
A Smart Catheter System for Minimally Invasive Brain Monitoring
Dongxuan Bao
1
, Zhuo Zou
2
, Yuxiang Huan
1
, Chuanying Zhai
2
, Tiberiu Bagaian
3
, Hannu Tenhunen
2
,
Bengt Källbäck
3
and Li-Rong Zheng
1,2
1
State Key Laboratory of ASIC & System, Fudan University, Shanghai 201203, China
2
iPack Vinn Excellence Center, KTH-Royal Institute of Technology, 164 40 Kista, Sweden
3
CathPrint AB, SE-114 19 Stockholm, Sweden
Keywords: Smart Catheter, TBI, Real-Time Monitoring, Pressure, Temperature.
Abstract: This paper demonstrates a smart catheter system with intracranial pressure (ICP) and temperature sensing
capability which is designed for real-time monitoring in traumatic brain injury (TBI) therapy. It uses a
single flexible catheter with a 1 mm (3 Fr) diameter that integrates electrodes and sophisticated silicon chip
on flexible substrates, enabling multimodality monitoring of physiological signals. A micro-electro-
mechanical-system (MEMS) catheter pressure sensor is mounted on the distal end. It can be used for
detecting both pressure and temperature by different switch configurations, which minimizes the size of
catheter and reduces the cost. The interconnects (signalling conductors) are printed on a bio-compatible
flexible substrate, and the sensor is interfaced with an embedded electronic system at the far-end. The
electronic system consists of analog front end with analog-to-digital converter (ADC), a microcontroller,
and data interface to the hospital infrastructure with a graphical user interface (GUI). The overall smart
catheter system achieves a pressure sensing root mean square error (RMSE) of ±1.5 mmHg measured from
20 mmHg to 300 mmHg above 1 atm and a temperature sensing RMSE of ±0.08 ºC measured from 32 ºC to
42 ºC. The sampling rate can be up to 10S/s. The in vivo performance is demonstrated in laboratory animals.
1 INTRODUCTION
Traumatic brain injury (TBI) is a type of acquired
brain injury, occurs when a sudden force
traumatically injures the brain. The main causes
include falls, traffic accidents, and violence. TBI is
one of the major causes of death and disability in
patients from ages 1 to 44 years. TBI results in 1.4
million reported injuries and 52000 deaths each year
in the United States (Faul, 2010). Secondary
neurological damage, a variety of events that take
place in the ensuing hours and days following the
primary injury, contribute substantially to the worse
damage caused by primary injury and accounts for
the greatest number of TBI deaths occurring in
hospitals. Raised intracranial pressure (ICP) is a
common factor in secondary injury. The causes of
raised ICP include swelling or a mass effect from a
lesion such as subdural hematoma. When the ICP
rises, the cerebral perfusion pressure (CPP)
decreased, resulting in ischemia or even brain death.
Therefore, a precise monitoring of the ICP is very
important for minimizing secondary ischemic injury
in TBI. In addition, the brain of neurosurgical
patients with severe traumatic brain injury is
extremely sensitive and vulnerable to small
temperature variations, thus fever is considered a
secondary injury to the brain (Mrozek, 2012).
Hence, continuous monitoring of intracranial
temperature is also highly recommended.
The intraventricular catheter is the most accurate
pressure monitoring method, in which catheters are
inserted into the lateral ventricle through a hole
drilled on the skull (MedlinePlus, 2014). Current
TBI care unit uses separate catheters for monitoring
multiple signals, which are collected by external
electronic system through separate cables for signal
processing and real-time data display (Stiefel, 2005).
However, a big burr hole is needed to accommodate
multiple catheters, which is susceptible to infection
and complications. Therefore a smart catheter
system providing ICP and temperature monitoring
capability with single catheter insertion is highly
desirable to minimize incision.
Thanks to the steady and considerable effort
directed towards the development of sensor
fabrication technology, some pressure sensors for
biomedical applications have been reported. They
198
Bao D., Zou Z., Huan Y., Zhai C., Bagaian T., Tenhunen H., Källbäck B. and Zheng L..
A Smart Catheter System for Minimally Invasive Brain Monitoring.
DOI: 10.5220/0005285501980203
In Proceedings of the International Conference on Biomedical Electronics and Devices (BIODEVICES-2015), pages 198-203
ISBN: 978-989-758-071-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)
usually fall into two categories, pressure sensor on
solid substrate and on flexible substrate. Pressure
sensors manufactured using MEMS technology,
typically provide increased reliability and higher
precision. However, they are often expensive and
fabricated on rigid substrates (Wahab, 2008).
Meanwhile, electronics on flexible substrates is
considered as an alternative approach that enables
low-cost manufacturing of thin, flexible, light
devices. The revolutionary technologies have
enabled displays, sensors (Pritchard, 2008), antennas
on flexible substrates. Flexible pressure sensor is
highly non-linear; thus careful, frequent calibration
may be necessary. However, it provides a promising
solution for chip-system integration (Xie, 2012). In
this work, a heterogeneous system which seamlessly
integrates MEMS sensor with flexible printed circuit
board (PCB) is employed to develop a low cost
catheter. A piezoresistive MEMS pressure sensor is
employed in proposed system.
The temperature can be detected by a separate
sensor (Li, 2012). However, it is limited in
applications required more sensors because of the
small size of catheter. In (Chan, 2013), a
temperature sensor circuit which consists of a
portional to absolute temperature (PTAT) voltage
generator, a bandgap voltage generator, and a V
BE
amplifier is integrated. Nevertheless it is non-contact
sensor. Thermistors are very low cost and available
in a wide variety of packages. However, the resistive
change is relatively small. Therefore, an
amplification circuit is necessary to ensure the
output signal quality.
In this paper, a 1 mm (3 Fr) diameter smart
catheter, inserted with flexible PCB, is proposed to
sense the ICP and temperature signal for detection of
any anomaly in the patient. A piezoresistive MEMS
pressure sensor is utilized to provide accurate
pressure measurement within the very small spaces
and harsh environments of the catheter. The sensor
can also be used for detecting temperature by switch
configurations, which minimizes the catheter size.
The sensor signals are fed into an external electronic
system by flexible PCB. An instrumentation
amplifier in electronic system provides the required
amplification of the sensed signal and the
temperature sensing output can be used to
compensate pressure sensor error caused by
temperature variations. The electronic system reads
out signal and quantizes it with an integrated ADC.
Therefore, not only physiological parameters can
be shown directly in real time in vivo, but also
reduce the effects and complications caused by
surgery. To demonstrate the proof of concept, a
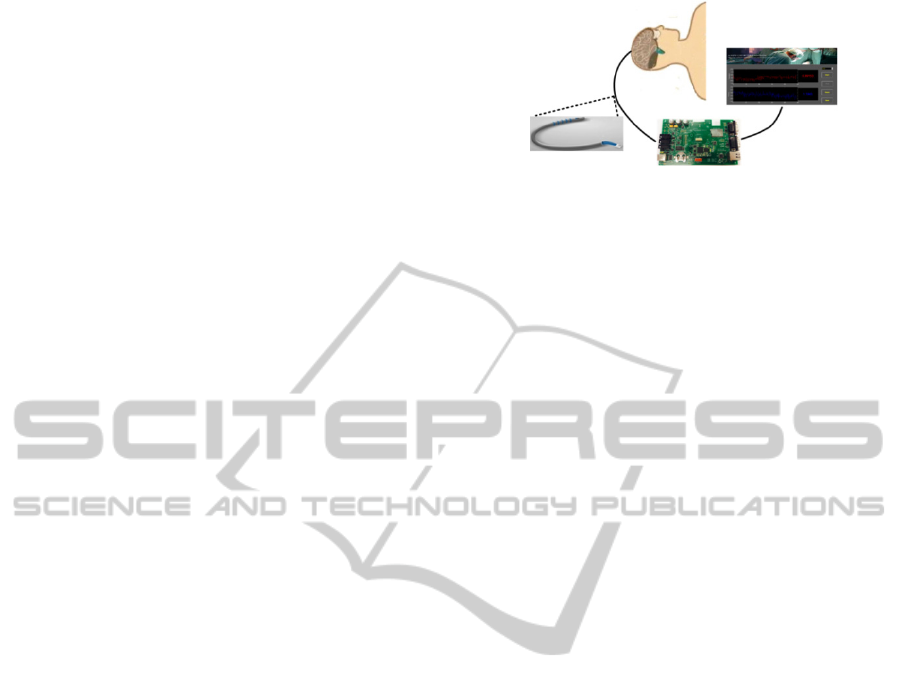
Figure 1: Smart catheter system for continuous ICP and
temperature measurement.
smart catheter system is implemented and measured
in laboratory animals.
The remainder of this paper is organized as
follows. The proposed smart catheter system is
described in Section 2. The catheter and electronic
system are elaborated in Section 3 and 4
respectively. The system characterization is
discussed in Section 5 with conclusions given in
Section 6.
2 SYSTEM DESCRIPTION
The objective is to develop a catheter for invasive
measurement of ICP and temperature and to show
that it can be produced at a low enough cost and be
integrated in current hospital procedures and
infrastructure. Due to the small size of mini-invasive
catheter, the proposed system adopts flexible PCB
for transmission such that the pre-mount sensor
information can be collected outside of the body
using an external electronic device. Fig. 1 illustrates
the whole system. The system is composed by four
major components: a catheter with pre-mount
sensors and electrodes, a sensor interface and
measurement logic, a microcontroller and a
computer with GUI. The proposed mini-invasive
catheter measures pressure and temperature in vivo
and sends the signal to the analog signal
conditioning circuitry through flexible PCB. The
output signals of sensors are collected by an analog
interface of instrumentation amplifier, which is
followed by a microcontroller-based socket board
comprised an integrated ADC and a RS-232 serial
port interfacing to the computer. The computer will
process the data received from external electronic
devices to display the situation of the patient. The
calibration algorithm will also run on the computer.
Then the corresponding pressure and temperature
can be calculated based on the measured voltage
after calibration.
ASmartCatheterSystemforMinimallyInvasiveBrainMonitoring
199
3 HETEROGENEOUS
INTEGRATION CATHETER
To measure physiological parameters, such as tissue
pressure and temperature, sensors should be
incorporated in the catheter. Moreover, a single
catheter provides multiple signal sensing capability
is highly desirable to minimize wound. In this work,
Prefab technology from CathPrint AB is adopted
(CathPrint AB, 2014) (Kallback, 2009). The Prefab
is inserted into a lumen of the customer’s extrusion
which is prepared with holes for electrodes and pre-
mounted sensors. It enables an uncomplicated
solution for connecting electrodes, sensors inside
body to external electronic and data analyzing
system.
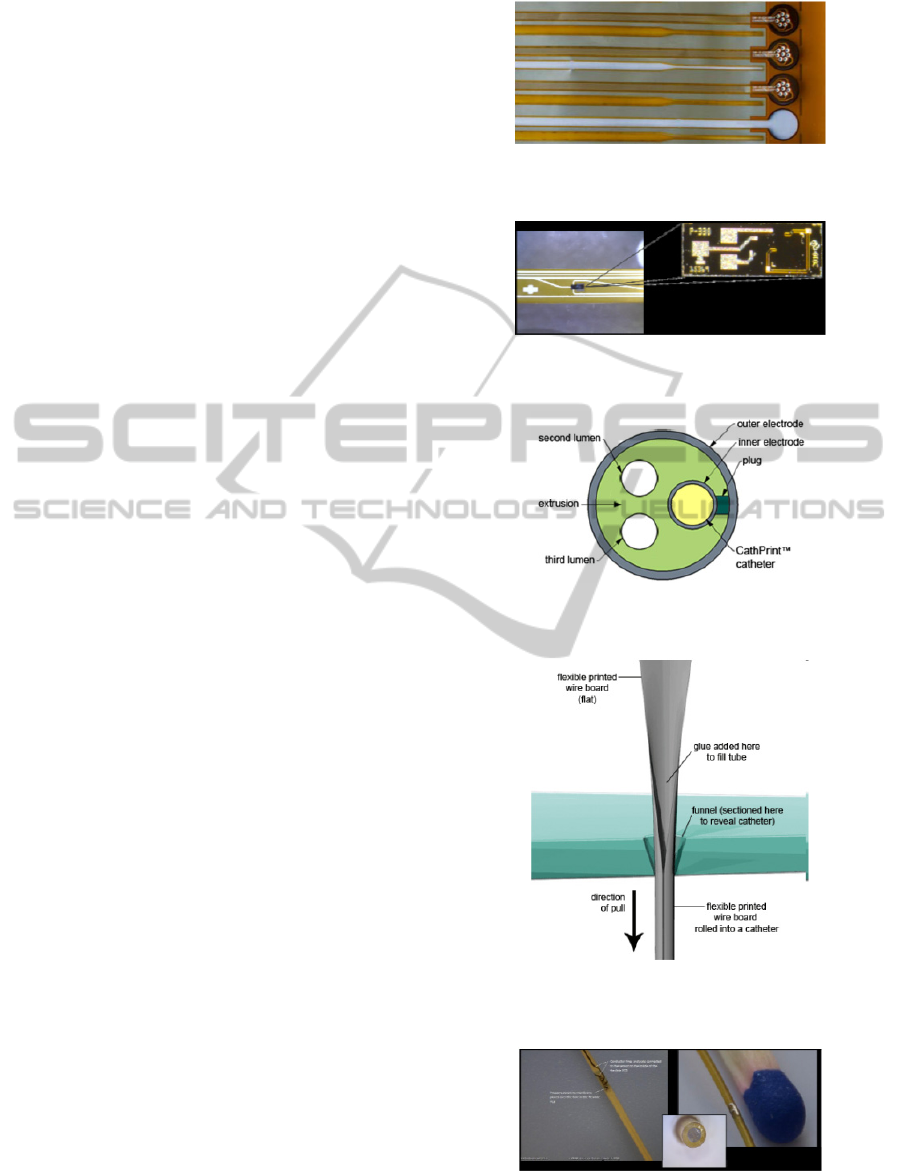
In general the catheters are long (in the order of
one meter) and thin (between 0.3 and 3 mm)
(Kallback, 2009). Therefore, a thin but long PCB
(e.g. 2 meters with 350 um diameter) is the basis for
catheter manufacturing as illustrated in Fig. 2
(CathPrint AB, 2014).
In this Prefab technology, sensors are mounted
on the flexible board, having contact with the
surrounding substance through an access hole in the
catheter for measurement use as shown in Fig. 3.
The bond pads on the flexible PCB are connected to
respective bond pads on the sensors by bonding
wires. In this work, a MEMS pressure sensor is
integrated to demonstrate the potential applications
as shown in Fig. 3 (CathPrint AB, 2014). This
heterogeneous integration catheter combines flexible
substrates based technology and silicon based
electronics which takes advantages from both
technologies. Thus the proposed heterogeneous
integration approach provides a promising solution
for mini-invasive applications. Electrodes can also
be integrated in the catheter, which are in contact
with the liquid surrounding the device for invasive
applications, such as blood oxygen detection. The
electrodes are placed outside the tube, and they are
connected to an inner catheter via a conductive plug
as shown in Fig. 4 (CathPrint AB, 2014). Therefore
it is convenient to connect the electrodes to an
electronic system at the far-end.
To enables the possibility of producing flexible
catheters with a diameter that is as small as 0.35
mm, the flexible circuit board is then rolled up to
form an extremely narrow tube, which is done by
feeding the flexible PCB through a funnel as
illustrated in Fig. 5 (CathPrint AB, 2014) (Kallback,
2009). The inner space of catheter-to-be is filled
with glue that holds the catheter in a tube shape after
the process. The resulting flexible catheter features a
Figure 2: Thin flexible PCBs for catheter (CathPrint AB,
2014).
Figure 3: Pressure sensor mounted on the flexible board
(CathPrint AB, 2014).
Figure 4: CathPrint integrated catheter with electrodes
outside (CathPrint AB, 2014).
Figure 5: The flexible PCB is pulled through a funnel
producing a catheter (CathPrint AB, 2014).
Figure 6: A miniature solid catheter with sensor inside and
electrode outside (CathPrint AB, 2014).
BIODEVICES2015-InternationalConferenceonBiomedicalElectronicsandDevices
200
diameter ranging from 0.33 to 1 mm and a
maximum length of approximately 1.5 meters. This
technique significantly reduces the fabrication
process, and decreases the cost as well as the
catheter size. The proposed method for
manufacturing catheters transforms the flat circuit
board into a solid catheter which carries the sensor
inside the flexible PCB and has the electrodes
outside as shown in Fig. 6 (CathPrint AB, 2014).
4 ELECTRONIC SYSTEM
4.1 Pressure and Temperature Sensor
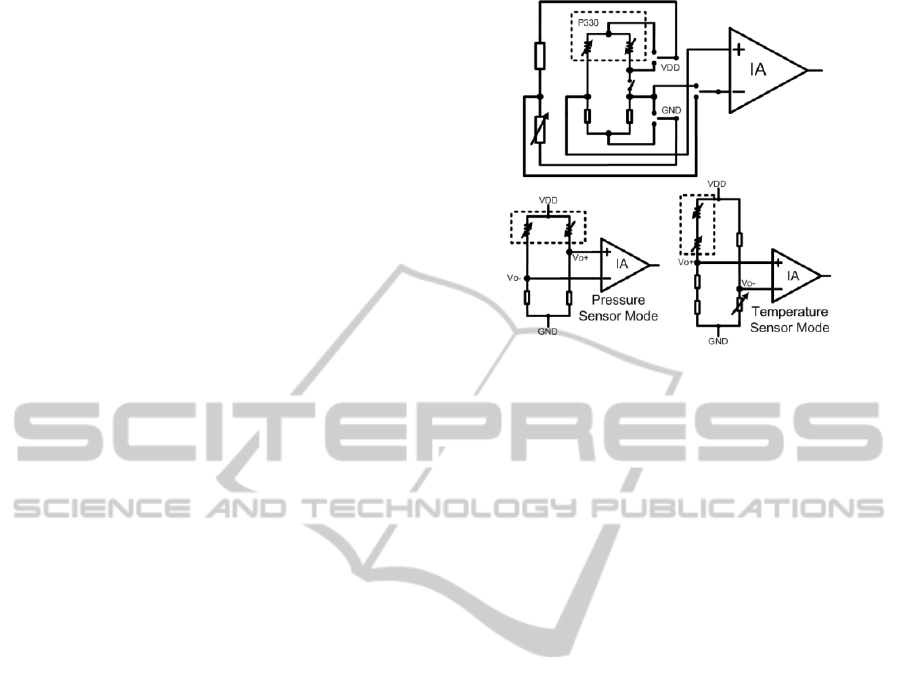
A switch regulator on socket board will regulate 3.3
V, which provides the power supply for the analog
interface and sensors. The pressure sensor employed
is P330 silicon MEMS pressure die, which is from
GE Measurement & Control. Its equivalent circuit is
illustrated in Fig. 7. A stable 3.3 V power supply is
applied between VDD and GND. In pressure sensor
mode, two 3.3 KΩ external resistors are utilized to
form a half bridge. When a change in pressure
causes the sensor to deflect, a corresponding change
in resistance is induced. Then the differential output
voltage on Vo+ and Vo- will also be changed by the
pressure. As the input range of ADC on socket board
is from 0 to 2 V with 14-bit effective number of bits
(ENOB), 1 LSB will be presented as 122.1 µV.
While the sensitivity of sensor in proposed system is
about 8.6
//V V mmHg
. Therefore the pressure
sensing resolution of this system is nearly
122.1/ 8.6 / 3.3 4.3
mmHg at 3.3 V power
supply. This is because the changes in strain and
resistance are extremely small. To improve the
overall resolution, in proposed sensor interface, an
instrumentation amplifier (IA), INA155 from Texas
Instruments, is used to amplify the changes in
resistance as shown in Fig. 7. INA155 is a CMOS
instrumentation amplifier (IA) with rail-to-rail
output. The gain can adjusted to any value between
10 and 50 by connecting a resistor
G
R
between the
gain pins according to the following equation (Texas
Instruments, 2014):
10 400 / (10 )
G
Gain k k R (1)
And the output voltage of IA is (Texas
Instruments, 2014)
(V )
O IN IN REF
VVGainV
(2)
Where
V
IN
and V
IN
are the input voltages and
Figure 7: Schematic of the pressure/temperature sensor
and interface circuit.
V
REF
is the reference voltage.
The pressure sensor in proposed system provides
a differential output voltage nearly 40 mV at 1 atm.
Therefore we set 0 mV to be
REF
V which
maximizes the swing range and 30 be the gain which
take full advantage of ADC’s input range. The
system performance can be estimated using
specifications. The intrinsic output voltage of IA at
1-atm pressure will be 1.2 V. If we set 20 to 300
mmHg above 1 atm to be measurement ranges, the
sensor output range will be from 1.217 V to 1.455 V
at 3.3 V power supply. Then the span of this system
including proposed sensor interface and ADC is
1951 LSBs. The overall pressure sensing resolution
is therefore nearly 0.14 mmHg. The resolution
improvement is due to amplified resistance changes
by INA155.
The resistance of resistors in pressure sensor
decreases with increasing temperature. Therefore the
pressure sensor can also be used for temperature
measurement. However, the two resistors are
sensitive to both pressure and temperature change. It
is difficult to separate the two reasons for resistance
change. Note that the 2 resistors in the half bridge
sensor are both pressure sensitive but the resistances
change in opposite directions. While these
resistances also change with temperature but in the
same direction. Hence, the series resistance of the 2
bridge resistors can be used for temperature
measurement independent of pressure. In
temperature sensor mode, the two resistors in P330
and the two external resistors compose a branch.
Due to the small changes in resistance, an on-board
reference voltage is also used in a differential
configuration with INA155 providing the required
ASmartCatheterSystemforMinimallyInvasiveBrainMonitoring
201
amplification of the sensed signal. In proposed
sensor interface, a simple voltage-divider with a
resistor and a trimmer in series is employed for
reference voltage. Moreover, the sensor has to be
switched between pressure and temperature
measurement. As shown in Fig. 7, three analog
multiplexers and one analog switch are needed. The
data amount to be transmitted is not heavy that many
off-shelf products meet the mentioned requirements.
A triple 2-channel CMOS analog multiplexers
SN74LV4053A and an analog switch TS5A1066
from Texas Instruments are used in this system at
3.3 V VDD operation. The temperature coefficient
of resistance (TCR) of sensor employed is 0.04
%/ºC, which can be used for estimating temperature
sensing resolution. The two bridge resistances are
assumed to be 3 KΩ in subsequent analysis. If 32-42
ºC is set to be measurement range and the
differential output voltage of IA is 1 V at 32 ºC, the
temperature sensor output range will be from 1 V to
1.099 V at 3.3 V power supply. Then the total range
of this system is 811 LSBs. The temperature sensing
resolution of system is about 0.012 ºC. However,
non-ideal factors will result in apparent system
performance degradation.
4.2 Data Recording and Analyzing
System
The data recording is important when the proposed
system is used for in vivo signal observing. The data
recording and analyzing system including an analog
interface PCB board, a socket board from Imsys
Technologies AB and a computer. The micro-
controller on socket board collects sensor data and
outputs it to a RS-232 serial port. With a RS232-
USB cable, the computer is allowed to connect serial
port through USB ports. The computer receives and
analyzes gathered data from socket board by
programming software. Power is also supplied to the
socket board from the USB interface of computer.
The sensor will be switched between pressure and
temperature measurement automatically by the
socket board. The sampling rate of temperature or
pressure sensing is 10S/s. A graphic user interface
(GUI) that processes the signal sent by the mini-
invasive system is installed on the computer. We can
continuously display the pressure and temperature
from the start point. The results will be displayed in
either pressure or temperature chart. And the
average values of the last 10 readings are shown in
digital format at the right-hand side of the GUI.
Calibration is executed with reference data to
increase system resolution. And then we can
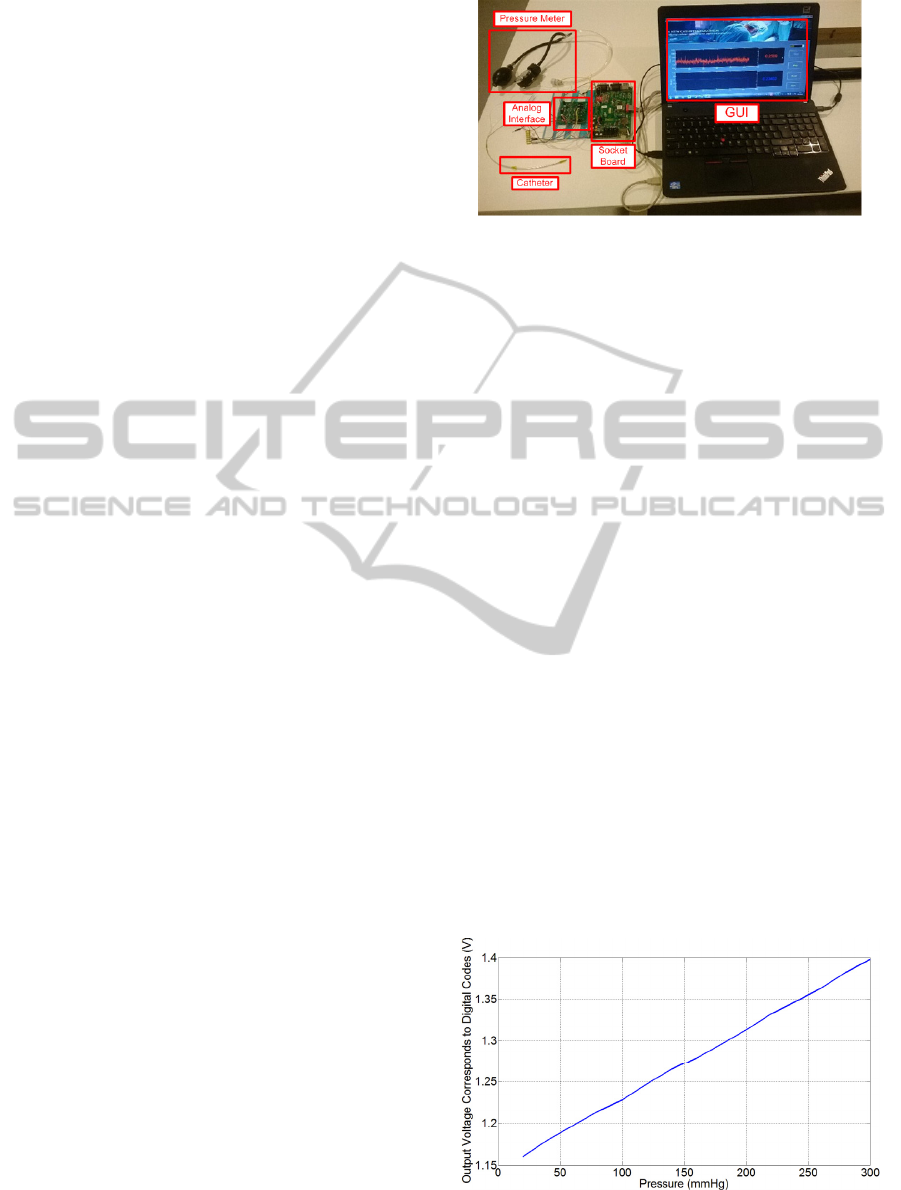
Figure 8: The measurement site of the propose system.
calculate the original physiological parameters using
the gathered digital codes. The main function of this
program is to analyze and display all the data
delivered by the socket board. It also records them
into files for future statistics and analysis.
5 MEASUREMENT RESULTS
The measurement site of the system is illustrated in
Fig. 8. A blood pressure meter based device is used
to control the pressure of catheter. The device
consists of an inflatable arm cuff, a manual gauge
and a rubber bulb for pumping up the cuff. The
internal pressure of the cuff hose with a catheter in it
is controllable by the rubber bulb. The manual gauge
can measure the pressure in the chamber to calibrate
the proposed mini-invasive system with the overall
pressure range from 20 mmHg to 300 mmHg above
1 atm. An incubator with thermostat is employed for
temperature sensor measurement. A connector
joining flexible PCB together is placed at the
proximal end of catheter. The analog interface board
connects to catheter by dupont lines. The socket
board records sensor data and feeds the serial digital
signal into the data recording and analyzing
computer. The computer can process the digital
codes by the program of the GUI.
Figure 9: The linearity relative to pressure.
BIODEVICES2015-InternationalConferenceonBiomedicalElectronicsandDevices
202
The linearity of the whole system for pressure
measurement is shown in Fig. 9 indicating that the
root mean square error (RMSE) is 1.43 mmHg.
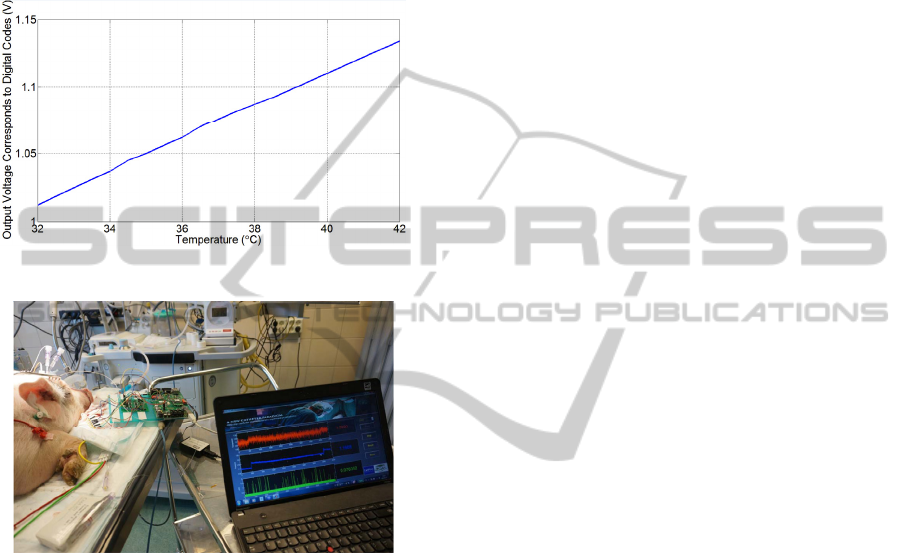
While the linearity of system for temperature
sensing is shown in Fig. 10 indicating that the
RMSE is 0.08 ºC. The catheter is also measured in
laboratory animals as shown in Fig. 11. The results
show the system works properly.
Figure 10: The linearity relative to temperature.
Figure 11: The animal experiment.
6 CONCLUSIONS
This paper proposed a smart catheter system to
acquire the ICP and temperature signal for TBI
measurement. A piezoresistive MEMS based
pressure sensor is mounted on a 1 mm (3 Fr)
diameter catheter to detect both pressure and
temperature, which minimizes the required catheter
space. Flexible PCB is inserted into the catheter for
signal transmission. An electronic system records
sensor signal and transmits the information to a
computer. Measurements results show the system is
able to sense the pressure in the range of 20-300
mmHg above 1 atm with RMSE of ±1.43 mmHg
and the temperature in the range of 32-42 ºC with
RMSE of ±0.08 ºC.
ACKNOWLEDGEMENTS
Dongxuan Bao thanks financial support from China
Scholarship Council for study at KTH-Royal
Institute of Technology. This work was supported in
part by Vinnova (The Swedish Governmental
Agency for Innovation Systems) through the Vinn
Excellence centers program.
REFERENCES
M. Faul, et al., 2010. Traumatic brain injury in the united
states: Emergency department visits, hospitalizations
and deaths 2002–2006. Centers for Disease Control
and Prevention, Injury Prevention & Control:
Traumatic Brain Injury.
Ségolène Mrozek, et al., 2012. Brain Temperature:
Physiology and Pathophysiology after Brain Injury.
Anesthesiology Research and Practice.
MedlinePlus, 2014. Intracranial pressure monitoring.
Available:http://www.nlm.nih.gov/medlineplus/ency/a
rticle/003411.htm.
Michael F. Stiefel, et al., 2005. Reduced mortality rate in
patients with severe traumatic brain injury treated with
brain tissue oxygen monitoring. J. Neurosurg. 103 (5),
805-811.
Yufridin Wahab, et al., 2008. Design of MEMS
biomedical pressure sensor for gait analysis. IEEE
International Conference on Semiconductor
Electronics. 166-169.
Emily Pritchard, et al., 2008. Flexible capacitive sensors
for high resolution pressure measurement. IEEE
Sensors. 1484-1487.
Li Xie, et al., 2012. Heterogeneous Integration of Bio-
Sensing System-on-Chip and Printed Electronics.
IEEE Tran. Emerging and Selected Topics in Circuits
and Systems. 2 (4), 672-682.
Chunyan Li, Raj K. Narayan, 2012. Development of a
novel catheter for early diagnosis of bacterial
meningitis caused by the ventricular drain. IEEE
International Conference on Micro Electro
Mechanical Systems (MEMS). 120-123.
W. P. Chan, et al., 2013. A pressure/oxygen/temperature
sensing SoC for multimodality intracranial neuro-
monitoring. IEEE Asian Solid-State Circuits Conf.
Dig. Tech Papers. 89-92.
CathPrint AB, 2014. Available: http://cathprint.se/.
Bengt Kallback, et al., 2009. Device for Invasive Use.
United States Patent Application 20090143651A1.
Texas Instruments, 2014. INA155. Available: http://www.-
ti.com/general/docs/lit/getliterature.tsp?genericPartNu
mber=ina155&fileType=pdf.
ASmartCatheterSystemforMinimallyInvasiveBrainMonitoring
203
