
A Clinical Data Warehouse Architecture based on the Electronic
Healthcare Record Infrastructure
Fabrizio Pecoraro
1
, Daniela Luzi
1
and Fabrizio L. Ricci
2
1
Institute for Research on Population and Social Policies, National Research Council, Via Palestro 32, Rome, Italy
2
Institute for Systems Analysis and Computer Science, National Research Council, Viale Manzoni 30, Rome, Italy
Keywords: Electronic Healthcare Record (EHR), Secondary Uses, Clinical Indicators, Data Warehouse, Dimensional
Model.
Abstract: The development of clinical data warehouses is becoming increasingly important in the healthcare domain
to support organizations in the improvement of decision-making, business processes as well as the
communication between clinicians, patients and the administration. However, data and process integration is
a big challenge considering the heterogeneous and distributed nature of healthcare information systems.
This paper proposes a data warehouse architecture based on the Italian Electronic Health Record (EHR)
technological infrastructure. It describes the main advantages in the application of EHR systems for
secondary purposes and reports the data warehouse design framework outlining its architecture as well as a
dimensional model based on a dashboard defined to manage the intervention of patients with diabetes. The
adoption of EHR systems enhances interoperability given that these systems share standardized clinical data
among multiple parties involved in different healthcare settings.
1 INTRODUCTION
The widespread diffusion of Information
Technologies in different healthcare settings has led
to a production of a massive amount of both clinical
and administrative data. Despite all the efforts, these
information are often stored in standalone
heterogeneous information systems developed for
specific specialties (radiology, admissions, general
ledger, scheduling, pharmacy and patient records)
that do not interchange data with each other
(Wickramasinghe and Schaffer, 2006). Therefore,
researchers doing data analysis still face
interoperability and technical challenges in the
support of administrative and clinical processes for
purposes different than those they were gathered for
(e.g. management information, quality assessment
and research) (Kush et al., 2008, Taylor, 2008). In
addition, data analysis can be a complex task
considering that medical and sensitive information
(Koh and Tan, 2011) are usually restricted in access
due to ethical, legal and privacy issues. This makes
it also necessary to collect and integrate these
information before data analysis can be performed
and to adopt specific techniques for data
anonymisation and processing.
An important initial step toward the integration of
data provided by heterogeneous multiple systems is
the development of enterprise clinical data
warehouses that are becoming increasingly
important in the healthcare domain (Botsis et al.,
2010, Kamal et al., 2005). This approach is adopted
by different parties (e.g. hospital, GP, specialists)
(Zhou et al., 2010, Sahama and Croll, 2007) and at
different organizational level (i.e. local, regional and
national authorities) (De Mul et at., 2012, Stow et
al., 2006) in order to improve decision-making,
business processes as well as communication
between clinicians, patients and the administration.
However, the implementation of data warehouses
implies the solution of issues related to missing,
corrupted, inconsistent or non-standardized data
collected in different formats and data sources. In
particular, the lack of a standard vocabularies is a
serious barrier for the integration and analysis of
data (Gillespie, 2000).
Electronic Health Record (EHR) systems
represent a core source of information, managed and
processed by multiple parties involved in healthcare
settings. Their main purposes are to support
physicians and other professionals in the delivery of
care management services giving direct benefits to
287
Pecoraro F., Luzi D. and L. Ricci F..
A Clinical Data Warehouse Architecture based on the Electronic Healthcare Record Infrastructure.
DOI: 10.5220/0004764502870294
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2014), pages 287-294
ISBN: 978-989-758-010-9
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

citizens in terms of speed and appropriateness of
healthcare service delivery (primary uses). However,
different recent experiences have recognized the
successful use of EHRs for secondary purposes
(Safran et al., 2007), such as clinical research
(Hussain et al., 2012), epidemiological studies
(Diomidous et al., 2009), ambulatory clinical care
(Jensen et al., 2012), pharmacovigilance (Wang et
al., 2009), comorbidity detection (Roque et al.,
2011) or to alert providers of potential clinical risks
(Lurio et al., 2010). However, these secondary uses
of EHR are generally limited to a single institution
(e.g. Hospital) or a single provider (e.g. General
Practitioners) and/or on a specific target population
(e.g. diabetics, investigational patients). Conversely,
in our approach EHR is considered as a large-scale
information infrastructure that integrates
heterogeneous information systems managed by
different organizations in a distributed environment.
In our vision this EHR infrastructure can be the basis
to develop a data warehouse as a business
intelligence tool in a clinical governance framework.
In this perspective EHR systems can be used to
evaluate the effectiveness and appropriateness of
healthcare services from the structural,
organizational, financial and professional points of
view. This improves the transparency of economic
and clinical activities as well as the availability of
real time information to decision makers (Mettler
and Rohner, 2009). Moreover, the use of EHRs
increases healthcare data quality and facilitates the
interoperability between different systems and
organizations. In particular, standardized data model
as well as international widespread vocabularies and
nomenclatures ensure a reliable data collection and a
consistent data comparison even when collected
from heterogeneous information systems. This
approach can also provide additional values in
different healthcare-related sectors including
education, clinical research, public health, security
and policy support (Committee on Data Standards
for Patient Safety, 2003).
This paper proposes a clinical data warehouse
architecture based on the EHR infrastructure
developed in Italy. To demonstrate the feasibility of
the data warehouse architecture a set of indicators
related to diabetes pathology is proposed in
particular to implement a chronic disease
management intervention. Afterwards, starting from
these indicators a business process is presented
highlighting the design methodology of a
dimensional model.
2 DATA WAREHOUSE DESIGN
2.1 EHR Infrastructure and
Conceptual Model
In Italy the development of a local EHR system is
delegated to each regional administration. To ensure
the interoperability between the different local
solutions the Department for the digitization of
Public Administration and Innovation Technology in
collaboration with the Department of Information
and Communication Technologies of the National
Research Council (CNR) have carried out the InFSE
project (EHR technological infrastructure) (Ciampi
et al., 2012) that defines a set of technological
requirements with the aim of developing an
interoperable EHR national infrastructure. InFSE
provides a set of infrastructural components that
notify clinical events to the involved local EHR
systems through the adoption of a publish-subscribe
pattern. Moreover, it archives clinical documents as
generated by authorized users during a clinical event
guaranteeing their persistency, security and
reliability. To ensure semantic interoperability
among local systems clinical documents stored in
the relevant repository are structured using HL7
CDA (Clinical Document Architecture) Release 2
standard (Dolin et al., 2006). This standard allows to
structure the content of both header and body of a
document using the XML standard based on HL7
Reference Information Model (RIM) (Schadow et
al., 2006), coupled with terminology. Moreover, to
facilitate documents retrieval and localization InFSE
components manage a set of descriptive metadata,
such as document type, patient ID, document author,
organization responsible for the document security,
date of creation and update of the document,
location of the document (URI), etc. However, to
simplify the relationship between documents
produced in different clinical events as well as to
facilitate their sharing between different actors it is
necessary to introduce a higher level of document
aggregation and classification schema, providing a
set of concepts that represents both content and
context of healthcare services. These concepts were
defined in the CONTsys standard (EN 13940, 2007)
to describe different aspects of clinical and
organizational processes such as health issue,
contact and episode of care. They enable the
information management of the healthcare delivery
process to an individual subject of care as well as its
continuity, taking into consideration data handling,
decision processes, quality control and resource
management. These concepts and their relationships
HEALTHINF2014-InternationalConferenceonHealthInformatics
288
have been the basis of the EHR conceptual model as
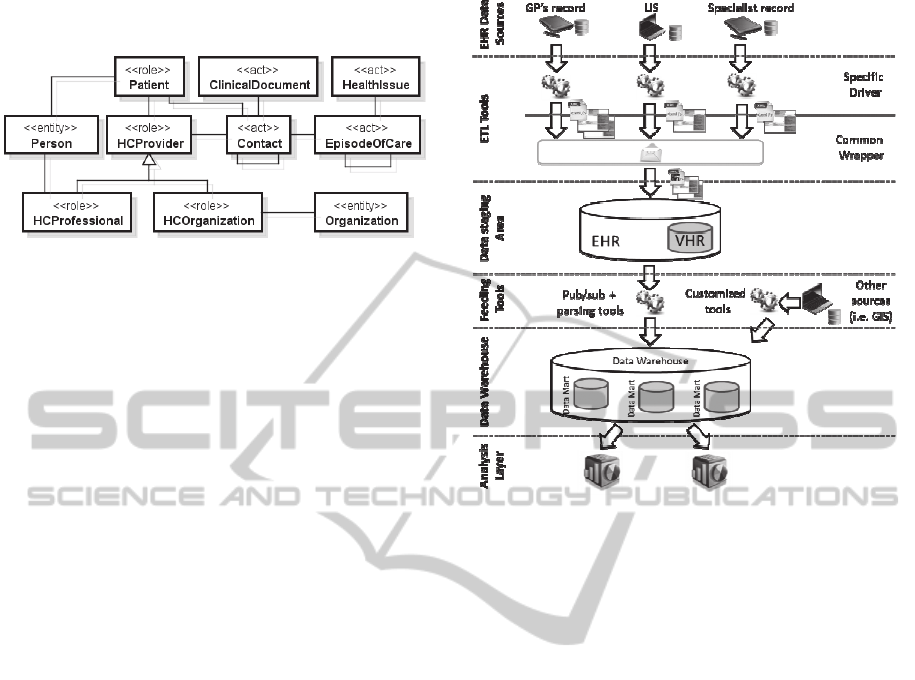
shown in Figure 1 mapped in the HL7 RIM.
Figure 1: Portion of the EHR domain model based on the
CONTsys concepts.
The RIM is not just the starting point to represent
a clinical document backbone but it is also used as a
standard for defining the structure of a message to be
exchanged between heterogeneous information
systems to achieve semantic interoperability (Oemig
and Blobel, 2005). The main class of this model is
the Contact that describes an encounter between the
Patient and a Healthcare Provider (e.g. GP). Each
Contact is associated with one or more Episode Of
Care (e.g. weight gain), each one related to one or
more Health Issue (e.g. diabetes) suffered by the
Patient. During a Contact a set of Clinical
Documents are produced by the Provider. An
extended model of the proposed diagram has been
used to define the conceptual model of LuMiR, a
region-wide EHR system (Contenti et al., 2008).
Based on the conceptual model shown in Figure 1 it
is possible to define relevant indicators that can be
used for secondary purposes such as the comparison
of different phenomena over a period of time and
between different areas of the same region.
2.2 Data Warehouse Architecture
From the architectural point of view, the data
warehouse has been designed as a three-tier
architecture considering the information collected
and the relevant infrastructure of the EHR described
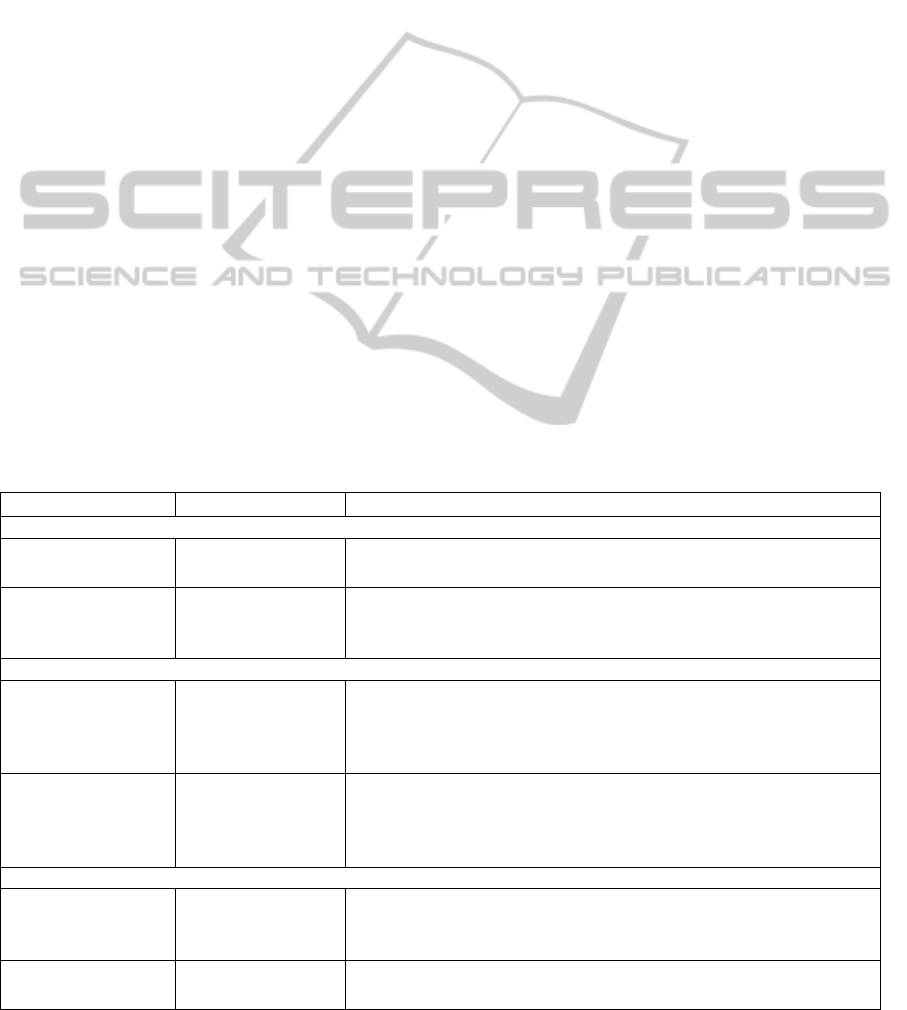
in the previous paragraphs. As highlighted in Figure
2, data are extracted from the legacy operational
systems (EHR data sources) and subsequently
cleaned-up and integrated in a data staging area
represented by an Operational Data Store (ODS).
Moreover, ETL (Extract, Transform, Load) tools
feed the data warehouse (and data marts) with
already integrated data based on a shared message
model that do not require transformation. This
makes it easier to extract the information from the
data source layer and load them in the data
warehouse for statistical purposes.
Figure 2: Data warehouse architecture proposed.
The source layer is represented by the set of
legacy systems and repositories (e.g. GP’s electronic
healthcare record, laboratory information systems,
radiology information systems) that manage
healthcare and administrative information related to
citizens. Identification of data sources represents a
critical process to be carried out for the success of a
data warehouse project. It is important to obtain
information about selected data sources identifying
the role played by each information system in the
development of the data warehouse and data marts.
Given that data collected in source information
systems are usually stored in different formats and
on a variety of platforms, it is necessary to define a
common data model that integrates data handled by
multiple sources into a single database. To achieve
this aim some authors have proposed to use a
module called wrapper (Roth and Schwarz, 1997),
that is responsible for data gathering from different
sources, data cleansing, format conversions as well
as data integration. Data managed by each wrapper
can therefore be loaded in the data warehouse and
thus in the relevant data mart. However, a change in
a data warehouse schema makes the revision of each
wrapper not straightforward. Therefore, it is
necessary to include in the architecture an
intermediate stage between the data sources and the
data warehouse tiers. This middleware system,
called ODS can also be used as a database for
operational processing, as proposed by Inmon
AClinicalDataWarehouseArchitecturebasedontheElectronicHealthcareRecordInfrastructure
289

(Inmon, 1999). It contains detailed and integrated
data with specific constraints including referential
integrity that ensures data accessibility by relevant
units. In the proposed architecture the ODS is
represented by two inter-related systems: a) the EHR
repository that contains individual’s structured
clinical documents together with the EHR registry
that manages metadata for indexing clinical
documents stored in relevant repositories; and b) the
Virtual Healthcare Record (VHR) that manages data
extracted from the documents contained in EHR
repositories, parsing the HL7 CDA document. The
integration of these systems is an appropriate
approach to define the ODS considering both
conceptual and operational point of views. Referring
to the first one, a common data model has already
been defined to ensure semantic interoperability
between heterogeneous legacy systems and the
EHR/VHR system based on the conceptual model
shown in Figure 1. This model comprises message
information models to exchange data about events,
health issues, episode of care, etc. as well as to
structure and share clinical documents produced in
each event. Considering the operational point of
view message exchange between legacy software
and EHR/VHR is based on a standard protocol
already implemented in some regional EHR
infrastructure. In particular, each source system has
installed a specific driver that extracts relevant
information from the proprietary database describing
the event happened (e.g. GPs visit) along with data
and documents provided already in HL7 CDA
format (e.g. drug prescription). The driver creates an
XML standard file that is then provided to a generic
wrapper that transforms it in a standardized HL7
message subsequently loaded in the EHR/VHR
system. In this way the specific driver installed in
each legacy system and the generic wrapper can be
seen as an ETL tool in the data warehouse
architecture. This makes it easier to integrate data
provided by different systems in the EHR/VHR and
thus in the data analytical process. The data
warehouse collects information stored in the
EHR/VHR in an OLAP (On-Line Analytical
Processing) approach that facilitates the integrated
analysis to develop specific dashboards based on
business processes and clinical indicators. Given that
VHR is composed by data extracted from clinical
documents, there is a need to develop a specific tool
that parses relevant information from EHR/VHR and
store them in the data warehouse. At this stage of the
design process an important role is played by the
Hierarchical Event Manager the InFSE module
responsible for a real-time notification of clinical
data and documents generated during each notified
event (Ciampi et al., 2012). This component can be
used not only to integrate different systems in the
EHR infrastructure, but also to feed the data
warehouse as well as the data marts. In particular,
this manager notifies users with events that occurred
and they are interested in, through a federation of
brokers operating on a publish-subscribe paradigm.
Of course other techniques are allowed to extract
data from the EHR and load them in the data
warehouse, in particular in case of frequent
monitoring of services. It is important to emphasize
that confidential information exchanged between the
ODS and the data warehouse must be anonymized to
preserve patient’s privacy. At this architectural level
clinical information managed by the EHR/VHR can
be also integrated with other data such as social,
demographic, economic, etc.
Finally, the analysis layer concerns tools and
techniques for data analysis, such as data mining,
reporting and OLAP tools. For instance, they can be
used to define a set of clinical indicators, as
highlighted in the following.
2.3 Dashboard
In order to identify a set of reliable indicators, in this
study the attention has been focused on the diabetes
mellitus type 2 pathology. This disease leads to
several extremely debilitating complications that can
impair the function of vital organs such as heart (e.g.
myocardial infarction), kidney (e.g. renal failure),
blood vessels (e.g. cardiovascular diseases, stroke)
and eyes (e.g. retinopathies). These health issues are
monitored in complex processes with frequent
contacts between patient and healthcare facilities
and professionals. This makes it necessary to timely
collect data and to foresee the verification of the
healthcare assistance processes in a regional and
national benchmarking framework. In Italy, a
comprehensive strategy for implementing a chronic
disease management intervention for people with
diabetes is defined in the IGEA project (Maggini,
2009). Within this project a set of clinical indicators
has been defined to measure the process, structure
and outcomes of patient care in order to assess a
particular clinical situation and to indicate whether
the healthcare delivered is appropriate. They are
used by different bodies at different levels to
identify areas of concerns, which might require
further review or development. Clinical indicators
are usually included in a benchmarked framework
comparing the outcome of each local agency over
different period of time with other agencies or with
HEALTHINF2014-InternationalConferenceonHealthInformatics
290
the literature results published, for instance, for other
populations or pathologies. In this paper the
attention is focused on this type of indicators that are
further divided into two categories: 1) process: to
assess whether a program is properly implemented
by the provider; 2) outcome: to measure the
program’s level of success in improving service
accessibility, utilization or quality. They capture the
effect of care processes on the health and wellbeing
of patients and populations. Outcome indicators are
intermediate if they reflect changes in biological
status or in life-style or final indicators if they assess
the incidence of new episodes, events or
comorbidity within a specific period of time.
Examples of clinical indicators are reported in Table
1 highlighting: 1) the type of indicator, 2) the source
class (based on the Figure 1 conceptual model), and
3) an example of the indicator based on the IGEA
project dashboard (Maggini, 2009). Moreover, for
each example the attribute to be taken into account
to extract the relevant information is reported.
Process indicators are assessed considering the
proportion of patients that have been treated in a
specified number of visits/controls/measurements
over the total number of diabetic patients involved in
the program. From the EHR/VHR point of view
these indicators can be measured considering on the
one hand the contact type (e.g. GP-patient encounter
to assess, for instance, the proportion of patients
who carried out at least two GP visits in one year)
and on the other hand a specific therapy used to treat
a patient’s health problem (e.g. proportion of
patients treated with antihypertensive drug).
Intermediate outcome indicators are assessed
considering the proportion of patients that have
values for a clinical parameter (e.g. micro
albuminuria, glycated hemoglobin, central arterial
pressure, weight) within a relevant threshold over
the total number of diabetic patients involved in the
program with at least one measure of that parameter.
This type of indicators is measured similarly to the
process indicators thus considering a specific
healthcare service (e.g. laboratory test) provided to
measure a metabolic parameter (e.g. glycated
hemoglobin). Another type of intermediate
indicators is related to the patient change in life style
(e.g. number of patients that has reduced the number
of cigarettes smoked during a day) and is assessed
considering the patient summary document
established and updated by the GP to snapshot, at a
specific time point, the health status of a patient with
a given pathology. Final outcome indicators are
measured considering the proportion of patients that
have suffered an event during a specific period of
time over the total number of patients who did not
suffer from the same event at the beginning of the
period.
Table 1: Examples of clinical indicators.
Indicator Concept / Class Example
Process indicators
Services
accessibility
HCService
Proportion of patients with at least two GP visits in a year
HCService.Type: GP visit
Treatment of
medical condition
HCService
Proportion of patients treated with antihypertensive drug
HCService.Type: Pharmacotherapy
Pharmacotherapy.Type: Antihypertensive drug
Intermediate outcome indicators
Services outcome
monitoring
HCService
Laboratory test
Proportion of patients whit hemoglobin < 7%
HCService.Type: LaboratoryTest
LaboratoryTest.Measure: Hemoglobin
Measure.Value: < 7%
Lifestyle behavior
changes
Document
Patient summary
Proportion of patients who reduced the number of cigarettes smoked
Document.Type: PatientSummary
PatientSummary.Entry: CigarettesSmoked
Entry.Value (to be compared over time)
Final outcome indicators
Services
accessibility
Episode of Care
HCService
Hospitalization
Proportion of patients hospitalized by episode category
HCService.Type: Hospitalization
EpisodeOfCare.Type
Episode of care
observation
Episode of Care
Incidence of proliferative diabetic retinopathy
EpisodeOfCare.Type: Diabetic retinopathy
AClinicalDataWarehouseArchitecturebasedontheElectronicHealthcareRecordInfrastructure
291
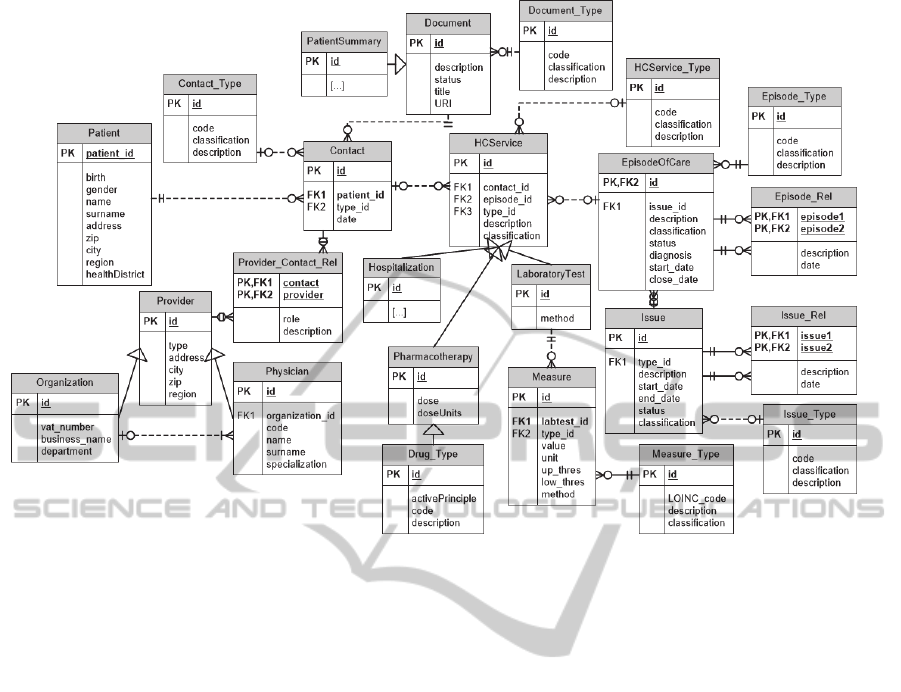
Figure 3: EHR high-level Entity Relationship diagram.
From the EHR/VHR point of view final outcome
indicators are mainly assessed considering two EHR
concepts: 1) the episode of care (e.g. incidence of
proliferative diabetic retinopathy) and 2) the
healthcare service (e.g. proportion of patients who
accessed the emergency room) that is usually
calculated considering the related disease (e.g.
episode of care classified using the ICD
classification).
2.4 Business Process Modelling
According to the dimensional modelling framework
the first step of the data warehouse design was to
identify the business processes to be modelled. In
this paper the attention is focused on the treatment of
medical condition to define process indicators, such
as the percentage of patients treated with
antihypertensive drug. This business process has
been used as a starting point to identify the main
tables and attributes to be used to design the high
level Entity Relationship (ER) diagram reported in
Figure 3. This diagram is based on the conceptual
model proposed in Figure 1 where essential concepts
are further identified, such as Patient who interacts
with the healthcare Provider that can be either an
Organization (e.g. the diabetologic centre) or a
Physician (e.g. the GP). Each Physician can also
belong to an Organization (e.g. the radiologist who
works in an hospital). Moreover, the HCService
describes the different activities performed during
each Contact. A HCService can be for instance a
Laboratory test or a Pharmacotherapy. Given a
portion of the ER schema needed to properly
describe the investigated business process the
attribute tree has been defined and afterward pruned
and grafted in order to remove the unnecessary
levels of detail such as, irrelevant attributes or
relationships (Figure 4). Starting from the attribute
tree a dimensional fact model was defined (Figure 5)
with the following characteristics: a) Fact table
(TreatmentIndex) is based on the atomic data
extracted from the structured clinical Document and
stored in the VHR that describe drugs delivered to a
patient to treat a specific episode of care; b) four
dimensions have been detected: Drug (type of
pharmacological product delivered by the
pharmacists to the patient, e.g. antihypertensive),
Patient, Date (when the drug has been delivered)
and District (where the drug has been provided to
the patient, i.e. the pharmacy district). To determine
costs attributable to a particular drug or treatment
and related to a specific episode of care the model
depicted in Figure 5 includes an additional
dimension (EpisodeOfCare) and two measures: the
quantity of product sold and the price for each unit
of product. These information are provided by the
Italian Medicines Agency (AIFA) that is the national
HEALTHINF2014-InternationalConferenceonHealthInformatics
292
authority responsible for drugs regulation in Italy.
Figure 4: Attribute tree after pruning and grafting.
Figure 5: Dimensional model based on service
accessibility and outcome monitoring business processes.
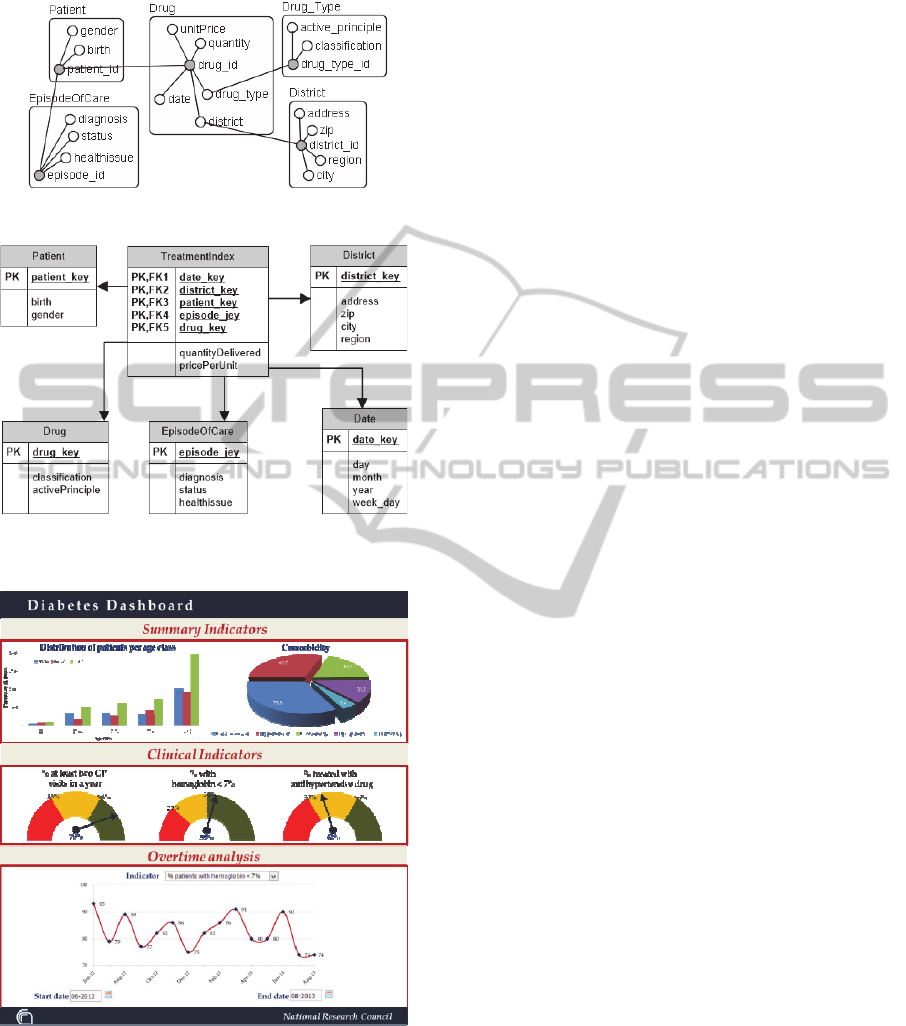
Figure 6: Diabetes dashboard displaying clinical indicators
based on the IGEA project (see paragraph 2.2).
A diagram picturing a hypothetical dashboard for
diabetes patients is reported in Figure 6. It provides
a snapshot of a set of clinical indicators to monitor
the effectiveness of healthcare service delivery in a
benchmarking framework.
3 CONCLUSIONS
In this paper we demonstrated the feasibility of
secondary uses of EHR to develop an enterprise data
warehouse architecture in a clinical governance
framework. To our knowledge this is a novel
approach that intends to exploit the entire EHR
infrastructure to develop a Business Intelligence tool
that supports the evaluation of healthcare activities
under different points of view. As shown in the case
study reported in this paper this approach can be
used for instance to benchmark local/national
healthcare services as well as to monitor the
effectiveness of applied guidelines. The EHR
represents the core of the proposed architecture as it
entails different advantages. First of all, it ensures
data quality using standardized data and documents
already integrated in a health infrastructure. In
particular, HL7 CDA used to exchange structured
clinical documents makes it easier to retrieve and
process atomic data that are usually coded using
international nomenclatures and dictionaries such as
ICPC (International Classification of Primary Care),
SNOMED (Systematized Nomenclature of Medicine
Clinical Terms) and ICD (International
Classification of Diseases). This also supports
semantic interoperability between different source
systems. Data are provided using a publish-subscribe
paradigm that guarantees health data to be promptly
exchanged at the moment an event is published, with
an automatic detection of relevant information
directly from source systems. This ensures a timely
and continuously updated information flow as well
as data integrity and consistency based on a sample
size that covers the entire target population.
Moreover, this approach makes it possible to
gradually integrate other applications within the data
warehouse infrastructure such as geographical or
socio-demographic information systems. EHR
represents the operational data store that guarantees
the separation between the transactional and the
analytical processing. The feasibility study described
in this paper will be implemented in a regional EHR
environment.
REFERENCES
Botsis T., Hartvigsen G., Chen F., Weng C., 2010.
Secondary use of EHR: data quality issues and
informatics opportunities. In AMIA Summits
Translational Science Proceedings pp. 1–5.
Ciampi M., De Pietro G., Esposito C., Sicuranza M.,
Donzelli P., 2012. On Federating Health Information
AClinicalDataWarehouseArchitecturebasedontheElectronicHealthcareRecordInfrastructure
293

Systems. In International Conference on Green and
Ubiquitous Technology (GUT), pp. 139-143.
Committee on Data Standards for Patient Safety, 2003.
Key Capabilities of an Electronic Health Record
System. Institute of Medicine Report 5.
Contenti M., Mercurio G., Ricci F.L., Serbanati L.D.,
2008. LuMiR: A Region-wide Virtual Healthcare
Record. In Proceeding of the 9th International HL7
Interoperability Conference. Crete, Greece. pp. 80-3.
De Mul, M., Alons, P., Van der Velde, P., Konings, I.,
Bakker, J., Hazelzet, J., 2012. Development of a
clinical data warehouse from an intensive care clinical
information system. Computer methods and programs
in biomedicine 105 (1) pp. 22-30.
Diomidous M., Zimeras S., Mantas J., 2009. Spatial
Electronic Health Record for the epidemiological
clinical data. Travel Health Informatics and Telehealth
1, pp. 66-72.
Dolin R. H., Alschuler L., Boyer S., Beebe C., Behlen F.
M., Biron P. V., Shvo A. S., 2006. HL7 clinical
document architecture, release 2. Journal of the
American Medical Informatics Association 13 (1) pp.
30-9.
EN 13940-1:2007 Health informatics - System of concepts
to support continuity of care - Part 1: Basic concepts.
CEN 2007. British Standards Institution.
Gillespie G., 2000. There’s gold in them thar’ databases.
Health Data Management 8 (11) pp. 40-52.
Hussain S., Ouagne D., Sadou E., Dart T., Jaulent M. C.,
De Vloed B., Daniel C., 2012. EHR4CR: A semantic
web based interoperability approach for reusing
electronic healthcare records in protocol feasibility
studies. In Proceedings of the 5th International
Workshop on Semantic Web Applications and Tools
for Life Sciences. Paris, France.
Inmon W., 1999. Building the Operational Data Store.
John Wiley & Sons. New York. 2
nd
edition.
Jensen P. B., Jensen L. J., Brunak S., 2012. Mining
electronic health records: towards better research
applications and clinical care. Nature Reviews
Genetics 13 (6) pp. 395-405.
Kamal J., Pasuparthi K., Rogers P., Buskirk J., Mekhjian
H., 2005. Using an information warehouse to screen
patients for clinical trials: a prototype. In Proceeding
of American Medical Informatics Association
Symposium. Washington DC, USA. pp. 1004.
Koh H. C., Tan G., 2011. Data mining applications in
healthcare. Journal of Healthcare Information
Management 19 (2) p. 65.
Kush R. D., Helton E., Rockhold F. W., Hardison C. D.,
2008. Electronic health records, medical research, and
the Tower of Babel. New England Journal of Medicine
358 pp. 1738–40.
Lurio J., Morrison F. P., Pichardo M., Berg R., Buck M.
D., Wu W., Calman N., 2010. Using electronic health
record alerts to provide public health situational
awareness to clinicians. Journal of the American
Medical Informatics Association 17 (2) pp. 217-9.
Maggini M., 2009. IGEA-A chronic disease management
project for people with diabetes. Annali Istituto
Superiore di sanità 45 pp. 349-352.
Mettler T., Rohner P., 2009. Supplier Relationship
Management: A Case Study in the Context of Health
Care. Journal of Theoretical and Applied Electronic
Commerce Research 4 pp. 58-71.
Oemig F., and Blobel B., 2005. Does HL7 Go towards an
architecture standard? Studies in Health Technology
and Informatics 116 pp. 761-6.
Roque F. S., Jensen P. B., Schmock H., Dalgaard M.,
Andreatta M., Hansen T., Søeby K., Bredkjær S., Juul
A., Werge T., Jensen L. J., Brunak S., 2011. Using
Electronic Patient Records to Discover Disease
Correlations and Stratify Patient Cohorts. PLoS
Computational Biology 7 (8), pp. 1-10.
Roth M. T., Schwarz P., 1997. Don’t scrap it, wrap it! a
wrapper architecture for legacy data sources. In
Proceeding of the Conference on Very Large Data
Bases (VLDB). Athens, Greece. pp. 266–275.
Safran C., Bloomrosen M., Hammond W. E., Labkoff S.,
Markel-Fox S., Tang P. C., Detmer D. E., 2007.
Toward a national framework for the secondary use of
health data: an American Medical Informatics
Association white paper. Journal of the American
Medical Informatics Association 14 (1) pp. 1-9.
Sahama T. R., Croll P. R., 2007. A data warehouse
architecture for clinical data warehousing. In
Proceedings of the fifth Australasian symposium on
ACSW frontiers 68. Ballarat, Victoria, Australia. pp.
227-32.
Schadow G., Mead C. N., Walker D. M., 2006. The HL7
reference information model under scrutiny. Studies
Health Technology Informatics 124 pp. 151–6.
Stow P. J., Hart G. K., Higlett T., George C., Herkes R.,
McWilliam D., Bellomo R., 2006. Development and
implementation of a high-quality clinical database: the
Australian and New Zealand Intensive Care Society
Adult Patient Database. Journal of Critical Care 21
(2) pp. 133-41.
Taylor P., 2008. When consent gets in the way. Nature
456 pp. 32–3.
Wang X., Hripcsak G., Markatou M., Friedman C., 2009.
Active Computerized Pharmacovigilance using
Natural Language Processing, Statistics, and
Electronic Health Records: a Feasibility Study.
Journal of the American Medical Informatics
Association 16 (3) pp. 328-37.
Wickramasinghe N., Schaffer J.L., 2006. Creating
knowledge-driven healthcare processes with the
intelligence continuum. International Journal of
Electronic Healthcare 2 (2) pp. 164-74.
Zhou X., Chen S., Liu B., Zhang R., Wang Y., Li P., Guo
Y., Zhang H., Gao Z., Yan X., 2010. Development of
traditional Chinese medicine clinical data warehouse
for medical knowledge discovery and decision
support. Artificial Intelligence in Medicine 48 (2) pp.
139-52.
HEALTHINF2014-InternationalConferenceonHealthInformatics
294
