appear.
Wozak, F., Ammenwerth, E., Hoerbst, A., Soegner, P., Mair,
R., and Schabetsberger, T. (2008). IHE based Interop-
erability - Benefits and Challenges. volume 136 of
Studies in Health Technology and Informatics, pages
771–776. IOS Press.
ThePresentandFutureofDynamice-HealthInteroperabilityinSwitzerland-ResultsofanOnlineQuestionnaire
249
