
Serious Games for Assessment and Training in Post-stroke Robotic
Upper-limb Telerehabilitation
Cristina Rodríguez-de-Pablo
1
, Joel C. Perry
1
, Sivakumar Balasubramanian
1
, Aitor Belloso
1
,
Andrej Savić
2,3
, Tijana Dimkić Tomić
4,5
and Thierry Keller
1
1
Rehabilitation Technologies, Health Division, TECNALIA, San Sebastian, Spain
2
Tecnalia Serbia Ltd, Belgrade, Serbia
3
Signals and Systems Department, University of Belgrade - School of Electrical Engineering, Belgrade, Serbia
4
Clinic for rehabilitation Dr Miroslav Zotović, Belgrade, Serbia
5
University of Belgrade, School of Medicine, Belgrade, Serbia
Keywords: Serious Games, Upper-limb Rehabilitation, Robotic Rehabilitation, Quantitative Assessment, Reach
Training, Motivation, Stroke, Home-based Telerehabilitation.
Abstract: Research shows that better results in post-stroke rehabilitation are obtained when patients receive more
intensive therapy. However, the increasing affected population and the limited healthcare resources prevent
the provision of intense rehabilitation care. Thus, there is a need for a more autonomous and scalable care
provision methods that can be transferred out of the clinic and into home environments. Serious games in
combination with robotic rehabilitation can provide an affordable, engaging, and effective way to intensify
treatment, both at the clinic and at home. Furthermore, they can offer quantitative assessment of motor
performance, allowing individualized treatments and to keep the patient and their therapists informed about
therapy progress. Towards this end, a set of games for assessment and training of upper-limb motor
impairment after stroke with the ArmAssist is presented. A special effort has been made to design the
assessment games in order to be able, not only to measure the effectiveness of the training, but also to
compare the assessment results with the standard assessment scales used in the clinic. Feedback from
usability testing of previous versions of the system has also been crucial for the final design. Preliminary
results of an ongoing clinical testing are presented.
1 INTRODUCTION
Research confirms that better results in terms of
rehabilitation outcome are obtained in specialized
care centres where patients receive more therapy per
day and with more quality for extended periods of
time (Sluijs et al., 1993; Kwakkel, et al., 1997).
However, the amount of professionally-
supported rehabilitation training provided to the
average patient is still far from the ideal. A Dutch
report published in 2008 (Peerenboom et al., 2008)
reported that the average treatment time for stroke
patients in skilled nursing facilities was about 4.5
hours per week, and only about 2 of them was spent
in physical therapy.
Healthcare resources are suffering from constant
cutbacks due to economic constraints and the
prevalence of stroke continues to increase
dramatically together with the aging of the
population. As a matter of fact, European statistics
as a whole report that nearly 1 million people
experience a first or recurrent stroke each year
(Hesse et al., 2005). In that context, the amount of
intensive therapy required cannot be provided in the
regular way that rehabilitation care has been
provided up to now. There is a need for more
autonomous and scalable care that can be transferred
out of the clinic. Robot-assisted rehabilitation based
on serious games may offer that care.
Robots offer precision and repeatability of
movements that can be used to provide safe and
intensive rehabilitation exercises. Serious games can
provide an enjoyable and effective way to motivate
patients to increase both the quality and quantity of
therapy by decreasing the monotony of performing
hundreds of repeated motions and by providing
126
Rodriguez-de-Pablo C., Perry J., Balasubramanian S., Belloso A., Savi
´
c A., Dimki
´
c Tomi
´
c T. and Keller T..
Serious Games for Assessment and Training in Post-stroke Robotic Upper-limb Telerehabilitation.
DOI: 10.5220/0005168601260134
In Proceedings of the 2nd International Congress on Neurotechnology, Electronics and Informatics (VirtRehab-2014), pages 126-134
ISBN: 978-989-758-056-7
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

challenging performance feedback. In addition, these
technologies can also be used to remotely assess the
motor impairment of patients without the need for
the therapist to be present. Therefore, a large
increase in robotic rehabilitation based on serious
games has been seen over the last years (Robertson
et al., 2010). Recent commercial players in the field
include Telefonica, MediTouch, HomeTelemed,
Tyromotion and Hocoma.
However, even with the players involved,
commercial success is limited. The solution may lie
in the development of a system that can be easily
integrated with current practice and which can verify
its effectiveness correlating the results of both
assessment and training tools with the assessment
scales and physical therapy performed at the clinic.
Towards this end, this paper presents a new
version of 5 games for assessment and 5 games for
training of post-stroke arm used with the ArmAssist
together with the TeleReha web platform for at-
home telerehabilitation. ArmAssist allows the planar
movement of the arm by supporting the arm while
measuring the movement parameters (2D position,
orientation and arm support/lifting force) that are
used to control the games. The TeleReha platform
allows the patient to perform game-based
rehabilitation both at the clinic and at home, while
the doctor is able to monitor the progress, update the
therapy correspondingly, and communicate with the
patient when necessary. The system components and
functionality have been previously described in
publications (Zabaleta et al., 2011; Perry et al.,
2012; Arcas Ruiz-Ruano et al., 2012).
2 GAMES
2.1 Design Process
A first set of requirements for the games was defined
after a comprehensive review of the key elements
that promote the rehabilitation process and the role
of gaming in robot-aided rehabilitation therapy was
done (Perry et al., 2011). A more detailed list of
requirements and games to be developed was drawn
out integrating this preliminary information with a
series of interviews and focus groups with clinicians.
Then, an iterative approach was used for the
games' design and implementation, meaning that the
games were tested by patients and therapists all
along the implementation process.
Throughout the game design and implementation
process, game design principles and ergonomic and
user interface design standards were closely
observed. Design criteria considered included
aspects such as clarity of instructions and feedback,
optimization of the level of challenge in order to
keep patient motivation, consistency between games,
suitability toward visual or cognitive impairments,
and robustness, i.e., tolerance to user error. A
detailed description of the methods used for the
design was already presented in (Rodriguez-de-
Pablo et al., 2012).
A first version of the games was implemented
and tested in a 12-week clinical pilot test with 9
patients. This usability testing and its results were
further described in (Perry et al., 2013). Then, a
second version of the games was developed in order
to first, include the usability feedback obtained in
previous testing and second, improve the assessment
methodology in order to be able to properly evaluate
the effectiveness of the system and compare the
results of that assessment with the standard scales
used at the clinic. Finally, a shorter usability testing
of the new version of the software was carried out in
the Rehabilitation Service at ‘Hospital Universitario
de Álava- Sede Txagorritxu’ (Spain). The feedback
extracted from that testing was used for the design of
the final version of the software, which is currently
being used in an ongoing clinical study.
2.2 Requirements
In this section, the requirements for the redesign of
the games are presented. A detailed list of the initial
requirements of the games was already presented in
(Rodriguez-de-Pablo et al., 2012).
The main goal of the redesign was to improve
the games in order to be able to properly evaluate
the effectiveness of the system and compare the
assessment results with the standard scales used at
the clinic. For that, first of all, levels in the
assessment games needed to be removed in order to
facilitate intra- and inter-patient comparison. They
had to be kept, however, for the training games in
order to adapt the challenge, motivate the patient and
avoid frustration. Also, it was necessary to make
some of the games simpler and faster; for example
different versions of the Control of Force
assessment game were developed and later
determined to be too time consuming and
cognitively taxing for a rapid assessment. Others
needed a redesign in order to avoid undesired
movements; therefore, the new version of the
Control of Movement game asks only for reach
movements, and the new Range of Movement game
measures only when the user stops in order to avoid
counting ballistic movements. It was observed to be
SeriousGamesforAssessmentandTraininginPost-strokeRoboticUpper-limbTelerehabilitation
127
of major importance the fact that the score was
perfectly aligned with the metric evaluated, as that is
what the patients focused on when trying to
improve. In that way, the reaching movement
requirements have been removed from the new
Control of Force in order to focus on the control of
the lifting force and its smoothness evaluation. And
last, some improvements needed to be done in the
data collection to address some issues detected in the
post-processing work of data from the previous
games.
In addition, most of the feedback obtained in the
usability testing was taken into account for the
redesign. Some examples of the changes included
are:
The improvement of the selection/de-selection
strategies, with an optimization of the timing in
the waiting strategy and a refinement of the
feedback in the lifting force strategy;
The improvement of feedback, e.g., in the
Point to Point game when a piece is inserted;
this was not always properly understood by
patients and they kept trying to insert it;
The clarification of some instructions, e.g.,
providing the hint in the Words game or
allocating a concrete space where the Jigsaw
Puzzle has to be assembled;
The improvement of the visualization, e.g.,
making the back image of the cards in the
Memory game unmistakable with the content
itself;
The empirical adjustment of the time-outs and
level parameters.
2.3 Games’ Description
2.3.1 General Features
There exist two kinds of games. The assessment
games are short tasks (1-2 min.) designed to provide
the therapist with an objective evaluation of the
different parameters that define the arm movement
and to adjust correspondingly the training games.
The training games are longer, more complex and
entertaining tasks, which can also integrate cognitive
components and whose objective is to motivate the
patient to train harder and longer. In both of them,
reach extension movements are encouraged, which
require simultaneous abduction/ adduction of the
shoulder and extension of the elbow.
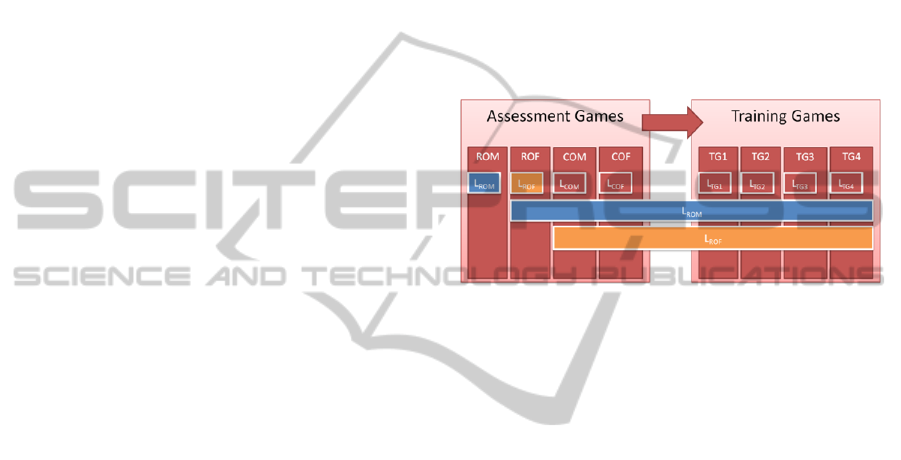
In all the games (Fig. 1) the level is composed by
two aspects: the Movement level (ROM) and the
Force Level (ROF). The ROM, the range of
movement that each game requires, is determined by
the performance of the patient in the first assessment
game, Range of Movement. For accessibility reasons,
the visualization of the games is always the same,
that is, the objects keep their sizes and their
positions; however, the area of the mat where the
ArmAssist has to be moved varies according to the
range of motion of the patient. This avoids some
visualization problems when the range is too small
and has proven to be well understood by patients.
The ROF is the range of vertical force required by
each game, i.e. the percentage of the arm weight that
the patient must lift. This is determined by the
performance of the patient at the second assessment
game, Range of Force.
Figure 1: Influence of the result obtained at ROM and
ROF in the other games.
Furthermore, in the training games a task level
component is included. This is avoided in the
assessment games in order to facilitate the intra- and
inter-patient comparison of the evaluation results.
Each game presents five levels and is scored based
on a combination of evaluated features. The game
levels are automatically adapted by the platform
based on performance. The adaptation method
adopted is the following: a game score of 100
percent or two consecutive scores of at least 80
percent prompt a level increase. Still, if considered
inadequate, the level can be modified by the
therapist from within the platform at any time.
Each time that a game starts, the user will be
asked to move the device slowly over the mat in
order to calibrate the device position. This will not
take more than two seconds. Also, before playing
any game, the user is asked to calibrate the weight of
his arm in a relaxed state in order to calibrate the
vertical force component of the device. This second
calibration needs to be done only once; however, it
can be repeated when desired for changes in the
position of the table or chair that may affect the
weight of the arm.
There are two strategies for selection/ de-
selection of objects in the training games.
ArmAssist’s natural strategy is the use of the vertical
force, that is, lift the arm to pick up a piece, move
and relax the arm to leave it. However, for some
NEUROTECHNIX2014-InternationalCongressonNeurotechnology,ElectronicsandInformatics
128
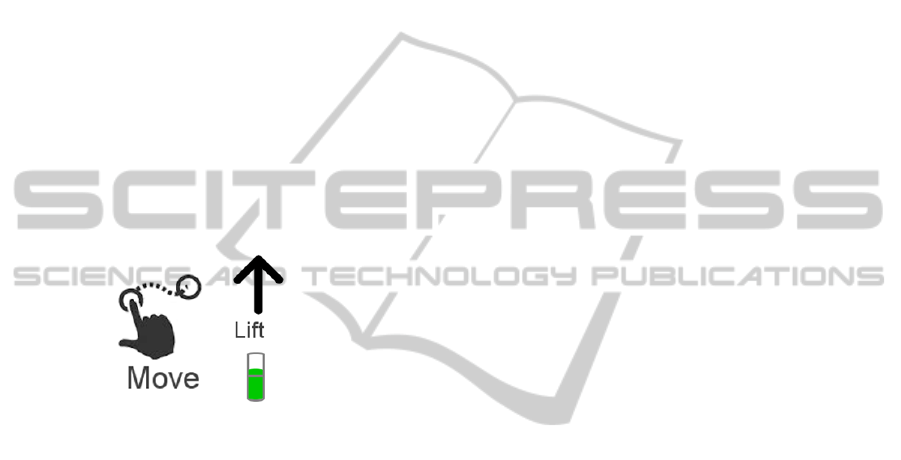
patients this strategy has proven to be more difficult
to understand or to control in the early stages of
rehabilitation. Therefore, another strategy is
provided which does not require the use of the
vertical force, requiring instead a brief pause over
the piece to select it. The piece will be deselected
when the patient pauses after having moved it.
Moreover, in order to avoid unwanted selections, to
reactivate the selection of a part, the user must bring
the cursor out of the piece and place it back over
briefly again. Proper timing is key for this strategy
to work properly. When the therapist deems
appropriate, he will enable the use of force in the
patient’s profile. In both cases, the strategy that
should be used to pick or drop an object is indicated
by a message and icon at the top of the screen (Fig.
2). In order to facilitate the comprehension of the
vertical force selection strategy, the feedback force
is also displayed, indicated in green when the
required threshold lifting force is being performed,
and in red when not.
Figure 2: Indications for the two selection strategies.
Strict overall times and intermediate countdowns
in the case of inactivity are employed in all the
assessment games to ensure that assessments are
carried out efficiently. The intermediate countdowns
ensure, for example, that the cursor is placed at the
required area or that the achieved value is improved
in a determined amount of time. In the training
games, the total time can be assigned by the
therapist. In the games in which the time is
associated with the task level, the game will be
launched successively as many times as necessary to
complete the total time assigned. A ‘direct exit’ has
been enabled in case the user or therapist wants to
finish a game before the assigned training time; this
can be done pressing the center bar of the device
with both hands. However, when exited in this way,
no data is stored, nor the level updated, etc. thus, it
should not be used as a normal course of action.
General performance indicators are stored for all
the games in each session. During the assessment
games, full force and trajectory information is also
stored in order to allow a detailed post-processing
analysis. The data collection has been improved in
order to solve some problems found in previous data
analysis. The sampling frequency has been increased
from 10 to 100Hz and descriptive data of every state
of the game is collected. In addition, data is split in
blocks, each block corresponding to analog groups
of movements, e.g., extension and flexion; for each
of them the target position and force, events, times
and performance are stored.
2.3.2 Assessment Games
The Force Calibration game (Fig. 3(a)) serves to
weigh the patient's arm in a relaxed position and
thereby calibrate the vertical force characteristic of
the device. Therefore, it should be performed before
any other game. Moreover, without any limitation of
time, it helps the patient to have an initial contact
with the vertical force characteristic of the device,
which generally causes some confusion for the
patients at first. In this way the patient can try as
much as needed to use this feature and see the
feedback result of his actions on the screen. When
the patient understands this concept and is prepared,
correct posture of the torso and the relaxation of the
arm must be checked and then the calibration can be
started. This arm weight calibration needs to be done
only once; however, it can be repeated at any time.
The Range of Movement game (Fig. 3(b))
evaluates the range of extension movements from a
central position towards the different directions of
the transverse plane. Being the one that defines the
ROM required by the rest of the games, this should
always be the first game to be played; or just after
the Force Calibration game in the case that this later
was never played before. In the game, different
sectors have to be deleted with a reach extension
movement of the arm from the central ball to the
furthest point reached in that direction as indicated
by the white arrow. The patient needs to stop at the
furthest point reached in order for the result for that
sector to be saved, thereby avoiding the acceptance
of ballistic movements. Then he must return to the
centre ball and start again with another sector. In
order to improve the user feedback, there are two
ways in which sectors are visually erased (Fig. 3(b)):
instantaneously as the cursor passes (in light green),
which gives real-time feedback to the user; and once
they stop (in white), when the score is really saved,
and that part of the sector deleted permanently. The
patient must ensure that he remains upright during
the game. The game detects if the patient leans over
the table in order to achieve a greater range of
movement; in that case the game is interrupted until
he corrects the posture.
The Range of Force game (Fig. 3(c)) assesses the
SeriousGamesforAssessmentandTraininginPost-strokeRoboticUpper-limbTelerehabilitation
129
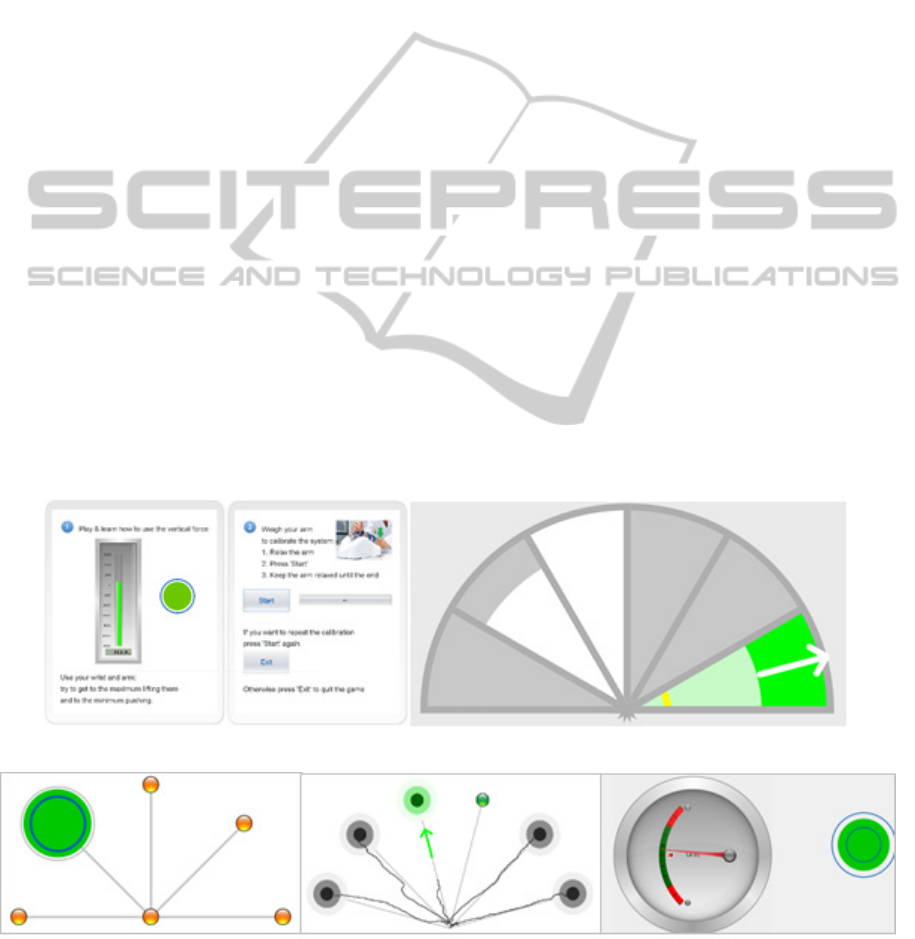
arm support/lifting capacity in different positions of
the plane by placing the cursor over a circular target
and lifting the arm. As the arm is unloaded from the
device, the size of the target is increased in
proportion to the lifting force in order to reach the
diameter of a peripheral ring which indicates the
target unloading level. Being the one that defines the
ROF required by the rest of the games, this should
always be the second game to be played, after the
Range of Movement game.
The Control of Movement game (Fig. 3(d))
evaluates the patient's motion control when he has to
follow a path from one point to another and stop in a
very restricted time. For that, the user must first,
move the cursor to the centre ball; second, to the
target that is blinking and stop in the centre as
quickly as possible. Then, go back to the centre and
start the task over moving to the new ball that blinks.
As in the Range of Movement game, the patient
must ensure that he remains upright during the
game; otherwise, the game will be interrupted until
he corrects the posture.
The Control of Force game (Fig. 3 (e)) evaluates
the patient's ability to control the level of vertical
force, that is, the ability to lift the arm. Keeping the
arm in a centred position on the mat, the patient
must lift the arm slightly trying to keep the needle in
the middle of the dial, always in the green area. This
area will become narrower, and therefore will
require a greater control of the arm as the time
passes. The patient should keep this position until
the progress bar completes. The goal value is based
on the ROF evaluated in the Range of Force game.
For consistency with other games, in the case that
the user prefers the feedback on the right side of the
screen, the user must try to keep the green circle
within the two blue circles.
2.3.3 Training Games
These games aim to train in an enjoyable way the
reach extension movements of the arm, generally
having to pick objects and move them to different
positions of the plane. To accomplish this, the user
has to first, place the cursor over the corresponding
object and stop briefly, or lift the arm in the case that
the vertical force component is being used, which
will be indicated; second, move it to the
corresponding position; and third, stop briefly again
or rest the arm in the previously mentioned case.
Each game presents five levels and is scored based
on a combination of evaluated features. Time
available is also adjusted according to the level in
each case.
In the Words game (Fig. 4(a)) the missing letters
in the words have to be completed with the spare
letters at the bottom of the screen. The letter will go
back to its initial position if it is introduced into the
wrong space or is released, that is, if we stop for 1
second after moving the piece or rest the arm. As the
level increases, the number of missing letters to be
filled in each word, the difficulty of the word and the
(a) (b)
(c) (d) (e)
Figure 3: Assessment games: (a) Force Calibration (b) Range of Movement (c) Range of Force (d) Control of Movement (e)
Control of Force.
NEUROTECHNIX2014-InternationalCongressonNeurotechnology,ElectronicsandInformatics
130

(a) (b)
(c)
(d)
(e)
Figure 4: Training games: (a) Words (b) Jigsaw Puzzle (c) Memory (d) Point to Point (e) Solitaire.
difficulty of the task also increase. Task difficulty,
for example, increases by having to fill in vowels or
consonants and the accuracy needed for a letter to be
considered selected or introduced. In the Point to
Point game (Fig. 4(d)) each object has to be placed
in its box. The levels are defined by the number of
elements to be introduced and the accuracy needed
for an object to be considered selected or introduced.
For the Memory game (Fig. 4(c)) the user has to
discover pairs of matching cards, remembering the
ones previously discovered by the user or the
opponent (the PC). The number of pairs and the
intelligence of the PC define the levels. The users
can also train by putting together a Jigsaw Puzzle
(Fig. 4 (b)) whose number and size of pieces
increase with the levels. As a fifth training game, the
user can play the typical Solitaire game (Fig. 4(e))
with different numbers of cards dealt and times to
complete the task.
3 TESTING
The games are currently being used informally at the
Rehabilitation Service at ‘Hospital Universitario de
Álava- Sede Txagorritxu’ (Spain) in order to get
further usability feedback.
Furthermore, a clinical study is being conducted in
the Clinic for Rehabilitation ‘Dr Miroslav Zotović’
in Belgrade, Serbia. The main purpose of this study
is to determine the correlation between ArmAssist
assessment results and standard clinical assessment
scales. Patients included in this study are 40 to 70-
year-old stroke survivors in the sub-acute phase with
unilateral paresis, able to understand simple
instructions, and who have some voluntary
movements in elbow and shoulder joints. The
program lasts four weeks during which patients have
at least one hour of conventional therapy and at least
thirty minutes of additional therapy per day, five
days per week. The additional therapy differs
depending on whether the patient was randomly
assigned to the ArmAssist group, where they
exercise within the TeleReha platform, or the
Control group where they receive work therapy,
designed to match the training received by the
experimental group. Each group comprises 15
patients.
All patients will be assessed at the beginning and
the end of the program. The Fugl-Meyer Assessment
(Sanford et al., 1993), the Action Research Arm Test
(Van der Lee et al., 2001), the Barthel index (Collin
et al., 1988), the Modified Rankin scale (De Haan et
al., 1995), the Beck depression scale (Beck et al.,
1961), the Wolf Motor Function test (Wolf et al.,
2001) and the Modified Drawing Test (Kostić et al.,
2013) are among the measurements used. In
addition, an experimental psychologist interviews
patients to evaluate comfort, pain, fatigue,
enjoyment, benefits, desire to continue, and
motivation to exercise.
SeriousGamesforAssessmentandTraininginPost-strokeRoboticUpper-limbTelerehabilitation
131
4 RESULTS
Initial informal feedback from patients and
clinicians at the usability testing has been highly
positive. It shows that the system is easy to use and
integrates well in the clinical setting. The majority of
the issues and feedback items have been addressed
in the redesign and this was very much appreciated
by the users involved.
Patients felt motivated, trained for longer and
their perception of pain and fatigue was lower. The
knowledge of performance clearly motivated them
to continue the training and to improve in every
session. For that reason, it was observed that, in
order to avoid frustration, the difference between
assessment and training games must be clear for the
patients; the significant difference being that the
maximum values for the first ones are defined by
healthy patients and are not adapted to their capacity
as in the case of the second ones.
Therapists considered the system useful and
appreciated the fact that it allows them to treat
several patients at the same time.
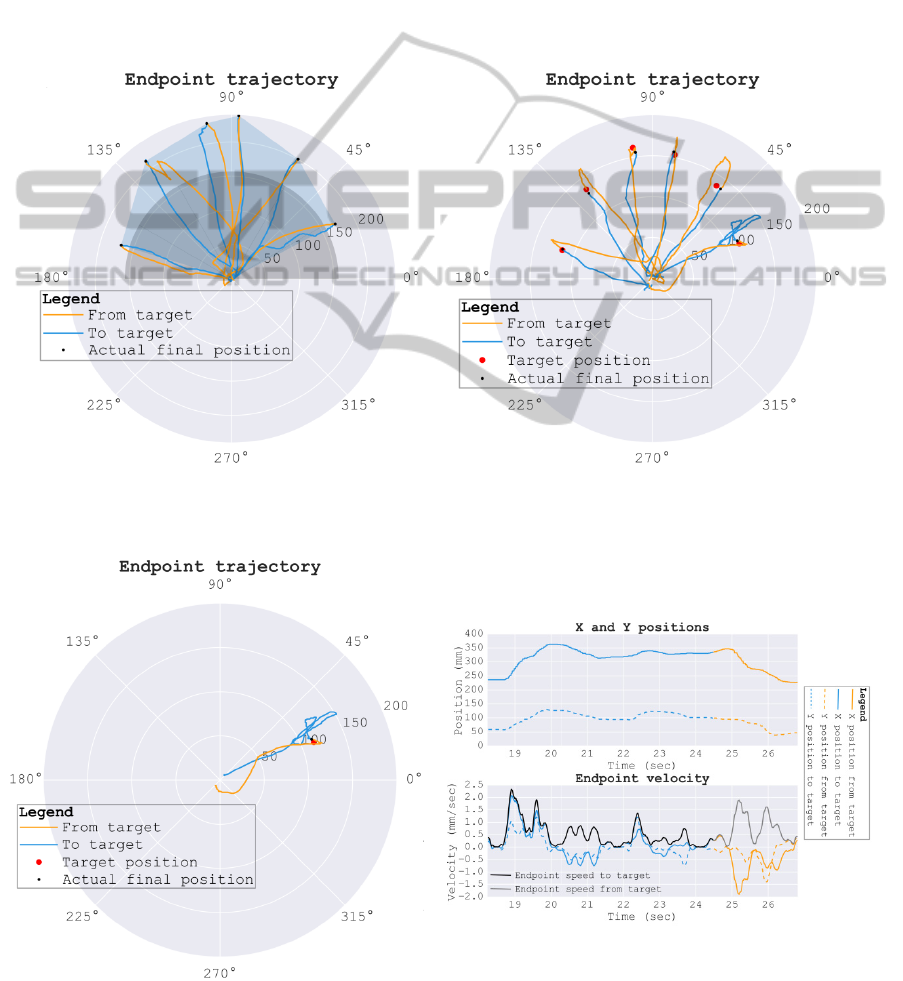
(a)
(b)
Figure 5: Full position data visualization for (a) Range of Movement game (b) Control of Movement game.
Figure 6: Data block analysis for the Control of Movement game.
NEUROTECHNIX2014-InternationalCongressonNeurotechnology,ElectronicsandInformatics
132

Still, the number of training games is too low to
keep the user motivated after the first weeks. For
that reason, a special application is currently being
developed in order to be able to use the ArmAssist
as a normal mouse and, in that way, be able to surf
the Internet and play any other games available.
However, standard games in the Internet usually
need an advanced use of the cursor; therefore,
precision of the cursor positioning must be improved
for the application to work properly.
Preliminary analysis of the first data obtained
from the ongoing clinical study shows that the
quality of the data has been improved, which will
facilitate post-processing and conclusions extraction.
For example, a one-shot analysis of the range and
control of motion of the patient in the different
directions of the plane can be performed, shown in
(Fig. 5). Also, detailed analysis of each trial, e.g.
extension plus flexion movement, can be carried out,
providing very visual and useful information of the
movement. As an example, the detailed analysis of
a block of data of the Control of Movement game is
presented in (Fig. 6), were smoothness of the
movement can be clearly observed.
However, further data is needed in order to extract
any trends and conclusions regarding the validity of
the assessment and the effectiveness of the training
games. This data will be further obtained in the
ongoing testing.
5 CONCLUSIONS
A new version of assessment and training games has
been developed for at-home post-stroke arm
rehabilitation. The aim was to include feedback
gathered in previous usability testing and to improve
the assessment methodology in order to be able in
the future, not only to measure the effectiveness of
the system, but also to compare the assessment
results with the standard assessment scales used in
the clinic up to now. Initial feedback from patients
and clinicians of the new version of the games has
been highly positive. Preliminary analysis of data
from the currently ongoing testing shows that the
quality of the data has been improved; this will
facilitate post-processing and conclusions extraction
regarding effectiveness and assessment validity.
Future work comprises the analysis of data obtained
from the ongoing clinical study, the corresponding
redesign of games according to the results obtained,
if necessary, and the development of new training
games.
ACKNOWLEDGEMENTS
The authors would like to thank the Rehabilitation
Service at the ‘Hospital Universitario de Álava-
Sede Txagorritxu’ for their contributions to the
design of the games and J. Arcas, H. Zabaleta and D.
Valencia for their contributions to the whole system.
REFERENCES
Sluijs, E.M., Kok, G.J., Zee, J., 1993. Correlates of
exercise compliance in physical therapy, In Physical
Therapy, 73 (11), pp. 771–782.
Kwakkel, G.,Wagenaar, R.C., Koelman, T.W., Lankhorst
G.J., Koetsier, J.C., 1997. Effects of intensity of
rehabilitation after stroke, a research synthesis, In
Stroke 28.8 (1997): 1550-1556
Peerenboom, P. B. G., Spek, J., Zekveld, I., Cools, H. J.
M., van Balen, R., & Hoogenboom, M. J., 2008.
Revalidatie in de AWBZ, omvang, aard en intensiteit.
Etc Tangram. In LUMC/PHEG Verpleeghuisgenees-
kunde, 31. [Online]: http://www.vumc.nl/afdelingen-
themas/69713/27797/tangram_RapportRevalidatieD1.
pdf, accessed April 2013.
Hesse, S., Werner, C., Pohl, M., Rueckriem, S., Mehrholz,
J., Lingnau, M.L., 2005. Computerized Arm Training
Improves the Motor Control of the Severely Affected
Arm After Stroke A Single-Blinded Randomized Trial
in Two Centers. In Stroke, 36:1960-1966.
Robertson, J. V. G., Roby-Brami, A., 2010. Augmented
feedback, virtual reality and robotics for designing
new rehabilitation methods. In Rethinking Physical
and RehabilitationMedicine, J.-P.Didier and E.
Bigand, Eds., pp. 223–245. Springer.
Zabaleta, H., Valencia, D., Perry, J., Veneman, J., Keller,
T., 2011. Absolute position calculation for a desktop
mobile rehabilitation robot based on three optical
mouse sensors. In Engineering in Medicine and
Biology Society, EMBC, 2011 Annual International
Conference of the IEEE (pp. 2069-2072). IEEE.
Perry, J. C., Zabaleta, H., Belloso, A., Rodriguez-de-
Pablo, C., Cavallaro, F. I., Keller, T., 2012.
ArmAssist: Development of a functional prototype for
at-home telerehabilitation of post-stroke arm
impairment. In Biomedical Robotics and Biomecha-
tronics (BioRob), 2012 4th IEEE RAS & EMBS
International Conference on (pp. 1561-1566). IEEE.
Arcas Ruiz-Ruano, J., Perry, J.C., Rodriguez-de-Pablo, C.,
Keller, T., 2012. TeleREHA: online/offline web
platform for telerehabilitation of post-stroke arm
impairment. In Intl. Conf. on Neurorehabilitation,
ICNR 2012, November 14-16, Toledo, Spain.
Perry, J. C., Andureu, J., Cavallaro, F. I., Veneman, J.,
Carmien, S., Keller, T., 2011. Effective game use in
neurorehabilitation: user-centered perspectives. In
Handbook of Research on Improving Learning and
SeriousGamesforAssessmentandTraininginPost-strokeRoboticUpper-limbTelerehabilitation
133

Motivation through Educational Games, IGI Global,
Ch. 32, pp:683-725.
Rodríguez-de-Pablo, C., Perry, J. C., Cavallaro, F. I.,
Zabaleta, H., Keller, T., 2012. Development of
computer games for assessment and training in post-
stroke arm telerehabilitation. In Engineering in
Medicine and Biology Society (EMBC), 2012 Annual
International Conference of the IEEE (pp. 4571-
4574). IEEE.
Perry, J.C., Rodriguez-de-Pablo, C., Cavallaro, F. I.,
Belloso, A., Keller, T., 2013. Assessment and
training in home-based telerehabilitation of arm
mobility impairment. In Journal of Accessibility and
Design for All (CC) JACCES, 2013, Vol 3, No 2: 117-
135. ISSN: 2013-7087
Sanford, J., Moreland, J., Swanson, L. R., Stratford, P. W.,
and Gowland, C., 1993. Reliability of the Fugl-Meyer
assessment for testing motor performance in patients
following stroke. In Physical therapy, vol. 73, no. 7,
pp. 447-454
Van der Lee, J. H., De Groot, V., Beckerman, H.,
Wagenaar, R. C., Lankhorst, G. J., and Bouter, L. M.,
2001. The intra-and interrater reliability of the action
research arm test: a practical test of upper extremity
function in patients with stroke. In Archives of
physical medicine and rehabilitation, vol. 82, no. 1,
pp. 14-19
Collin, C., Wade, D. T., et al., 1988. The Barthel ADL
Index: a reliability study. In International Disability
Studies 10(2): 61-63
De Haan, R., Limburg, M., et al., 1995. The clinical
meaning of Rankin 'handicap' grades after stroke. In
Stroke 26: 2027-2030
Beck, A.T., Ward, C. H., Mendelson, M., Mock, J.,
Erbaugh, J., 1961. An inventory for measuring
depression. In Archives of General Psychiatry, 4, 561-
571.
Wolf, S. L., Catlin, P. A., et al., 2001. Assessing Wolf
motor function test as outcome measure for research in
patients after stroke. In Stroke 32: 1635-1639.
Kostić, M. D., and Popović, M. D., 2013. The modified
drawing test for assessment of arm movement quality.
In Journal of Automatic Control, 21(1), 49-53.
NEUROTECHNIX2014-InternationalCongressonNeurotechnology,ElectronicsandInformatics
134
