
An Architecture to Support Ultrasound Report Generation
and Standardisation
Nur Zareen Zulkarnain
1
, Gillian Crofts
2
and Farid Meziane
1
1
Informatics Research Centre, School of Computing, Science and Engineering, Newton Building, M5 4WT, Salford, U.K.
2
School of Health Science, Allerton Building, M6 6PU, University of Salford, Salford, U.K.
Keywords: Ultrasound, Ultrasound Reporting, Ontology, Radiology, Digital Healthcare.
Abstract: Ultrasound reports are developed in different ways by clinicians and radiologists. These variations in
reporting style, content and format could impact on the value of the report and the way it is interpreted,
which in turn have implications on patient management and decision making. There are many reasons for
the poor success rate of some reporting systems which is usually down to poor adaptability and the main
one being the human factor. In this paper, we present a system architecture model for a proposed medical
ultrasound reporting system that attempt to address some of these problems. In this system, we propose a
solution where humans will not need to adapt to the system, instead the system acknowledge the various
styles, contents and format being produced by the humans and uses an ontology to standardise the
terminology and Natural Language Processing techniques to transform free text reports to the preferred
proposed model of a structured and standardised report.
1 INTRODUCTION
Medical ultrasound reports are the main tool for
communicating the result of an ultrasound
examination from a sonographer or radiologist to a
referring clinician. Ultrasound images alone are of
limited value since the outcomes of any ultrasound
investigation are based on the findings during the
scan (Boland, 2007). The ultrasound report therefore
can be considered as a vital part in diagnosing a
patient because of the way the ultrasound
examination is performed.
Tissues characterisation alongside quantitative
measurements, are features typically reported on
during the scan (Sluis and Mankovich, 2002). The
amount of data therefore obtained during the
examination is huge. Variations in reporting styles
vary widely; this leads to variations in the structure
of reports as well as in the terminologies used. These
variations may impact on the way a report is
interpreted and in turn affect the decision making
process and the way a patient is managed.
According to Kahn et al. (2009), the industry
believes that the solution to this problem resides in
using structured reporting with the support of
ontology as its knowledge base. There are several
benefits, including inserting measurements and key
images in reports (Sluis and Mankovich, 2002). This
in turn makes it easier to perform estimations and
aids in decision making. Structured reporting has
been shown to improve the accuracy of reports
(Bosmans et al., 2012) since the reports produced
incorporate standardised terms.
Compared to free-form text, data from structured
reporting can be easily queried and populated.
Structured reporting also increases the accessibility
of data for research. Furthermore, structured
reporting gives the ability to improve the quality of a
medical report since individual elements measuring
quality are more easily defined (Schwartz, et al.,
2011).
It is known that in medical and healthcare
disciplines, there are a significant number of
terminologies being used. To add to that, several
terminologies are often used to describe the same
condition. For example, carcinoma and cancer,
calculi and stone, as well as neoplasm and tumour
are both different words that have the same meaning.
The development of ontology allows for these
terminologies with commonly accepted definitions
to be sorted in a dictionary similar to a framework
for knowledge representation (Smith, 2003). It
defines a common vocabulary of machine-
interpretable definitions of basic concepts in the
508
Zulkarnain N., Crofts G. and Meziane F..
An Architecture to Support Ultrasound Report Generation and Standardisation .
DOI: 10.5220/0005252505080513
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 508-513
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

domain and the relations among them (Noy and
McGuinness, 2001). With the existence of
ontologies, it is possible to annotate terms published
on the internet to allow computers to query and
extract relevant information pertaining to a concept
even though it uses different terms. In our case, the
use of an ontology will allow for standardization of
terminologies used in ultrasound reports.
For a better exploitation and use of these reports,
computerised tools that can facilitate these processes
need also to be developed. In this paper, we describe
the architecture of a software system that is designed
to support the standardisation of the process of
generating ultrasound images reports.
The remainder of the paper is organised as
follows; in section 2 we review the literature and
identify related works and research. Section 3 will
explain the proposed architecture model before we
conclude the paper in section 4.
2 RELATED WORK
Realising the effectiveness of conveying information
in structured forms, several researchers have
developed models and proposals to apply structured
reporting as a method to create radiology and
ultrasound reports (Bell, Greenes and Doubilet,
1992; Kuhn et al., 1993). The early structured
reporting systems were constructed using
checkboxes and radio buttons for the radiologists to
choose concepts from a list of terminologies (Bell et
al., 1992). These checkboxes and radio buttons were
used to answer a set of predefined questions to
develop the content of the report. One disadvantage
of this approach is that it limits the inclusion of
additional information that could be important for
the case, and would not allow the form to be
submitted with certain fields being left blank. These
options are important as sometimes reports may
contain more information than the predefined one
and in some instances some information cannot be
obtained.
In previous studies (Naik et al., 2001; Johnson,
et al., 2009; Plumb et al., 2009) attempts were
made to identify the radiologists preferences when
creating reports. As a result, it is shown that both
radiologists and referring clinicians prefer structured
reporting over other methods of reporting. Whilst
this type of system has been used in some Radiology
Departments (Bell and Greenes, 1994), there are
challenges which have limited it to wider
implementation
Radiologists found that the implementation of
structured reporting systems was time consuming
and overly constrained where it did not allow them
to include more content than what the system asked
for (Johnson et al., 2009; Langlotz, 2009).
Structured reporting is also seen as interference
during the image interpretation process (Bosmans et
al., 2012; Weiss and Langlotz, 2008) and does not
give any productivity advantage to the radiologist.
In a recent study conducted by Bosmans et al.
(2012), radiologists were convinced that a structured
report should allow for free-form remarks to allow
for reflections or expression of uncertainty. This is
important because different cases would have
different observations and would need to include
different types of information. It is also important
for a structured report to allow for certain
information to be left out but with some remarks
explaining the reason (United Kingdom Association
of Sonographers (UKAS), 2008), because not all
information can always be obtained due to
limitations often encountered during the scan
process. Structured reporting would be readily
accepted by radiologists if it is more flexible
whereby they would be able to choose what to
include and what to leave out in the report
depending on the case that is being reported. This
flexibility is the main characteristic that we would
like to incorporate in our proposed model together
with standardisation.
Ontologies serve several purposes in the medical
field. This is proven by the existence of many
medical related ontologies such as Foundational
Model of Anatomy (FMA), Systematized
Nomenclature of Medicine - Clinical Terms
(SNOMED CT) and Radiology Lexicon (RadLex)
(Rubin, 2008). One of the main purposes of an
ontology in radiology domain is to annotate images
and reports. Radiology departments, produce
thousands of images and reports concerning
examinations performed on patients. By annotating
these images and reports, it is easier for
automatically searching and extracting information
from these images and integrates them in teaching
and research where they can play an important role.
RadiO, a prototype application by Marwede,
Fielding, & Kahn (2007) is one example of
annotating reports using ontologies. In this
application, image features of image entities are
annotated using an application ontology of imaging
‘findings’ and their interpretation as a knowledge
base. Another example of an application is
Interdisciplinary Prostate Ontology Project (IPOP)
(Overton et al., 2011), which uses ontologies from
OBO Foundry to annotate clinical reports about
AnArchitecturetoSupportUltrasoundReportGenerationandStandardisation
509
prostate cancer.
Ontology also serves a purpose in report
generation such as the one in the MIAKT project
(Bontcheva and Wilks, 2004). In this project, reports
are generated automatically from knowledge
encoded in the domain ontology using Natural
Language Generation Techniques (NLG). Semantic
data such as patients’ information and diagnosis are
encoded in the ontology of the breast cancer domain.
The role of NLG is to turn these data to textual
description in order to generate complete reports.
These reports however are in a free-form structure
which defies the notion that structured report with
the support of ontology is the way to go forward in
ultrasound reporting.
Therefore, we propose a model that will give
flexibility while at the same time ensuring
standardisation in terminologies and reporting styles
by applying natural language processing technique
and ontology.
3 THE PROPOSED MODEL
The proposed model is designed with the needs of
the radiologists and clinicians at the centre of the
new system. It is known that humans sometimes
have a resistance to change or adapt to new working
procedures. In order for them to accept changes it is
important for the system to have a level of flexibility
and for the practitioners to get involved in the design
of the new system. This would help the transition
from free-form text reporting to structured reporting
without causing too many frustrations and
inconveniences.
From the studies done by Bosmans et al. (2012)
and Danton (2010) radiologists were found to have
problems with not having more options in creating
their reports. With that in mind, we designed a
model that allows flexibility for the radiologist to
choose whichever way they are comfortable with in
writing the report but at the same time producing the
same result which is a standardized ultrasound
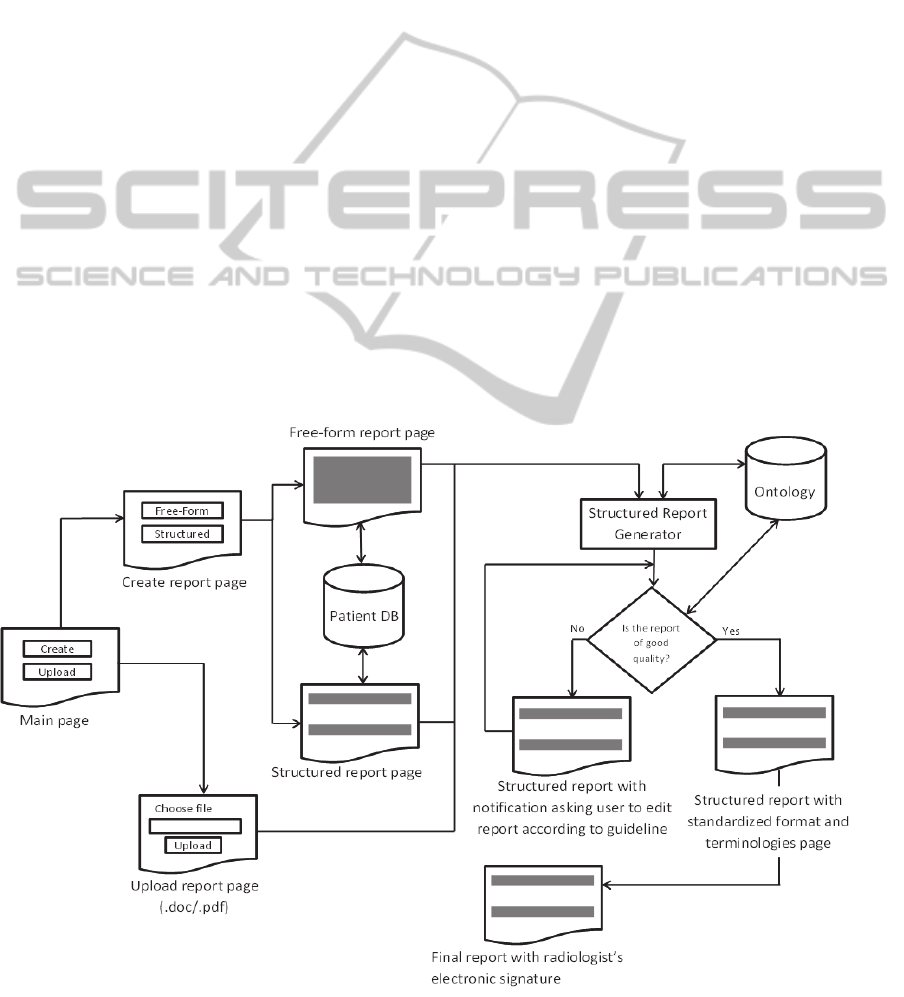
report. Figure 1 shows the components of the
proposed model. In the following subsections, we
describe the different components of the system.
3.1 The High Level of the System
To allow flexibility, portability and its access from
various locations, the system is currently developed
as a web-based application. Security and data
Figure 1: Proposed System Architecture Model of the Reporting System.
HEALTHINF2015-InternationalConferenceonHealthInformatics
510
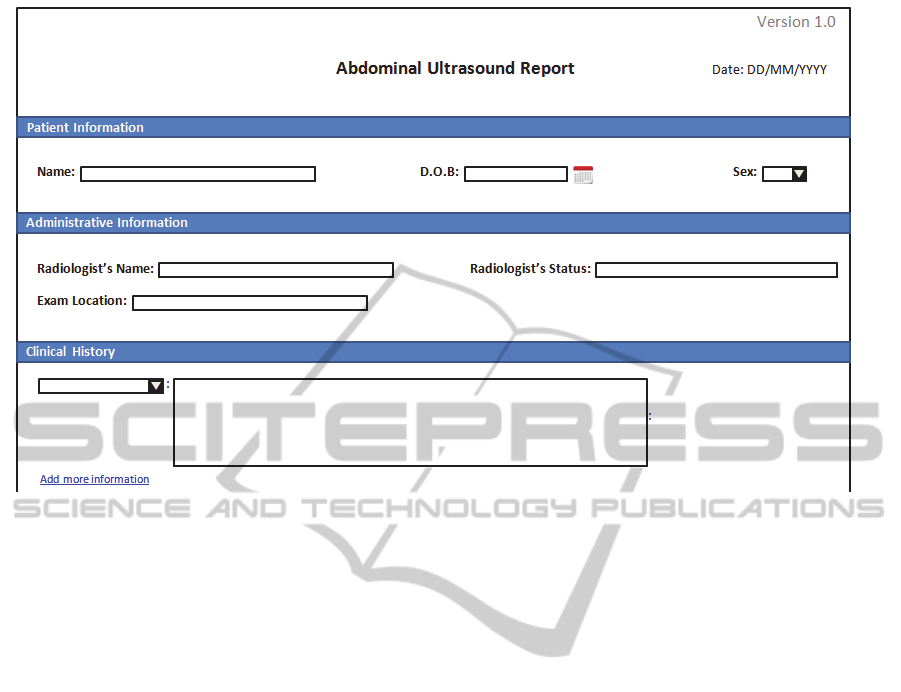
Figure 2: User Interface Design for Structured Report Page.
protection issues are recognised as extremely
important and are an integral part of this system.
Data protection however is not the main focus of this
paper. When logging into the system, there are two
options to choose from; (i) create the report using
the online form or (ii) upload a report. This offers
flexibility as they would not need to stick to one
method of writing the report and could use the
option that best suit the case they are handling.
3.2 Create Report Page
Once the path to create the ultrasound report using
the online form is chosen further options are
presented which are using guided free-form or
structured report form. Most medical ultrasound
reporting system uses a structured form for the
radiologist to fill in. This requires a lot of mouse
control and clicking. Structured form is also often
rigid where it forces the healthcare professional to
complete most parts of the form and in this case, the
form cannot be submitted until all sections are
completed. This could cause frustration to the
radiologist and deter their interest in using the
system.
In our proposed model, we designed the form to
be less rigid compared to the usual structured report
form and if they prefer, they can still opt to create
reports using the free-form. Both of these forms will
be explained further in section 3.2.1 and 3.2.2.
3.2.1 Free-from Report Page
The free-form report page allows the ultrasound
report be created by freely typing in their
observations without the need to adhere to a certain
structure. Creating a report using our system negates
the need to provide patient information because the
system will automatically link this report to the
patient’s record.
The free-from report page will consist of three
questions related to the ultrasound examination.
These questions will act as a guide for report
writing. Submission of the report is easily facilitated
once the report is complete.
3.2.2 Structured Report Page
In our proposed system, we include a structured
report page similar to what was proposed by other
researchers (Bell et al., 1992;
Kahn, Wang & Bell,
1996). The main difference is that the proposed
structured report form will be less rigid compared to
the previous ones which allows for a variation in
report style.
This can be allowed in our proposed model
because all reports that are submitted will need to go
through a quality checker before it could be signed
off. If the quality checker finds that the report is
good enough, it will be accepted. Otherwise, the
report will be returned for amendment. This will be
further explained in the next sections.
AnArchitecturetoSupportUltrasoundReportGenerationandStandardisation
511

Figure 2 shows a snippet of the user interface
design for the structured report page. Similar to the
free-form report page, the radiologist will not need
the patient’s information as this will be
automatically included by the system. The same is
true for the radiologist’s name and status. When the
radiologist signs-in to the system, it will
automatically display the radiologist’s information.
In filling in the report, the radiologist will find that
the report form is much more flexible compared to
other available structured report forms.
For example, under clinical history, the
radiologists can choose from the drop-down menu
what type of information they would like to include.
If they wish, they could add more information by
clicking on the ‘add more information’ link. This
allows the radiologist to give as much information as
they want in the report.
Though this form still requires a lot of mouse
control and clicking, the radiologist will always have
the option of using free-from report if they find it
hard to fill the structured one. The benefits of using
a structured report form is that it would help guide
the radiologist in giving enough information about
the ultrasound examination and ensure that the
report they produce will be rated as being of a good
quality report by the report quality checker. This
reduces the probability of them needing to edit the
report to conform to the quality guidelines
3.3 Upload Report Page
Another option that the radiologists have in creating
a standard ultrasound report is by uploading a report
that they have written elsewhere. The report could
be in formats such as .doc and .pdf and could be
written in any way that they prefer. This option is
not only for reports that have been recently written.
The radiologist could use this option to upload a
free-form report that has been written before in order
to convert it into a standard form. However, this will
depend on the amount of information available in
the report. If the report does not contain enough
information and is regarded as a low quality report,
the generator will not allow for it to be signed off.
3.4 Structured Report Generator
Whether the radiologists choose to create the report
using our proposed system or by uploading reports
they have created elsewhere, the report will go
through a structured report generator which will
transform the report into a standardised report. The
structured report generator uses domain ontology as
its knowledge base. The ontology will consist of
thousands of medical terms commonly used in
medical ultrasound reports and will be developed by
reusing terminologies in existing ontologies such as
FMA, SNOMED CT and RadLex. The ontology will
help the system to understand what is written in the
report and will use that information to ensure
standard and consistent terminologies are being
used.
The transformation of free-from to structured
form will be done using the computational linguistic
approach of Rhetorical Structure Theory (RST)
which is a descriptive theory of a major aspect of
organisation of natural text (William & Thompson,
1988). It allows for the classification of a chunk of
texts and the description of relations between two
chunks of texts in the free-form report. This will
then serve as the information needed to fill in the
structured form.
Before the structured report can be displayed to
the radiologist, it will go through a quality checker
in order to ensure that the report meets the standard
quality measure. The quality checker will also use
the ontology as its knowledge base together with a
set of quality metrics. If the report meets the
minimum requirement of the quality checker, the
standardized report will be displayed for the
radiologist to check and sign off. If the report does
not meet the minimum requirement, a standardised
report will be displayed to the radiologists but with
notifications to edit the parts of the report that do not
meet the guidelines. After changes have been made
to meet the minimum quality requirement, then only
can it be signed off by the radiologist.
4 CONCLUSIONS
In this paper, we presented a system architecture
model for a medical ultrasound reporting system. In
this model, we proposed a solution where
radiologists are allowed to choose a style of
reporting that they are most comfortable with.
Whether the radiologists choose to create their report
in free-form or structured form or they choose to
upload their report, this system will automatically
generate a standardised structured version of the
report with the support of a medical ultrasound
ontology as its knowledge base. It is anticipated that
a standardised report based on domain ontology will
improve and enhance the quality of an ultrasound
report.
HEALTHINF2015-InternationalConferenceonHealthInformatics
512

REFERENCES
Bell, D. S., & Greenes, R. a. (1994). Evaluation of
UltraSTAR: performance of a collaborative structured
data entry system. Proceedings / the ... Annual
Symposium on Computer Application [sic] in Medical
Care. Symposium on Computer Applications in
Medical Care, 216–22. Retrieved from
http://www.pubmedcentral.nih.gov/articlerender.fcgi?a
rtid=2247858&tool=pmcentrez&rendertype=abstract.
Bell, D. S., Greenes, R. a, & Doubilet, P. (1992). Form-
based clinical input from a structured vocabulary:
initial application in ultrasound reporting. Proceedings
/ the ... Annual Symposium on Computer Application
[sic] in Medical Care. Symposium on Computer
Applications in Medical Care, 789–90.
Boland, G. (2007). Enhancing the radiology product: the
value of voice-recognition technology. Clinical
Radiology, 62(11), 1127.
doi:10.1016/j.crad.2007.05.014.
Bontcheva, K., & Wilks, Y. (2004). Automatic report
generation from ontologies: the MIAKT approach.
Natural Language Processing and Information …,
(Section 2).
Bosmans, J. M. L., Peremans, L., Menni, M., De
Schepper, a M., Duyck, P. O., & Parizel, P. M. (2012).
Structured reporting: if, why, when, how-and at what
expense? Results of a focus group meeting of
radiology professionals from eight countries. Insights
into Imaging, 3(3), 295–302. doi:10.1007/s13244-012-
0148-1.
Danton, G. H. (2010). Radiology Reporting, Changes
Worth Making Are Never Easy. Applied Radiology,
5(May), 19–23. Retrieved from
http://www.appliedradiology.com/Issues/2010/05/Arti
cles/Radiology-Reporting,-Changes-Worth-Making-
Are-Never-Easy.aspx.
Johnson, A. J., Chen, M. Y. M., Swan, J. S., Applegate, K.
E., & Littenberg, B. (2009). Cohort study of structured
reporting compared with conventional dictation.
Radiology, 253(1), 74–80.
doi:10.1148/radiol.2531090138.
Kahn, C. E., Langlotz, C. P., Burnside, E. S., Carrino, J.
A., Channin, D. S., Hovsepian, D. M., & Rubin, D. L.
(2009). Toward best practices in radiology reporting.
Radiology, 252(3), 852–6.
doi:10.1148/radiol.2523081992.
Kahn, C. E., Wang, K., & Bell, D. S. (1996). Structured
entry of radiology reports using World Wide Web
technology. Radiographics : a review publication of
the Radiological Society of North America, Inc, 16(3),
683–91. doi:10.1148/radiographics.16.3.8897632.
Kuhn, K., Zemmler, T., Reichert, M., Heinlein, C., &
Roesner, D. (1993). Structured data collection and
knowledge-based user guidance for abdominal
ultrasound reporting. Proceedings / the ... Annual
Symposium on Computer Application [sic] in Medical
Care. Symposium on Computer Applications in
Medical Care, (311), 311–5.
Langlotz, C. P. (2009). Structured radiology reporting: are
we there yet? Radiology, 253(1), 23–5.
doi:10.1148/radiol.2531091088.
Marwede, D., Fielding, M., & Kahn, T. (2007). RadiO: a
prototype application ontology for radiology reporting
tasks. AMIA ... Annual Symposium proceedings /
AMIA Symposium. AMIA Symposium, 513-517.
Naik SS, Hanbidge A, Wilson SR (2001) Radiology
reports: examining radiologist and clinician
preferences regarding style and content. AJR Am J
Roentgenol 176:591–598.
Noy, N., & McGuinness, D. (2001). Ontology
development 101: A guide to creating your first
ontology, 1–25.
Overton, J., Romagnoli, C., & Chhem, R. (2011). Open
Biomedical Ontologies applied to prostate cancer.
Applied Ontology, 6, 35–51.
Plumb, a a O., Grieve, F. M., & Khan, S. H. (2009).
Survey of hospital clinicians’ preferences regarding
the format of radiology reports. Clinical radiology,
64(4), 386–94; 395–6. doi:10.1016/j.crad.2008.11.009.
Rubin, D. L. (2008). Creating and curating a terminology
for radiology: ontology modeling and analysis.
Journal of digital imaging, 21(4), 355–62.
doi:10.1007/s10278-007-9073-0.
Schwartz, L. H., Panicek, D. M., Berk, A. R., Li, Y., &
Hricak, H. (2011). Improving communication of
diagnostic radiology findings through structured
reporting. Radiology, 260(1), 174–81.
doi:10.1148/radiol.11101913.
Sluis, D., Lee, K., & Mankovich, N. (2002). DICOM SR-
Integrating structured data into clinical information
systems. Medicamundi, (August), 31–36.
Smith, B. (2003). Ontology: philosophical and
computational. In Floridi L (Ed.), The Blackwell
Guide to the Philosophy of Computing and
Information. Oxford: Blackwell Publishers.
United Kingdom Association of Sonographers (UKAS)
(2008). Guidelines for Professional Working
Standards-Ultrasound Practice. P45-51.
Weiss, D. L., & Langlotz, C. P. (2008). Structured
reporting: patient care enhancement or productivity
nightmare? Radiology, 249(3), 739–47.
doi:10.1148/radiol.2493080988.
William, M., & Thompson, S. (1988). Rhetorical structure
theory: Towards a functional theory of text
organization. Text, 8(1988).
AnArchitecturetoSupportUltrasoundReportGenerationandStandardisation
513
