
Estimation of Arterial Stiffness through Pulse Transit Time
Measurement
Avinash S. Vaidya
1
, T. S. L. Radhika
1
, M. B. Srinivas
1
and Mannan Mridha
2
1
BITS Pilani, Hyderabad Campud , Hyderabad, India
2
Royal Institute of Technology, KTH, Stockholm, Sweden
Keywords: Cardio-Vascular Disease, Arterial Striffness, Pulse Transit Time, Pulse Wave Velocity.
Abstract: Early detection of cardiovascular disease (CVD) and its treatment is significantly expected to reduce the
mortality rate across the world. While several diagnostic techniques have been developed for early detection
of the CVD, recent focus has been on measuring the ‘arterial stiffness’, which appears to be a major
indicator of onset of cardio vascular disease. In this work, authors consider three mathematical models that
relate pulse wave velocity (PWV) with arterial stiffness. While one model considers blood to be a non-
viscous and incompressible fluid, the other considers it to be a viscous and compressible. Pulse transit time
has been measured experimentally for five different individuals of different ages and heights from where
PWV has been estimated. Using values of PWV, Young’s modulus of elasticity has been derived. Data
related to arteries such as radius, wall thickness, density and viscosity of blood have been taken from
published literature where these parameters have been measured using techniques such as MRI. Initial
results indicate that different models predict different estimates for arterial stiffness that depend on
assumptions made.
1 INTRODUCTION
Arterial stiffness is considered to be an indicator of
vascular changes that may eventually result in major
vascular disease (Fung et al., 2004); (Hasegawa et
al., 2004); (Mazumdar et al., 2004). Early detection
of a stiffening artery might help in taking preventive
medication that will slow down the progress of
vascular changes.
Propagation of blood pressure pulse wave is
affected by the arterial stiffness and thus pulse wave
velocity (PWV) is a good measure of stiffness of
artery. Since PWV is related to pulse transit time
(PTT), it is possible to derive PWV by measuring
PTT experimentally (Fung et al., 2004;Ye et al.,
2010). There are two different ways in which PWV
can be measured:
1. By dividing the distance between two arterial
sites by the difference in time of pressure pulse
arrival w.r.t the R wave of EKG signal
2. By measuring the time difference between R
wave of ECG signal and characteristics point of
PPG signal and dividing the same with length of
the artery.
Further, different mathematical models have been
proposed from time to time to estimate arterial
stiffness by relating PWV with young’s modulus of
elasticity (Fung et al., 1984); (Olufsen et al., 2000);
(Kurtz et al., 2003). These models include that of
inviscid (incompressible) flow and viscous flows. In
what follows, these models are discussed in some
detail and used to estimate young’s modulus of
elasticity of arteries of a small sample of subjects
using experimental data obtained. A comparison is
also made of estimates given by different models.
2 MATHEMATICAL MODELS
2.1 Inviscid Flow – Moens-Kortweg
Equation
We know that the flow of blood in arteries is
pulsative due to the beating of the heart. This beating
produces a pressure wave to travel through the blood.
Let u and v be the axial and radial components of the
fluid velocity. Let ρ be the density of the fluid. The
following assumptions have been made in deriving a
mathematical model for the above mentioned
problem (Mazumdar et al., 2004).
238
S. Vaidya A., S. L. Radhika T., B. Srinivas M. and Mridha M..
Estimation of Arterial Stiffness through Pulse Transit Time Measurement.
DOI: 10.5220/0004912002380242
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2014), pages 238-242
ISBN: 978-989-758-013-0
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

The flow is pulsatile and axi-symmetric
The pipe is an elastic circular straight pipe with
radius ‘a’.
The fluid is Newtonian with constant viscosity
‘µ’
The axial flow velocity is small relative to the
pulse wave velocity
The vessel diameter is of an order of magnitude
smaller than the wave length.
Hence, the equation of continuity and the momentum
equation take the form:
1
0
u
rv
x
rr
(1)
up
tx
(2)
0
p
r
(3)
The wall displacement η is governed by
2
,
a
p
xt
hE
(4)
Where E is the wall material elastic modulus and h is
the thickness of the wall.
Using the boundary conditions given by
,,
w
vxt xt
(5)
Where
w
v
is the wall velocity, we have that the
pressure p satisfies the wave equation
22
222
1
p
p
x
ct
(6)
With
1/2
2
Eh
c
a
(7)
where c is the pulse wave velocity.
2.2 Viscous Flow
In this model, the viscous effects are taken into
consideration. The governing equations are:
1
0
u
rv
x
rr
(8)
2
2
1up uu
tx rrr
(9)
0
p
r
(10)
Further, the displacement equations of the elastic
tube of wall thickness ‘h’, wall density ‘ρ
w
’, wall
modulus ‘E’ and Poisson ratio ‘ν’ are taken as
2
222
1
w
Eh
hp
taax
(11)
22
222
1
w
uEh
h
tr xax
Where ζ is the axial displacement and η is the radial
displacement of the tube (Mazumdar et al., 2004).
Boundary conditions are:
,
ra ra
uv
tt
(12)
Assuming that
()
0
(,,) ()
ikx wt
uxrt u re
(13)
()
0
(,,) ()
ikx wt
vxrt v re
()
0
(,)
ikx wt
pxt pe
()
0
(,)
ikx wt
xt e
()
0
(,)
ikx wt
xt e
Where,
2
*
60
Heartrate
2
k
(Wave length) and
c
k
(wave speed).
Solving equations (8)-(11) and using the boundary
conditions given by (12), we have that the elastic
modulus E is given by
2
0 0
1 1
1
12 2 2 0
Ja Ja
XX X
aJa a a Ja
(14)
Where
2
22
(1 )
kEh
X
a
(15)
EstimationofArterialStiffnessthroughPulseTransitTimeMeasurement
239
i
(16)
3 EXPERIMENTS
Experiments have been performed on a small sample
of five different human subjects of different ages and
heights. Experimental measurement of ECG and PPG
has been carried out and time difference between R-
wave peak and characteristic point of PPG signals
calculated to determine PTT.
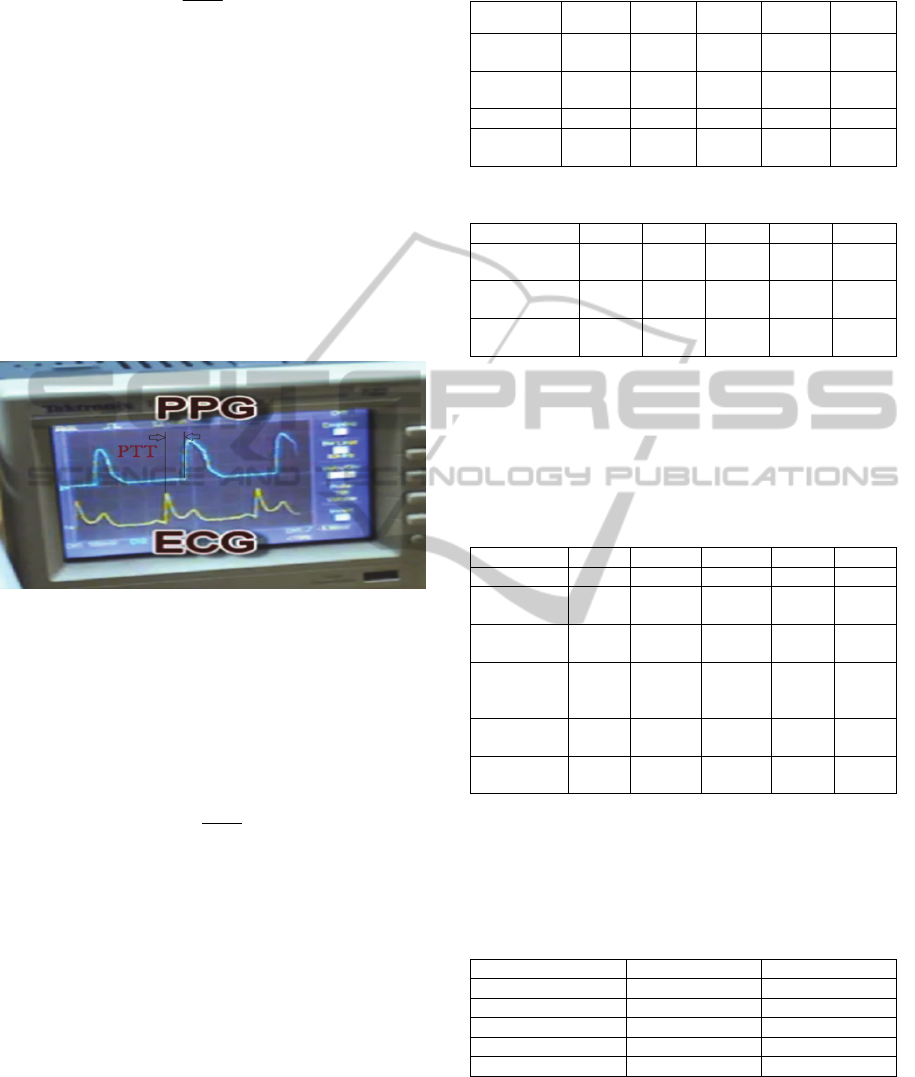
The following picture illustrates the recorded
ECG/PPG signals on one subject for the calculation
of PTT.
Figure 1: Measurement of PTT from PPG and ECG.
Two mathematical models described above have
been used to estimate the Young’s Modulus E of the
arteries.
Since both models require value of PWV, PTT
needs to be calculated using which PWV is estimated
by equation below (Avril et al., 2008).
(17)
Where d is the arterial length between the heart
and fingertip, which is correlated with height of
a person through (Ye et al., 2010):
0.6
(18)
4 RESULTS
Table 1 below lists the measurements made on five
different individuals of different heights and age.
The estimated value of Young’s Modulus using
Model 1, assuming physiological parameters of
artery given in (Avril et al., 2008), is given in Table 2
below.
Table 1: Physiological parameters.
Parameter Sub-1 Sub-2 Sub-3 Sub-4 Sub-5
Age 27 years
49
years
25
years
29 years
39
years
Height 174 cms
152.4
cms
175
cms
173 cms
170
cms
PTT 244ms 205 ms 205 ms 275 ms 260 ms
PWV 4.28 m/s
4.46
m/s
5.12
m/s
3.77 m/s
3.92
m/s
Table 2: Parameters for Model I.
Parameter Sub- 1 Sub- 2 Sub-3 Sub-4 Sub-5
Radius of radial
artery
2.5
mm
2.5
mm
2.5
mm
2.5
mm
2.5
mm
Wall thickness
of radial artery
0.25
mm
0.25
mm
0.25
mm
0.25
mm
0.25
mm
Young’s
Modulus
563.8K
Pa
612.3
KPa
556.2K
Pa
302.1
KPa
326.2K
Pa
The estimated value of Young’s Modulus using
Model 2 and assuming physiological parameters of
artery given in (Hasegawa et al., 2004; Mazumdar et
al., 2004; Avril et al., 2008) is given in Table 3
below.
Table 3: Parameters for Model II.
Parameter Sub-1 Sub-2 Sub-3 Sub-4 Sub-5
Poison’s ratio 0.5 0.5 0.5 0.5 0.5
Density of
blood
1050
kg/m3
1050
kg/m3
1060
kg/m
3
1060
kg/m
3
1060
kg/m
3
Radius of
radial artery
2.5
mm
2.5 mm 2.5 mm
2.5
mm
2.5
mm
Wall
thickness of
radial artery
0.25
mm
0.25
mm
0.25
mm
0.25
mm
0.25
mm
Viscosity of
blood
0.004
PaS
0.004
PaS
0.004
PaS
0.004
PaS
0.004
PaS
Young’s
Modulus
4.8964
MPa
5.3169
MPa
7.01229
MPa
3.8082
MPa
4.1138
MPa
A comparison of Young’s modulus obtained by
both the models for all five subjects is given in Table
4 below.
Table 4: A Comparision of young’s modulus derived
using Model I and Model II.
Subject / Model Used Model I Model II
Subject 1 388.12 KPa 4.8934 MPa
Subject 2 421.794 KPa 5.3181 MPa
Subject 3 556.17 KPa 7.01229 MPa
Subject 4 302.04 KPa 3.8082 MPa
Subject 5 326.28K 4.1138 MPa
5 DISCUSSION
Table 4 provides the value of Young’s modulus for
five different subjects of different ages and heights. It
BIODEVICES2014-InternationalConferenceonBiomedicalElectronicsandDevices
240

is clear from the Table there is a wide variation in the
modulus values predicted by the two models with
almost 2-3 orders of difference in magnitude. This
may possibly be because of the assumptions made
while deriving the models, that is, while one model
assumes the blood to be an inviscid fluid, the other
assumes it to be a viscous one. However, the
measured values of blood pressure for each of the
subjects showed a strong correlation with PTT, that is
smaller the PTT, higher the blood pressure.
Further, the arterial data considered in this paper
have been taken from the literature and no distinction
has been made between the five subjects. That is,
same data related to arterial radius, wall thickness,
etc. have been used for all the subjects. This may
have again given rise to errors in values for arterial
stiffness.
Additionally, but more importantly, there appears
to be still no agreement on true values of arterial
stiffness even using the same model as other
researchers have reported widely varying values for
the Young’s modulus that may even differ by about
300% (Avril et al., 2008).
6 A MORE REALISTIC MODEL
In view of limitations of above-mentioned models,
the authors have started working on another model
that attempts to model blood more realistically. This
model considers blood to be a non-Newtonian fluid
due to the presence of plasma, red blood cells etc.
This model is known as power law model (Nadeem
et al., 2011); (Basu et al., 2013). The constitutive
equation for this model is given by
n
u
r
(19)
Using the expression for the stress tensor given by
equation (19) and using the assumptions mentioned
in the beginning of the paper, the continuity and
momentum equations, take the form
(20)
(21)
0
p
r
(22)
As in the case of the viscous fluid model, the
displacement equations of the wall are taken as
follows:
2
222
1
w
Eh
h
taax
(23)
22
222
1
n
w
uEh
h
tr xax
(24)
Using the boundary conditions given in equation (12)
together with the forms for velocity, pressure and the
displacement components given by equation (13), we
solve equations (20) - (24) for the velocity and the
displacement components.
As the equations given by equation (20) – (24)
are nonlinear in nature, approximate analytical
methods are to be adopted to find an approximate
analytical solution to the problem. In a future study,
it is proposed to use OHAM (Optimal Homotopy
Asymptotic Method) to find an approximate solution
to the problem.
7 CONCLUSIONS
In this work, an attempt has been made to
understand the mathematical models for blood flow
and arterial stiffness as well as derive practical
values for Young’s modulus of elasticity that is an
indicator of stiffness. There appears to be a wide
variation which needs to be understood through
further experimentation.
It should however be mentioned that results
reported in this study are based on an extremely
small set of data (with no controls) and many
assumptions have also been made. It is proposed to
extend this work by considering more realistic
models such as the power law model mentioned
above, a much larger sample size, standardizing the
experiments and using more accurate data for arterial
dimensions while computing the arterial stiffness in
our future studies.
REFERENCES
Fung, P., Dumont, G., Ries, C., Mott, C., and Ansermino,
M., 2004. Continuous Noninvasive Blood Pressure
Measurement by Pulse Transit Time, in Proceedings
of the 26th Annual International Conference of the
IEEE EMBS, San Francisco, CA, USA.
Avril, S., Huntley, J. M., and Cusack, R., 2008.
1
0
u
rv
x
rr
1
nn
up u u
tx rrrr
EstimationofArterialStiffnessthroughPulseTransitTimeMeasurement
241

Charachterization of Wall Stiffness in A Blood Vessel
Using Cine-PC-MRI, in XI International Congress
and Exposition, Orlando, Florida, USA.
Hasegawa, H., and Kanai, H., 2004. Measurement of
Elastic Moduli of the Arterial Wall at Multiple
Frequencies by Remote Actuation for Assessment of
Viscoelasticity, Japanese Journal of Applied Physics,
vol. Vol. 43, no. No. 5B, p. 3197–3203.
Mazumdar, J.N., 2004. Bio-Fluid Mechanics, World
Scientific Publishing. Singapore.
Ku2, Y. M., Kim1, Y. O., Kim3, J. I., Choi4, Y. J.,
Yoon1, S. A. and Kim1, Y. S., 2006. Ultrasonographic
measurement of intima-media thickness of radial
artery in pre-dialysis uraemic patients: comparison
with histological examination, Nephrol Dial
Transplant, vol. 21, pp. 715-720,
Kurtz, M., 2003. Standard Handbook of Biomedical
Engineering and Design, McGraw-Hill Professional
Publishing
Olufsen, M. S., Peskin, C. S., Kim, W. Y., Pedersen, E.
M., Nadim, A. and Larsen, J., 2000. Numerical
Simulation and Experimental Validation of Blood
Flow in Arteries with Structured-Tree Outflow
Conditions, Annals of Biomedical Engineering, vol.
28, pp. 1281-1299.
Fung, Y. C., 1984. Biodynamics Circulation, Springer
Verlag, New York:
Ye, S. Y., Kim, G. R., Jung, D. K., Baik, S. W. and Jeon,
G. R., 2010. Estimation of Systolic and Diastolic
Pressure using the Pulse Transit Time," World
Academy of Science, Engineering and Technology, pp.
726-731.
Nadeem, S., Noreen Sher Akbar, Awatif A. Hendi,
Tasawar Hayat, 2011. Power law fluid model for
blood flow through a tapered artery with a stenosis,
Applied Mathematics and Computation, pp. 7108-
7116.
Basu Mallik, B., Saktipada Nanda, Bhabatosh Das,
Debanshu Saha, Debanu Shankar Das and Koustav
Paul. 2013. A Non Newtonian fluid model for blood
flow using PowerLaw through an Artherosclerotic
arterial segment having Slip velocity. IJPCBS, pp.
752-760.
BIODEVICES2014-InternationalConferenceonBiomedicalElectronicsandDevices
242
