
Partopens at the Point of Care
Evaluating Digital Pen-based Maternal Labor Monitoring in Kenya
Heather Underwood
1
, John Ong’ech
2
, Maya Appley
1
, Sara Rosenblum
1
, Addie Crawley
1
,
S. Revi Sterling
1
and John K. Bennett
1
1
ATLAS Institute, University of Colorado Boulder, Boulder, CO, U.S.A.
2
Kenyatta National Hospital, Nairobi, Kenya
Keywords: Digital Pens, Maternal Health, ICTD, Kenya, Partograph, Clinical Decision-Support System (CDSS).
Abstract: The goal of the PartoPen system is to enhance the partograph, a paper-based labor monitoring tool intended
to promote timely delivery of quality care by birth attendants in developing countries. The PartoPen digital
pen hardware and software system supports partograph use by providing audio instructions for measuring
and recording labor progress indicators, real-time decision support based on recorded measurements, and
time-based patient-specific reminders for taking measurements. Earlier work found the PartoPen system
effective in nursing classrooms at the University of Nairobi (UoN), Kenya where the PartoPen was used to
support teaching and training of students in maternal labor monitoring procedures. This paper presents the
results of several follow-on studies conducted in the maternity ward of Kenyatta National Hospital (KNH)
in Nairobi. Through these studies, we successively refine our understanding of the benefits of PartoPen use
in this setting. We also identify and discuss the interrelated factors impacting PartoPen adoption and use in
the labor ward at KNH, and review the challenges and opportunities likely to face digital pen deployments
in other healthcare settings.
1 INTRODUCTION
The World Health Organization (WHO) estimates
that 300,000 women die every year due to
pregnancy-related complications, most of which
occur in developing countries (World Health
Organization 2012). Timely and informed labor
monitoring by a skilled attendant can help prevent
many of the main causes of maternal death –
hemorrhage, infection, unsafe abortion, eclampsia,
and obstructed labor (United Nations 2010).
Globally, the WHO promotes the paper partograph
as an effective and cost-efficient tool for monitoring
labor, and preventing obstructed labor and resulting
complications. Used correctly, the partograph
provides decision support that assists in early
detection of maternal and fetal complications during
labor. Especially in rural clinics, early detection
allows transport decisions to be made in time for a
woman to reach a regional facility capable of
performing emergency obstetric procedures.
Despite the positive reports of improved
maternal outcomes resulting from correct partograph
use (Kwast et al. 1994; Mathai 2009; Lavender et al.
2013), several recent studies in Kenya have reported
underuse and incorrect use of the partograph at all
levels of maternity care (Opiah et al. 2012; Qureshi
et al. 2010; Lavender et al. 2011). The well-
documented barriers to partograph use include
partograph shortage, staff shortage, low partograph
knowledge and training, and the perspective that the
partograph is time consuming and redundant (Opiah
et al. 2012). The goal of the PartoPen project is to
mitigate some of the barriers preventing correct and
widespread partograph adoption using an interactive
digital pen, dedicated pen software, and partograph
forms printed with a background dot pattern that is
recognized by the pen. Using only the digital pen
and the existing paper form, the PartoPen addresses
training and resource barriers by providing audio-
based decision support, patient-specific reminders,
and partograph use instructions. Prior PartoPen work
at the University of Nairobi (Underwood, Sterling &
Bennett 2013b) suggests that the PartoPen is
effective in multiple healthcare settings: initial
training, training reinforcement, and use with actual
patients. These results motivated two of the studies
described in this paper. These studies focus on
90
Underwood H., Ong’ech J., Appley M., Rosenblum S., Crawley A., Sterling S. and K. Bennett J..
Partopens at the Point of Care - Evaluating Digital Pen-based Maternal Labor Monitoring in Kenya.
DOI: 10.5220/0004798600900100
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2014), pages 90-100
ISBN: 978-989-758-010-9
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

populations at two ends of the healthcare spectrum:
nursing students with little training or clinical
experience using the partograph, and nurse
midwives at KNH, who are well-trained and
generally have many years of experience using the
partograph in the labor ward.
Our previous work examined the effect of
PartoPen use on partograph completion in nursing
classrooms with third and fourth year nursing
students. The results of follow-on maternity ward
studies are presented here. In addition, we discuss
various environmental factors that led to different
outcomes in the two studies.
We first summarize the results from the PartoPen
nursing student study, and give an overview of the
technological components of the PartoPen system.
The remainder of the paper discusses the results of
maternity ward studies conducted at KNH in July
and August 2012, with follow-up in July 2013.
2 BACKGROUND
2.1 PartoPen Software System
Over the past fifty years, a large body of work on
pen-and-paper computing and pen-and-paper user
interfaces (PPUIs) has been developed. More
recently, digital pens have been used and evaluated
for usability and efficiency in the healthcare context
both by patients (Lind et al. 2007; Lind et al. 2008),
and by nurses (Procuniar & Murphy 2008; Estellat et
al. 2008). The key findings in these studies is that
digital pen technology is an intuitive and usable
technology with great potential, but healthcare-
specific digital pen applications must be designed to
meet the actual needs of the user. The Livescribe
(LS) digital pen technology (Livescribe Inc.) used
by the PartoPen system captures pen input and
digitizes paper content by using a unique location
tracking and page identification technique patented
by the Anoto AB group (Anoto).
The current implementation of the PartoPen
system uses the LS Echo digital pen running the
custom PartoPen software that allows the pen to
meaningfully interact with the paper partograph. The
Echo pen has a built in microphone, speaker, and
OLED display. The pen relies on a rechargeable
lithium ion battery, which is advertized to last about
36 hours during normal use. A battery life of 20 to
26 hours has been observed, depending upon the
amount of audio played during use. Pens can store
between 200 and 800 hours of audio, or the
equivalent amount of text data, depending on the pen
model, and all stored data can be downloaded to a
desktop computer using a standard micro-USB
cable.
One of the goals of the PartoPen system is to
enforce birth attendant training on correct use of the
partograph, as this has been cited as a significant
barrier to consistent use of the form. The WHO
partograph user manual, and a local partograph
manual issued to clinics by the Kenyan Ministry of
Health, are the primary resources for partograph
instruction in Kenya. The PartoPen system makes
the instructions found in these manuals accessible
directly from the partograph itself. The PartoPen
uses fixed print “button” regions around the
partograph text to provide verbatim audio recordings
of the instructions found in the partograph use
manuals. Thus, by tapping on these “buttons,”
nurses and nursing students can get short
informational prompts on how to use each section of
the form correctly.
One of the most commonly cited barriers to
partograph use is the inability to interpret the data
plotted on the partograph and take appropriate
action. Nursing students and less-experienced nurses
often plot the data correctly on the partograph, but
fail to derive the meaning of the plotted data, or do
not remember what actions to take based on the data
that they have plotted. The decision support
functionality of the PartoPen addresses these issues
by interpreting plotted data based upon page
location, and providing real-time feedback on the
appropriate actions to take. Currently, the PartoPen
provides decision support in three of the partograph
sections: cervical dilation, liquor/amniotic fluid, and
fetal heart rate.
The labor ward at KNH delivers approximately
1000 babies during the “busy” months from October
to March, or roughly 34 babies every day. On
average there are 4-6 nurses working at a time, and
based on survey data collected at the end of the
PartoPen study, nurses on average are responsible
for 5-7 patients during a day shift and 7-10 patients
during a night shift. The WHO recommends a
maximum ratio of one nurse to three patients to
ensure compliance with partograph completion
protocols. In the survey, nurses nearly unanimously
reported that staff shortage is the most common
reason for low partograph completion rates. While
the PartoPen does not replace nurses or supplement
the shortage of nurses in the labor ward, it does
provide a reminder system intended to help busy and
tired nurses keep track of when patients need
measurements taken.
PartopensatthePointofCare-EvaluatingDigitalPen-basedMaternalLaborMonitoringinKenya
91

2.2 PartoPen Nursing Student Study
Ninety-five nursing students in their third and fourth
years of study at the UoN School of Nursing
Sciences participated in the study. Students were
asked to complete a partograph worksheet, which
consisted of two patient case studies and two blank
partograph forms printed with the dot pattern. The
students recorded the patient data on the blank
partograph forms as if they were actively monitoring
that patient during labor. In each worksheet, students
received two of three possible patient case studies.
The three case studies represent three possible labor
outcomes. Mrs. A’s data represents an
uncomplicated, timely labor that progresses without
medical intervention. Mrs. B’s data illustrates a case
of prolonged or obstructed labor. Mrs. C’s labor
progression data illustrates an increasing number of
complications, including fetal distress, and
ultimately results in a cesarean section.
The students were first divided into three groups.
Group 1 was the control group, and Groups 2 and 3
were the intervention groups. Group 1 students
completed a partograph worksheet task with a
PartoPen in “silent logging mode,” and received no
instructions on how to use the technology. Group 2
completed the same worksheet task, but used a fully
functional PartoPen in “use” mode. The PartoPen
software in “use” mode for the student pilot has two
main components: instructions and decision support.
Group 2 received no training on how to use the
technology. Group 3 received a fully functional
PartoPen in “use” mode and a 15-minute
introduction and demonstration of the PartoPen
system before completing the partograph worksheet
task.
Using an unpaired t-test, the difference between
Group 1 (M=.520, SD=.141) and Group 3 (M=.722,
SD=.089) for the patient case study Mrs. C, a
prolonged labor resulting in a CS, was found to be
significant; t(8)=2.709, p=0.0267. These data
suggest that for more challenging or complex labor
cases, the availability and utilization of the PartoPen
instruction prompts promotes more accurate form
completion.
After each group completed the worksheet task,
students were asked to participate in a short focus
group session. Students unanimously reported that
plotting contractions was one of the most difficult
sections of the partograph, because both duration
and frequency are plotted together using a
combination of bar charts and coloring patterns.
Students also reported unanimously that plotting
descent of the fetal head was particularly
challenging. Difficulties plotting descent of the fetal
head can also be attributed to having to plot on the
same graph as another measurement (cervical
dilation), but may also be due in part to the nursing
school transitioning to a different partograph version
that requires users to plot the descent in increments
of one instead of two, and on the left side of the
graph instead of the right.
The completion results of the ‘contractions’
section of the partograph show improvements in all
three case studies (Mrs. A, B, and C) between
groups that did and did not use the PartoPen. There
was a statistically significant improvement in
contraction plotting on the Mrs. C case study
between Group 1 (M=.513, SD, .232) and Group 3
(M=.803, SD=.139); t(8)=2.399, p=0.0433.
‘Descent of fetal head’ measurements also
showed a significant improvement on the Mrs. C
case study between Group 1 (M=.337, SD=.152) and
Group 2 (M=.585, SD=.162); t(10)=2.699,
p=0.0223.In addition, there was a very significant
improvement on descent plotting on the Mrs. C case
study between Group1 and Group 3 (M=.705,
SD=.137); t(8)=4.028, p=0.0038.
The UoN PartoPen study indicated that PartoPen
use in classrooms can improve students’ ability to
correctly complete a partograph form. The study
results also suggest that significant PartoPen training
is not required to achieve these benefits. A
significant increase in partograph completion and
accuracy was observed with minimal prior training,
due to the intuitive design, push-based functionality,
and the enhancement – rather than replacement – of
the current paper-based system.
3 MATERNITY WARD STUDY
The follow-on PartoPen studies in the maternity
ward at KNH examined the impact of the digital pen
software system on partograph completion by nurse-
midwives monitoring patients during actual labor.
The partograph used in this study is pictured in
Appendix A. The first study was conducted in July-
August of 2012 at Kenyatta National Hospital. The
study was designed as a pre- and post study, which
compared partograph completion rates for
partographs completed in June (without the PartoPen
system) and in August when the PartoPen system
was in use by nurses.
3.1 Methodology
Currently KNH evaluates partograph completion
HEALTHINF2014-InternationalConferenceonHealthInformatics
92

using a rubric with four options – “complete,”
“incomplete,” “correct,” or “incorrect” – boxes for
each partograph category (fetal heart rate, moulding,
cervical dilation, etc.) Due to the wide range of
variation in how partographs are used and
completed, this basic evaluation rubric does not
correctly capture the actual completeness of the
partograph, or the real usefulness the data recorded
on the partograph. We therefore created a new rubric
that would better assess these measures. This rubric
is built upon the basic tenants of the evaluation tool
used by KNH. The rubric has grading criteria for
each partograph category, including a separate set of
grading criteria for the labor summary printed at the
bottom of each partograph. For each partograph
category there are three grading criteria: (1)
measurements recorded, (2) symbols correct, and (3)
spacing correct. The total possible value for each of
these grading criteria is determined by the time
between patient admission and delivery.
Previous efforts to evaluate partograph
completion required researchers to continuously
observe nurses during labor monitoring to assess
partograph completion (Rotich et al. 2011), or
researchers were required to use a coarse-grained
categorization scheme similar to the original KNH
rubric (Khonje 2012).
The new rubric also has some limitations. Chief
among these is the fact that the time of admission is
used to determine how many measurements are
expected on the partograph form. The time of
admission, however, does not always accurately
reflect when the woman went into active labor or
when the partograph was started.
All of the partographs collected during the study
were first categorized by delivery mechanism –
spontaneous vaginal delivery (SVD) and cesarean
section (CS). The CS deliveries were further
categorized into emergency CS (EmCS) and “other”,
which includes voluntary CS and CS due to previous
CS scars. Deliveries of twins, triplets, or deliveries
lasting less than one hour were noted among the
SVD partographs, but not included in the data
analysis because partographs a) are not designed to
monitor multiple births, and b) do not provide
beneficial monitoring for labors that are less than
one hour in length.
3.2 Quantitative Results
Initially all of the collected partographs from June
(369) were compared to all of the collected
partographs from August (457). This blanket
analysis of partograph completion rates between
June and August attempted to capture any broad
improvements that may have occurred due to
researcher presence, or a general increase in interest
and attention to the partograph because of the
PartoPen study taking place. These results are
captured in a previous paper (Underwood, Sterling
& Bennett 2013a), and briefly summarized below.
3.2.1 Phase 1 Data Analysis Summary
In the initial data analysis process, the collected
partographs were graded and checked by two pairs
of research assistants according to the new
evaluation rubric. Each partograph received two
scores: a composite completion score and a
summary score. The composite score was calculated
by dividing the number of points received by the
total number of points possible for all three grading
criteria (mark existence, correct mark symbol, and
correct mark spacing) for each partograph section
(fetal heart rate, cervical dilation, etc.). The
summary score reflects the completion percentage
for the partograph summary section at the bottom of
the form, which summarizes the labor (and is usually
completed after a patient delivers).
Based on this initial analysis, there were no
statistically significant improvements in the
composite scores between June and August
partographs. However, there were improvements in
the summary scores for both SVDs and CSs. This
result can be attributed to several possible factors.
First, the partographs used in June were slanted and
blurred due to frequent photocopying, whereas the
partographs used in August were printed
individually (to assure the unique dot pattern on
each form). This made the August partographs
significantly easier to read and, presumably easier to
complete. Second, the improvement in summary
scores was likely a result of the increased awareness
and underscored importance of the partograph that
occurred during the PartoPen study.
The lack of improvement in completion rates for
the overall composite partograph scores in the
presence of the increased focus on the partograph is
likely due to the impact of understaffing.
Understaffing thwarts completing the graphical
portion of the partograph because the ratio of nurses
to patients (often between 1:5 and 1:10) does not
allow for regular half-hour measurements to be
taken for each patient. The PartoPen system cannot
replace trained staff members, and does not directly
address the understaffing barrier to partograph
completion.
The data from the broad comparison of June and
PartopensatthePointofCare-EvaluatingDigitalPen-basedMaternalLaborMonitoringinKenya
93

August partographs suggest that the PartoPen does
not have an overall impact on partograph
completion, at least not in facilities like KNH, which
have highly trained and experienced, but critically
over-worked, staff.
3.2.3 Phase 2 Data Analysis
After the initial broad data analysis, a more fine-
grained analysis was performed on the PartoPen data
to ascertain if and how the PartoPen functionality
impacted partograph completion rates. Partographs
completed in June were compared to August
partographs that were actually completed with the
PartoPen. The PartoPen was used to complete 48 of
these partograph forms. PartoPens were only given
to nurses at KNH during the study, which excluded
the nursing students who were actively working in
the labor ward as part of their clinical rotation.
Student-completed partographs in August, which
were not completed with a PartoPen, were excluded
from Phase 2 analysis. In addition, many
partographs were only partially completed with the
PartoPen, due to nurse rotations and patient
handoffs. These partially completed partographs
were also excluded from Phase 2 analysis.
The comparison of all the partographs completed
with PartoPens versus the August partographs not
completed with the PartoPens versus all of the June
partographs is represented in the Figure 1. This
histogram illustrates that August partographs
completed with the PartoPens never received a
completion score lower that 25%, whereas both June
and August partographs completed without the
PartoPen did. Additionally, the August partographs
completed with the PartoPen had the highest
Figure 1: A histogram of partograph completion scores for
August partographs completed with a PartoPen, August
partographs not completed with a PartoPen, and June
partographs.
percentage of partographs in the 75-100%
completion range.
4 2013 FOLLOW-UP STUDY
At the conclusion of the PartoPen maternity ward
study, the nurses and hospital staff had successfully
incorporated the PartoPen system into the daily
operations of the labor ward. The system in place at
KNH at the end of the study included 20 PartoPens,
a printer capable of printing the dot pattern
partographs, PartoPen chargers, and extra pen caps
and ink replacements. Nine months after the
completion of the 2012 PartoPen maternity ward
study, a follow-up study was conducted with KNH
nurses to assess the performance and impact of the
PartoPen system.
Upon returning to the KNH labor ward in May
2013, researchers found that all 20 of the PartoPens
were accounted for, 19 out of the 20 PartoPen were
functional, and over 600 digital partograph records
were present on the PartoPens ranging from
September 2012 to April of 2013 (the printer used to
print dot-patterned partographs failed in April 2013,
and replacement parts were not readily available in
Nairobi). During the May 2013 visit, PartoPen
researchers identified a local printer model
alternative and worked with hospital IT staff to
establish a recurring printer toner order, so as to
remove this responsibility from the already busy
nurses and record-office staff in the labor ward.
4.1 Methodology
During the May 2013 visit, PartoPen researchers
surveyed KNH labor ward nurses regarding their
impressions of PartoPen deployment and use.
Twenty-six nurses completed a paper survey about
the PartoPen and its affect on labor ward operations
and patient care.
The paper survey consisted of nine questions
(see Appendix B); four YES/NO questions, two
Likert scale questions, and three free response
questions. The survey also included basic
demographic information, and a rank-order question
where nurses ranked the importance of the
partograph sections. The surveys were completed
during morning patient handoff. Nurses took an
average of 15 minutes to complete the survey, and
the nurses were not compensated for their time.
HEALTHINF2014-InternationalConferenceonHealthInformatics
94

4.2 Follow-up Survey Results
Thirteen of the 26 nurses who completed the survey
felt they were ‘experts’ using the PartoPen system.
The majority of the nurses (19 out of 26) used some
combination of partograph information and other
patient information to make decisions about patient
care. The nurses were asked to rank in order of
importance the different sections of the partograph
as they relate to providing quality patient care. Nine
nurses ranked patient name and age as the most
important section of the partograph to complete.
Eight nurses ranked fetal heart rate as the most
important section of the partograph, and seven
nurses ranked the partograph sections sequentially
(i.e., the most important section is the topmost
section of the form, and the least important is the
bottommost portion of the form). One nurse ranked
contraction frequency as the most important, and
one nurse ranked cervical dilation as the most
important section of the partograph to complete. The
responses from the survey suggest that certain
information on the partograph is more useful for
making critical decisions about patient care, which
may indicate that a simplified and restructured form
that highlights these sections (and makes them easier
to complete) could be useful in this setting. Nurses
largely prioritized patient information and fetal heart
rate as the most important portions of the form. In
the PartoPen study, some of the qualitative feedback
received by nurses indicated that using larger boxes
for information entry for these sections considerably
improved the usability and readability of these
critical pieces of information.
The survey also asked nurses to identify if there
are certain kinds of labor or patients who do not
need a partograph. Twenty of the 26 nurses said that
there were patients who do not need a partograph
during labor. Elective cesarean sections, false labors,
and patients who arrive already in the second stage
of labor were the most common responses for labors
that do not require a partograph to monitor labor
progress. Elective cesarean sections are scheduled in
advance and are categorized separately from
emergency C-sections that happen as a result of
complications during labor. Additionally, Kenyatta
National Hospital, as the leading referral hospital,
receives a very high volume of patients who are in
the second stage of labor. Although KNH
administrative policies require that a partograph be
used during all labors without exception, staff
shortages make prioritization necessary when
deciding to begin or continue a partograph for a
patient. Since KNH is a referral hospital, many
patients arrive late in labor in poor condition, and
completing paperwork or a partograph is not the
highest priority of hospital staff. The result is blank
or retroactively completed partographs.
Nurses were also asked to identify patients and
labor types that benefit the most from being
monitored with a partograph. Nurses were allowed
to circle more than one labor type out of SVD, CS,
IUFD, Referral, and ‘Other’. Twenty-three out of 26
nurses said that spontaneous vaginal deliveries
(SVD), which are often categorized as ‘normal’
labors, benefit the most from correct partograph use.
Eleven out of 26 nurses circled CS, emergency
cesarean sections, as benefiting the most from
partograph use, and 7 out of 26 nurses circled
‘Referral’.
The survey asked several PartoPen-specific
questions, including whether the nurses had
observed any changes in the labor ward because of
the PartoPen. This question was included in the
survey to follow up on qualitative observations and
discussions at the end of the 2012 studies that
suggested labor ward nurses were feeling an
increased sense of pride in their job because of the
interest of senior hospital staff, and reliance on labor
ward nurses to explain the project and demonstrate
its functionality. Additionally, only labor ward
nurses were given PartoPens, and this sense of
privilege was mentioned several times by nurses as
rewarding. Twenty-four of the 26 nurses said ‘yes’,
there had been changes in the labor ward because of
the PartoPen. The majority of the changes nurses
described related to the reminder functionality of the
PartoPen. Nurses frequently noted the reminders
being effective for providing more timely care and
making patient care more efficient. Better decisions
and easier chart interpretation were also noted as
significant changes resulting from PartoPen use in
the labor ward.
4.3 Secondary Data Analysis
Based on the data from the 2013 surveys, the data
from the 2012 maternity ward study was re-
examined, as follows: First, only the SVD
partographs were included, as the majority of nurses
indicated that SVD patients benefit most from
partograph use. In addition, partograph sections that
nurses deemed most important (i.e., (patient
information and fetal heart rate) were examined
individually.
The SVD partographs were analyzed in three
categories: August SVDs completed with the
PartoPens, August SVDs completed without the
PartopensatthePointofCare-EvaluatingDigitalPen-basedMaternalLaborMonitoringinKenya
95

PartoPens, and all of the SVDs from June. Using the
same grading and evaluation rubric, these
partographs were analyzed with respect to
completion. The results of this analysis are shown in
Figure 2. Frequency in this histogram is represented
as a percentage of the total number of partographs
present in the sample (37 August partographs
completed with the PartoPens, 206 August
partographs completed without the PartoPens, and
153 partographs completed in June). The histogram
illustrates that August partographs completed with
the PartoPens never received below 25%
completion, and this set had the highest percentage
of partographs in the 75-100% range.
The same set of SVD partographs was then
analyzed, looking specifically at the completion of
the ‘patient information’ and ‘fetal heart rate’
sections. While fetal heart rate completion did not
change significantly between the three groups, a
significant difference was observed in patient
information completion between August PartoPen
SVDs (M=.949, SD=.086) and June SVDs (M=.882,
SD=.152) using a paired t-test (t(188)=2.6178,
p=.0096). This difference may be attributable to
several factors, including the improved readability
and larger space for the patient information fields on
the PartoPen version of the partograph form.
Figure 2: A histogram of SVD-only partograph
completion scores (for August partographs completed with
a PartoPen for spontaneous vaginal deliveries only,
August partographs completed without a PartoPen for
SVDs only, and June partographs for SVDs only).
5 DISCUSSION
The results from the maternity ward studies do not
generally exhibit significant differences in
partograph completion rates between partographs
completed with the PartoPens and those not
completed with the PartoPens. In retrospect, this
result is not surprising. The PartoPen system was
designed to address training barriers that have been
cited as significant obstacles to correct partograph
use. However, the PartoPen system was deployed at
Kenyatta National Hospital, one of the leading
training and teaching facilities in Kenya. KNH has a
highly trained and knowledgeable staff who are less
likely to benefit from the training re-enforcement
aspects of PartoPen use. The other cited barriers to
partograph use, including staff shortages and lack of
supplies, are not directly addressed by the PartoPen
system, thus at KNH, any training reinforcement
benefit the PartoPen provided was overshadowed by
other barriers.
The positive results in the nursing student study
demonstrate that the PartoPen is beneficial for
partograph training for less-trained staff or for
students learning how to use the partograph. In a
controlled environment like a classroom where the
primary focus is on the task of completing a form
rather than delivering a baby, the PartoPen’s training
reinforcement and decision-support functionality are
fully utilized. In the chaotic and understaffed
environment of the labor ward at KNH, the primary
focus is on patients, not on paperwork, thus the
design objectives of the PartoPen system did not
align well with the primary focus of the KNH
nurses.
The next iteration of the PartoPen project will be
deployment at more rural and local levels of
maternity care, where nurse training, rather than
staff numbers and supplies, is the more problematic
issue. The primary contributions of the PartoPen
study in the maternity ward at KNH include nurses’
reflections on PartoPen usability, nurses’
perceptions of useful versus complete partographs,
and initial data on the durability and infrastructure
requirements of the PartoPen system, which can be
used in future deployments of the platform in other
labor wards.
From interviews with the nurses and researcher
observations, the reminders issued by the PartoPen
had the most impact on nurse behavior, although this
impact did not translate into increased partograph
completion, for the reasons described below. The
partograph used in the study was supplemented with
PartoPen Reminder ID boxes at the very bottom of
the form. Nurses were instructed to use these boxes
to record a memorable patient code, such as a
patient’s initials or the room number where the
patient was located. This patient code would be
displayed on the OLED display on the PartoPen
when the reminder for that patient sounded. The goal
HEALTHINF2014-InternationalConferenceonHealthInformatics
96

of the reminder system was to ensure timely patient
checkups by nurses who are busy, distracted, or
simply have forgotten to check on one of their many
patients. However, when the ratio of nurses to
patients is between 1:7 and 1:10, even if a nurse has
correctly recorded a patient code and receives the
patient’s reminders, she may be assisting with
another labor, checking on another patient, etc.
Many of the nurses reported receiving the reminders
but being unable to act on them because they were
already involved with a different patient.
Additionally, the design of the system was not as
helpful to nurses who had their hands busy, as the
patient code was displayed textually on the screen,
and nurses were often unable to stop what they were
doing to look at the pen and read the patient
reminder ID.
6 CONCLUSIONS
The initial objective of the PartoPen maternity ward
studies was to examine the impact of digital pen
technology on partograph completion. This
objective assumed that a primary barrier to
partograph completion was a lack of training and
knowledge on how to complete and interpret the
form. However, the highly skilled staff at KNH did
not lack in training or knowledge, but rather,
suffered from staff and resource shortages, which
the PartoPen was not designed to address. Despite
the disparity between the study goals and observed
study site realities, several important observations
were made that may contribute to future work in this
area.
First, every clinic or hospital has a unique set of
problems, personnel and procedures, which have to
be identified and addressed during both study design
and implementation. The PartoPen maternity ward
study design did not adequately account for the
myriad confounding factors present at KNH,
including under-staffing issues, different birth rates
between months compared, and the presence of
(different groups of) nursing students in the labor
ward during the intervention month, but not the
control month. Unlike the PartoPen nursing student
study design, the maternity ward study was not
designed such that only the affect of the PartoPens
on partograph completion could be measured. In one
analysis, study results were evaluated assuming an
experimental study where nurses were given the
intervention (the PartoPen) and the nursing students
present in the labor ward were the controls. This was
not the ideal study design, as the experimental and
control groups were not well matched in terms of
training, background, or experience. A more
appropriate study design for this environment would
be a paired comparison of individual nurses’
performance on partographs for similar labor types
with and without the PartoPen during comparably
busy shifts.
The study design that was used – a combination
of qualitative and quantitative data collection –
illustrates a disparity between the data from nurse
surveys and research observation and the data from
the partograph completion evaluation. When
surveyed, all of the nurses reported that they
considered partograph information to be important,
and that they relied upon this information.
Interviews with nurses also revealed that nurses
considered the partograph is an essential tool in the
labor ward. However, the low partograph
completion scores, regardless of the PartoPen
intervention, suggest that the partograph was often
under-utilized, filed out retroactively, or filled out
incompletely. This result is not indicative of a lack
of diligence or aptitude, rather a lack of adequate
staffing. Thus, partograph completion rates should
not be routinely equated with quality of care,
particularly at a short-staffed referral facility. It
would therefore be premature to promote the
partograph universally without conducting large-
scale studies on the direct association between
partograph use and maternal and child outcomes,
which account for environmental and social
circumstances unique to the study site.
Second, health informatics interventions,
especially in developing countries, are often
consumed by the technological aspects of the
project. We sometimes fail to recognize the benefit
of addressing immediate and simple issues, which
do not necessarily require technological
intervention. The qualitative feedback received by
nurses indicated that the cleaner PartoPen form with
larger boxes for information entry considerably
improved the usability and readability of the form.
The cleaner form was simple to produce within the
existing workflow and with existing equipment, and
could have been done independently of the PartoPen
project.
Finally, the PartoPens deployed at KNH were
successfully used and sustained for over nine-
months of continuous hospital use. This illustrates
the robustness of the system, as well as a willingness
among nurses to use the PartoPens on a daily basis.
The PartoPen maternity ward study helped identify
the environmental and physical challenges present in
the KNH labor ward, and illustrated both the
PartopensatthePointofCare-EvaluatingDigitalPen-basedMaternalLaborMonitoringinKenya
97

challenges and opportunities that arise when
deploying a digital pen software system in a
maternity ward setting. The results of this study are
encouraging for the continued and expanded use of
digital pen systems in healthcare, and stress the need
for more in-depth and well-designed studies in this
area.
ACKNOWLEDGEMENTS
We would like to express our sincere appreciation to
the staff and nurse-midwives at Kenyatta National
Hospital, without whose support and participation
this work would not have been possible. This
research was funded in part by the ATLAS Institute
at the University of Colorado Boulder, a National
Science Foundation Graduate Research Fellowship,
and a Bill and Melinda Gates Foundation Grand
Challenges Exploration Grant (OPP1061309).
REFERENCES
Anoto, Anoto Products. Available at: http://anoto.com
(Accessed September 26, 2013).
Estellat, C. et al., 2008. Data capture by digital pen in
clinical trials: A qualitative and quantitative study.
Contemporary Clinical Trials, 29(3), pp.314–323.
Khonje, M., 2012. Use and documentation of Partograph
in urban hospitals in Lilongwe - Malawi: Health
workers perspective.
Kwast, B. E., Lennox, C. E. & Farley, T. M. M. 1994.
World Health Organization partograph in management
of labor. Lancet, 343, pp.1399–1404.
Lavender, T. et al., 2011. Students’ experiences of using
the partograph in Kenyan labor wards. African Journal
of Midwifery and Womens Health, 5(3), pp.117–122.
Lavender, T., Hart, A. & Smyth, R.M.D., 2013. Effect of
partogram use on outcomes for women in spontaneous
labor at term. The Cochrane database of systematic
reviews.
Lind, L., Karlsson, D. & Fridlund, B., 2007. Digital pens
and pain diaries in palliative home health care:
professional caregivers' experiences. Medical
informatics and the Internet in medicine, 32(4),
pp.287–296.
Lind, L., Karlsson, D. & Fridlund, B., 2008. Patients' use
of digital pens for pain assessment in advanced
palliative home healthcare. International journal of
medical informatics, 77(2), pp.129–136.
Livescribe Inc., Livescribe Echo Smartpen Specs.
Available at: http://livescribe.com (Accessed
September 26, 2013).
Mathai, M., 2009. The partograph for the prevention of
obstructed labor. Clinical obstetrics and gynecology,
52(2), pp.256–269.
Opiah, M. M. et al., 2012. Knowledge and utilization of
the partograph among midwives in the Niger Delta
Region of Nigeria. African journal of reproductive
health, 16(1), pp.125–132.
Procuniar, M. & Murphy, S., 2008. Intuitive information
technology: enhancing clinician efficiency. AMIA
Annual Symposium proceedings / AMIA Symposium
pp.1247–1248.
Qureshi, Z. P., Sekadde-Kigondu, C. & Mutiso, S.M.,
2010. Rapid assessment of partograph utilisation in
selected maternity units in Kenya. East African
medical journal, 87(6), pp.235–241.
Rotich, E. et al., 2011. Evaluating partograph use at two
main referral hospitals in Kenya. African Journal of
Midwifery and Womens Health, 5(1), pp.21–24.
Underwood, H., Sterling, S.R. & Bennett, J., 2013a. The
PartoPen in Practice: Evaluating the Impact of Digital
Pen Technology on Maternal Health in Kenya.
ICTD'13 proceedings.
Underwood, H., Sterling, S.R. & Bennett, J., 2013b. The
PartoPen in Training and Clinical Use: Two
Preliminary Studies in Kenya. 6
th
International
Conference on Health Informatics/HealthINF2013
proceedings.
United Nations, 2010. The Millennium Development
Goals Report. pp.1–80.
World Health Organization, Maternal mortality. Available
at: http://www.who.int/mediacentre/factsheets/
fs348/en/ (Accessed September 26, 2013).
HEALTHINF2014-InternationalConferenceonHealthInformatics
98
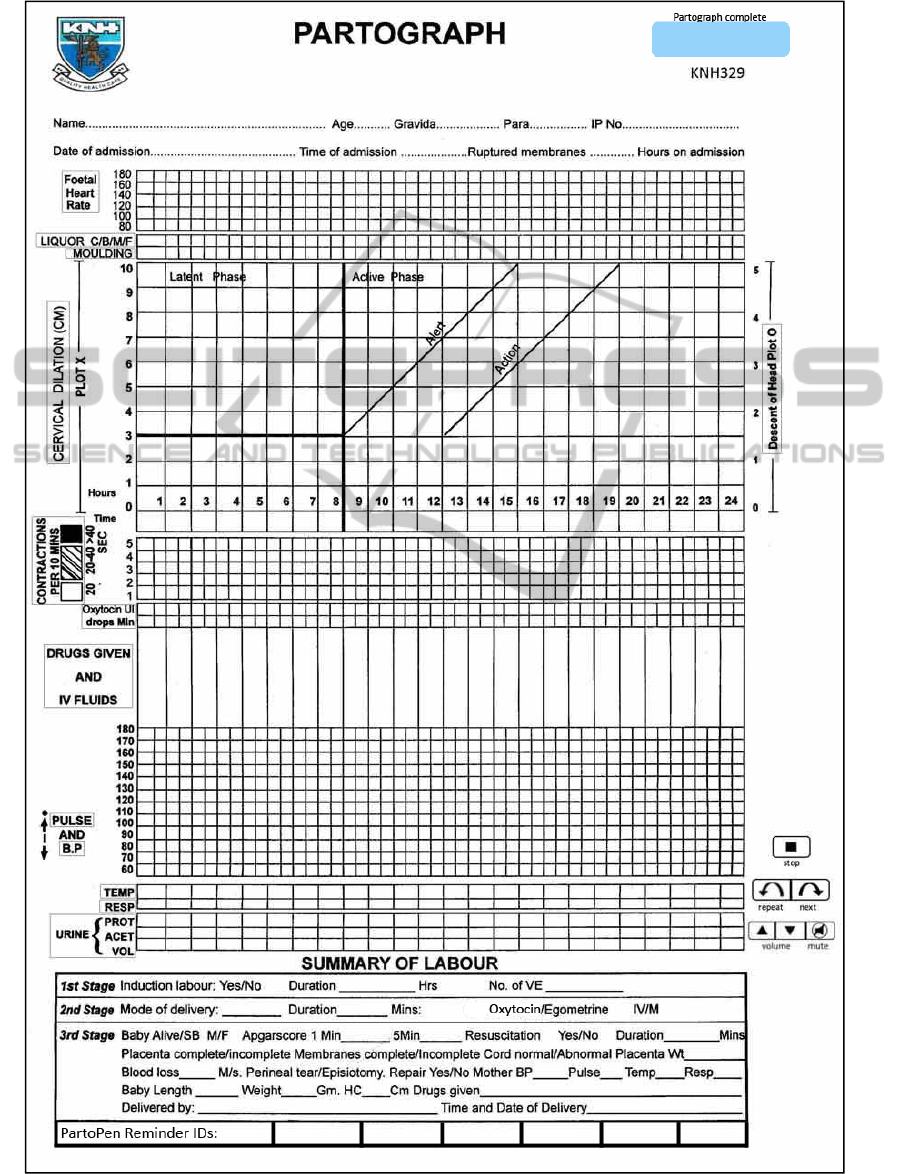
APPENDIX A
PartopensatthePointofCare-EvaluatingDigitalPen-basedMaternalLaborMonitoringinKenya
99

APPENDIX B
KNH PartoPen Study – Participant Survey – June 2013
Please provide answers for the following questions:
Age: __________ Gender: __________
1) Did you participate in the PartoPen study in July and August 2012? YES NO
2) What is your level of experience using the PartoPens? (circle a choice below)
1 2 3 4 5
No experience Expert
3) How much do you rely on the partograph to make decisions about patient care? (circle a choice below)
1 2 3 4 5
I don’t use partograph I only use partograph
information at all information
4) Please number the following partograph sections in order of importance from 1 to 24, where 1 is the first
thing you look at on a partograph to make patient care decisions, and 24 is the partograph section that
you need the least to feel confident making patient care decisions. (Partograph sections were listed
below in original survey, but space constraints prevents us from listing them here.)
5a) Are there certain patients that do not need a partograph? YES NO
5b) If yes, what type of patients do not need a partograph?
6a) What kind of labors/births benefit the most from correct partograph use? (circle all that apply)
SVD CS IUFD Referral Other?
6b) For the answers you circled in 6a, please explain why these types of births benefit the most from correct
partograph use.
7a) Have there been any changes in the labor ward because of the PartoPen? YES NO
7b) What are they? How did they affect you?
8a) Have there been any problems with the PartoPen? YES NO
8b) If yes, what are they? How did they affect you?
9) Now that you have used the PartoPens for several months, what would you like the next steps to be in the
project? (Please list any other comments about the PartoPen project here).
HEALTHINF2014-InternationalConferenceonHealthInformatics
100
