
Information Model for Radiology Performance Indicators
based on DICOM
Milton Santos
1
, Luís Bastião
2
, Alexandra Queirós
1
, Augusto Silva
3
and Nelson Pacheco Rocha
4
1
Health Sciences School/IEETA, University of Aveiro, Aveiro, Portugal
2
IEETA, University of Aveiro, Aveiro, Portugal
3
Department of Electronics, Telecommunications and Informatics/IEETA, University of Aveiro, Aveiro, Portugal
4
Heath Sciences Department/IEETA, University of Aveiro, Aveiro, Portugal
Keywords: DICOM Data Mining, Health Care Quality, Quality Dimensions, Radiology Quality Indicators.
Abstract: The paper presents the information model of the DICOM - Radiology Performance Indicator (DICOM-
RPI). This model can be used to aggregate information related to the characterization of medical imaging
health care services, namely information incorporated in the studies according to the format of the Digital
Imaging and Communication in Medicine (DICOM). The model comprises several components including
the ones required to define the context of medical imaging health care services (e.g. the entities involved)
and the context of use of the indicator (e.g. Quality Dimensions). For the validation of the proposed
information model 51,277 Digital Radiography (DX) studies performed on 27,559 patients from a single
health care facility were considered. The results of this validation within the scope of DX modality make
possible to anticipate the DICOM-RPI relevance in other imaging modalities and its contribution for
comprehensive analysis of medical imaging health care services.
1 INTRODUCTION
Whenever we seek to understand the concept of
quality of health care we find several definitions
(Piligrimiene and Buciuniené, 2008; Donabedian,
1988) which may vary over the course of time
(Pisco, 2007).
For the World Health Organization (WHO), the
quality of health care is understood as the extent to
which the provision of care meets the existing
professional standards which are thought to be
important for the patient (WHO, 2004). The
Organisation for Economic Cooperation and
Development (OECD) (Kelley and Hurst, 2006) uses
the definition of the Institute of Medicine (IOM)
(Lohr and Schroeder, 1990). According to this
definition, the quality of health care is defined as the
extent to which the provision of health care to the
individual or the population increases the probability
of achieving the desired health results, consistent
with the professional knowledge existing at the time.
The characterisation of the professional practice
with regards to the quality of health care provided,
may refer to the Structure, the Processes or the
Outcomes of the provision of care (Donabedian,
1988) in different Quality Dimensions such as, for
example, the ones recommended by the WHO
(WHO, 2007): Clinical Effectiveness, Staff
Orientation, Responsive, Efficiency, Safety,
Governance and Patient Centeredness. These
dimensions are also accepted in different countries,
namely United Kingdom, Canada, Australia or
United States of America, where other less common
dimensions are also considered, i.e. Acceptability,
Appropriateness, Competence or Capability,
Continuity and Timeliness (Kelley and Hurst, 2006).
The six dimensions recommended by WHO are
the bases of a conceptual model to allow health care
providers to assess their performance and which is
backed by a set of transversal and specific
indicators. Transversal indicators may be used in
every hospital and specific indicators are defined
according to the characteristics and the reality of
each health care facility (WHO, 2007). Furthermore,
the WHO conceptual model and the respective
indicators allow comparative characterisations of the
performances of different health care facilities
(WHO, 2007).
The OECD also has a long-term objective to
develop a set of indicators to robustly reflect the
quality of the provision of health care and to be
182
Santos M., Bastião L., Queirós A., Silva A. and Pacheco da Rocha N..
Information Model for Radiology Performance Indicators based on DICOM.
DOI: 10.5220/0005286201820190
In Proceedings of the International Conference on Health Informatics (HEALTHINF-2015), pages 182-190
ISBN: 978-989-758-068-0
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

disclosed in a reliable manner between different
countries using comparable data (Kelley and Hurst,
2006).
With regard to the European Union, in the scope
of the project Health Indicators for the European
Community, generic indicators were recommended
encompassing the major areas in public health, with
the definition of the following categories:
demography and socio-economic situation, health
status, determinants of health and health
interventions (Kramers, 2003).
In addition to enable the monitoring and
comparison of the existing data, the indicators are
used to develop policies (EC, 2013). Presently, there
are more than 40 core health indicators in the
European Union (EC, 2013). With regards to the
International Quality Indicator Project (Associates,
2010), indicators were developed in the areas of
emergency care, psychiatric care, continuing care
and home health care.
2 BACKGROUND
Performance indicators can be used differently:
either individually or in groups as part of an
integrated and interdependent set of measures or as
part of broader programmes. For instance, they can
be part of performance analysis frameworks and
certification programs developed by entities such as
Kings Fund (Kings Fund, 2014) or Joint
Commission International (Joint Commission,
2014).
With regards to medical imaging health care
services and respective Quality Dimensions, Lau
(2007) mentions the same dimensions that Kelley
and Hurst (2006) had identified in their paper for the
OECD. On the other hand, the definition of quality
in Radiology proposed by Hillman et al. (Hillman et
al., 2004), quoted in (Rubin, 2011), comprises the
dimensions related to Suitability of the Examination,
Suitability of the Protocol for the Procedure, Acuity
in Interpreting the Results, and Measurement and
Monitoring of the Improvement of the Performance
in Quality, Safety and Efficiency.
Also in the context of Radiology, Quality
Dimensions such as Safety, Efficiency,
Effectiveness, Opportunity or Focus on the Patient
are clearly seen in the professional practice (Kruskal
et al., 2009), as well as the need for improving
processes, professional performance and satisfaction
of patients and health care professionals (Johnson et
al., 2009).
The development and use of specific
performance indicators in Radiology may occur in
several situations with different objectives according
to the requirements of the stakeholders who use
them and the Quality Dimensions being considered.
Therefore, indicators may be required to analyse
financial aspects, productivity, possibility to conduct
studies, time spent doing and delivering medical
reports and patient satisfaction or to provide
information for continuous improvement of quality
programmes (Ondategui-Parra et al., 2004;
Ondategui-Parra et al., 2005; Ondategui-Parra et al.,
2006; Abujudeh et al., 2010; Kruskal et al., 2009).
In Radiology, the information concerning the
results of imaging procedures may be found in
medical reports, normally stored in the Radiology
Information System (RIS), or in images stored at the
Picture Archiving and Communication System
(PACS). Indeed, images stored in the format Digital
Imaging and Communication in Medicine (DICOM)
include data that identify the entities involved in the
studies as well the technical parameters used for the
completion, identification and transmission of the
images.
In general, PACS provide a limited set of search
functions, i.e. we can only use a restricted number of
DICOM fields to carry out queries. This means that
it is only possible to perform inflexible queries to
search DICOM data (Costa et al., 2009; Källman et
al., 2009).
Therefore, to enable customized queryng some
solutions have been developed to complement the
standart search options provided by PACS-DICOM
query and retrieve services (Vano et al., 2002; Vano
et al., 2005; Vano and Fernandez, 2007; Vano et al.,
2008; Källman et al., 2009; Stewart et al., 2007). A
solution that seeks to meet the requirements
mentioned previously is the Dicoogle tool (Costa et
al., 2011).
The purpose of this paper is to define and
validate an information model to support the
definition of DICOM Radiology Performance
Indicator (DICOM-RPI) taking into account the
diversity of contexts arising from different
professional situations such as those related to
health care facilities with distinct health care profiles
and providing different imaging modalities.
2 METHODOLOGY
The Dicoogle tool (Costa et al., 2011) can be used to
access and retrieve information included in the
DICOM metadata. This tool has already been
validated in hospital settings and allows data mining
InformationModelforRadiologyPerformanceIndicatorsbasedonDICOM
183

using DICOM metadata. Several initiatives
involving pilot studies conducted in different health
care facilities were implemented (Santos et al.,
2011, Santos et al., 2013), such as the analysis of X-
radiation exposure levels in mammograms (Santos et
al., 2014).
The access and retrieval of information included
in the DICOM metadata and its use as statistical
variables may occur in an isolated manner (e.g.
analysing the variation of the value of an attribute
throughout a certain period of time) or in
combination with other attributes, depending on the
goals to be attained. One way to promote its use is to
develop standardized performance indicators to
allow both intra-institutional and inter-institutional
benchmarking taking into consideration the
involving contexts. This means that a correct
characterisation of the context, although complex,
becomes the cornerstone for the assertiveness
needed to develop, maintain and use DICOM-RPI.
Keeping this in mind, the definition of an
information model that allows the characterisation of
indicators and respective contexts was achieved by
using the Unified Modelling Language (UML)
(Booch et al., 2001; Pender, 2004), in particular
class diagrams. The classes may represent
information objects from different sources, namely
PACS.
In this context, the DICOM metadata that is
relevant for DICOM-RPI can be obtained using
Dicoogle, especially to identify the different
stakeholders involved in the process of doing
imaging studies, such as, for example, the patient,
the health care facility or referring physician. This
approach enables the inclusion of information which
characterises the context in which the professional
activity unfolds.
The methodological approach that was followed
comprised two steps. First an information model was
defined and, afterwards, the model was validated
using data acquired by Dicoogle tool from 51,277
Digital Radiography (DX) studies of 27,559 patients
that were selected from 7,525,275 images, belonging
to 154,635 studies of 64,163 patients.
3 RESULTS
When defining the DICOM-RPI we consider that
they should be relevant for the analysis of the quality
of the professional practice in its different Quality
Dimensions (e.g. Security or Efficiency). The
Quality Dimensions may be included in different
Areas of Performance (i.e. Structure, Processes and
Outcomes). On the other hand, the Quality
Dimensions and the Areas of Performance to be
analysed rely on the context in which medical
imaging health care occurs.
3.1 The Information Model Supporting
DICOM-RPI
The DICOM-RPI comprises information that
characterise different aspects relevant for the
analysis of medical imaging health care provision. In
Figure 1 some concepts that can be part of a
DICOM-RPI and can characterise different levels of
information are presented.
When we analyse Figure 1, we see that the
definition of a DICOM-RPI requires the
characterisation of: Intervening Entity/ies; Quality
Dimensions; DICOM Metadata; Areas of
Performance; and Contexts of Use (e.g. where the
indicator was developed and used). On the other
hand, the specification of the Areas of Performance
is supported by information that identify the specific
area (i.e. Structure, Process or Outcomes) and the
respective sub-area (e.g. Use of Equipment,
Exposure Factors or the Number of Studies
Conducted by each Professional).
The information that characterises the Type of
Entity may include the entity’s address and is used
to identify the intervening entity.
Finally, the characterisation of the DICOM
Metadata includes the metric supporting the
DICOM-RPI as well as the Metadata Origin and the
Operational Definition.
Within the scope of the object-oriented
information modelling, the different concepts
presented in Figure 1 may represent different classes
which are related. Therefore, the Intervening Entity,
Quality Dimension, DICOM Metadata, Context of
Use and Area of Performance classes are related to
the DICOM-RPI class.
Keeping in mind the complexity of the
information associated to the different classes, they
must be divided into subclasses. This is the case of
the Intervening Entities class, which must include a
subclass supporting the identification of different
types of entities (e.g. manager, developer, user or
owner), or the Area of Performance class, which
must include subclasses supporting the identification
of the sub-area under analysis.
One way to generalise the information model
that supports DICOM-RPI is to define structures that
do not support only specific information, but also
information that is transversal to all indicators.
Within the scope of the model proposed in Figure 2,
HEALTHINF2015-InternationalConferenceonHealthInformatics
184
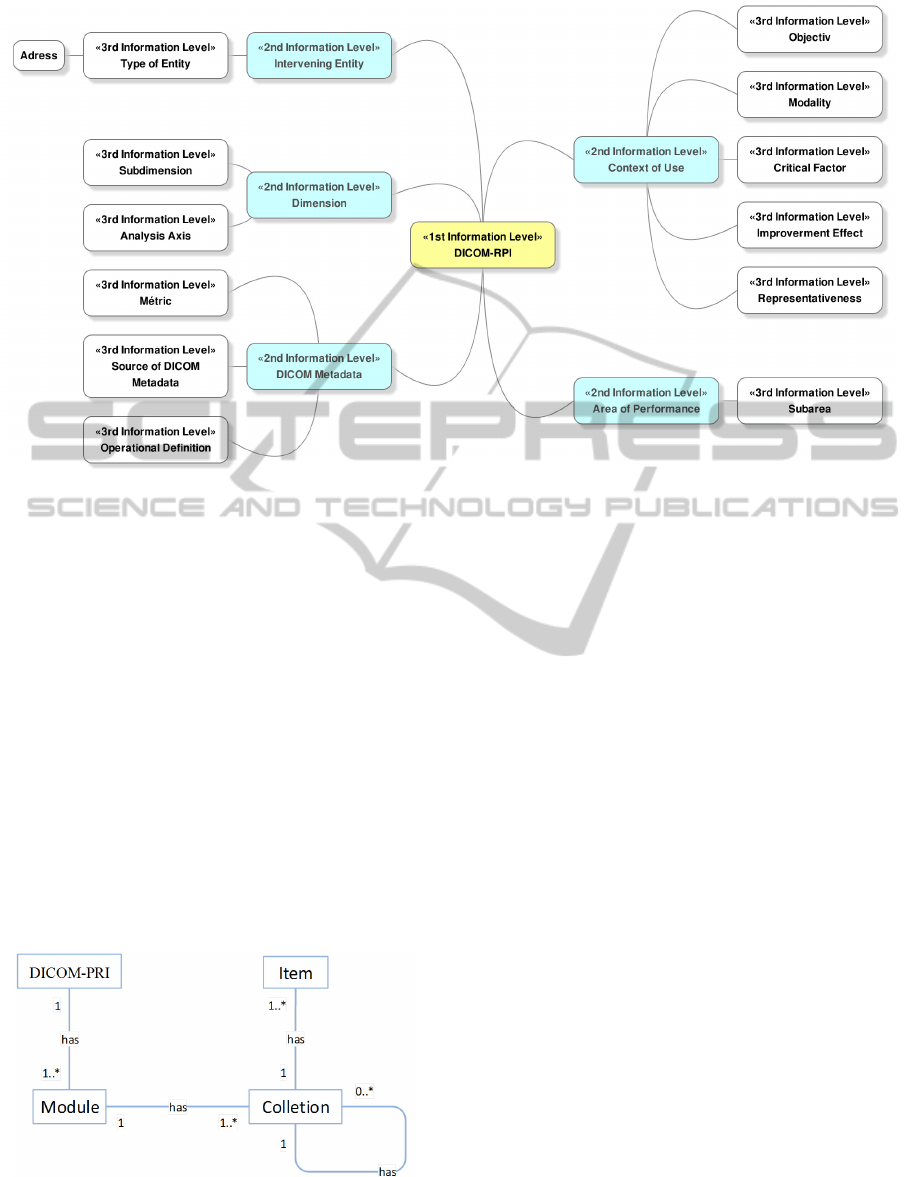
Figure 1: Different DICOM-RPI information levels (example).
the Modules and Collections are the elements
responsible for the flexibility and expandability of
the information structure. The possibility to use
different Modules and Collections, with different
structures, adapted to the reality under analysis,
enables the use of the DICOM-RPI information
model in different contexts and with different
purposes.
Therefore, a high-level generic information
model that supports the DICOM-RPI information
may be described as follows: Each DICOM-RPI
class (first level of detail) has one or more Module
classes (information of a second level of detail).
Each Module class has one or more Collection
classes (information of a third level of detail). Each
Collection class may or not include other Collection
classes that are characterised by one or more items
(Figure 2).
Figure 2: Generic information model supporting the
DICOM-RPI.
The definition of a DICOM-RPI, supported by the
information model being proposed always starts
with a question concerning the medical imaging
health care provision and access to the DICOM
metadata.
Taking into account the specific characteristics
of the different contexts in which the development
of indicators may occur, the related information can
be considered as persistent (e.g. the item Name or
Identifier) and as dynamic, (i.e. items related to the
specificity of each DICOM-RPI). The collected
information may be structured in several different
Collections of items belonging to different Modules
(Figure 3).
3.2 Validation of the Model
The validation of the information model was based
on data pertaining to the studies performed in a
health unit of average size (400 beds) during the
years 2011 and 2012. Data from 7 directories,
forming part of the PACS archive, were analysed in
a total volume of 4,152 TB of information. This
process lasted for 648 hours and resulted in the
collection of information on 7,525,275 images,
belonging to 154,635 studies performed by 64,163
patients.
For example, in Figure 4 presents a DICOM-RPI
related to the number of patients (based on the
DICOM attribute Patient ID) with DX modality
studies performed in the health care facility, as well
InformationModelforRadiologyPerformanceIndicatorsbasedonDICOM
185

1
*
1
1..*
1
0..1
1
0..*
1
1
1
1
1
1
1
1
1..*
1
1..*
1
0..*
1
1
DICOM‐RPI
CreationDate
ChangeDate
AreaofPerformance
Module
Designation
Identifier
Metric[collection]
Designation
Identifier
DICOMMetadata
MonitoringFrequency
Version
Designation
Identifier
TypeofDICOM‐RPI
Value
Version
CreationDate
ChangeDate
Sub‐area[collection]
Designation
Identifier
ContextofUse
IndicatorObjective
Coveredmodalities
Criticalfa cto rs
Effectof
Improvement
Query[collection]
Characterization
Representativeness[collection]
Designation
Identifier
HealthUnits
Patients
Studies
PeriodofAnalysis
OperationalDefinition[collection]
Designation
Identifier
OperationalDefinitionOrigin
ReferenceValue
Numerator
Denominator
UnitofMeasure
Identifier
DICOM attribute[collection]
Designation
Identifier
DICOMMetadataSource[collection]
Designation
Contact
Identifier
DimensionInterveningEntities
Sub‐Dimension[collection]
Identifier
Designation
AxisofAnalysis[collection]
Identifier
Designation
Entity[collection]
Designation
Identifier
Address
[collection]
Name
Street
TypeofEntity
Role
Responsibility
ProfessionalMembership
Contact
Location
PostalCode
City
country
Figure 3: Example of the instantiation of the Generic Information Model that supports DICOM-RPI.
as related to the values pertaining to the number of
patients with studies performed in a year (Macro
DICOM-RPI type), month (Intermediate DICOM-
RPI type), day (Elementary DICOM-RPI type), and
the number of female patients with studies
performed on that day (Sub-indicator DICOM-RPI
type). With regards to the period of time covered by
a DICOM-RPI, it arises from the query performed
on the repository of imaging studies. In the example,
the Analysis Axis is the number of patients. This
Analysis Axis is used in the scope of the
Radiological Security Sub-Dimension (with
ID:SD.1) belonging to the Security Dimension (with
ID:S.1), which in turn is part of the Area of
Performance Results (with ID:AP.1) (Figure 4).
The model must support information that
contributes to a better understanding of the DICOM-
RPI. In Figure 5, and as an example, information is
made available on the contextualisation of DICOM-
RPI with ID: 1.1.1.1 and whose analysis must
always take into account the intrinsic characteristics
of the indicator (e.g. Area of Performance, Quality
Dimension or Type of Indicator) as well as
information about the imaging modalities included
in each DICOM-RPI and the representativeness of
the data sample from which the value of the
indicator is obtained.
Particularly, the value for DICOM-RPI in Figure
5 is obtained from a sample of 27,559 patients and
the corresponding 5.1277 studies of the health care
facility throughout in 2011. The period covered by
DICOM-RPI is a day (24h). With regards to the
Operational Definition, it can be internal or external
to the health care facility. Additionally, its reference
value may be external or defined internally by the
user.
In Figure 5 there is information regarding the
number of patients with DX modality studies
performed in the health care facility per year as well
as the number of studies performed on those
patients. These data contribute to the
characterisation of the profile of health care
provision and to the critical analysis of the value
presented by DICOM-RPI (regarding the number of
patients with studies performed on 11/11/2011). The
characterisation of the entities intervening in the
definition, use and maintenance of the DICOM-RPI,
presented in Figure 6, is based on the role they take
HEALTHINF2015-InternationalConferenceonHealthInformatics
186
AreaofPerformance(ID): Results(AP.1)
Dimension(ID): Security(S.1)
Sub‐Dimension(ID): RadiologicSecurity(SD.1)
AnalysisAxisID): NumberofPatients(AA.1)
ID:1.1.1
Query:StudyDate:201111*ANDModality:DX
Value:3743
ID:1.1.1.1.1
Query:StudyDate:20111111*AND
PatientSex:FANDModality:DX
Value:87
TypeofDICOM‐RPI: Intermediate
ID:1.1.1.1
Query:StudyDate:20111111*AND
Modality:DX
Value:139
TypeofDICOM‐RPI: Elementary
TypeofDICOM‐RPI: Sub‐Indicator
TypeofDICOM‐RPI: Macro
ID:1.1
Query:StudyDate:2011*ANDModality:DX
Value:27559
AreaofPerformance(ID): Results(AP.1)
Dimension(ID): Security(S.1)
Sub‐Dimension(ID): RadiologicSecurity(SD.1)
AnalysisAxisID): NumberofPatients(AA.1)
ID:1.1.1
Query:StudyDate:201111*ANDModality:DX
Value:3743
ID:1.1.1.1.1
Query:StudyDate:20111111*AND
PatientSex:FANDModality:DX
Value:87
TypeofDICOM‐RPI: Intermediate
ID:1.1.1.1
Query:StudyDate:20111111*AND
Modality:DX
Value:139
TypeofDICOM‐RPI: Elementary
TypeofDICOM‐RPI: Sub‐Indicator
TypeofDICOM‐RPI: Macro
ID:1.1
Query:StudyDate:2011*ANDModality:DX
Value:27559
Figure 4: Example of DICOM-RPI types related to Area
of Performance “Results”.
on in the processes (Type of Entity). Here, we
characterise the entities responsible for developing
and managing a DICOM-RPI as well as the entity
owning the indicator. In the example there is only
information regarding the address of the DICOM-
RPI Proprietary Entity.
From the analysis of Figure 6 it can be seen that
all entities have an assigned responsibility, as well as
a unique identifier to identify them in a repository of
DICOM-RPI indicators.
The assertiveness of the use of DICOM-RPI
depends on many factors such as, for example, the
information that supports them, namely the Metric,
the DICOM attributes that were accessed and the
query method that was performed.
DICOM‐RPIdesignation
ID:
NumberofpatientswithDXradiographicstudiesperformedinone
day
1.1.1.1
CreationDate
AlterationDate
Version
10/11/2013 12/11/2013 1
TypeofDICOM‐RPI Value
Elementary 139
Module:ContextofUse
Designation ID Version
DICOM‐RPI1.1.1.1contextualization Context_1.1.1.1 V1
CreationDate AlterationDate
18/11/2013 ‐‐‐‐‐‐‐‐‐‐‐‐‐‐
Objective
Identifythenumberofpatientswithradiologicstudiesperformedinoneday
Modalities
DigitalRadiology
CriticalFactors EffectofImprovement
DICOMmetadataquality
DecreaseofpopulationexposuretoX
radiation
Collection:Representativeness
Designation Patients
HealthCareFacility1 27559patients/year
ID Studies
R.HD.HCF1.1.1.1.1 51277studies/year
HealthUnits PeriodofAnalysis
1 November112011(24h)
Collection:OperationalDefinition
Designation Origin
Numberofstudiesperformedduringaday(24h) Intern(HealthCareFacility1)
ID ReferenceValue
DO.1.1.1.1 (tobeestablishbytheuser)
Figure 5: Module “Context of Use”.
Module: Intervening Entities (related with 1.1.1.1 DICOM-RPI )
Designation: Version
DICOM‐RPI1.1.1Intervening
Entities
V.1
ID:
AlterationDate CreationDate
EI_1.1.1.1 19/11/2013
18/11/2013
Collection: Entity Collection:Entity
TypeofEntity: TypeofEntity:
DICOM‐RPIManager DICOM‐RPIManager
Name: Name:
UserA UserB
ID: ID:
1234 2345
Role: Role:
ResponsibleforQuality
Improvement
HeadofDepartment
(MD)
Responsibility: Responsibility:
DICOM‐RPIstorageand
management
DICOM‐RPIDefinition
ProfessionalMembership: ProfessionalMembership:
HealthCareFacility1exclusivity
(technologist)
HealthCareFacility1exclusivity
Contact: Contact:
UserA@gmail.com UB@outlook.com
Collection:Entity
Collection:Address
TypeofEntity: Name:
DICOM‐RPIProprietary HealthCareFacility1
Name: Street:
HealthCareFacility1 Mystreet
ID: Location:
3456 Mycity
Responsibility: PostalCode:
DICOM‐RPIProprietary 1111‐111Mycity
ProfessionalMembership: City:
StateDepartmentofHealth Mycity
Contact: Country:
HF1@ab.com Mycountry
Figure 6: Example of entities intervening in the definition
and use of a DICOM-RPI.
In Figure 7, and as an example, information is
provided about the data that support the DICOM-
RPI with ID: 1.1.1.1. With regards to the
characterisation of the Metric that supports the
indicator we verify that the denominator is 1.
InformationModelforRadiologyPerformanceIndicatorsbasedonDICOM
187

However, this value may be different. For example,
if we want to know the average number of patients
with studies performed per hour, the numerator of
the Metric would be the total number of studies
performed during the day and the denominator
would be the number of hours.
Module:DICOMMetadata(relatedwith1.1.1.1DICOM‐RPI)
Designation ID: Version:
1.1.1.1DICOM‐RPIMetadata D.1.1.1.1 V1
CreationDate: AlterationDate
18/11/2013 19/11/2013
Monitoring
Frequency:
Daily
Collection:Metric
Designation:
Numberofdigitalradiographystudies(DX)performedinaday.Metric
supportedbytheStudyInstanceUIDandStudyDateDICOMattributes
Numerator: Numberofdigitalradiographystudies(DX)performedinaday
Denominator:1
Unitof
Mesure:
Studies/Day
Collection:Query
ID.: P.1.1.1.1 Characterization: [StudyDate:20111111]
DICOMAttributes
Designation: StudyDate ID: [0008,0020]
DICOMMetadataSource
Designation: HealthCareFacility1PACS
ID: HealthCareFacility1
Contact: HF1@ab.com
Figure 7: Example of the data characterisation which
supports an DICOM-RPI.
As is the case with all information Modules, the
DICOM Metadata Module also has the creation date
(18/11/2013), the alteration date (19/11/2013), and
information regarding the version (Version V1). The
inclusion of the query that was used enables an
easier identification of the DICOM Metadata that
supports the DICOM-RPI.
In another aspect, the identification of the origin
of the DICOM metadata, in particular through its
naming, enables a faster communication between the
different stakeholders interested in the analysis and
use of DICOM-RPI.
4 DISCUSSION AND
CONCLUSION
This study has highlighted its relevance in the
definition of the DICOM-RPI. The information
model presented allows the use of DICOM metadata
to provide metrics as well the context of these
metrics. The characterisation of the origin of the
DICOM metadata that supports each indicator, as
well as the context in which it emerges, promotes a
better knowledge of the professional reality.
Therefore, the resulting metrics can be analysed in
accordance with the profile of provision of medical
imaging health care of different health care facilities.
The definition of the Area of Performance and
the Quality Dimension gives the information model
that supports the DICOM-RPI the scalability it
requires to be used in multiple professional settings.
On the other hand, it considers the information
pertaining to the different Quality Dimensions of
health recommended by different international
organizations (Kelley and Hurst, 2006; WHO, 2007)
as well as those outlined in the framework of
Radiology (Lau, 2007, Hillman et al., 2004; Johnson
et al., 2009; Kruskal et al., 2009; Rubin, 2011),
which may be useful to identify areas for
improvement in the provision of medical imaging
health care.
The use of DICOM-RPI, based on the proposed
information model, may contribute to the evaluation
of the provision of medical imaging services.
The inclusion of DICOM metadata in a
comprehensive structure of information that supports
DICOM-RPI contributes to the characterisation of
the quality of health care provision in Radiology.
This characterisation can be made in different Areas
of Performance and Quality Dimensions of medical
imaging health care provision.
The DICOM-RPI related to the professional
activity of the Radiology departments, supported by
the access to DICOM metadata using Dicoogle, may
become an important resource and valuable tool in
the characterisation of the quality of medical
imaging health care provision. However, the
validation of the information model that supports the
DICOM-RPI presented in this paper was only done
at the level of DX modality. Therefore, in future
work, it is relevant to develop strategies for the
consolidation of the information model in the scope
of other medical imaging modalities, as well as in
the scope of broader studies for the characterisation
of the professional practice in the Radiology
departments. On the other hand, the success of the
information model presented is dependent of the
understanding by all users of the semantics being
used and of the acceptance of a standardised
methodology for the definition of DICOM-RPI that
can be used by different stakeholders.
ACKNOWLEDGEMENTS
This work was partially supported by COMPETE -
Sistema de Incentivos à Investigação e
Desenvolvimento Tecnológico, Projectos de I&DT
HEALTHINF2015-InternationalConferenceonHealthInformatics
188

Empresas em co-promoção, under QREN
TICE.Healthy. LBS is funded by FCT, Fundação
para a Ciência e a Tecnologia, under the grant
agreement SFRH/BD/79389/ 2011.
REFERENCES
Abujudeh, H. H., Kaewlai, R., Asfaw, B. A., Thrall, J. H.,
2010. Quality Initiatives: Key Performance Indicators
for Measuring and Improving Radiology Department
Performance1. Radiographics, 30, 571-580.
Associates, P. G., 2010. International Quality Indicator
Project, viewed 2014-03-03,
«http://www.internationalqip.com/index-pt-PT.aspx».
Booch, G., Jacobson, I., Rumbaugh, J., 2001. The Unified
Modelling Language User Guide, Addison-Wesley.
European Comission, 2013. ECHI - List of Indicators,
viewed 2014-03-03, «http://ec.europa.eu/health/
indicators/echi/list/index_en.htm».
Costa, C., Ferreira, C., Bastião, L., Ribeiro, L., Silva, A.,
Oliveira, J., 2011. Dicoogle - an Open Source Peer-to-
Peer PACS. Journal of Digital Imaging, 24, 848-856.
Costa, C., Freitas, F., Pereira, M., Silva, A. Oliveira, J.,
2009. Indexing and Retrieving DICOM Data in
Disperse and Unstructured Archives. International
Journal of Computer Assisted Radiology and Surgery,
4, 71-77.
Donabedian, A., 1988. The Quality of Care: How Can it
be Assessed? JAMA, 260, 1743-1748.
Kelley, E., Hurst, J., 2006. Health Care Quality Indicators
Project: Conceptual Framework Paper. In: Dictorate
for Employment, L. A. S. A. G. O. H. (ed.).
Organisation for Economic Co-operation and
Development. «http://www.oecd.org/health/health-
systems/36262363.pdf».
Hillman, B. J., Amis JR, E. S., Neiman, H. L., 2004. The
Future Quality and Safety of Medical Imaging:
Proceedings of the Third Annual ACR FORUM.
Journal of the American College of Radiology, 1, 33-
39.
Johnson, C. D., Krecke, K. N., Miranda, R., Roberts, C.
C., Denham, C., 2009. Developing a Radiology
Quality and Safety Program: A Primer1.
Radiographics, 29, 951-959.
Joint Commission International. 2014. Pathway to
Certification.
«http://www.jointcommissioninternational.org/improv
e/get-certified/».
Kallaman, H.-E., Halsius, E., Olsson, M., Stenstrom, M.,
2009. DICOM Metadata Repository for Technical
Information in Digital Medical Images. Acta
Oncologica, 48, 285-288.
Kings Fund, 2014. Measurement and Performance.
«http://www.kingsfund.org.uk/topics/measurement-
and-performance».
Kramers, P., 2003. The ECHI Project: Health Indicators
for the European Community. The European Journal
of Public Health, 13, 101-106.
Kruskal, J. B., Anderson, S., Yam, C. S., Sosna, J., 2009.
Strategies for Establishing a Comprehensive Quality
and Performance Improvement Program in a
Radiology Department1. Radiographics, 29, 315-329.
Lau, L., 2007. Leadership and Management in Quality
Radiology. Biomed Imaging Interv Journal, 3, 21.
Lohr, K. N., Schroeders, S. A., 1990. A Strategy for
Quality Assurance in Medicare. New England Journal
of Medicine, 322, 707-712.
Ondategui-Parra, S., Bhagwat, J. G., Zou, K. H., Gogate,
A., Intriere, L. A., Kelly, P., Seltzer, S., Ros, P., 2004.
Practice Management Performance Indicators in
Academic Radiology Departments. Radiology, 233,
716-722.
Ondategui-Parra, S., Bhagwat, J. G., Zou, K. H.,
Nathanason, E., Gill, I., Ros, P., 2005. Use of
Productivity and Financial Indicators for Monitoring
Performance in Academic Radiology Departments:
U.S. Nationwide Survey. Radiology, 236, 214-219.
Ondategui-Parra, S., Erturk, S. M., Ros, P. R., 2006.
Survey of the Use of Quality Indicators in Academic
Radiology Departments. Am. J. Roentgenol., 187,
W451-455.
Pender, T., 2004. UML, A Biblia, Rio de Janeiro, Elsevier.
Piligrimiene, Z., Buciuniené, I., 2008. Different
Perspectives os Health Care Quality: Is the Consensus
Possible? Economics of Engineering Decisions, 104-
110.
Pisco, L. 2007. Perspectivas Sobre a Qualidade na Saúde.
«http://www.dge.ubi.pt/aalmeida/Gestao-medicina-11-
12/Perspectivas%20 qualidade%20saude.pdf».
Rubin, D., 2011. Informatics in Radiology: Measuring and
Improving Quality in Radiology: Meeting the
Challenge with Informatics. Radiographics, 31, 1511-
1527.
Santos, M., Couto, P., Silva, A., Rocha, N., DICOM
metadata-mining in PACS for Computed Radiography
X-Ray Exposure Analysis. A Mammography Multisite
Study. European Congress of Radiology, 2014
Vienna, Austria.
Santos, M., De Francesco, S., Bastião, L., Silva, A., Costa,
C., Rocha, N., Multi vendor DICOM metadata access
a multi site hospital approach using Dicoogle. Infor-
mation Systems and Technologies (CISTI), 2013 8th
Iberian Conference on, 19-22 June 2013 2013. 1-7.
Santos, M., Bastião, L., Costa, C., Silva, A., Rocha, N.,
2011. DICOM and Clinical Data Mining in a Small
Hospital PACS: A Pilot Study. In: Cruz-Cunha, M.,
Varajão, J., Powell, P., Martinho, R. (eds.)
ENTERprise Information Systems. Springer Berlin
Heidelberg.
Stewart, B. K., Kanal, K. M., Perdue, J. R., Mann, F. A.,
2007. Computed Radiography Dose Data Mining and
Surveillance as an Ongoing Quality Assurance
Improvement Process. Am. J. Roentgenol., 189, 7-11.
Vano, E., Fernandez, J. M., Ten, J. I., Guibelalde, E.,
Gonzalez, L., Pedrosa, C., 2002. Real-Time
Measurement and Audit of Radiation Dose to Patients
Undergoing Computed Radiography. Radiology, 225,
283-288.
InformationModelforRadiologyPerformanceIndicatorsbasedonDICOM
189

Vano E., Fernandez Soto J.M., 2007, Patient dose
management in digital radiography, Biomed Imaging
Interv J; 3(2):e26.
Vano, E., Padovani, R., Bernardi, G., Ten, J. I., Peterzol,
A., Dowling, A., Bosmans, H., Kottou, S., Olivari, Z.,
Faulkner, K., Balter, S., 2005. On the Use of DICOM
Cine Header Information for Optimisation: Results
from the 2002 European DIMOND Cardiology
Survey. Radiat Prot Dosimetry, 117, 162-165.
Vano, E., Ten, J. I., Fernandez, J. M., Prieto, C., Ordiales,
J. M., Martinez, D., 2008. Quality Control and Patient
Dosimetry in Digital Radiology. On Line System:
New Features and Transportability. Radiation
Protection Dosimetry, 129, 144-146.
WHO, World Health Organization Centre for Health
Development, 2004. A Glossary of Terms for
Community Health Care and Services for Older
Persons, Ageing and Health Technical Report.
Geneva: World Health Organization.
WHO, World Health Organization, 2007. PATH:
Performance Assessment Tool for Quality
Improvement in Hospitals. In: Systems, D. O. C. H.
(ed.). Spain: World Health Organization.
HEALTHINF2015-InternationalConferenceonHealthInformatics
190
