
Medical-treatment Recommendation and the Integration of Process
Models into Knowledge-based Systems
Laia Subirats
1,2
, Luigi Ceccaroni
1
, José María Maroto
3
, Carmen de Pablo
3
and Felip Miralles
1
1
Barcelona Digital Technology Centre, Roc Boronat, 117, 5th floor, 08018 Barcelona, Spain
2
Universitat Autònoma de Barcelona, Campus UAB, 08193 Bellaterra, Spain
3
Cardiac Rehabilitation Unit, Hospital Universitario Ramón y Cajal, 28034 Madrid, Spain
Keywords: Ontologies, Rule-based Reasoning, Cardiac Rehabilitation Processes, Clinical Decision Support Systems.
Abstract: Decision making based on evidence other than human reasoning is becoming increasingly important in
healthcare. Valuable evidence is in the form of treatment processes used by healthcare institutions and this
paper presents a new framework for representing and modeling knowledge from these processes.
Specifically, it presents the integration of data from literature, business processes and decision trees through
workflows that cover the full cycle of health care, from diagnosis to prognosis and treatment. With respect
to patient status, as single instants cannot convey sufficient information, time series are analyzed and
classified to improve decision-making ability. The elicitation of new knowledge takes into account
international standards, ontologies, information models, nomenclatures and multiple types of indicators. The
integration of formal process-modeling in knowledge-based systems is exemplified by a real-world
recommendation scenario. After evaluation with a medical-rehabilitation data set, results show a strong
correspondence between treatment recommended by the proposed system and clinical practice.
1 INTRODUCTION
In medical rehabilitation, to evolve from the current
situation to a more individualized one and to solve
interoperability problems, the involvement of all
stakeholders in the development of models for
rehabilitation processes is needed. Clinicians use
guidelines, workflows and experience in the form of
past cases.
Here, we focus the attention on the integration of
past cases and workflows as a valuable source of
implicit knowledge not previously recognized by
clinicians. Because workflows are often informally
described (e.g., in diagrammatic languages, such as
the business process modeling notation or the
unified modeling language activity diagram), they
cannot be automatically included into a
computational reasoning system, but need to go
through some sort of nontrivial formalization
process. For this, a variety of languages can be used,
viz. procedural languages (e.g., the business process
execution language) or highly-formal languages
(e.g., Petri nets). Existing knowledge, including case
libraries when a case-based reasoning (CBR)
system is used, constitutes the input source for
workflows, and the output data of these workflows
are then delivered back to knowledge containers as
well as case libraries.
Effective management of processes is critical to
the development as well as sustainment of
rehabilitation capabilities. In the context of this
paper, a process defines a description and ordering
of work activities across time and space that is
designed to yield specific results or services while
ensuring the rehabilitation's overall objectives. It
provides a conceptual basis for the integration and
coordination of distributed resources, tasks and
individuals (Cichocki et al., 1998).
Process models produced by healthcare experts
are represented as formal rules, providing a
framework that allows their semantic enrichment.
Whilst some progress in this direction has been
made in recent research (Jafarpour et al., 2011; Peek
et al., 2011 and Smith et al., 2012], the integration of
data from literature, business processes and decision
trees through workflows that cover the full cycle of
health care, from diagnosis to prognosis and
treatment, has not been presented before.
The rest of the paper is organized as follows.
Section 2 introduces a real-world scenario with 200
491
Subirats L., Ceccaroni L., María Maroto J., de Pablo C. and Miralles F..
Medical-treatment Recommendation and the Integration of Process Models into Knowledge-based Systems.
DOI: 10.5220/0004822004910498
In Proceedings of the 6th International Conference on Agents and Artificial Intelligence (ICAART-2014), pages 491-498
ISBN: 978-989-758-015-4
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

cases, which illustrates the complexity of the domain
at hand. Section 3 describes the methods and the
architecture of a reasoning system that provides
recommendation about personalized rehabilitation
therapy and prognosis. Section 4 presents the results
of the application of the recommendation system to
the real-world scenario. Finally, conclusions and
future work are drawn in Section 5.
2 SCENARIO
This study is based on the anonymized data of 200
patients who performed cardiac rehabilitation at the
Hospital Universitario Ramón y Cajal that is
summarized in Table 1.
The map of processes
performed in cardiac rehabilitation programs at the
Hospital Universitario Ramón y Cajal is described in
Calvo et al., (2013). We will consider, as
representative examples, the Walking and the
Relaxation sessions activities. Each activity is part
of a hierarchy; the Walking activity, for example, is
a subprocess of Motor rehabilitation, which is a
subprocess of Cardiac rehabilitation.
Let us consider a 50-year-old man from Spain
(the patient), who suffered an acute myocardial
infarction. (This refers to the condition when blood
supply to the heart is stopped. When the heart does
not get enough oxygen, heart muscles die or get
permanently damaged.) Now, two weeks after his
hospital discharge, he starts a cardiac rehabilitation
program. His initial evaluation shows he has some
risks factors, such as smoking and hypertension, and
some problems with his functional capacity,
measured in metabolic equivalent of task (MET).
His left ventricular ejection force is normal, and he
does not have problems with anxiety, depression,
dyslipidemia, sedentary lifestyle, diabetes, alcohol,
abdominal perimeter or body mass index. His
therapist wants to plan a personalized rehabilitation
process for him. The aim of the clinical decision
support system (CDSS), apart from providing him a
summary of his main indicators, is to provide her:
Personalization of the Treatment. It
provides a recommendation about the
personalization of a treatment, such as the
intensity of the Walking activity, if the
Relaxation activity should be performed.
Prognosis. The state of risk factors such as
hypertension and other indicators after
rehabilitation treatment can be predicted.
Therefore, his therapist, based on her knowledge
and experience, decides to prescribe the patient a
Cardiac rehabilitation process including the
Walking activity and the Relaxation activity. His
therapist documents her decision in the rehabilitation
platform which the CDSS is integrated to. The next
week, our patient starts the first rehabilitation
session of the Walking activity. The aim of the
CDSS in this stage of the rehabilitation process is to
personalize the session providing the therapist
support about when to stop it. Figures that
summarize the map of processes performed in the
cardiac rehabilitation scenario, the methodology and
the main structure of the ontology can be found at
https://code.google.com/p/cardiacrehabilitation/wiki/
Summary.
3 METHODOLOGY
The proposed rule-based framework is composed of
five components.
(1) An ontology, written in the ontology web
language (OWL) with rules implemented in the
semantic web rule language (SWRL). SWRL was
chosen because it is a de facto standard to extend
OWL and can be easily integrated in Protégé (the
editor used to define the ontology). Rules are
extracted from several sources with different levels
of interpretation: literature (requiring more
interpretation), business processes and decision trees
(requiring less interpretation):
Business Processes are modeled using business
process modeling notation 2.0 (BPMN). BPMN was
chosen for being a standard for business process
modeling. These rules are used to personalize a
session.
Literature rules can be extracted from Velasco
et al. (2009). These rules are used to provide
prognosis and to personalize a rehabilitation
treatment.
Decision Trees are obtained using Weka, a data
mining and machine learning software. Weka was
chosen for being a Java-based open source tool. The
J48 classifier is applied to the Hospital Universitario
Ramón y Cajal data set to obtain personalization of
psychotherapy and psychotropic therapy and predict
risk of hypertension, emotional functions and
exercise tolerance functions. Due to the limited
number of patients, only solutions which a certain
level of recall and precision set by the professional
are taken into account. These rules are used to
provide prognosis and to personalize a rehabilitation
treatment.
(2) A reasoner, Pellet, which infers properties
ICAART2014-InternationalConferenceonAgentsandArtificialIntelligence
492
and relationships from rules. Pellet was chosen
because it is an open-source Java OWL DL reasoner
with SWRL-support.
(3) A querying system, SPARQL Protocol and
RDF Query Language (SPARQL), to perform the
queries.
(4) A Java framework, Jena, to link with data
applications.
(5) A Java-based content management system
(CMS), Liferay, to provide an interface to interact
with users. The CMS includes the medical health
record (MHR) were data from patients is stored.
SPARQL, Jena and Liferay were chosen because
they are open-source Java-based systems.
This section includes a description of the
ontology’s structure and examples of rules and
queries.
3.1 Ontology
Data obtained from the MHR of the hospital are
expressed as virtual medical record (vMR) classes.
The vMR is an information model developed within
HL7, which is designed to solve interoperability
problems in the electronic exchange of clinical
information and to reduce development costs and
time responses in CDSSs that use it. The vMR is
used by the CDSS and stored in an ontology.
Evaluated Person (subclass of Person) contains
patient’s static information such as birth time and
sex. Problem is used to represent diseases, following
the ICD-10, such as myocardial infarction, chronic
rheumatic heart diseases, heart failure,
atherosclerosis, other peripheral vascular diseases
and congenital malformations of the circulatory
system. Observation Base (subclass of Observation)
is coded following the ICF and is used to represent
indicators, such as risk factors (e.g., tobacco,
hypertension, alcoholism, body mass index,
sedentarism, abdominal perimeter, arrhythmia,
creatinine, glucose), range of emotion, walking
activity, functional capacity, left ventricular ejection
fraction, state-trait anxiety inventory, Beck
depression inventory, and work situation. Data are
available in three instants of time: before disease,
before rehabilitation, and after rehabilitation. Goal is
used to represent the indicators whose value we
want to predict. Finally, General Knowledge is used
to represent the recommended therapeutic plan and
includes: (1) medical and surgical procedures, such
as surgical revascularization, valve prosthesis,
corrected congenital pathology, defibrillator
implantation, pacemaker implantation or
arrhythmias correction, (2) processes, such as
intense aerobic exercise, motor rehabilitation,
psychological rehabilitation, and (3) specific
activities, such as walking or psychotherapy.
These standard annotations of processes and result
indicators from biomedical ontologies and
terminologies (ICF, SNOMED CT, ICD-10 and
ICD-11) are used in a semantic, rule-based
framework.
3.2 Rules
Rules are extracted from literature, a fragment of
BPMN 2.0 and decision trees from classification
algorithms; needing different degrees of human
interpretation during the formalization process. In
Table 1: Summary of some attributes of the cardiac data set (SD = standard deviation).
Attribute: options (separated by /)
Values
# Missing
values
Gender: man / woman 163 / 37 0
Age [11, 78], Mean: 53, SD: 14.3 0
Left ventricular ejection fraction (LVEF) [0, 89], Mean: 35, SD: 29.4 35
METs before rehabilitation [2, 12], Mean: 7, SD: 2.3 57
Beck index before rehabilitation [0, 34], Mean: 8, SD: 6.2 35
Psychotherapy: yes / no 15 / 157 15
Psychotropic therapy: yes / no 6 / 166 28
Exercise tolerance after rehabilitation: no / mild / moderate
/ severe / complete deficiency
19 / 58 / 51 / 20 / 4 48
Emotional functions after rehabilitation: no / mild /
moderate / severe / complete deficiency
93 / 48 / 18 / 4 / 1 36
Hypertension risk after rehabilitation: low / medium / high 94 / 39 / 43 24
Medical-treatmentRecommendationandtheIntegrationofProcessModelsintoKnowledge-basedSystems
493

this section, rules to execute therapies, define
activities, execute activities and evaluate patients are
specified using SWRL. All rules are available at
[http://code.google.com/p/cardiacrehabilitation]; in
the following paragraphs a representative set of
examples is described in details.
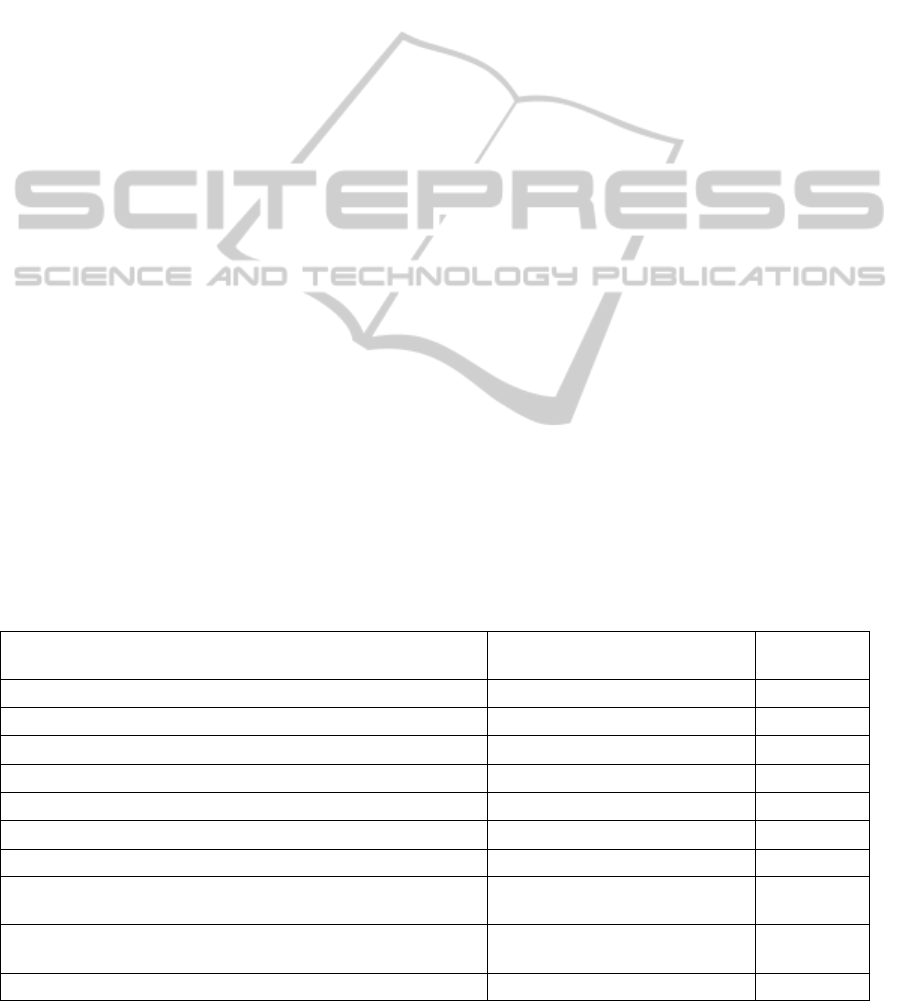
Rules from Rehabilitation Processes Written
in BPMN 2.0. In Fig. 1 it is modeled the Walking
activity as an example. The tasks carried out (by
different actors) in the Walking activity are: routine
personalization; time personalization; pulsometer
placement and heart rate measurement; warm up;
walk; cardiac frequency observation; cool down;
basal heart rate measurement; patient’s activity
evaluation. The core tasks of the Walking activity
consist of the three typical phases of a walking
physical exercise in an open environment outside of
a healthcare institution: Warm up, Walk and Cool
down, each of which has a predefined duration,
which can be respected or not by the patient. In the
Walking activity, three indicators are monitored and
their values are stored in a MHR. (1) Treatment-
result indicators, which are periodically quantified.
METs are extracted from an exercise testing is a
treatment-result indicator. (2) Process indicators are
execution, security or end-session. In this activity
heart rate is a process indicator. (3) Session
indicators to indicate the end of the session. In the
walking activity maximum heart rate, Borg score,
walked distance and walked time are session
indicators. As described in Section 1, decision
support is provided to the Walking activity in
prognosis and session’s personalization. The
walking activity ends when one of the following
conditions is reached in the patient’s evaluation if a
certain level of maximal oxygen consumption (VO
2
max); the maximum heart rate below a predefined
limit and the walked distance above a predefined
limit.
The Relaxation activity is included in
Psychological rehabilitation, which is a subprocess
of Cardiac rehabilitation. It is modeled in a similar
way as the Walking activity in Fig. 1. The tasks
performed in the Relaxation activity are: place the
patient, relaxation tasks and patient assessment. The
core tasks of the Relaxation activity consist of
inhaling, exhaling, muscle contraction and muscle
extensions. In the Relaxation activity, several
indicators are monitored and their values are stored
in a MHR. Treatment result-indicators are
occupational status and Beck depression inventory
(BDI); process indicators are depth of inhalation,
depth of exhalation and muscle activity; and activity
result-indicators are therapist visualization,
measuring tape, Borg scale and anxiety assessment.
As an example, let us consider rule (1), below,
which ends an activity if a process indicator is
greater than or equal to 2 (moderate deficiency).
ActivityEnd (?ae),
ProcessIndicator (?pi),
Patient (?p),
greaterThanOrEqual (?pi, 2),
hasIndicator (?p, ?pi)
hasNextTask (?p, ?ae) (1)
This codification means that, if a patient p has a
process indicator pi which is greater than or equal to
2, the activity is stopped and the next task is ae.
Similar rules are applied to several process
indicators of rehabilitation activities. Process
indicators are used to stop activities because of
severe alterations in body functions (such as a too
high heart rate) or in environmental factors (such as
a too high temperature or humidity).
Rules from Cardiac Rehabilitation Literature.
The risk of having another infarction after cardiac
rehabilitation is translated to rules using semantic
annotations. Problems appear when there are partial
matches in rules. To solve them, priorities among
attributes are established according to the proximity
to the root of the generated decision tree after
applying a classifier. These priorities are: disease,
tolerance to exercise, contraction force of ventricular
muscles and heart rhythm. A sample rule is (2),
which predicts that a person will have medium risk
of suffering a myocardial infarction, if a patient has
thallium stress test abnormal, a severe deficiency in
the treatment indicator of contraction force of
ventricular muscles and has suffered an angina
pectoris.
Patient (?p),
Thallium stress test abnormal (?th),
hasIndicator (?p, ?th),
Contraction force of ventricular muscles (?cfvm),
Deficiency (?severe),
hasDeficiency (?cfvm,?severe),
TreatmentIndicator (?ti),
hasType (?cfvm,?ti),
hasIndicator (?p, ?cfvm),
Angina Pectoris (?ap),
hasDisease (?p, ?ap),
Risk (?mediumRisk)
hasRisk (?p, ?mediumRisk) (2)
Rules from Decision Trees. The J48 classifier
from Weka is applied on data sets about
psychotherapy, psychotropic therapy, risk of
hypertension and prognosis of emotional functions
and exercise tolerance functions; and rules are
ICAART2014-InternationalConferenceonAgentsandArtificialIntelligence
494
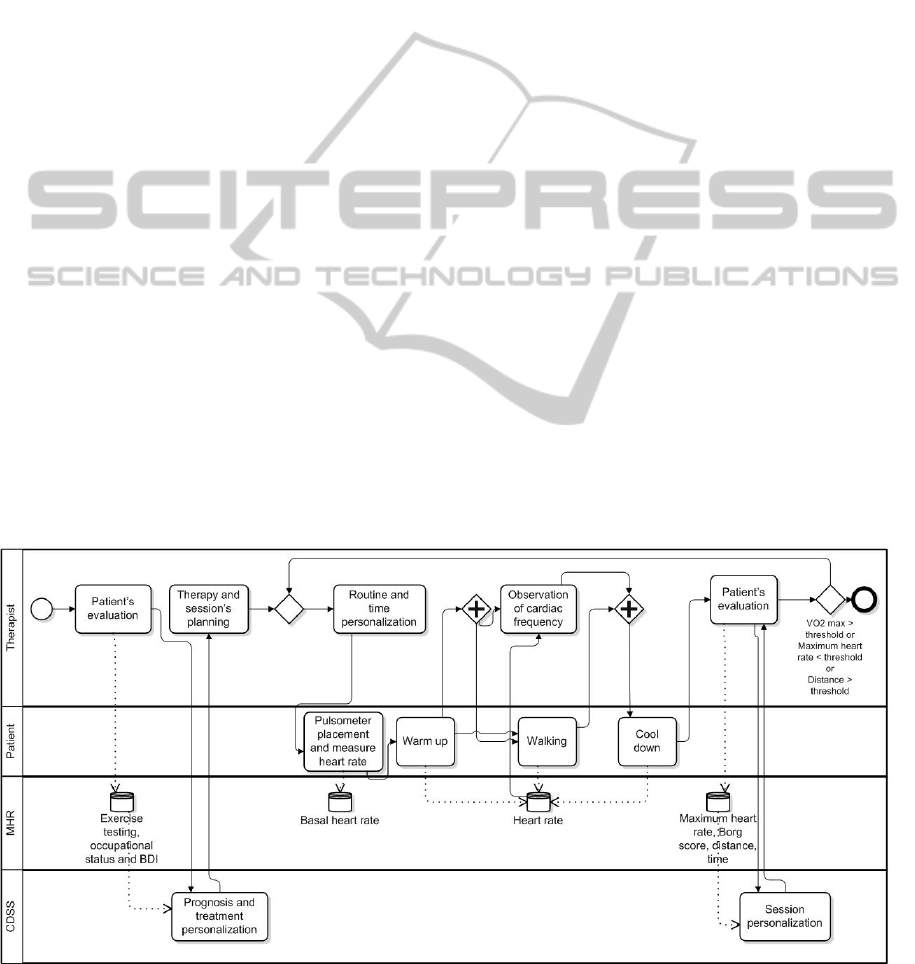
obtained from the resulting decision trees. An
example is the rule (4), which predicts that if a
patient does not suffer from arrhythmia, has as
treatment indicators a severe deficiency in emotional
functions and dyslipidemia less than or equal to 3
(severe deficiency) and follows a psychotropic
therapy; the prognosis of the treatment indicator of
emotional functions after cardiac rehabilitation is no
deficiency.
Patient (?p), Arrythmia (?a), hasnotDisease (?p,
?a), Dislipidemia (?di), TreatmentIndicator (?ti),
hasType (?di,?ti), lessThanOrEqual (3, ?di),
hasIndicator (?p, ?di), hasTherapy (?p,
?psychotropic), EmotionalFunctions (?ef),
Deficiency (?severe), hasDeficiency (?ef, ?severe),
hasType (?ef, ?ti), EmotionalFunctions (?efa),
Deficiency (?no), hasDeficiency (?efa, ?no),
CardiacRehabilitation (?cr), after (?efa, ?cr),
hasType (?efa,?ti)
hasIndicator (?p, ?ef) (4)
This rule is part of the implementation of the
decision tree in Fig. 2.
3.3 Querying
The proposed framework allows querying using
SPARQL. The following example shows how the
definition of the Walking activity is used by the
therapeutic plan. First, the system evaluates which
session indicators the patient should improve
through the following query:
Count(?i) where Patient (?p),
SessionIndicator (?i), Deficiency (?mild),
hasDeficiency (?i, ?mild),
has Indicator (?p, ?i) (5)
Then, activities which cover this objective are
shown. If Apollo wants to improve his exercise
tolerance functions, the query would be:
Select (?a) where Activity (?a),
Exercise Tolerance Functions (?i),
has Objective (?a, ?i) (6)
Finally, it is checked if the activity is not
contraindicated to the patient. In the Walking
activity, the corresponding query would be:
Count (?contraindication) where Patient (?p),
Moderate, severe or complete neuromusculoskeletal
and movement-related functions (?mscn),
has Contraindication (?p, ?mscn) (7)
4 RESULTS
Results are based on the application of the cardiac
rehabilitation scenario described in Section 1. Fig. 3
shows the interface of the CDSS provided to the
therapist. The interface shows an initial diagnosis
which includes causes of the functional limitation,
past procedures and functioning indicators.
Functional diversity levels of indicators are
represented as red/4 (complete), orange/3 (severe),
yellow/2 (moderate), green/1 (mild) and blue/0 (no
functional diversity) (Subirats et al., 2013). The
Figure 1: Cardiac rehabilitation processes.
Medical-treatmentRecommendationandtheIntegrationofProcessModelsintoKnowledge-basedSystems
495
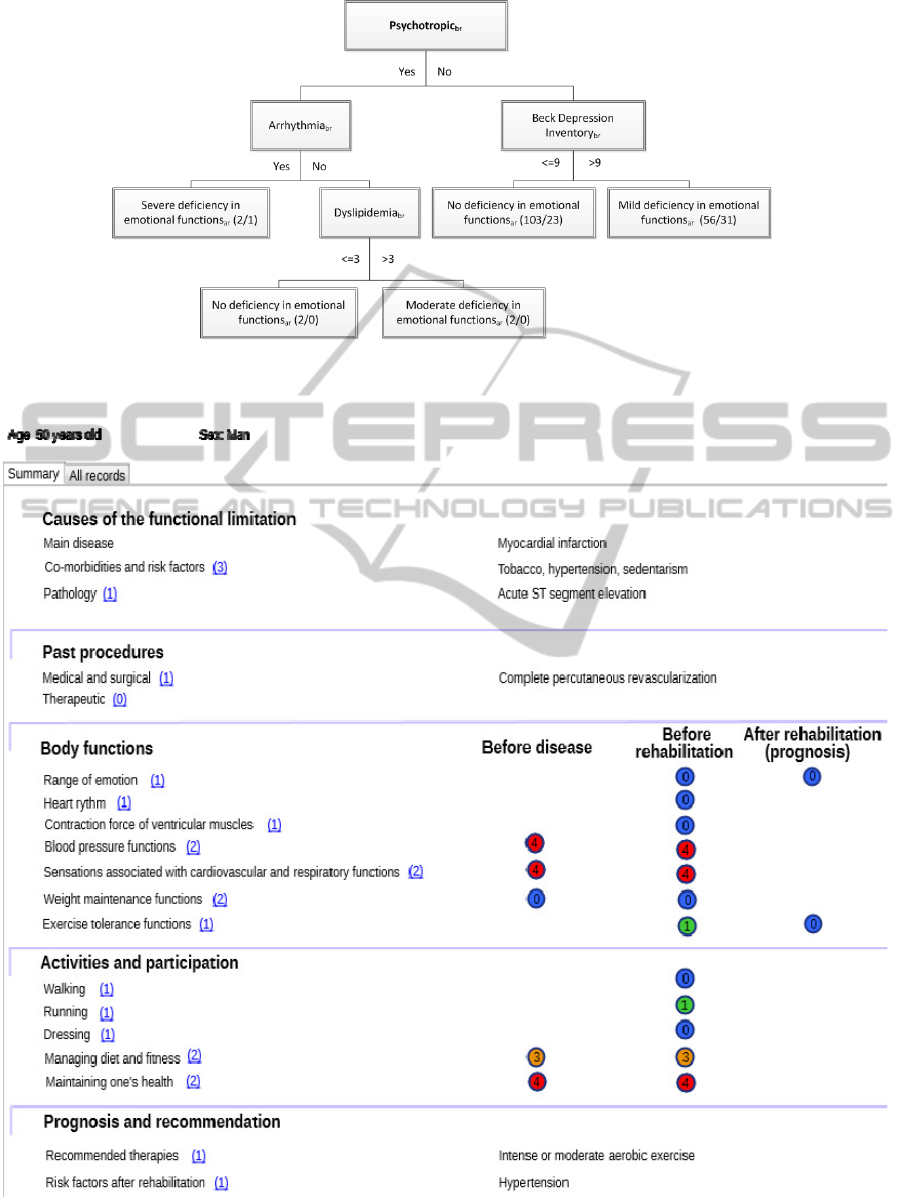
Figure 2: Decision tree of emotional functions prognosis (br = before rehabilitation; ar = after rehabilitation); in brackets,
total/misclassified instances reaching the leaf.
Figure 3: CDSS's interface of patient's prognosis and personalization.
ICAART2014-InternationalConferenceonAgentsandArtificialIntelligence
496

Table 2: Evaluation of the CDSS.
Decision
support
Treatment or treatment indicator:
possible solutions (separated by /)
Accuracy Precision Recall
Personalization
of the treatment
Psychotherapy: yes / no 0.8 0.2 / 0.9 0.6 / 0.8
Psychotropic therapy: yes / no 0.9 0.2 / 0.9 0.3 / 0.9
Prognosis
Exercise tolerance
functions after
rehabilitation: no / mild / moderate /
severe / complete deficiency
0.5
0.2 / 0.6 / 0.5 / 0 /
0
0.1 / 0.8 / 0.6 / 0 / 0
Emotional functions: no / mild /
moderate / severe / complete deficiency
0.6
0.7 / 0.5 / 0.3 / 0 /
0
0.8 / 0.4 / 0.2 / 0.1 /
0
Hypertension risk after
rehabilitation: low / medium / high
0.7 0.8 / 0.8 / 0.6 1.0 / 0.4 / 0.8
Infarction risk: low / medium / high 0.9 0.9 / 0.9 /1.0 0.9 / 0.9 / 1.0
prognosis of the treatment indicators range of
emotion and exercise tolerance functions are
provided, and in the prognosis section it appears the
recommended therapy (that in this case is intense or
moderate aerobic exercise and hypertension risk
factor after rehabilitation).
Rules are evaluated through the correct
execution of the cardiac rehabilitation process in
order to verify completeness of the rule set.
However, the knowledge of the system can
increase/change over time due to (1) more patients
(rules from decision trees can change), (2) an update
of processes; and (3) an update of literature. As all
rules in this model are static, in the future, a Java
library which generates decision trees using Weka,
converts them automatically to SWRL rules, and
integrates them in the ontology will be created.
Table 2 shows the evaluation of the
personalization of therapies, prognosis and risk. In
order to evaluate the performance of prediction of
treatment indicators’ behavior, accuracy, recall (or
sensitivity) and precision (or positive predictive
value) are considered and defined as follows:
T
N
F
N
F
P
T
P
TNTP
accuracy
,
F
P
T
P
TP
precision
,
F
N
T
P
TP
recall
.
where TP are true positives, FN are false
negatives, FP are false positives and TN are true
negatives. Considering that low values of recall can
cause potential harm in the clinical domain,
hypothesis which higher values of recall are
generally considered better, while maintaining
precision above a specific threshold set by an expert
(Huang et al., 2006). In the personalization of the
treatment, the CDSS has recall values of 0.8 and 0.9
when recommending not to prescribe psychotherapy
and not to prescribe psychotropic therapy,
respectively. In the prognosis of exercise tolerance
functions after rehabilitation, recall values for mild
and moderate deficiency are 0.8 and 0.6,
respectively. In the prognosis of emotional
functions, recall values for mild and no deficiency
are 0.4 and 0.8, respectively. In the prognosis of
hypertension risk after rehabilitation, the recall
value for high risk is 1.0. In the prognosis of
infarction risk, recall values for low, medium and
high risk are 0.9, 0.9 and 1.0, respectively; however,
in this case, the CDSS was tested only on 19
patients. Some very low recall and precision values
are due to classes with a very low number of cases
(see Table 1). This is the case, for example, of
severe and complete deficiency in emotional
functions.
Paths of the decision trees which correspond to
predictions with a recall less than 0.8 or a precision
less than 0.6 are not encoded as rules. In these cases,
consequently, no support is provided to therapists.
Paths of the decision trees which are encoded as
rules correspond to bold values in the Treatment or
treatment indicator: possible solutions column of
Table 2.
In Van et al. (2011), a study that predicts risk
factors with decision trees with data from 3931
patients, the accuracy of the prediction of emotional
functions (which is the ICF encoding of the Hospital
Anxiety and Depression Score) is 0.5, while the
accuracy of the prediction of hypertension is 0.5.
Although the accuracy of the prediction of emotional
functions and hypertension is a little bit higher in the
proposed approach than in the study of Van et al.
(2011), this approach is not able to predict minor
classes. On the other hand, the study of Chang et al.
(2011), predicts the risk factors of hypertension and
hyperlipidemia with a combined accuracy of 0.9.
5 CONCLUSIONS
This paper introduced a framework, based on rules
from three sources (business processes, literature
Medical-treatmentRecommendationandtheIntegrationofProcessModelsintoKnowledge-basedSystems
497

and decision trees) and including biomedical
annotations, to provide formal semantics to cardiac
rehabilitation processes represented in BPMN 2.0.
This semantics, together with rules obtained from
literature and data mining, can be used to introduce
automatic reasoning in decision support. The rule-
based framework uses existing ontologies and
formal process notation to enhance interoperability
and reasoning in rehabilitation and, specifically, to
allow working with different types of indicators, and
to merge medical ontologies and terminologies such
as ICF, SNOMED CT, ICD-10 and ICD-11.
Different issues appeared when implementing
rules obtained from sources needing different
degrees of human interpretation. Difficulties due to
the high number of rules coming from BPMN 2.0
processes were solved generalizing them. And only
rules from decision trees which have recall and
precision above a threshold of 0.8 and 0.6,
respectively, were encoded.
The proposed CDSS, which uses data from 200
patients carrying out cardiac rehabilitation at a
hospital, has high values of recall in the
personalization of therapies, and in the prognosis of
activities and risk factors.
Future work includes making the framework
more dynamic and able to automatically reorganize
itself when new or updated data or processes are
available. In addition, more cases will be analyzed to
cover classes which are less represented in the
knowledge base.
ACKNOWLEDGEMENTS
The research described in this paper is partly
supported by a Spanish research project called
Rehabilita (Disruptive technologies for the
rehabilitation of the future) (CEN-2009-1043). This
work is also partly supported by the Catalonia
Competitiveness Agency (ACC1Ó).
REFERENCES
Calvo, M., Subirats, L., Ceccaroni, L., Maroto J. M., de
Pablo, C., Miralles, F. Automatic assessment of
socioeconomic impact in cardiac rehabilitation. Int. J.
Environ. Res. Public Health, 10(11), 5266-5283, 2013.
C. D. Chang, C. C. Wang and B. C. Jiang. Using DM
techniques for multi-diseases prediction modeling of
hypertension and hyperlipidemia by common risk
factors. Expert Syst. Appl. 38(1):5507-5513, 2011.
A. Cichocki, A. Helal, M. Rusinkiewicz and D. Woelk.
Workflow and Process Automation. Kluwer Academic
Publishers, 1998.
K. Huang, H. Yang, I. King and M. R. Lyu. Maximizing
sensitivity in medical diagnosis using biased minimax
probability machine. IEEE Transactions on
Biomedical Engineering, 53(5):821–831, 2006.
B. Jafarpour, S. Raza Abidi and S. S. Raza Abidi.
Exploiting OWL reasoning services to execute
ontologically-modeled clinical practice guidelines.
AIME 2011, LNCS, 6747: 307-311, 2011.
N. Peek, R. Goud, N. de Keizer, M. van Engen-Verheul,
H. Kemps and A. Hasman. CARDSS: Development
and evaluation of a guideline based decision support
system for cardiac rehabilitation. AIME 2011, LNCS,
6747:109-118, 2011.
F. Smith, M. Missiko and M. Proietti. Ontology-based
querying of composite services. Business System
Manag. and Engineering, 7350:159-180, 2012.
Subirats, L., Ceccaroni, L., Lopez-Blazquez, R., Miralles,
F., García-Rudolph, A. and Tormos, J.M. Circles of
Health: towards an advanced social network about
disabilities of neurological origin. J. Biomed. Inform.,
46(6), 1006-1029, 2013.
A. Van, V. Gay, P. J. Kennedy, E. Barin, P. Leijdekkers.
Understanding Risk Factors in Cardiac Rehabilitation
Patients with Random Forests and Decision Trees. 9
th
ADM, 121: 11-22, 2011.
Velasco, J. A, Cosín, J., Maroto, J. M., Muñiz, J.,
Casasnovas, J. A., Plaza, I. and Abadal, L. T. GPC en
Prevención Cardiovascular y Rehabilitación Cardiaca
de la Sociedad Esp. de Cardiología. Rev. Esp. Cardiol.
53: 8 1095-1120.
ICAART2014-InternationalConferenceonAgentsandArtificialIntelligence
498
