
An Observational Study to Improve the Surgical Safety Checklist
Viability
V. Estima
1
, A. Castro
2
, P. Gomes
3
, V. Nunes
4
and D. Pereira
3,5
1
Instituto Superior de Engenharia do Porto, Instituto Politécnico do Porto, Porto, Portugal
2
Faculdade de Engenharia, Universidade do Porto, Porto, Portugal
3
Instituto de Telecomunicações, Universidade do Porto, Porto, Portugal
4
Hospital Prof. Doutor Fernando Fonseca, EPE, Amadora, Portugal
5
Faculdade de Medicina, Universidade do Porto, Porto, Portugal
Keywords:
Surgical Safety Checklist, Evaluation and Use of Healthcare IT, Electronic Health Records and Standards,
e-Health.
Abstract:
To improve safety, and to reduce the mortality and complication rates during surgeries, the World Health
Organization developed the Surgical Safety Checklist (SSC). The SSC has been recently implemented in
Portuguese hospitals and we have performed an observational study where several health professionals were
observed during their normal surgical routine and interviewed. The objective of this study was to understand
the current use of the SSC, and how it may be improved in terms of usability, taking advantage of current
technological advancements. During two days, in a public health center in Portugal, a clinical team (surgeons,
anesthesiologists and nurses) was observed in 14 surgeries. Some observations disclose that several health
professionals are not familiarized with the SSC guidelines, which demonstrates that it is urgent to change the
mindset of health professionals, and that the addition of some features in the SSC may be necessary. With the
results of the observational study, we have designed and developed a web application for the SSC with new
functionalities to improve and aid the health professionals in its use.
1 INTRODUCTION
The Surgical Safety Checklist (SSC) is a support of
information that helps humans to reduce mistakes,
compensating for the possible limits in his memory
and attention. In other words, the checklist guaran-
tees consistency and entirety in the realization of a
task (Emerton et al., 2009). The use of checklists is
broad in fields such as aviation, and more recently in
clinical settings.
The concept of a checklist was first introduced by
the administration and engineers of the Boeing Cor-
poration, in sequence of the prototype B-17 accident
(1935) in the field of Wright, in Dayton, Ohio, killing
two pilots. The investigation showed that the plane
did not present any mechanical problem, and that the
accident was caused by human error. The Boeing
Corporation confronted with this problem, developed
and implemented a checklist, and the B-17 aeroplane
flew more 1.8 million miles without further incidents
(Downey, 2010),(Schamel, 2012). It is estimated that
surgeries on the wrong body part, and to the wrong
patient take place in around 1 in each 50000 to 100000
proceedings in the United States of America (USA),
representing 1500 to 2500 adverse events of this type
yearly (Kwaan et al., 2006).
Between 2007 and 2008, inspired by the aviation,
the World Health Organization (WHO), identifying a
problem with surgical complications and errors, cre-
ated the programme “Safe Surgery Saves Lives” to
improve the surgical safety and to reduce the num-
ber of deaths and surgical complications. Within
this programme the WHO developed the SSC, and
it was tested between October 2007 to September
2008‚ in a multicentric study (8 hospitals in 8 differ-
ent cities: Toronto‚ Nova Deli‚ Amman‚ Auckland‚
Manila‚ Ifakara‚ London and Seattle). After the intro-
duction of the checklist, the incidence of patient com-
plication lowered from 11.0% to 7.0% (P<0.001),
and the rate of death declined from 1.5% to 0.8%
(P = 0.003) in all institutions (Haynes et al., 2009).
In a different study, it was observed that after
390
Estima V., Castro A., Gomes P., Nunes V. and Pereira D..
An Observational Study to Improve the Surgical Safety Checklist Viability.
DOI: 10.5220/0005215303900396
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 390-396
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

the SSC introduction the nurses recognized that pa-
tients identity was more often confirmed (81.6% to
94.2%, P<0,01), and the anesthesiologists were bet-
ter aware of available cross-matched blood and of
due checking of anesthesia equipment. This study
also stated that anesthesiologists discussed more often
the possible critical events with surgeons (of 22.0%
for 42.6%, P<0.001) after the post-operative (Takala
et al., 2011).
In June 2010, in Portugal, the “Direção-Geral da
Saúde” (DGS) in the use of the technical or normative
norms, determined the implementation of the “Safe
Surgery Saves Lives”, in all the operation rooms (OR)
of the National Health System until the end of the
September 2010 (George, 2010). In 2011 the im-
pact of the SSC in 5 Portuguese hospitals was stud-
ied. The authors observed, after interviewing 153
health professionals, that 41.6% did not know the
SSC. Another interesting result is that before Septem-
ber 2010 (mandatory adhesion by all the OR to the
SSC) just one hospital had implemented the SSC
(Valido, 2011). In June 2013, a circular normative
has been issued reinforcing the mandatory implemen-
tation of the project “Safe Surgery Saves Lives” in ac-
cordance with the “Implementation manual - Surgical
Safety Checklist” (George, 2013).
Knowing this, there is a need to understand the
workflow of the SSC in Portuguese hospitals and the
difficulties felt by the users. All due to the importance
of patient safety, since that surgical procedures are an
integrant part of healthcare systems all over the world.
1.1 The Surgical Safety Checklist (SSC)
The Surgical Safety Checklist (SSC) divides the
surgery in three phases, each one corresponding to a
specific period in the normal flow of the surgery: the
period before induction of anesthesia; the period after
induction and before skin incision; and the period dur-
ing or immediately after the wound close, but before
patient leaves the room. To ensure the fulfilment of
the SSC one person should be designated to verbally
check all the steps and actions with the team, usually
the circulating nurse but it may be any element of the
team, by the checklist coordinator.
In the first phase (before induction of anesthesia)‚
at least one nurse and one anesthesiologist must be
present. In the second (before skin incision) and third
(before patient leaves operating room) phases all the
participants should be present, nurses, anesthesiolo-
gists and surgeons.
2 OBSERVATIONAL STUDY AND
INTERVIEWS
METHODOLOGY
This observational study was performed at public
health center in Portugal, after institutional approval.
During two days the clinical team in one of the hospi-
tal’s operating rooms (OR) was observed during their
standard clinical practice. This observational study
encompassed 14 surgeries, and the clinical team was
not aware of the true intent of the observer. After the
observational study a set of questions were made to
the intervenients and other related professionals.
2.1 Observational Study
The observations aimed to understand the functioning
of the SSC in the OR during the standard clinical rou-
tine, and observe how the different health profession-
als were involved in this task, surgeons, anesthesiolo-
gists and nurses. In this study, the observer degree of
involvement and relation to the observed was consid-
ered to be passive. He was not directly involved in the
situation that was observed, meaning, the observer did
not interact, neither intentionally affected the object
of observation (bystander). In addition, the partici-
pants did not knew the objective of this observational
study. The observer focused on the same points of
interest in all interventions:
• At what surgery stage is recorded each SSC phase;
• Which health professionals register each checklist
phase;
• Are all items of the SSC read out loud;
• Are there items of the checklist said out loud that
are not registered immediately after.
This information was registered throughout the
surgical interventions.
2.2 Interviews
After the observational study, the researcher con-
ducted the interviews to these professionals, using a
semi-structured approach. One of the objectives of
the semi-structured interviews was to know the opin-
ion of health professionals on the use and utility of
the SSC. The respondents were surgeons, anesthesi-
ologists and nurses in the same OR of the observa-
tional study. The semi-structured interviews followed
a previously prepared questionnaire that served as a
guideline, with no strict order of questions, manag-
ing to adapt the development of the interview to the
respondent, ensuring that participants responded to
AnObservationalStudytoImprovetheSurgicalSafetyChecklistViability
391
these same questions outlined, but with a high degree
of flexibility depending on the answers given. The
guideline was as follows:
• What is your profession?
• Is the SSC used in the operating rooms of your
hospital according to the rules explained in the
WHO manual:
– Each item of SSC is validated at the time that
statement is read?
– How is the validation performed (item by item,
phase by phase, all at once)?
– All questions are listed in the predetermined or-
der?
• In your opinion, are all the questions correctly for-
mulated?
• Did the checklist change the way you work?
• In your opinion, what are the benefits and disad-
vantages of implementing the checklist, defined
by WHO / DGS in 2010?
• In your opinion, would it be advantageous to
adapt the checklist to each type of surgery?
• In your opinion, would it be advantageous to use
a Tablet / Smartphone for implementing the SSC?
In addition of the health professionals, the IT pro-
fessionals of the hospital were also interviewed. The
semi-structure guideline of the interviews followed
the same rules of the script for the health profession-
als. The questions were as follows:
• In your opinion, would it be advantageous to
adapt the SSC to each type of surgery?
• In your opinion, would it be advantageous to use
a Tablet/Smartphone for implementing the SSC?
• Do external application may be added into the
hospital software?
The answers to the questions made were not
recorded by any kind of device, we just took notes
during an interview, compiling them right after.
3 RESULTS
The clinical setting observed was one of the opera-
tion rooms (OR) of the 11 available at the hospital.
Surgical interventions in this hospital cover several
medical specialties such as General Surgery, Orthope-
dics and Traumatology, Gynecology, Urology, Pedi-
atric Surgery, Otorhinolaryngology, Ophthalmology,
Plastic Surgery and Maxillofacial Surgery.
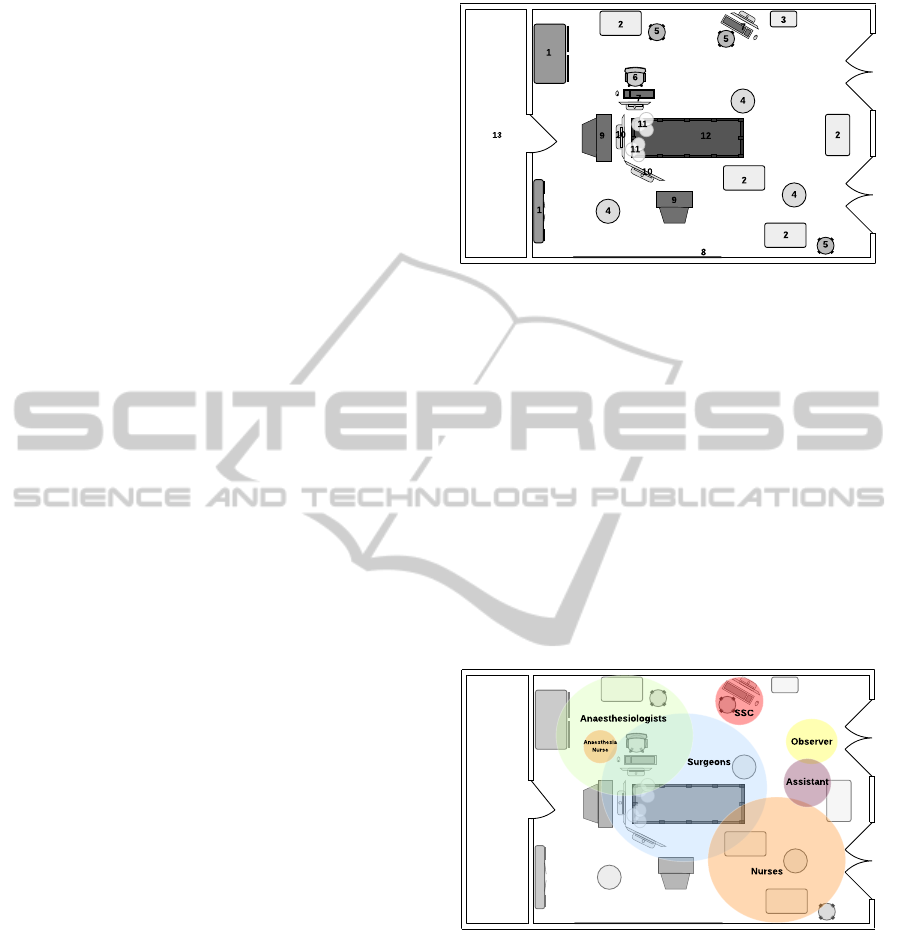
Figure 1 presents an overview of the OR were the
observational study took place. It is possible to see the
Figure 1: Operating Room (view from the top): 1. anesthe-
sia material and equipment cabinet; 2. surgical and anaes-
thesia equipment/material trolleys; 3. refrigerator with ma-
terial; 4. trash cans; 5. stools; 6. chair; 7. computers;
8. white board, and x-ray light; 9. surgical equipment; 10.
ventilator and anaesthesia monitors; 11. surgery lights; 12.
operating table; 13. sterilization room.
setting organization, and display of the material in the
available space, including the material trays, anesthe-
sia monitors and ventilator, operating table and sup-
port tables.
Figure 2 presents the action zones for each actor
inside the OR. This observation can help us to under-
stand why and how each actor interacts with the SSC
and if we can adjust the guidelines to their current
methodology.
Figure 2: Zones of action inside the Operating Room (view
from the top) for each actor.
3.1 Observation
On the first day, the study was performed during the
morning period, from 10:30 am to 2:30 pm, and af-
ternoon period, from 3:30 to 9:30 pm. The observer
was present in 4 surgeries through the entire process
of the Surgical Safety Checklist (SSC), and in 4 surg-
eries for some of the parts of the procedure. On the
second day, during the afternoon period, from 04:00
pm to 8:30 pm, the observer was present in 6 surgeries
HEALTHINF2015-InternationalConferenceonHealthInformatics
392
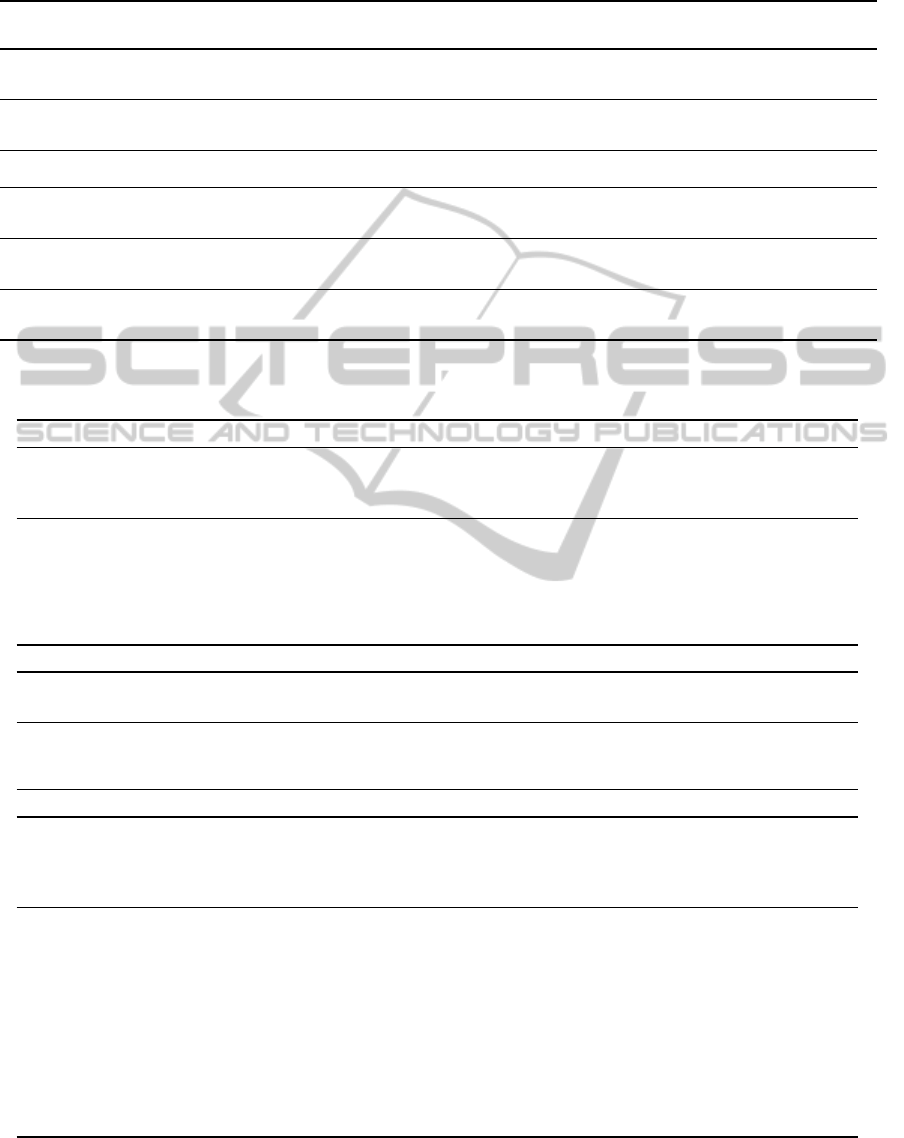
Table 1: Observations to the Surgical Safety Checklist usage in the operating room at a public health center. In this table
we can see, for each surgery, what stages of the Surgical Safety Checklist where properly done and what was not done in
accordance with the guidelines.
Surgery ID
Items with-
out immediate
registration
Sign In Time Out Sign Out Actors Read Aloud
1st and 8th _______ During surgery During surgery
Before patient
leaves operating
room
Circulant Nurse or Circulant and In-
strumentalist Nurse
Only the items that were unknown
to the user or no item
2nd Sign In Anaesthesia
When anaesthe-
sia
Before patient
leaves operating
room
Circulant Nurse and Surgeon in
Sign Out
Only Sign Out
3rd, 6th and
9th
Sign In During surgery During surgery During surgery Circulant Nurse No item
4th, 5th,
7th, 10th
and 11th
Sign In
Before patient
leaves operating
room
Before patient
leaves operating
room
Before patient
leaves operating
room
Circulant and Instrumentalist Nurse
or Anaesthetist Nurse
No item or Anticipated blood
loss and completion of instrument,
sponge and needle counts
12th Sign In, Time Out During surgery During surgery
Before patient
leaves operating
room
Circulant Nurse Time Out and Sign Out
13th
and14th
_______
Before induction
of anaesthesia
Before skin inci-
sion
Before patient
leaves operating
room
Circulant Nurse All itens
Table 2: Pros and cons retrieved from the interviews to the health professional (surgeons, anesthesiologists and nurses) about
the Surgical Safety Checklist use.
Nurses
Pros
"The use of the checklist is important and should be enforced properly"
"If the checklist was a team work, this time would not be a waste, and its use would be improved"
The adaptation of the checklist to the type of surgery would be a good solution
Cons
At the beginning of the implementation of the checklist, professionals complied with the rules of the
user manual, but due to the attitudes of some surgeons they have stopped doing it
The collaboration of surgeons is scarce
The registration of the checklist in the hospital software is done by these professionals, their names can
be held liable if an incident occurs
The use of a mobile application would not improve the functioning of the checklist
Anesthesiologists
Pros
"The use of the checklist is important and should be enforced properly"
The adaptation of the checklist to the type of surgery would be a good solution
Cons
The use of a mobile application would not improve the functioning of the checklist
The checklist is not used properly because no one is blamed if an incident occurs due to lack of data
completion
Surgeons
Pros
The adaptation of the checklist to the type of surgery would be a good solution
"It is a memory aid, because we are human and we all fail"
"The first questions should be asked before the patient is sent down to the operating room, and surgeons
should have access to them"
Cons
It is difficult to apply the checklist when experienced health professionals do not set an example, espe-
cially to the younger ones
It is necessary to change minds, they are aware that many colleagues do not collaborate with the nurses
"If anyone who did not fill up the checklist, or did not cooperate in their fulfillment was punished, it
was possible to work"
Demotivation of health professionals with the health system at the moment (possible justification for
not completing the checklist)
"When there are new implementations, especially surgeons, are very reticent"
"It would take several serious incidents to open the minds of these professionals"
Many of the resident surgeons, do not know the function of the checklist
"There is always a way to not comply with the rules of the checklist or other computerized program"
AnObservationalStudytoImprovetheSurgicalSafetyChecklistViability
393

through the entire SSC process. Table 1 summarizes
the observed procedures regarding the checklist use in
the two days.
In the two days of the observation, and of the 14
observed surgeries, only 2 surgeries met the require-
ments for the three phases of the SSC, as defined by
the WHO. Of the remaining 12 observed surgeries, 9
surgeries completed the last phase at the correct time.
The SSC was always filled by any of the nurses that
were available, except for a surgery in which a sur-
geon helped the nurses to fill one of the last phases.
It was also observed that only in 2 surgeries all
the phases of the SSC were read aloud to the team.
In the remaining surgeries, in 4 of them some of the
phases were read aloud and in 8 of them none of the
phases were read aloud to the team. We also observed
that, in 7 surgeries, several items were read aloud and
answered but no one was checking the SSC, only after
the end of the phase.
3.2 Interviews
I the end of the two days, several health professionals
and technicians (surgeons, circulating nurses, anes-
thesiologists and IT) were interviewed by the same
observer. Their opinions are presented in Table 2.
In general, the circulating nurses have the opinion
that the use of the SSC is very important, but reported
that not all health professionals involved collaborate
the same way. When the SSC became mandatory they
tried to follow with all the rules of the World Health
Organization (WHO), but due to lack of cooperation
of the surgical team, they decided to stop asking a few
items aloud, stating: “if the SSC was a team work, this
time would not be a waste, and its use would be im-
proved”. In their opinion, a mobile application would
not help to improve the functioning of the SSC. They
consider that the SSC could be adapted to each type
of surgery, for example, they consider that the iden-
tification of all team members by name and role, in
most of the Portuguese hospitals would be unneces-
sary, because usually the teams are known to each
other. Other example is the different materials used,
depending on the type of surgery that the SSC request
to confirm in the last phase.
The anesthesiologists were also in favor of the
SSC and in their opinion, the main reason for the low
commitment to not follow the rules according to the
WHO guidelines, is that nobody wants to be held re-
sponsible in case of a preventable complication: “it is
filled according to some of the rules but I admit that
not all of them, there is not a lot of rigour in its regis-
ter”. The anesthesiologists also do not find the use of
a mobile application a surplus value for the SSC, but
quite the opposite, stating that the adaptation of the
SSC would be a good improvement.
All the surgeons that have participated in the surg-
eries(orthopedics, urology and plastic surgeons) were
interviewed, and presented very divergent opinions.
Some considered that the use of SSC is very impor-
tant for the safety of the patient, mainly in the points
of the laterality and identification, but recognize that
many health professionals, mainly the surgeons, still
have not adapted to its use. Also, they stated that
if in the case of complications, if the SSC was used
to find the reason of the problem, they would rapidly
change their attitude towards it. Other surgeons state
that the SSC may be important but they do not usually
do it. Actually they consider that the years of expe-
rience are more important than a single SSC. Finally,
one of the problems cited is the fact that “the register
of the SSC or any register was easier when done in
paper when compared to a computer program”. Re-
garding the mobile application, they consider it to be
useful in the confirmation of the material and equip-
ment necessary for the procedures, so the nurses could
register that information in the place where the mate-
rial is stored. The SSC adaptation to different surgery
types, in their opinion, would be ideal, since they con-
sider some items superfluous.
The IT staff of the hospital was surprised with the
observations because they never thought that the pro-
fessional were not complying with the WHO guide-
lines. Also, they explained that it is possible to adapt
the SSC software available at the hospital to a new
application (software that may for example adapt the
SSC for each type of surgery), after approval from
“Direção-Geral da Saúde” (DGS).
4 SURGICAL SAFETY
CHECKLIST APPLICATION
PROPOSAL
After an analysis of the results obtained in the obser-
vational study, and the opinions gathered in the inter-
views, the next step of this study was the development
of a SSC application responding to the health profes-
sionals requests, that may be adapted to the type of
surgery, and easily introduced in the hospital’s sys-
tem. We have chosen an web approach due to all
the advantages of this platform (Umbach, 2004; Man-
freda et al., 2002).
In this application the user can chose between a
SSC already created to a specific surgery or to create
a new SSC, adding and adapting some questions from
the World Health Organization (WHO) standard. In
HEALTHINF2015-InternationalConferenceonHealthInformatics
394
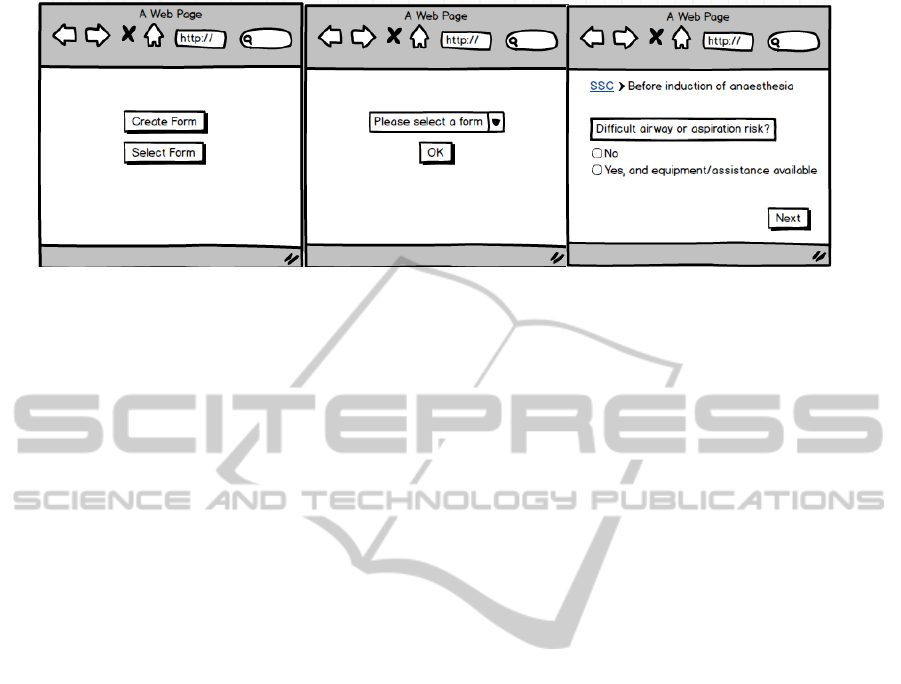
Figure 3: Mockup layouts of the web proposal. In this mockup it is possible to see some of the improvements proposed
mainly in the third layout you can see the single question at time, the progress bar and the no go back option.
this proposal the improvements are focused in forcing
the user to focus in the workflow of the SSC and to
save the input timestamps and any actions made by
them. Therefore, we believe that the following fea-
tures implemented will achieve that goal (see figure
3).
• Display one item of the SSC at a time. This fea-
ture will force the user to focus on the question at
hand and will not allow the user to answer other
questions out of order;
• Display the stage where the SSC is, so the user
knows what he is doing and to help him, guiding
him through the SSC;
• Do not allow going back to the previous step. This
feature forces the user to be fully aware of his an-
swers. In this feature we will implement some
safeguards such as highlighting the answers and
only allowing keeping forward some time after the
answer is given. A go back button should be im-
plemented anyhow, but the user will be informed
that that action will be registered as a forced go
back requested by the user;
• Do not allow going forward to the next item if the
current is not filled;
• Do not allow going forward to the next item if the
time it took to fill the item was too short. This
feature tries to stop random inputs to just force
the SSC to go further, or to prevent any by heart
input;
• Log any action made by the user. This feature will
allow to access if the SSC is being filled properly
according to the WHO guidelines.
5 DISCUSSION AND
CONCLUSIONS
The surgical treatment is an integrant part of health-
care systems all over the world‚ with a respected value
of 234 million fulfilled surgeries‚ annually (Haynes
et al., 2009). Preventable surgical complications rep-
resent a large percentage of injuries and deaths world-
wide. It is estimated that adverse events affect 3 to
16% of all hospitalized patients, 3% of those adverse
events occurring during surgery and 0.5% ending in
mortality, i.e. almost 7 million patients have signifi-
cant surgical complications where each year 1 million
will die during or immediately after surgery (Kable
et al., 2002), (Gawande et al., 1999). It very impor-
tant that all health professionals comply with the rules
of the WHO manual because this numbers can be re-
duced with a simple gesture of teamwork.
The positive points of the observational study
were the full collaboration of the healthcare profes-
sionals involved, and also from the IT team of the hos-
pital. Also, observing the SSC use was of paramount
importance in the understanding of the entire process
at the operating room. It should be highlighted, that
due to the study design and specificity, data volatil-
ity may be an issue, since everything was noted down
and not recorded, and in the operating rooms several
simultaneous events were happening at the same time
which may have led to missed events.
The results of the observational study, indicate
that the SSC is not properly filled, in the majority of
times, according to the WHO guidelines. It is con-
cluded that it is urgent to change the mindset of many
health professionals, and that there is a need to raise
awareness to the SSC impact, through, for example,
interventions to various undergraduate courses related
to healthcare, or lectures from aviation profession-
als as a parallel example of the checklists successful
AnObservationalStudytoImprovetheSurgicalSafetyChecklistViability
395

used. We also believe that more hearings to the use of
the SSC in the hospitals or a certification may incite
is proper use. Reported incidents may serve as exam-
ples of the SSC impact, as it happens in the aviation
(Downey, 2010).
The designed application may be integrated in the
hospitals’ systems, to control the use of the SSC, and
the new proposed features may help the SSC to be-
come more user-friendly, and reliable. This needs to
be investigated in further studies and a collaboration
with the WHO is required to validate modifications
for each type of surgery.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the support
of Hospital Prof. Doutor Fernando Fonseca, EPE,
specially to all health professionals involved for their
participation, full collaboration, and insightful discus-
sions.
This work was partially funded by Project I-CITY
- ICT for Future Health/Faculdade de Engenharia
da Universidade do Porto, NORTE-07-0124-FEDER-
000068, funded by the Fundo Europeu de Desen-
volvimento Regional (FEDER) through the Programa
Operacional do Norte (ON2) and by national funds
through FCT/MEC (PIDDAC).
REFERENCES
Downey, T. (2010). Soaring ahead - unmanned systems
represent a fast-growing boeing business. Frontiers,
IX(III):50–53.
Emerton, M., Panesar, S. S., and Forrest, K. (2009).
Safer surgery: how a checklist can make orthopaedic
surgery safer. Orthopaedics and Trauma, 23(5):377–
380.
Gawande, A. A., Thomas, E. J., Zinner, M. J., and Brennan,
T. A. (1999). The incidence and nature of surgical
adverse events in colorado and utah in 1992. Surgery,
126(1):66–75.
George, F. (2010). Cirurgia segura salva vidas. Circular
Normativa 16/DQS/DQCO, Direcção Geral da Saúde,
Alameda D. Afonso Henriques, 45 - 1049-005 Lisboa
- Portugal.
George, F. (2013). Cirurgia segura, salva vidas. Cir-
cular Normativa 02/2013, Direcção Geral da Saúde,
Alameda D. Afonso Henriques, 45 - 1049-005 Lisboa
- Portugal.
Haynes, A. B., Weiser, T. G., Berry, W. R., Lipsitz, S. R.,
Breizat, A.-H. S., Dellinger, E. P., Herbosa, T., Joseph,
S., Kibatala, P. L., Lapitan, M. C. M., et al. (2009). A
surgical safety checklist to reduce morbidity and mor-
tality in a global population. New England Journal of
Medicine, 360(5):491–499.
Kable, A., Gibberd, R., and Spigelman, A. (2002). Adverse
events in surgical patients in australia. International
Journal for Quality in Health Care, 14(4):269–276.
Kwaan, M. R., Studdert, D. M., Zinner, M. J., and Gawande,
A. A. (2006). Incidence, patterns, and prevention of
wrong-site surgery. Archives of surgery, 141(4):353–
358.
Manfreda, K. L., Batagelj, Z., and Vehovar, V. (2002). De-
sign of web survey questionnaires: Three basic exper-
iments. Journal of Computer-Mediated Communica-
tion, 7(3):0–0.
Schamel, J. (2012). How the pilot’s checklist came about.
http://www.atchistory.org/History/checklst.htm.
Gilbert, James "The Great Planes", 1970; Jablonski,
Edward "Flying Fortress", 1965; Jones, Lloyd "U.S.
Fighters", 1975.
Takala, R., PAUNIAHO, S.-L., Kotkansalo, A., Helmiö, P.,
Blomgren, K., Helminen, M., Kinnunen, M., Takala,
A., Aaltonen, R., Katila, A., et al. (2011). A pilot
study of the implementation of whosurgical check-
list in finland: improvements in activities and com-
munication. Acta anaesthesiologica Scandinavica,
55(10):1206–1214.
Umbach, P. D. (2004). Web surveys: Best practices. New
Directions for Institutional Research, 2004(121):23–
38.
Valido, S. C. N. (2011). Checklist cirúrgica: contributo para
uma intervenção na área da segurança do doente.
HEALTHINF2015-InternationalConferenceonHealthInformatics
396
