
Serious Games-based System to Train Weight Shifting and Balance
after Stroke at Home
Description of a Pilot Study and Preliminary Experience
M. Pajaro-Blázquez, A. Dueñas-Ruiz, B. Ferrer-Gonzalez, A. Moreno-Conde, F. Jódar-Sánchez
and C. Parra
Technological Innovation Group, Virgen del Rocío University Hospital, Manuel Siurot Avenue, s/n, 41013 Seville, Spain
Keywords: Serious Games, Telerehabilitation, Stroke.
Abstract: Serious games specifically designed for rehabilitation have the potential to improve motor deficits and can
be used to enhance functional recovery after stroke. Serious games provide a repetitive and structured game-
based training while monitoring user performance and progress. In this paper, we present a description of an
ongoing pilot study of a serious games-based system to train posture, balance and weight shifting after
stroke at home. We also present a preliminary description of three patients enrolled in the pilot study that
are successfully accomplishing an in-home training program showing good adherence, acceptance and
satisfaction with the technology.
1 INTRODUCTION
Overall, in year 2010, an estimated 16.9 million
cases of incident stroke took place worldwide, 33
million prevalent stroke cases, 5.9 million stroke
deaths, and 102.2 million disability-adjusted life
years lost (Feigin et al., 2014). Stroke affects
physical, cognitive and emotional functioning, but
there are interventions that can be done to reduce the
impact of post-stroke effects. Despite adequate
treatment, stroke survivors experience a broad range
of lasting deficits that can impact their cognitive,
visual and motor systems. Moreover, at six to twelve
months after stroke, only 60% of the patients are
independent in personal care, 30% to 40% present
depression and 50% need help either with shopping
or housework (Cheeran et al., 2009). Given the
increasing figures of such events, this poses a large
burden to the National Health Service Providers that
have become overly saturated and are forced to
shorten the duration of the rehabilitation service.
Stroke has an enormous socioeconomic impact also
on the patient’s families that often feel left alone by
the health service providers. Patients that should
continue the therapy outside the hospital actually
drop out mostly due to high costs (Langhorne &
Duncan, 2001).
New technology presents potential benefits for
therapy and can represent an effective way of
providing intensive and structured rehabilitation at a
distance (telerehabilitation) to people with lasting
motor impairments after stroke (Loconsole, Bannò,
Frisoli, & Bergamasco, 2012). The field of game-
based rehabilitation for stroke is growing into a
significant area spurred by the growth in the use of
video games and of new methods for their
development (Fernández-Baena, Susín, & Lligadas,
2012). There are a number of studies published
related to the use commercial games for stroke
rehabilitation (Crosbie, McNeill, Burke, &
McDonough, 2009; Hung et al., 2014; Pedro & De
Paula Caurin, 2012), but efforts in the field of
customizing and creating specific games for
rehabilitation are increasing because commercial
games does not fit properly to the demands and
characteristics of these patients (Sandlund,
McDonough, & Häger-Ross, 2009). Serious Games
are aimed at improving motor deficits while
monitoring and evaluating patient progress, and
offer game-based rehabilitation environments that
motivate the patient during training (Webster &
Celik, 2014). The virtual environment of serious
games can provide safe and customizable training,
which may be tailored to a patient’s interest and
physical abilities. Serious games technology allows
135
Pajaro-Blázquez M., Dueñas-Ruiz A., Ferrer-Gonzalez B., Moreno-Conde A., Jódar-Sánchez F. and Parra C..
Serious Games-based System to Train Weight Shifting and Balance after Stroke at Home - Description of a Pilot Study and Preliminary Experience.
DOI: 10.5220/0005190401350142
In Proceedings of the 2nd International Congress on Neurotechnology, Electronics and Informatics (VirtRehab-2014), pages 135-142
ISBN: 978-989-758-056-7
Copyright
c
2014 SCITEPRESS (Science and Technology Publications, Lda.)

monitoring user performance to analyze results over
time (Deutsch et al., 2012). In this field, previous
studies reported the effectiveness of balance training
performed with video game-based therapy with Wii
Fit for improving balance and for reducing disability
in patients in the subacute phase after stroke
(Morone et al., 2014).
The potential of serious games to help deliver
rehabilitation at home still needs to be explored as a
tool to provide telerehabilitation. Although the
telerehabilitation is a viable alternative way of
delivering rehabilitation services, a systematic
review of telerehabilitation services for stroke
concluded that the evidence was insufficient to draw
conclusions on the effects of the intervention on
mobility, health-related quality of life or participant
satisfaction with the intervention. Moreover, no
studies evaluated the cost-effectiveness of
telerehabilitation (Laver et al., 2013).
We hypothesize that using an in-home virtual
reality system that aims to train posture and balance
at home is feasible and that the regularly training
with the system may improve balance, endurance
and motor function after stroke. The goal of this
paper is to describe the ongoing pilot study to
evaluate the use of a serious games-based
rehabilitation system constituted by a multi-level
rehabilitation platform and to give a preliminary
description of the experience of three patients with
post-stroke hemiparesis enrolled in the study that are
using the system at home.
2 MATERIAL AND METHOD
2.1 Recruitment and Study Population
Patients are recruited from the rehabilitation
department of the Virgen del Rocío University
Hospital (Seville, Spain). Patients meeting the
inclusion criteria are fully informed and included in
the study after signing the informed consent form.
The inclusion criteria are as follows: age over 18
years old, history of stroke ≥ 3 months, signed
informed consent, presence of caregivers,
Minimental State Examination score > 20, training 2
weeks at the hospital, Functional Ambulation
Classification > 3, ability to walk for six minutes,
Berg Balance Scale > 21, enough working space at
home for the use of the REWIRE system and WiFi
connection. The exclusion criteria are as follows:
previous neurological progresive disease, pain that
impossibility the use of the platform, psychiatric
illness, emotional deficit, vision impairments. The
pilot study received the aproval of the Ethical
Committe of our institution prior patient enrollment
2.2 Multilevel Platform
The REWIRE project develops and tests an
innovative rehabilitation platform based on a virtual
reality , which allows patients, discharged from the
hospital, to continue intensive rehabilitation at home
under remote monitoring by the hospital itself. The
main idea is to assemble off the shelf components in
a robust and reliable way to get a multilevel platform
system that enable to be deployed massively at the
patients’ homes. The platform is constituted of three
hierarchical components: a patient station (PS),
deployed installed at home, a hospital station (HS)
and a networking station (NS) at the health provider
site.
The PS is based on video-based tracking
(through a mix of 2D and 3D cameras) and virtual
reality. The patients perform their training or “
serious games” at home through a Kinect and force
platform systems (Tymo plate by Tyromotion, Graz,
Austria). The patient sees himself/herself or an
avatar interacting in real time with a virtual game.
Game variety of scenarios, balanced scoring system,
quantitative exercise evaluation, audio-visual
feedback aims at maximum patient’s motivation. A
robust and reliable auto-calibration and spatial
synchronization with the graphics is developed.
Patient’s daily activity is monitored by a Body
Sensor Networks (Lifestyle system) and his activity
is profiled through eigenbehavior (Krause, Lusseau,
& James, 2009). Environmental, physiological and
motion data are combined to tune the rehabilitation
exercise level, to assess potential risks and advice
clinicians on the therapy.
The HS main role is the definition and
monitoring of the treatment. Data mining in the NS
discovers common features and trends of
rehabilitation treatment among hospitals and
regions. A virtual community is setup to educate and
motivate patients (Wüest et al., 2014).
2.2.1 Serious Games
A set of ten serious games is available for the
intervention. Each game offers different difficulty
levels, ranging from 1 (lowest degree of difficulty)
to 5 (highest degree of difficulty).
1. “Balloon popper”: the goal of the game is to pop
the balloons that appear on the screen. To pop the
balloons, the patient should move the hips in all
directions (shifting the weight) to reach the balloons.
NEUROTECHNIX2014-InternationalCongressonNeurotechnology,ElectronicsandInformatics
136

To score points, the patient should pop red balloons.
If the patient pops blue balloons instead, an “X” icon
appears on the screen showing that he/she made an
error. A big blue hand represents the patient’s
movements as an avatar.
2. “Bubbles”: The objective of this game is to pop
the bubbles that appear inside a cauldron. The
patient is represented as a wooden stick. The hips
are used to pop the bubbles (Figure 1).
3. “Fire fighter”: In this game a 3D avatar man
inside a barn will represent the patient. To score
points, the patient should step over a fire that
appears around him/her (in eight different
directions). To extinguish the fire, the patient needs
to stay a determined amount of time over the flame.
If the patient does not extinguish it, the hay bales
that are in the barn may burn and the patient will
lose points.
A
B
C D
Figure 1: Videogames screenshots: A. Bubbles; B: animal
hurdler; C. Fruit catcher; D. Horse runner.
4. “Animal hurdler”: The purpose of this game is to
raise the leg when some small worms approach to
the 3D avatar man. Depending on the side of the
worm approaches, the patient will need to raise the
right or the left foot (Figure 1).
5. “Fruit catcher”: The objective of the game is
to catch apples falling from the top of the tree. In
“Fruit catcher” the patient will be represented as a
3D avatar man represented in front of a tree with a
basket on the head. To catch the fruit, the patient
should shift the body weight or step to the sides. The
patient will score points when the fruits fall into the
basket placed over the avatar´s head (Figure 1).
6. “Hay collect”: The objective of this game is to
shift the body weight to the left or to the right, and
score points collecting the hay bales scattered
around the field. In this game the patient´s avatar is
driving a tractor travelling forward automatically.
The score decreases when the patient does not
collect the bales or if the avatar hits against rock
formations.
7. “Scare crow”: The objective of this game is that
the patient increases his balance and equilibrium. In
this game, a scarecrow placed in a crop field
represents the patient. Birds come from the sky to
alight upon you. If the patient moves when the birds
are approaching to the avatar, the birds will be
scared and the patient looses points.
8. “Pump the wheel”: In this game the patient should
raise both legs alternately, as previously described in
“Animal hurdler”. The patient is represented by a 3D
avatar man that operates a pump connected to an
empty flat of a tractor that is in front of the avatar.
Patient operates the pump rising and lowering the
legs at both sides alternatively. A blue arrow
indicates which leg the patient has to lift and the
height necessary to achieve points.
9. “Horse runner”: The patient has to stand up to run
faster and getting floating honey jars (it give you
points) and to sit down to run slower and avoiding
branches (Figure 1). An avatar of a man who is on
the top of a horse represents the patient. The horse is
running in the woods and advances automatically.
10. “Butterfly catcher:” The objective of this game is
to catch butterflies appearing from one side of the
screen to the other. A floating butterfly net
represents the patient, who has to use the body
movements to catch butterflies (moving the hips). If
the patient catches dragonflies instead of butterflies,
he/she looses points.
2.3 Intervention
Description of the recruitment and intervention
protocol of the pilot study is presented in Figure 2.
2.3.1 Two-Week Training at the Hospital
Patients complete a two-week training program at
the hospital to instruct patients and caregivers in the
use the REWIRE platform (Figure 3). Caregivers are
encouraged to observe hospital training sessions. It
is required that one or more caregivers attend at least
one session in order to learn to assist in the system
SeriousGames-basedSystemtoTrainWeightShiftingandBalanceafterStrokeatHome-DescriptionofaPilotStudyand
PreliminaryExperience
137
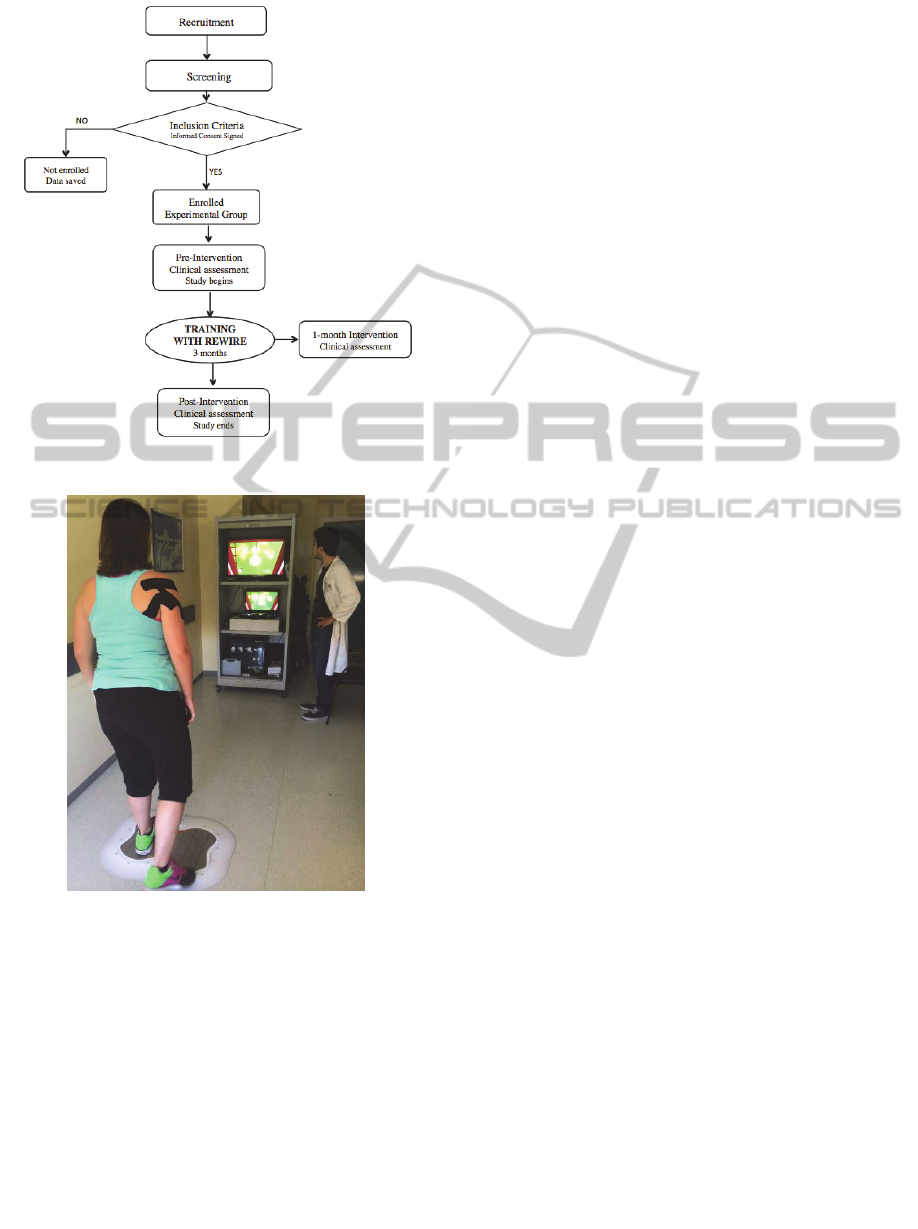
Figure 2: Pilot study flowchart.
Figure 3: Patient 1 performing a session during the two-
week hospital training.
utilization. At the end of the hospital training,
patients are able to set up the equipment correctly
and to complete a programmed session through the
PS. Patients are also instructed to solve simple issues
that may arise during sessions without assistance.
Assistance from caregivers is allowed to solve
potential issues if necessary.
Through the hospital training subjects are also
instructed in the use of the Lifestyle system.
During these two-week training, a physical
therapist defines subject’s motor and function ability
in order to program and customize sessions to
patient clinical characteristics.
At the end of these two weeks of training,
patients complete the usability questionnaire
Technology Acceptance Model (TAM). The TAM
questionnaire comprises 24 items (divided into four
sections detailed, Table 3) that are scored using a 7-
point Linkert scale ranging from “strongly disagree”
(scored as 1) to “strongly agree” (scored as 7). This
questionnaire explains the perceived usefulness and
usage intentions about a technology (Davis,
Bagozzi, & Warshaw, 1989; Davis, 1989;
Venkatesh, Davis, & College, 2000).
2.3.2 Three-Month Training at Home
After completing the two-week hospital training, the
REWIRE system is installed at patient's home to
start three-month intervention training. Three to five
sessions per week for a period of twelve weeks
(ranging from 36 to 60 session) are programmed for
every patient. The clinical team involved in the
investigation decides the number of sessions per
week for each patient, according to clinical criteria.
The length of each session time is 20 to 25 minutes
of actual training (time spent playing games). In
addition, subjects are allowed to rest as much as they
need between games.
2.3.3 Communication Between the Patient
and Clinicians
The PS includes a tool that allows for
communication between participants and clinicians
involved in the investigation through the HS. This
tool allows to participate in a forum for patients and
clinicians, to send direct messages to the therapist
and to make a video calls. Direct phone calls are
allowed in case of incidences during the session that
interfere with the training performance. The number
of phone calls made and time required for the
assistance are recorded to evaluate the usability and
costs at the end of the study.
2.3.4 Displacement to the Patient’s Home
The therapist is expected to go to the patient's home
in eight different scheduled visits (V):
- V1: the first day at the beginning of the in-home
training program to install the REWIRE system.
- V2-V7: to provide the Lifestyle system at the
beginning of the monitoring period, and to
collect the systems when done.
NEUROTECHNIX2014-InternationalCongressonNeurotechnology,ElectronicsandInformatics
138
- V8: to collect the REWIRE system at the end of
the three-months training period.
Additional visits may be necessary in case of
technical problems that cannot be solved through the
PS or phone call. Number of additional visits to
patient’s home required and time expended during
the visits is registered.
2.3.5 Outcome Measures
Clinical outcome measures are listed in table 1.
The Lifestyle System is a sensor-based wearable
system used to evaluate movement during activities
of daily living (ADLs). The system is composed of 5
IMUs (Inertial Measure Unites) that allow
evaluating movements to assess changes in the
ADLs. The objective is ubiquitous lifestyle
evaluation using ambulatory monitoring under real-
life conditions, in order to provide a multi-
parametric overview of motor functions (upper limb,
gait, and posture) and physical activity in the
patient’s daily environment. The sensors have to be
worn in the morning and carried continuously during
the day. At the end of the day they can be taken out
and attached to the Lifestyle Station through
dedicated mini-USB connector. Three assessments
with the lifestyle system will be carry out: the first
week, the seventh and the last week. During every
evaluation, subjects wear the sensors for 5 days a
week, 8 consecutive hours per day.
Two clinicians with experience in clinical
assessments measurements performed the evaluation
three times:
- T 0- before intervention: clinical assessments
and activity monitoring with the lifestyle system.
- T 1- one month after the beginning of the
intervention: clinical assessments and activity
monitoring with the lifestyle system (seventh week).
- T 3- at the end of the 3-months intervention:
clinical assessments and activity monitoring with
lifestyle system.
3 PRELIMINARY RESULTS
Fifteen eligible candidates were identified to
participate and completed the screening evaluation.
Nine out of fifteen patients were not enrolled (one
patient due to marked proprioception impairments,
one patient due to severe aphasia, two patients did
not have enough available space at home to use the
platform, two refused to participate, one did not
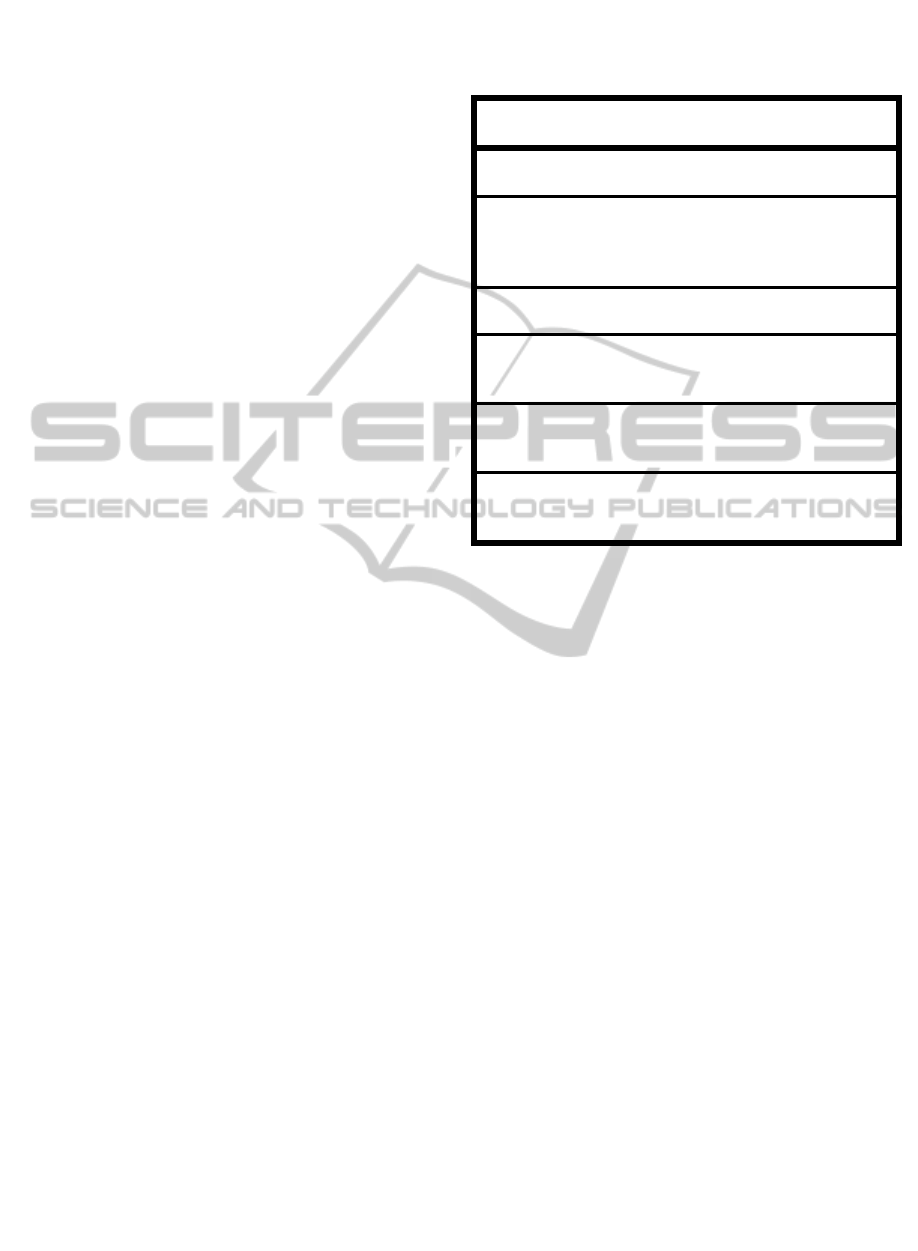
Table 1. List of clinical outcome measures evaluated in
this pilot study. Abbreviations: NIHSS, National Institute
of Health Stroke Scale; MMSE, Minimental State
Examination; ZüMAX, Zurich Maximental Status.
DOMAIN MEASUREMENT
INSTRUMENTS
Stroke deficit
severity
Fugl Meyer (lower limb)
N
IHSS
Motor Function
Berg Balance Scale (primary
outcome measure)
Six Minutes Walking Test
Ashworth
Cognitive deficit
MMSE
ZüMAX
Functional level
Barthel Index
Modified Rankin Scale
Timed Up and Go
Quality of Life
EuroQol Quality of Life Scale
(EQ5D)
Stroke Impact Scale -16 (SIS-16)
Questionnaires
TAM (Technology Acceptance
Model)
Patient Doctor Relationship
have internet connection at home, and two because
of absence of caregiver). Six patients signed the
informed consent, agreed to participate and were
enrolled in the study. After signing the informed
consent, one patient dropped out because the
primary caregiver was admitted to the hospital with
a serious illness. Three patients are performing the
in-home training phase (age, gender and diagnosis
described in Table 2) on the date of this article
submission. Baseline outcome measures of the three
patients are described in Table 3. The other two
patients already completed the two-week hospital
training.
An average of 6.16 phone calls per week made
by the patients were registered to date.
Phone calls made by patients were due to main
three reasons (ordered by frequency):
- Technical problems related to the games
during the session.
- To ask questions about the installation of the
system components
- To inform a short period missing sessions due
to vacation, illness or other personal
reasons.
SeriousGames-basedSystemtoTrainWeightShiftingandBalanceafterStrokeatHome-DescriptionofaPilotStudyand
PreliminaryExperience
139
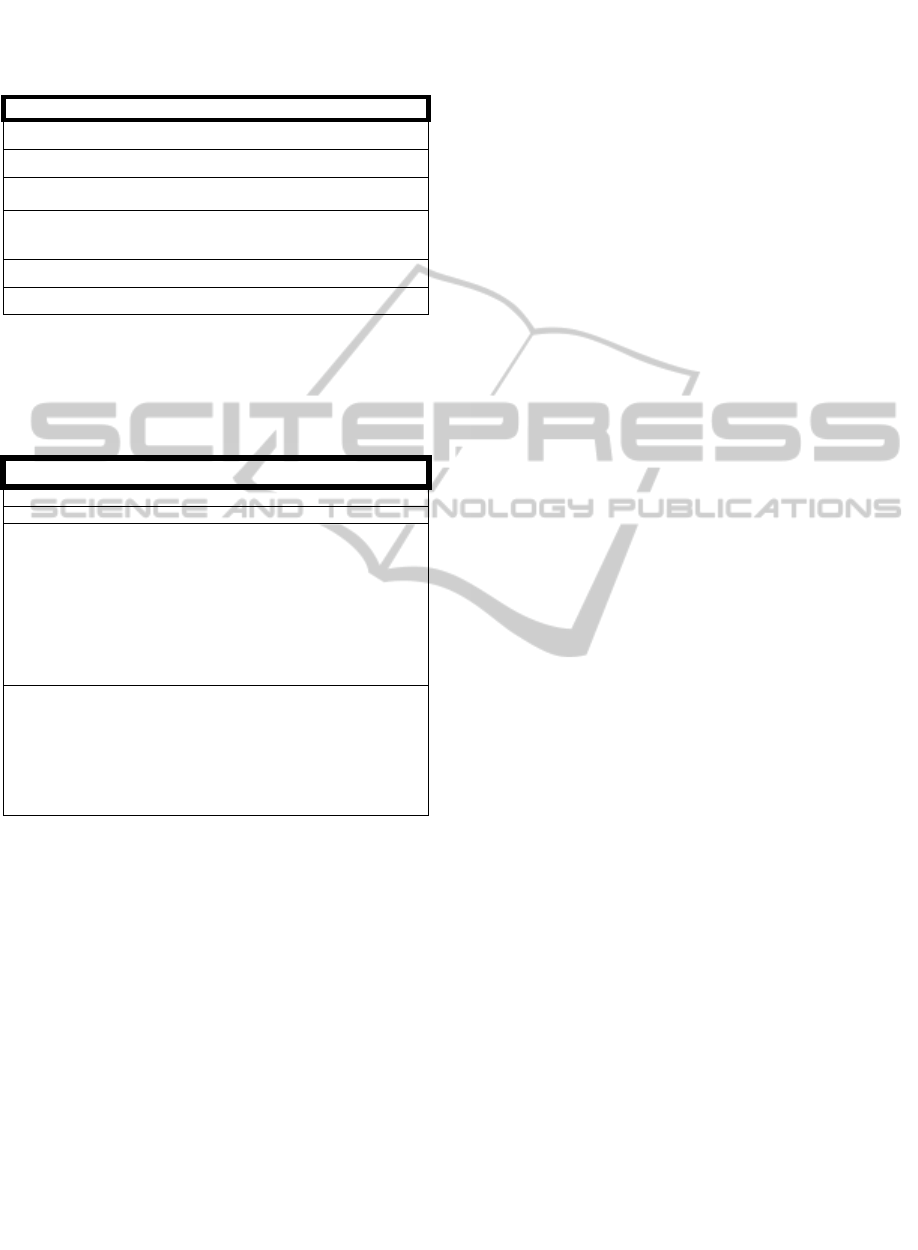
Table 2. Clinical characteristics of three patients included
in the pilot study. Abbreviations: MMSE, Minimental
State Examination; FAC, Functional Ambulation
Category.
Patient 1 Patient 2 Patient 3
Age
32 72 65
Gender
Female Female Male
Diagnosis
Left hemispheric
Ischemic Stroke
Left hemispheric
Ischemic Stroke
Right hemispheric
Ischemic Stroke
Months since
stroke
3 8 7,5
MMSE
35 25 32
FAC
5 3 3
Table 3. Baseline outcome measures and description of the
training of three patients included in the pilot study.
Abbreviations: 6MWT, Six Minutes Walking Test; m,
meters; BBS, Berg Balance Scale; TAM, Technology
Acceptance Model; SD: Standard deviation.
Patient 1 Patient 2 Patient 3
BBS
55 42 38
6MWT (m) 414 136 171
TAM
Questionnaire
- Perceived Ease
of Use
6 6.3 6.9
- Perceived
Usefulness
6.2 6.5 6.7
- Attitude
Toward Using
7 5 7
- Behavioral
Intention to Use
5.5 4.5 7
6 weeks-
training
- Sessions per
week
3.5 (3-5)
4.66 3.33
- Session
duration
(minutes)
(means ± SD)
37.01 ±
13.65
30.86 ± 8.07 29.72 ± 6.17
The phone calls made by the staff involved in the
study to contact patients were needed due to the
following reasons (ordered by frequency):
- Resolution of technical problems related the
system functioning.
- To schedule programmed therapist visits.
- To schedule visits to make the assessments.
A total of 16 visits to the patients home were
required during the first 6-weeks training, included
expected scheduled visits and additional visits,
involving an overall time of 23.75 hours (including
time for displacement and time spent at patients
home), with an average of 3.80 ± 5.29 hours per
week.
4 DISCUSSION
This paper describes the pilot study protocol and the
requirements to support and monitor the use of a
serious game-based system to train patients after
stroke at home. Three patients enrolled to date are
successfully training at home with the system,
showing good adherence to treatment and
motivation, as shown by the successful completion
of the programmed sessions. Satisfaction and good
acceptance from users is reflected by the positive
results obtained in the TAM questionnaire at the
beginning of the intervention. Phone assistance was
often required at the first stage of the in-home
training phase, but was progressively decreasing due
system modifications and adaptation successfully
implemented and to increase experience of the
patients in the use of the system.
This study goes a step beyond others studies
reported with the system because we described the
successfully transference of the training to the
patients home. Wüest et. al. (Wüest et al., 2014)
described the results of 13 elderly participants that
completed thirty-six sessions of twenty minutes with
five exergames of the REWIRE project for twelve
weeks. They found a significant improvement with
moderate to large effect sizes in Berg Balance Scale
(P = 0.007, r = 0.51) in the 7-m Timed Up and Go (P
= 0.002, r = 0.56) after training, and in the Short
Physical Performance Battery (P = 0.013, r = 0.48).
Wüest et al. described that subjects evaluated
positively the usability of the virtual reality training
intervention, assessed by the TAM questionnaire. In
contrast with Wüest et al. study protocol, which
involved the presence of an instructor during the
sessions, in our pilot study subjects complete the
sessions independently at home through the virtual
platform that allows monitoring the results at the
hospital through the HS. In the protocol of this pilot
study, individualized sessions are programmed from
the HS and are progressively adapted to subject
progresses and adherence. In addition, subjects
enrolled in our study present post-stroke residual
hemiparesis, increasing the challenge of the use of
virtual games at home.
The main challenges faced at the beginning of
the study were: frequency of system fails due to a
number of reasons related to the performance and
completion of the scheduled sessions, interaction
between the patient and objects captured by the
kinect at home and kinect calibration malfunctions.
All issues were successfully solved after some fine-
tuning adjustments and some modifications made by
the engineers and therapist participating in the study,
NEUROTECHNIX2014-InternationalCongressonNeurotechnology,ElectronicsandInformatics
140

increasing the system robustness and allowing to
perform the home program.
Study staff dedicated a significant amount of
time to attend phone calls and solve issues after
installing the system at home, especially during the
first two weeks. Although for the first weeks the
phone was the more efficient communication tool, it
is expected that all the consultations and issues will
be solved through the communication tool of the
REWIRE platform during the following weeks.
Similarly, the time spent on subjects-home visits
was variably distributed among weeks, including
some weeks where no visit was required and others
weeks that required significant in-person assistance
at patients home.
Although ideally, all stroke rehabilitation
exercises should be performed with therapist-
assisted daily practice; it is not feasible in most of
the health care systems due to the high cost of the
demand of therapists (Webster & Celik, 2014). The
final results of this study will analyze the cost
associated with the intervention and its benefit in
terms of clinical improvement and quality of life
related to health compared to conventional
rehabilitation in the hospital.
5 CONCLUSIONS
A multilevel rehabilitation platform to train balance
deficits at home has been successfully installed at
patients home. Preliminary experience shows good
adherence, satisfaction and good acceptance from
users, although close contact and feedback with the
hospital is still needed to solve initial issues. Further
studies with larger samples are needed to
demonstrate the benefits of these virtual systems for
stroke rehabilitation.
ACKNOWLEDGEMENTS
This work was partially supported by the REWIRE
project (www.rewire-project.eu), funded by the
European Commission under the FP7 framework
with contract 287713.
Author Disclosure Statement
No competing financial interests exist.
REFERENCES
Cheeran, B., Cohen, L., Dobkin, B., Ford, G., Greenwood,
R., Howard, D., … Wolf, S. (2009). The future of
restorative neurosciences in stroke: driving the
translational research pipeline from basic science to
rehabilitation of people after stroke.
Neurorehabilitation and Neural Repair.
doi:10.1177/1545968308326636
Crosbie, J. H., McNeill, M. D. J., Burke, J., &
McDonough, S. (2009). Utilising technology for
rehabilitation of the upper limb following stroke: the
Ulster experience. Physical Therapy Reviews.
doi:10.1179/108331909X12540993897892
Davis, F. D. (1989). Perceived Usefulness, Perceived Ease
of Use, and User Acceptance of Information
Technology. MIS Quarterly, 13, 319–340.
doi:10.2307/249008
Davis, F. D., Bagozzi, R. P., & Warshaw, P. R. (1989).
User acceptance of computer technology: A
comparison of two theoretical models. Management
Science, 35, 982–1003. doi:10.1287/mnsc.35.8.982
Deutsch, J. E., Brettler, A., Smith, C., Welsh, J., John, R.,
Guarrera-Bowlby, P., & Kafri, M. (2012). Nintendo
Wii Sports and Wii Fit Game Analysis, Validation,
and Application to Stroke Rehabilitation. Topics in
Stroke Rehabilitation. doi:10.1310/tsr1806-701
Feigin, V. L., Forouzanfar, M. H., Krishnamurthi, R.,
Mensah, G. A., Connor, M., Bennett, D. A., …
Naghavi, M. (2014). Global and regional burden of
stroke during 1990-2010: Findings from the Global
Burden of Disease Study 2010. The Lancet, 383, 245–
255. doi:10.1016/S0140-6736(13)61953-4
Fernández-Baena, A., Susín, A., & Lligadas, X. (2012).
Biomechanical validation of upper-body and lower-
body joint movements of kinect motion capture data
for rehabilitation treatments. In Proceedings of the
2012 4th International Conference on Intelligent
Networking and Collaborative Systems, INCoS 2012
(pp. 656–661). doi:10.1109/iNCoS.2012.66
Hung, J.-W., Chou, C.-X., Hsieh, Y.-W., Wu, W.-C., Yu,
M.-Y., Chen, P.-C., … Ding, S.-E. (2014). A
Randomized Comparison Trial of Balance Training by
Using Exergaming and Conventional Weight-Shifting
Therapy in Patients with Chronic Stroke. Archives of
Physical Medicine and Rehabilitation.
doi:10.1016/j.apmr.2014.04.029
Krause, J., Lusseau, D., & James, R. (2009). Animal social
networks: an introduction. Behavioral Ecology and
Sociobiology, 63(7), 967–973. doi:10.1007/s00265-
009-0747-0
Langhorne, P., & Duncan, P. (2001). Does the
organization of postacute stroke care really matter?
Stroke; a Journal of Cerebral Circulation, 32, 268–
274. doi:10.1161/01.STR.32.1.268
Laver, K. E., Schoene, D., Crotty, M., George, S., Lannin,
N. A., Sherrington, C., … Na, L. (2013).
Telerehabilitation services for stroke. The Cochrane
Database of Systematic Reviews, 12, CD010255.
doi:10.1002/14651858.CD010255.pub2
Loconsole, C., Bannò, F., Frisoli, A., & Bergamasco, M.
(2012). A new Kinect-based guidance mode for upper
SeriousGames-basedSystemtoTrainWeightShiftingandBalanceafterStrokeatHome-DescriptionofaPilotStudyand
PreliminaryExperience
141

limb robot-aided neurorehabilitation. In IEEE
International Conference on Intelligent Robots and
Systems (pp. 1037–1042).
doi:10.1109/IROS.2012.6386097
Morone, G., Tramontano, M., Iosa, M., Shofany, J.,
Iemma, A., Musicco, M., … Caltagirone, C. (2014).
The efficacy of balance training with video game-
based therapy in subacute stroke patients: A
randomized controlled trial. BioMed Research
International, 2014. doi:10.1155/2014/580861
Pedro, L. M., & De Paula Caurin, G. A. (2012). Kinect
evaluation for human body movement analysis. In
2012 4th IEEE RAS EMBS International Conference
on Biomedical Robotics and Biomechatronics BioRob
(pp. 1856–1861)doi:10.1109/BioRob.2012.6290751
Sandlund, M., McDonough, S., & Häger-Ross, C. (2009).
Interactive computer play in rehabilitation of children
with sensorimotor disorders: A systematic review.
Developmental Medicine and Child Neurology.
doi:10.1111/j.1469-8749.2008.03184.x
Venkatesh, V., Davis, F. D., & College, S. M. W. (2000).
Theoretical Acceptance Extension Model : Field Four
Studies of the Technology Longitudinal. Management
Science, 46, 186–204.
Webster, D., & Celik, O. (2014). Systematic review of
Kinect applications in elderly care and stroke
rehabilitation. Journal of Neuroengineering and
Rehabilitation, 11, 108. doi:10.1186/1743-0003-11-
108
Wüest, S., Borghese, N. A., Pirovano, M., Mainetti, R.,
van de Langenberg, R., & de Bruin, E. D. (2014).
Usability and Effects of an Exergame-Based Balance
Training Program. Games for Health Journal, 3, 106–
114. doi:10.1089/g4h.2013.0093
NEUROTECHNIX2014-InternationalCongressonNeurotechnology,ElectronicsandInformatics
142
