
Agent-based Modelling for Simulating Patients Flow
in a Community Hospital
Thomas Ostermann
Institute of Integrative Medicine, Witten/Herdecke University, 58313 Herdecke, Germany
Keywords: Agent-based Modelling, Hospital Management, Waiting times, Queueing.
Abstract: One of the most innovative tools in health care informatics is agent-based modelling. Such models change
dynamically and help to understand interactions in complex systems especially when simulating competitive
and cooperative behaviors in human systems. In our approach we use multi-agent modelling for simulating
and evaluating patients flow in a community hospital. The model proposed in this context consists of three
different types of agents: the hospital agent, the unit-agent and the patient-agent. Calculation of waiting
times was performed using previously collected data from elective patients entering the community hospital
ambulance. Poisson distribution was used to model waiting times. The simulation was carried out using the
JAVA-based multi-agent-modelling environment Quicksilver. After solving convergence problems, we
found, that the simulation especially for the ambulance entrance unit did show completely unexpected
results. We were able to prove that the waiting times did not solely refer to the service times of the modelled
units. To assure an unobstructed patient flow, we also showed that the mean service time at the entrance unit
should not exceed 25 min. Although no evidence was given by the isolated analysis of waiting times, the
simulation gave hints for a “hidden patient queue”, which after presenting the results in the quality circle
meeting was confirmed by the ambulance staff.
1 INTRODUCTION
Waiting times for elective (non-urgent) in- and
outpatient hospital treatment are a major health
policy concern generating dissatisfaction of patients
before their treatment has started. A recent study
from the Kopanong Hospital, South Africa found
waiting times of up to five hours due to bottlenecks
at the reception and the treatment areas (Nhlapo,
2012).
Additionally, waiting times are also economic
factors which may cause extra costs and loss of
utility (Olukotun and Ogbadu, 2013).
Especially in hopitals with interdisciplinary
ambulances which act as an interface in the patient
flow of different departments (i.e. surgery, internal
medicine) the managing of the clinic wait is an
important quality of care challenge (Rondeau, 1998).
To describe and optimize the process of patients
waiting in a hospital, methods of stochastic queuing
theory show possibilities for hospitals to optimize
clinical pathways of patients in time (Brahma, 2013;
Schwierz et al., 2011). A mathematical analysis of
waiting times of elective patients in a previous study
(Ostermann et al., 2003) found a good qualitative
agreement with the theoretically assumed results of
waiting-times-distribution. Within this theoretical
model, six homogenous groups of patients were
identified and their total waiting times were
calculated ranging from 24 to 53 minutes in the
mean which confirms the results of similar studies
(Kadivec et al., 2001; Sonnenberg, 2000).
However, this model did not explain how waiting
times of patients emerge and in which way they
depend on treatment times in the different units.
Moreover, it did not answer the question if there is
an interaction of different units within the patient
flow in the hospital.
One way of answering these question is the use
of simulation techniques to model different types of
environments. Especially for patients waiting times,
several simulation approaches do exist in the
literature. For example, Garcia et al. (1995)
presented a simulation model focussed on reduction
of waiting time in the emergency room of Mercy
Hospital in Miami. Another simulation used
complex optimization techniques of operation
research to model hospital emergency departments
queueing systems (Panayiotopoulos and
Vassilacopoulos, 1984).
14
Ostermann T..
Agent-based Modelling for Simulating Patients Flow in a Community Hospital.
DOI: 10.5220/0005178100140019
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 14-19
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)
This article presents an approach to simulate the
waiting process of patients using a combination of
queuing theory and agent-based modelling.
Agent-based modelling is a fairly new paradigm
in health care information science. Although there is
no common definition of what is called an artificial
agent, it can be described as an autonomous, social,
reactive and proactive entity, with a behaviour
predictable by attributing abstractions of
anthropomorphic attitudes (i.e. intention, obligation,
commitment, choice) to describe its behaviour
(Della Mea, 2001). Hence, a multi-agent system is a
open system, which may change dynamically, when
its agents change their behaviour or interact in
special ways. It therefore helps to understand
interactions in complex systems especially when
simulating competitive and cooperative behaviors in
human systems, which are difficult to capture in
other mathematical formalisms (Bonabeau, 2002).
Thus, agent-based modeling has become a powerful
simulation technique that has seen a number of
applications in the last few years.
In the health care sector, first attempts of using
multi agent systems concentrated in the scheduling
of operations especially in the field of organ
transplants (Moreno et al., 2001; Becker et al.,
2003). Meanwhile several applications have
demonstrated the power of agent based models in
health services research (Maglio and Mabry, 2011).
A first attempt to use agent based modeling for
hospital management simulation was presented by
Sibbel & Urban (2001).
In our approach we used multi-agent modelling
for simulating and evaluating patients flow in a
community hospital. The main question in our
approach is, whether the process of patients’ flow
itself induces the waiting times or if interactions
outside this process may be responsible for the
generation of waiting times. Therefore, we carried
out a simulation based only on the arrival times and
the service times distributions in the particular units.
On this bases we compared empirical waiting times
with the results of the multi-agent simulation.
2 MATERIAL AND METHODS
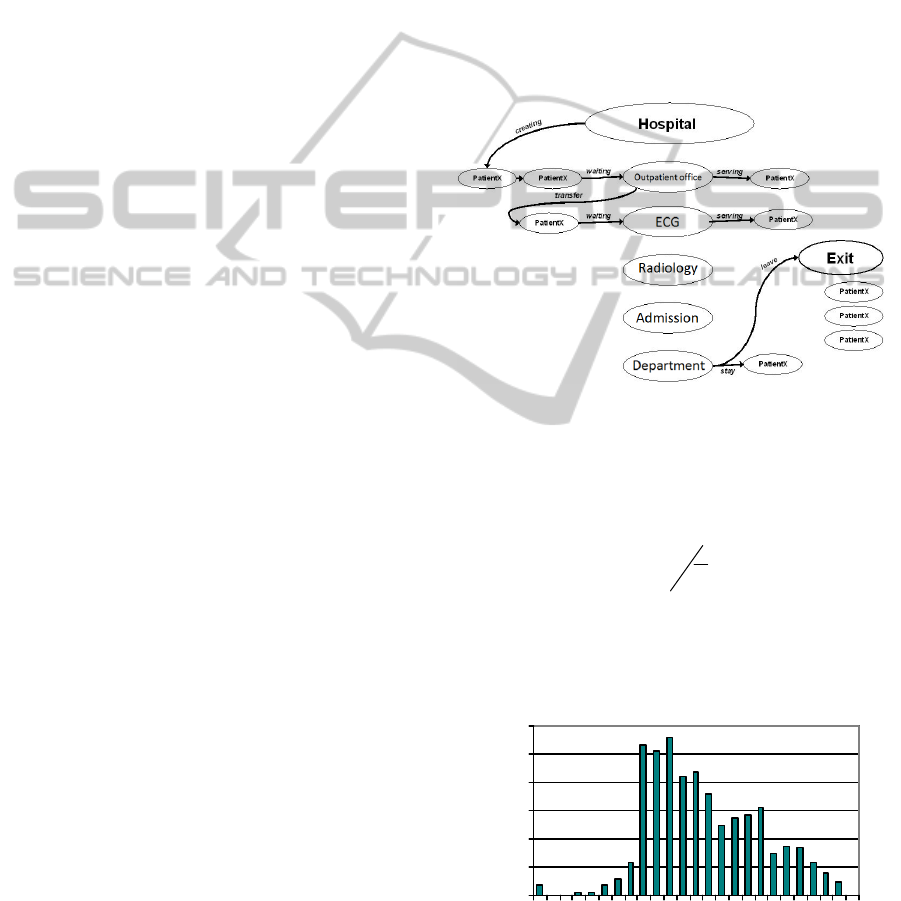
The model proposed in this context consists of three
different types of agents: the hospital agent, the unit-
agent and the patient-agent (Figure 1). The hospital
agent represents the hospital and is the models‘ root.
Here patients arrive and are sent to the “Outpatient
office”-unit. The time of the patient’s arrival is
determined by empirical data derived from
(Ostermann et al., 2003) given in Figure 2. With this
distribution a timetable is created which also defines
the exact times of arrival of the patient. As soon as it
is time for a new patient to appear, he is created by
the hospital agent. The patient’s type and his time of
arrival are determined.
The unit-agent describes a unit during the
admission. In this entity the units outpatient office,
radiology, ECG, admission-unit and departments are
described. The first four units are transient, since a
patient can be sent to another unit after passing this
one. The unit-agent holds two queues, one for the
patients waiting and one for the patients being
treated.
Figure 1: Interacting Agents of this Model.
At every moment there is exactly one patient
being treated. Each unit i is associated with a
lambda-value
i
, which is the reciprocal of the mean
service time at this unit:
i
i
T
1
It is derived from the empirical data given in
Table. 1 and generates an exponential distributed
service time, from which an individual patient’s
service time is randomly assigned.
0
2
4
6
8
10
12
0 2 4 6 8 1012141618202224
tim e in h
%
Figure 2: Empirical distribution of patients-arrivals during
the day measured for ten days.
Agent-basedModellingforSimulatingPatientsFlowinaCommunityHospital
15
The unit-agent also sends the patient to the next unit,
as soon as his treatment is completed. For this
purpose, it is necessary to find out, whether the
patient has to visit another unit. This can be decided
by the patient’s type and the units he has already
been sent to.
If the patient does not have to go to another unit,
he is inserted in the queue of treated patients and it is
decided whether he is hospitalized or discharged.
When a patient enters a unit, he is appended to
the end of the queue of already waiting patients
unless he is an emergency patient. Such patients are
treated as an exception and hence they are inserted at
the beginning of the queue. The time he has to wait
until his treatment begins, is measured and stored
into the patient-agent.
Table 1: Mean service times for the units.
Unit
Waiting time
(mean ± sd)
N
Outpatient office 29.2 ± 18.7
320
ECG 11.4 ± 8.7
89
Radiology 9.7 ± 7.9
197
Admission 9.2 ± 9.2
44
Department 25.8 ± 18.3
68
The patient-agent in this model is an agent
without any methods for acting individually i.e.
skipping a unit. Similar as in real life, he is sent from
unit to unit and just remembers his times of being
treated and of waiting. Each patient belongs to a
special type. This type specifies, whether the patient
is to be treated as an emergency, whether he is a
patient with or without transient units or if he needs
an inpatient or an outpatient treatment. The
Table 2: Groups of patients and their characteristics.
Group of patients N %
min
T
max
T
Stationary patients
directly transferred to a
hospital department
35 12,2% 37,4 37,4
Stationary patients with
one intermediate unit
27 9,4% 40,9 46,6
Stationary patients with
two intermediate units
40 13,9% 47,8 53,5
Stationary patients with
more than two
intermediate units
56 19,4% * *
Ambulant patients with
one intermediate unit
97 33,6% 24,5 27,9
Ambulant patients with
two or more
intermediate units
13 4,5% 31,4 31,4
distribution of the types was taken from the
empirical data of (Ostermann et al., 2003) and is
shown in Table 2.
The simulation was carried out using the JAVA-
based multi-agent-modelling environment Quick-
silver (Burse, 2000). Calculation of waiting times
were performed using SPSS with a Poisson-
distribution
t
etW
1)(
W(t) expresses the possibility of being served
after t minutes.
3 RESULTS
For this evaluation forty patients were simulated,
arriving at the hospital during a whole day from 0.00
h to 23.59 h. One minute is the smallest interval in
the model, since the empirical data also measure
time in minutes. Astonishingly, with the original
lambda values for the service times at the entrance
unit “Outpatient office” the model did not converge,
which means that after finishing one simulation
patients still were waiting at the entrance.
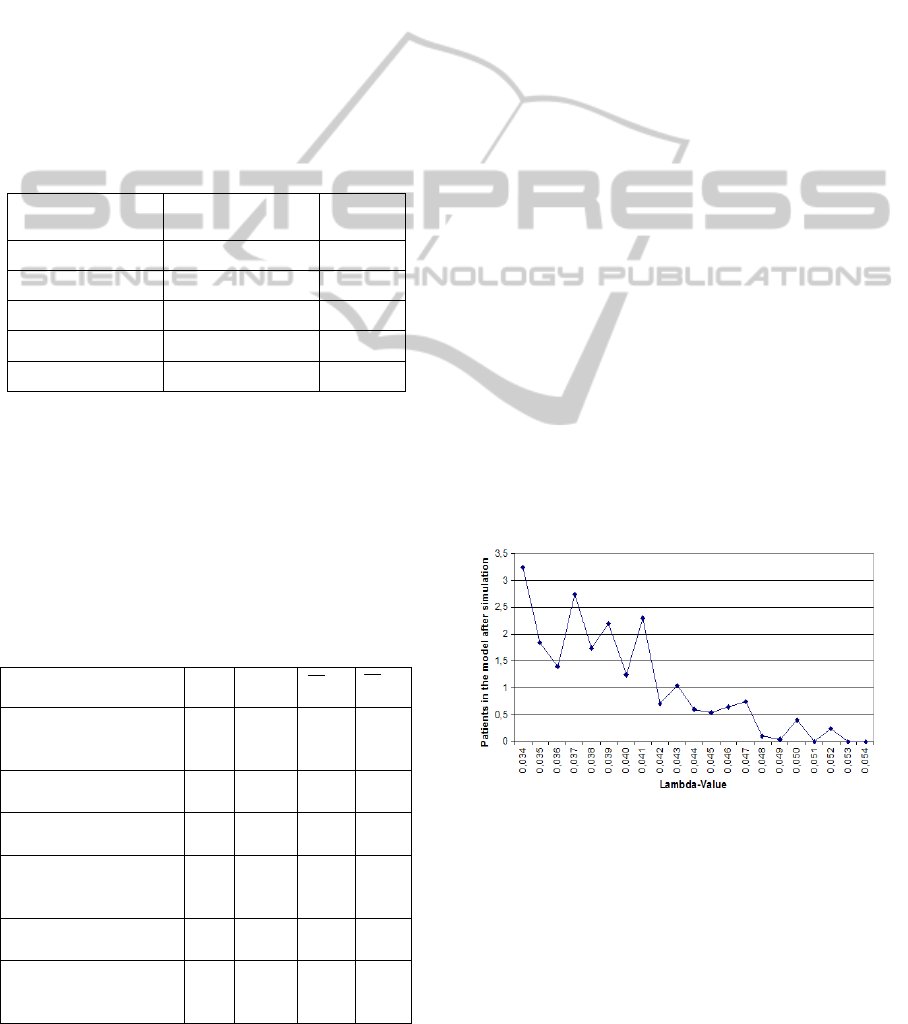
Therefore, simulations for different lambda-
values were made, with the value of lambda varying
from slightly bigger to slightly smaller than the
empirically quantified lambda. To further reduce
uncertainty, ten days with different initializations of
the random numbers were simulated for each
lambda-value. Figure 3 shows the convergence of
the model depending on the chosen lambda.
Figure 3: Convergence of the model depending on the
chosen lambda for the service time at the entrance unit.
For ≥ 0.054 the simulation did finish within the
day, thus, in the following, we compared the
empirical data with the simulation data for = 0.054
for the entrance unit “outpatient office”, which is
equivalent to a mean service time of 19 minutes.
Especially for the “Radiology”-unit but also for
HEALTHINF2015-InternationalConferenceonHealthInformatics
16
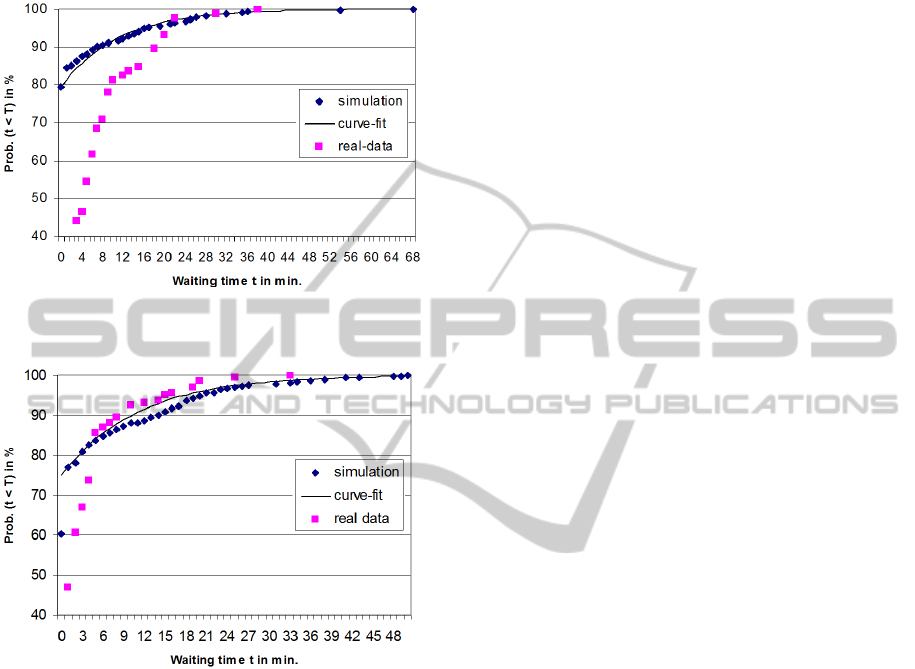
the “ECG”-unit, patients’ waiting-times were
sufficiently reproducible by the given service times
with the chosen multi-agent system. Simulated and
empirical data are given in Fig. 4 and 5.
Figure 4: Empirical and simulated waiting times for the
“ECG”-unit.
Figure 5: Empirical and simulated waiting times for the
“Radiology”-unit.
However, this agreement of simulation and
empirical data did not apply for the service times in
the outpatient-unit. The empirical mean service-
duration in the outpatient-unit was approx. 29
minutes, which lead to a lambda-value of 0.034.
This value as already stated did not lead to a
converging simulation of the patient flow. It wasn't
until a lambda-value of 0.08 when the simulation did
show sufficient similarities with the empirical data.
The best agreement was found with a lambda of
0.09, which denotes a mean service time at the
outpatient office of 11 minutes.
Thus, as a result, we found that the waiting times
are not solely generated by service times. Especially
for the ambulance unit, there have to be hidden
underlying processes beyond treatment which
explain the difference of 18 minutes between the
empirical measures mean service time of 29 minutes
and the fitting simulation result of 11 minutes.
One possible process which induces virtual
waiting time is sketched: The patient enters the
ambulance. Maybe due to misplacement, his file has
to be fetched from another unit a new file has to be
created. This will take some time whilst this patient
occasionally leaves the ambulance and the next
patient is served. Soon afterwards, the patient queues
again and is followed up after the actually served
patient.
In the empirical study, the patient has included
this interruption process into his serving time, which
by definition lasts until he is directed to the next
unit. Unfortunately, this event has not been part of
the model and thus was not reproduced in the
simulation.
4 CONCLUSIONS
Originally coming from the social science, agent-
based modelling is an innovative technique currently
used to simulate patient flows and patient scheduling
in hospital environments (Kirn et al., 2000;
Lettkemann et al., 2002; Paulussen et al., 2003;
Kanagarajah et al., 2008).
We aimed to show the possibilities of a
combination of mathematical queuing theory and
agent-based-modelling for the analysis of waiting
times in the setting of an interdisciplinary hospital
ambulance with different units visited by elective
appointed patients. After solving the convergence
problem of the simulation, we were quite surprised,
that the simulation especially for the ambulance
entrance unit did show completely unexpected
results. One reason for fluctuations in the results
might be the certainty and the stability of the model,
which is questionable, as different starting values for
the random number generator led to non-negligible
variations in the simulations.
Despite these structural problems of the
simulation, we could prove that the waiting times
did not solely refer to the service times of the
modelled units. To assure an unobstructed patient
flow, we also showed that the mean service time at
the entrance unit should not exceed 25 minutes.
Although no evidence was given by the isolated
analysis of waiting times, the simulation gave hints
for a “hidden patient queue”, which after presenting
the results in the quality circle meeting was
confirmed by the ambulance staff.
For further research the implementation of a
patient satisfaction function is a reasonable
Agent-basedModellingforSimulatingPatientsFlowinaCommunityHospital
17

enhancement of the proposed model. Empirical
studies like those carried out by Spaite et al. (2002)
found high correlations between the decreases in
waiting time intervals and improvement in patient
satisfaction. From the mathematical point of view
this correlation can be modelled by using a logistic
regression model, where the satisfaction s is a
function of the waiting time t (Hackl and Westlund,
2000):
ct
e
ts
1
1
)(
; t = waiting time.
The parameter c models the patients reactivity on
waiting and is randomly assigned to the patient
agent which cumulates the waiting times t
i
of each
station. Thus, some patient will show a bad temper
after waiting only a short time at one unit whilst
others will keep their head although they have high
waiting times at all units (Pruyn and Smidts, 1993).
If then an individually assigned threshold value i.e.
s=0.7 is passed, this could prompt the patient agent
to file a complaint to the hospital. Since the
incoming complaints increase, this leads to quality
measures to lower the service times at the units by
increasing the lambda-values. This would lead to a
model with a feedback loop, which can be used to
simulate special scenarios like queuing of elderly
patients (Andersson et al., 2011).
Apart from the analysis of waiting times, such
models can also provide useful insights when being
used e.g. to simulate patients’ drug compliance and
behaviour in outcome studies. Such a system for
planning, management and decision support of
clinical trials has recently been proposed by Heine et
al. (2005).
ACKNOWLEDGEMENTS
I would like to thank Georg Johann, University of
Osnabrück, Germany for his support in
programming the model in Quicksilver.
REFERENCES
Andersson, L., Burman, M., Skär, L., 2011. Experiences
of caretime during hospitalization in a medical ward:
older patients’ perspective. Scandinavian journal of
caring sciences, 25(4), 646-652.
Becker, M., Krempels, K.H., Navarro, M., Panchenko, A.,
2003. Agent Based Scheduling of Operation Theaters.
Proceedings des EU-LAT E-Health-Workshop,
Mexiko.
Bonabeau, E., 2002. Agent-based modeling: methods and
techniques for simulating human systems. Proc Natl
Acad Sci USA; 14;99 Suppl 3:7280-7.
Brahma, P. K., 2013. Queuing theory and customer
satisfaction: a review of terminology, trends, and
applications to hospital practice. Asia Pacific Journal
of Marketing & Management 2(6): 83-89.
Burse, J., 2000. Quicksilver: A Component-Based
Environment for Agent-Based Computer Models and
Simulations. In Computational Social Organisational
Science Conference, CASOS, Pittsburgh, PA.
Della Mea, V., 2001.Agents acting and moving in
healthcare scenario: a paradigm for telemedical
collaboration. IEEE Transaction on Information
Technology in Biomedicine: 5; 10-13.
Garcia, M.L., Centeno M.A., Rivera, C., DeCario, N.,
1995. Reducing Time in an Emergency Room via a
Fast-Track. In Proceedings of the 1995 Winter
Simulation Conference, Alexopoulus, Kang, Lilegdon
& Goldman (eds.): 1048-1053.
Hackl, P., Westlund, A. H., 2000. On structural equation
modelling for customer satisfaction measurement.
Total Quality Management, 11(4-6), 820-825.
Heine, C., Herrler, R., Kirn, S., 2005. ADAPT@Agent.
Hospital: Agent-Based Optimization & Management
of Clinical Processes. International Journal of
Intelligent Information Technologies 1, 30-48.
Kadivec, S., Eržen, D., Šorli, J., 2001, Waiting times in
the University hospital. ZDRAV VESTN; 70: 391–4.
Kanagarajah, A. K., Lindsay, P., Miller, A., Parker, D.,
2008. An exploration into the uses of agent-based
modeling to improve quality of healthcare. In Unifying
Themes in Complex Systems (pp. 471-478). Springer
Berlin Heidelberg.
Kirn, S., Heine, C., Petsch, M., Puppe, F., Klügl, F.,
Herrler, R., 2000. Agentenorientierte Modellierung
vernetzter Logistikkreisläufe als Ausgangspunkt
agentenbasierter Simulation – Beispiel
Wöchnerinnenstation. In Kirn, St.; Petsch M. (Eds.):
Proceedings 2. Kolloquium des DFG-Schwerpunkt-
programms „Intelligente Software-agenten und
betriebswirtschaftliche Anwendungs-szenarien“
Ilmenau, Germany.
Lettkemann, E., Meister, M., Hanft, A., Schröter. K.,
Malitz, R., 2002. The Description of Practical Roles in
Hospital Environments. In Lindemann G, Jonker C,
Timm IJ (Eds.): Proceedings of the KI'2002 Workshop
on Modelling Artificial Societies and Hybrid
Organizations MASHO'02 2002, Aachen, Germany;
29-36.
Maglio, P. P., Mabry, P. L., 2011. Agent-based models
and systems science approaches to public health.
American journal of preventive medicine, 40(3), 392.
Moreno, A., Valls, A., Bocio, J. A., 2001. Multi-Agent
System to Schedule Organ Transplant Operations.
Inteligencia Artificial, Revista Iberoamericana de IA
2001; 13: 36- 44.
Nhlapo, M. T., 2012. The appraisal of factors affecting
waiting times and recommendations for improvement
at out-patient department (OPD) of Kopanong
HEALTHINF2015-InternationalConferenceonHealthInformatics
18

Hospital. Doctoral dissertation, Faculty of Health
Sciences, University of the Witwatersrand.
Olukotun, G. A., Ogbadu, E. E., 2013. The Applications
Of Waiting Line Management On The Operations Of
Public Sector Organizations: The Kogi State Health
Sector Experience (2009-2012). International Journal
of Research in Business and Technology, 3(3), 252-
265.
Ostermann, T., Priegnitz, O., Jochheim, R., 2003.
Mathematical Analysis of Patient’s Waiting Times in
Clinical Pathways of an Interdisciplinary Ambulance.
Gesundh ökon Qual manag; 8(6): 379-384.
Panayiotopoulos J.C., Vassilacopoulos, G., 1984.
Simulating hospital emergency departments queueing
systems. Eur. J. Oper. Res., 18: 250-258.
Paulussen, T.O., Jennings, N.R., Decker, K.S., Heinzl, A.,
2003. Distributed patient scheduling in hospitals.
Proceedings of 18th International Joint Conference on
Artificial Intelligence, Acapulco, Mexico; 1224-1229.
Pruyn, A., Smidts, A.,1993. Customers’ evaluations of
queues: three exploratory studies. European Advances
in Consumer Research, 1, 371-382.
Rondeau, K., 1998. Managing the clinic wait: an important
quality of care challenge. J Nurs Care Qual; 13: 11–
20.
Schwierz, C., Wübker, A., Wübker, A., & Kuchinke, B.
A., 2011. Discrimination in waiting times by insurance
type and financial soundness of German acute care
hospitals. The European Journal of Health Economics,
12(5), 405-416.
Sibbel, R., Urban, C, 2001. Agent-based modeling and
simulation for hospital management. In Theory and
Decision Library Vol. 32, pp 183-202. Springer
Netherlands.
Sonnenberg, A., 2000. Waiting lines in the endoscopy
unit. Gastrointest Endosc; 52(4):517-24.
Spaite, D.W., Bartholomeaux, F., Guisto, J., Lindberg, E.,
Hull, B., Eyherabide, A., Lanyon, S., Criss, E.A.,
Valenzuela, T.D., Conroy, C., 2002. Rapid process
redesign in a university-based emergency department:
decreasing waiting time intervals and improving
patient satisfaction. Ann Emerg Med. 39(2):168-77.
Agent-basedModellingforSimulatingPatientsFlowinaCommunityHospital
19
