
Telegeriatrics
A Pilot Project to Reduce Unnecessary Hospital Admissions of Nursing Home
Residents in Singapore
H. J. Toh
1
, Chia J.
1
, E. Koh
2
, K. Lam
1
, G. C. Magpantay
1
, C. M. De Leon
1
, J. A. Low
3
1
gericare@north, AHS programme office, Khoo Teck Puat Hospital, Singapore, Singapore
2
Ageing-In-Place, AHS Programme Office, Khoo Teck Puat Hospital, Singapore, Singapore
3
Department of Geriatric Medicine and Palliative Care, Khoo Teck Puat Hospital, Singapore, Singapore
Keywords: Telemedicine, Telecommunications, Healthcare, Hospitalizations, Nursing Home, Nursing Home Residents,
Community Care.
Abstract: Geriatric specialists have been scarce in Singapore and this has drawn attention to a rising need in providing
quality care for the ageing society. Access to geriatric care could decrease nursing home to acute hospital
transfers, thus improving residents’ quality of life. A pilot project implemented by an acute hospital in
Singapore aims to use videoconferencing systems to improve access to geriatric specialist care for nursing
homes and thereby reduce unnecessary acute hospital admissions. We aim to assess the impact of the level
of engagement with Telegeriatrics has on nursing home to hospital transfer rates. Two nursing homes were
recruited from December 2010 to March 2014. A total of 379 telemedicine consultation episodes were
conducted over this period. Hospital admission rates were monitored over a 2-year period and compared
against the nursing home’s level of engagement with Telegeriatrics. The more-engaged nursing home
reported a significant decrease of 29% in hospital admission rates. In contrast, the less-engaged nursing
home only reported a 6% decrease. The findings show a reduction in hospital admission rate for both
nursing homes. When the two nursing homes were compared, the nursing home that was more engaged with
Telegeriatrics had a lower rate of unnecessary hospital admission. Telegeriatrics has the potential to reduce
unnecessary hospitalisation frequently experienced by nursing home residents. Furthermore, a decrease in
hospital readmission rates enables hospital beds to be better utilised, reduces medical spending and relieves
residents’ distress.
1 INTRODUCTION
Older people often require complex healthcare
treatment which may include hospitalizations.
However, several studies have shown that a large
percentage of people aged 65 years and above were
sent to hospitals for potentially preventable
conditions (Kim, et al., 2001; Wolff et al., 2002).
Singapore faces a rapidly ageing population and
a greater prevalence of chronic diseases (Cheah and
Heng, 2001; Cheah, 2001). Frequent hospitalizations
of nursing home (NH) residents is a growing
concern in Singapore as they result in increased
healthcare costs, hospital-acquired infections,
complications and morbidities. Furthermore, the
hospitalizations exert pressure to the healthcare
system’s problem of severe bed crunch (Tan, 2013).
Therefore, interventions involving frail NH residents
are needed to reduce unnecessary hospital
admissions while improving quality of care.
The specialized field of geriatrics has improved
diagnosis and treatment of common geriatric
problems such as falls (Tinetti et al., 1994), urinary
incontinence
8
, and delirium (Inouye, 1999). In order
to develop comprehensive care plans for frail elderly,
geriatricians also address social issues like economic
and demographic issues, lifestyle choices, social
isolation, and caregiver stress. Assessing and
considering these factors into an integrated plan of
care result in reduced rates of hospitalization, with
some studies suggesting a reduction in medical care
spending (Day and Rasmussen, 2004; Ellis et al.,
2011).
Currently, care of NH residents is largely
provided by the nursing staff and supplemented by
occasional visits by general practitioner. Lack of
91
J. Toh H., J. C., Koh E., Lam K., C. Magpantay G., M. De Leon C. and A. Low J..
Telegeriatrics - A Pilot Project to Reduce Unnecessary Hospital Admissions of Nursing Home Residents in Singapore.
DOI: 10.5220/0005436800910096
In Proceedings of the 1st International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AgeingWell-
2015), pages 91-96
ISBN: 978-989-758-102-1
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

geriatric specialist care has led to sub-optimal care
and potentially preventable NH to acute hospital
transfers (Ouslander et al., 2009).
Videoconferencing is a possible method to
provide telemedicine (Moehr et al., 2005; Casavant
et al., 2014) and tele-education (Graham, 2002;
Pedley, 2003). Telegeriatrics is an acute hospital’s
initiative to extend care from the acute hospital to
the NHs in the northern part of Singapore. Initiated
in December 2010, Telegeriatrics enabled the acute
hospital to deliver geriatric medical care to two
partnering NHs via videoconferencing. The aim of
this intervention is to promote early identification of
potential medical problems in NH residents so that
appropriate and timely medical interventions can be
carried out. Early medical interventions can reduce
the deterioration of medical conditions and non-
urgent use of emergency departments. In order to
achieve this aim, two main approaches are used in
Telegeriatrics: telemedicine consultation and
Telegeriatrics Nurse Training Course (TNTC).
Telemedicine consultation is a live, interactive
video technology that allows the NH nurse and
resident to communicate with the geriatrician
remotely. TNTC is a 9-months course that aims to
enhance the knowledge and skills of NH nurses to
carry out telemedicine-specific duties and improve
the management of medical conditions. Activities
that are necessary for the proper governance of NHs,
for example, multidisciplinary meetings and
mortality audits, are conducted regularly through the
videoconferencing system.
This study was conducted to assess whether
increased level of engagement with Telegeriatrics
translates to lower hospital admissions.
2 METHODS
2.1 Ethics Approval
Ethics approval was obtained from the National
Healthcare Group Domain Specific Review Board
(DSRB).
2.2 Recruitment & Setting
Over the study period from December 2010 to
March 2014, two non-profit NHs agreed to
participate in the study. They were selected as they
had existing partnership with the acute hospital.
NH1 began its partnership with the acute hospital
in December 2010 while NH2 joined in April 2012.
During the study period, both NHs were not
involved in any other interventions related to
reducing residents’ hospital admissions.
2.3 Telemedicine Consultation
The technology involved in this project included
software, hardware, and infrastructure setups. The
equipments used for carrying out two-way
videoconferencing included a high-resolution
camera and high-definition video monitor installed
in the acute hospital and the two NHs. These
equipments were mounted on a portable trolley
enabling telemedicine consultations at different
locations. For example, residents on wheelchairs
arewere wheeled to the consultation room while bed-
bound residents will have telemedicine consultations
by their beds.
Before consultation, the TNTC-trained nurse
identifies residents requiring specialist care for
consultation. During consultation, the nurse presents
the residents to the geriatrician, and conducts basic
clinical assessments on the residents. The
geriatrician discusses the medical problems with the
nurse and recommends a treatment plan. The
telemedicine consultation is documented in a
telemedicine consultation form. After consultation,
the form is endorsed by the geriatrician and emailed
to the NH so that the nurses can follow up with the
treatment plan. The form is then filed in the
resident’s case notes.
2.4 Continuous Nurse Training &
Education
Before telemedicine consultations can be carried out,
selected registered nurses from the NHs have to
undergo the TNTC to equip them with the necessary
skills and knowledge. This course is conducted by
the acute hospital’s clinical educators. The TNTC
includes early identification of changes in residents’
medical condition; presenting and documenting
residents’ case history in a systematic way; and
management of basic medical conditions.
In addition, as a part of continuing nursing
education, multidisciplinary meetings were held
among the geriatrician, the TNTC-trained nurses,
and other healthcare professionals. The purpose is to
promote discussions and knowledge-sharing on the
diagnostics and treatment aspects of resident care,
allowing for collective, evidence-based
recommendations, for better resident management.
In a mortality audit session, the geriatrician and
the nurses review deaths of particular residents to
identify and evaluate deficiencies of care in
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
92

practices, and make recommendations for
improvement.
2.5 Data Collection
We measured and compared the hospital admission
rate of two NHs from December 2010 to
March 2014. The hospital admission rate was
measured at two points: before joining Telegeriatrics
and 2 years after joining Telegeriatrics.
Hospitalization rates were obtained from the
monthly data sent by the NHs to the acute hospital.
Other data including demographics, health data and
consultation details were collected from the Resident
Assessment form (RAF), resident case notes and
telemedicine consultation form.
2.6 Statistical Analyses
Factors that affect the NH’s extent of engagement
with Telegeriatrics include number of scheduled and
ad-hoc telemedicine consultations, multidisciplinary
meetings and mortality audits. We defined the NH
with the higher number of telemedicine-related
activities as “more-engaged”, and the other NH as
“less-engaged”.
In examining NH residents’ hospitalizations, a
comparison of hospital admission rates before and
during intervention was conducted. Univariate
analysis was performed to study the differences
between the more-engaged and the less-engaged NH.
We also investigated whether the factors that
influenced the level of engagement with
telemedicine had any impact on the NH’s hospital
admission rates.
Data was analyzed using SPSS version 22.0 for
Windows (SPSS Inc., Chicago, IL, USA).
3 RESULTS
A total of 379 episodes of telemedicine consultation
were conducted for 198 unique residents during the
study period. The average consultation time per
resident is 22 minutes (range 5-75 minutes). In 90%
of the consultations, the resident had multiple
comorbidities. Polypharmacy was present in 35% of
the consultations. Recent history of admission
(within the last 6 months) was present in 34%. The
demography of residents who have undergone
telemedicine consultation is summarised in Table 1.
The average age of residents of the two NHs
requiring specialist telemedicine consultations was
75 years (range 15-103), with 78% aged 65 years
Table 1: Demography of residents (N = 198).
Characteristic
NH1
(N=101)
NH2
(N=97)
Gender
Female
65 (64%) 38 (39%)
Race
Chinese
87 (86%) 69 (71%)
Malay
5 (5%) 12 (12%)
Indian
4 (3%) 16 (16%)
Others
5 (5%) 0 (0%)
Functional Category
I
0 (0%) 1 (1%)
II
3 (4%) 5 (5%)
III
46 (45%) 49 (51%)
IV
52 (51%) 42 (43%)
and older. Their average length of stay in the NH
was 35 months (range 1-275). Majority were
Chinese, and almost all belonged to the functional
category III and IV. NH residents’ physical,
psychological, social and emotional needs are
assessed using the RAF and classified into 4
functional categories from I to IV. Those in category
I are the least dependent on others for care while
category IV residents are fully dependent on others
for care.
Table 2: Factors affecting the level of Telegeriatrics
engagement.
Factors
NH1 NH2
Scheduled consultations 72 52
Ad-hoc consultations 17 8
Residents seen at
scheduled consultations
207 147
Residents seen at
ad-hoc consultations
17 8
Multidisciplinary meetings 18 3
Cases reviewed during
multidisciplinary meetings
37 4
Mortality audits 15 7
Cases reviewed during
mortality audits
39 12
Table 2 presents the factors affecting the NH’s
engagement level with Telegeriatrics. NH1 carried
out more telemedicine-related activities when
compared to NH2. Significant differences were
found in factors such as the number of scheduled
telemedicine consultation sessions, residents who
have undergone telemedicine consultation and cases
reviewed during multidisciplinary meetings.
The presenting complaints that led to
telemedicine consultations are presented in Table 3.
The overall ranking of presenting complaints
reveals that dementia-related behavioural problems
Telegeriatrics-APilotProjecttoReduceUnnecessaryHospitalAdmissionsofNursingHomeResidentsinSingapore
93
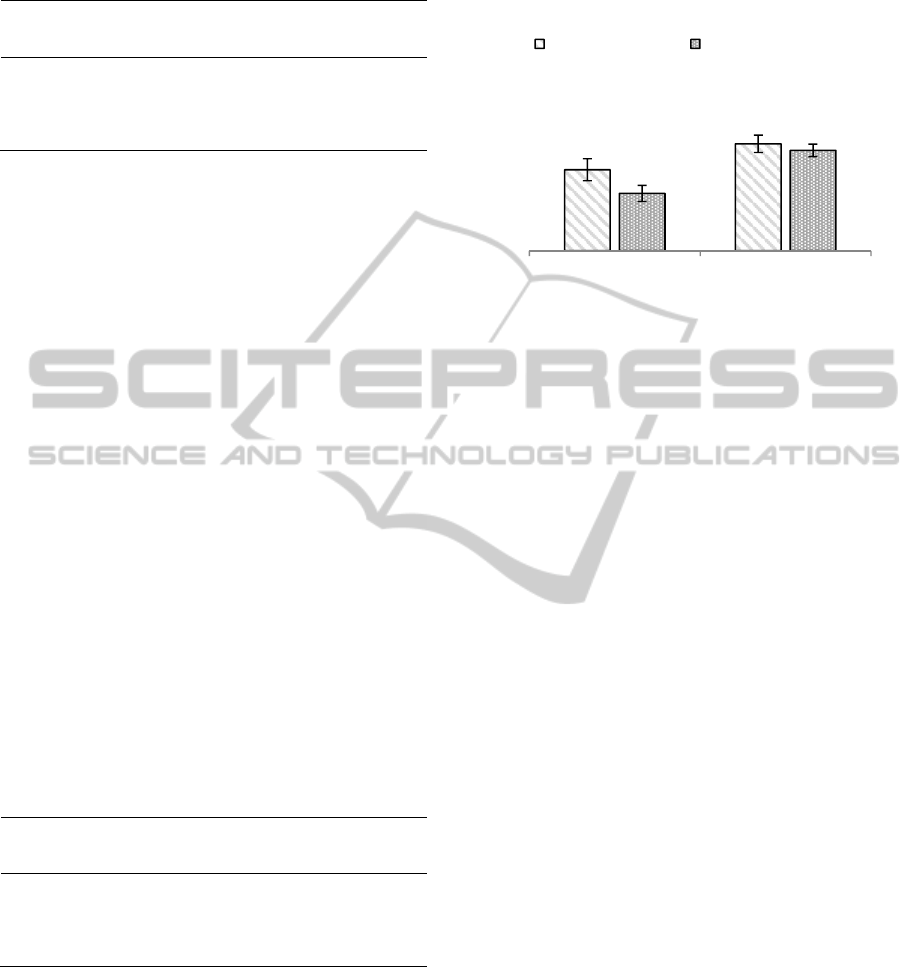
Table 3: Most common presenting complaints referred for
telemedicine consultations.
NH1
Presenting
Symptom (%)
NH2
Presenting
Symptom (%)
Behavioural problem (32) Behavioural problem (27)
Medication review (18) Medication review (14)
Skin lesion / rash (8) Management review (8)
Fever (6) Oedema (7)
Poor appetite (4) Skin lesion / rash (6)
were perceived by the nurses to be the most
unmanageable. It was the top presenting problem
referred for specialist telemedicine consultations.
The next most frequently referred presenting
problem by the NHs was medication review. In a
study conducted in NHs in Singapore (Mamun,
2004), a high prevalence of polypharmacy and
inappropriate medication use is observed in the NHs.
The current practice of medication use in the NHs
may lead to adverse drug reactions and interactions.
Review of medication on a timely basis is therefore
a good practice for the geriatricians to adopt to
reduce polypharmacy (Walsh and Cussen 2010;
Finkers et al., 2007).
Skin-related problems such as rashes and
cellulitis were also referred by the NHs for
consultations. The other common presenting
complaints were different for the two NHs. NH1
prioritized fever and poor appetite as concerns which
required specialist consultation, while the NH2 tend
to seek consultations for a follow-up review of
previous management and oedema.
The most common diagnoses made by the
geriatricians during telemedicine consultations are
shown in Table 4.
Table 4: Most common category of primary diagnoses in
telemedicine consultations.
NH1
Diagnosis
Category (%)
NH2
Diagnosis
Category (%)
General (31) General (26)
Neurologic (23) Psychiatric (19)
Skin rash (17) Infectious (17)
Psychiatric (13) Neurologic (12)
Neoplastic (7) Skin rash (7)
The most common category of primary diagnoses
made in telemedicine consultations for both NHs
was general (mainly poor appetite, muscular pain,
constipation, and nausea).
The other common diagnoses were neurologic-
related (mainly vascular dementia and Alzheimer’s
disease), psychiatric-related (mainly depression and
anxiety) and skin rash. Other conditions in the NHs
were more commonly diagnosed as infectious-
related (mainly cellulitis, infected wound and
pressure ulcer), and neoplastic (mainly metastatic
lung cancer).
Figure 1: Average monthly rate of hospitalizations per
100,000 resident days.
The average monthly hospitalization rate for NH1
before joining Telegeriatrics was 144 per 100,000
resident-days (Figure 1). At two years after joining
Telegeriatrics, the hospitalization rate had
significantly decreased by 29%. In NH2, a 6%
decrease in hospitalization rate was observed 2 years
after joining Telegeriatrics (P>0.01).
4 DISCUSSION
NH1 is categorized as “more-engaged” as it had a
higher number of telemedicine-related activities, and
NH2 as “less-engaged”.
We observed a statistically significant effect with
the use of telemedicine on hospitalization rates in
the more-engaged NH. Similarly, in a study
9
where
the 4 more-engaged skilled nursing facilities were
compared with 2 less-engaged ones, a significant
decline was found in the hospitalization rate of the
more-engaged facilities. The hospitalization rate for
non-engaged facilities was very similar to that of the
control facilities. Hence, it is likely that if NHs were
to be less engaged in the intervention, they appear to
perform like NHs which were never exposed to the
intervention.
Telemedicine may contribute towards achieving
the goal of improving clinical care. Its potential role
in addressing issues arising from an ageing
population, chronic conditions and rising healthcare
costs has been emphasized by the European
healthcare community
(European Commission,
2009). Studies have demonstrated that the use of
telemedicine in accessing care improves quality of
patient monitoring, and reduces hospitalizations and
144
190
102
178
More-Engaged NH Less-Engaged NH
Rate of hospitalizations per
100,000 resident days
Pre-Intervention During-Intervention
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
94

emergency department visits (Smart, 2011; Vander
Werf, 2004; Taylor et al. 2014). A study conducted
by the U.S. Department of Veteran Affairs (VA) on
281 patients with chronic illnesses demonstrated a
significant reduction in emergency department visits
and hospitalizations. Furthermore, there were high
levels of patient satisfaction and improved
perceptions of physical health (McLean et al., 2012).
The two NHs were scheduled for a weekly
consultation session and a bi-weekly session of
multidisciplinary meeting and mortality audit during
the study period. There was no restriction to the
number of cases that can be referred to the
geriatrician for each of these sessions. The less-
engaged NH referred fewer cases to each session
and during the last 3 months of the study period,
there was no telemedicine consultation session due
to cancellation initiated by the NH. However, the
more-engaged NH carried out consultations as per
normal. Also, shortly after the start of Telegeriatrics,
the less-engaged NH experienced a change in
management and three TNTC-trained nurses
resigned. The new management was not actively
engaged in Telegeriatrics. For the more-engaged NH,
there was no management and nurse turnover over
the course of Telegeriatrics. Many struggling
telemedicine programme innovators did not realize
that technology implementation is a social process
and requires the personnel in following through the
programme. The presence of a leader who can
manage day-to-day operations and encourage staff
acceptance is the key to achieve desired changes in
practice and targeted outcomes
25
. A study showed
that the leading reason for successful adoption of
telemedicine was that the support team had actively
identified barriers and found ways to address them
(Ellis et al., 2001). The programme champions
devoted time and effort in garnering resources for
consistent improvement and innovation, and
encouraging staff adoption (Chaiyachati et al., 2014).
The results of this study must be interpreted with
care because of its small sample size and lack of
randomization. However, this study provided
preliminary results from a comparison between a
more-engaged NH and a less-engaged NH. Hence, it
can be tested more rigorously with enrollment of
larger, randomized and more diverse sample of NHs.
Also, a control NH that did not receive telemedicine
consultations or received face-to-face consultations
was not included.
This study did not include unmeasured
confounding factors that could influence the level of
engagement of the NHs with Telegeriatrics. Thus,
the differences in hospitalizations observed between
more- and less-engaged facilities may not be of
significance, after adjusting for these unmeasured
factors.
Also, in this study, reduced hospitalizations were
regarded as the primary positive outcome of the
Telegeriatrics. Other telemedicine-related outcomes
such as the health-related quality of life and
functional status, and resident satisfaction with care
were not measured.
5 CONCLUSIONS
This pilot project showed promise for reducing
unnecessary hospital admissions among NH
residents. The early identification of clinical issues
and access to specialist support provided alternatives
to hospital care. By doing so, it could potentially
contain costs while optimizing resident outcomes.
It is observed from this study that increased
engagement with telemedicine could be fundamental
in preventing unnecessary hospitalizations. Savings
from hospitalizations were only apparent in the NH
that had a greater usage of telemedicine (Grabowski
and O’Malley, 2014). The intervention, even when
made available to the NH, does not guarantee the
NH staff’s active involvement. Telemedicine
providers will have to put in further efforts to
encourage engagement from the NHs. The
successful adoption of technological-related
interventions was reported to be generally due to
continuous support and comprehensive guidance
from the management (Moehr et al., 2006; Murray et
al., 2011). A team of skilled and knowledgeable NH
staff who work effectively together is crucial to
sustain the operations of using telemedicine, in order
to manage current and future influences.
Further work would be to measure the quality
outcome indicators, in order to better comprehend
the intrinsic value of distance support. These
indicators should measure mortality, cost savings,
and user satisfaction with the programme. Further
research is needed to qualitatively look into how the
NH users perceived Telegeriatrics and the barriers
that they face, which could potentially affect the
NH’s engagement level with Telegeriatrics.
REFERENCES
Kim, H. et al., 2001. ‘Potentially preventable
hospitalizations among older adults with diabetes.’
The American Journal of Managed Care, vol. 17, no.
1, pp. 419-26.
Telegeriatrics-APilotProjecttoReduceUnnecessaryHospitalAdmissionsofNursingHomeResidentsinSingapore
95

Wolff, J. L. et al., 2002. ‘Prevalence, Expenditures, and
Complications of Multiple Chronic Conditions in the
Elderly.’ Archives of Internal Medicine, vol. 162, pp.
2269-276.
Cheah, J. and Heng, B.H., 2001. ‘Implementing chronic
disease management in the public healthcare sector in
Singapore: the role of hospitals.’ World Hospitals
and Health Services, vol. 37, no. 3, pp.19-23, 40-3.
Cheah, J., 2001. ‘Chronic disease management: a
Singapore perspective.’ BMJ, vol. 323, no.7319, pp.
990-993.
Tan, J. (2013, February 19). Hospital-Acquired
Infections. The New Paper, p. 7.
Tinetti, M. E. et al., 1994. ‘A multifactorial intervention to
reduce the risk of falling among elderly people living
in the community.’ The New England Journal of
Medicine, vol. 331, pp. 821–827.
Burgio, K. L. et al., 1998. ‘Behavioral vs drug treatment
for urge urinary incontinence in older women: A
randomized controlled trial.’ The Journal of the
American Medical Association, vol. 280, pp. 1995–
2000.
Inouye, S. K. et al., 1999. ‘A multicomponent intervention
to prevent delirium in hospitalized older patients.’ The
New England Journal of Medicine, vol. 340, pp. 669–
676.
Day, P. and Rasmussen, P., 2004. ‘What is the evidence
for the effectiveness of specialist geriatric services in
acute, post-acute and sub-acute settings? A critical
appraisal of the literature.’ New Zealand Health
Technology (NZHTA) Report, vol. 7, no. 3, pp. 1–169.
Ellis, G. et al., 2011. ‘Comprehensive geriatric assessment
for older adults admitted to hospital: metaanalysis of
randomised controlled trials.’ BMJ , vol. 343, d6553.
Ouslander, J. G., 2009. ‘Reducing potentially avoidable
hospitalizations of nursing home residents: the
INTERACT II project.’ Florida Medical Directors
Association (FMDA) Progress Report.
Moehr, J. R. et al., 2005. ‘Video conferencing-based
telehealth--its implications for health promotion and
health care.’ Methods of Information in Medicine, vol.
44, no. 2, pp. 334-341.
Casavant, D. W., et al. 2014. ‘Trial of telemedicine for
patients on home ventilator support: feasibility,
confidence in clinical management and use in medical
decision-making.’ Journal of Telemedicine and
Telecare, vol. 20, no. 8, pp. 441-449.
Graham, A. R., 2002. ‘Teleeducation in medicine: why
and how.’ Riv Med Lab – JLM, vol. 3, no. 1, pp. 24–
26.
Pedley, D. et al., 2003. ‘A role for teleeducation in the
centralization of accident and emergency
services.’ Journal of Telemedicine and Telecare, vol. 9
no. 1, pp. 33–34.
Mamun, K. et al., 2004. ‘Polypharmacy and inappropriate
medication use in Singapore nursing homes.’ Annals
of the Academy of Medicine, Singapore, vol. 33, no. 1,
pp. 49-52.
Walsh, E. K. and Cussen, K., 2010. ‘"Take ten minutes": a
dedicated ten minute medication review reduces
polypharmacy in the elderly.’ The Irish Medical
Journal, vol. 103, no. 8, pp. 236-38.
Finkers, F. et al., 2007. ‘A study of medication reviews to
identify drug-related problems of polypharmacy
patients in the Dutch nursing home setting.’ Journal of
Clinical Pharmacy and Therapeutics, vol. 32, no. 5,
pp. 469-76.
Special issue on healthcare: healthy ageing and the future
of public healthcare systems. European Commission
(2009). Available at: http://ec.europa.eu/research/
social-sciences/pdf/efmn-special-issue-on-
healthcare_en.pdf. (Accessed November 22, 2011).
Smart, N., 2011. ‘Exercise training for heart failure
patients with and without systolic dysfunction: an
evidence-based analysis of how patients benefit.’
Cardiology Research and Practice vol. 2011.
Vander Werf, M., 2004. ‘Ten critical steps for a successful
telemedicine program.’ Studies in Health Technology
and Informatics, vol.104, pp. 60-68.
Taylor, J. et al., 2014. ‘Examining the use of telehealth in
community nursing: identifying the factors affecting
frontline staff acceptance and telehealth adoption.’
Journal of advanced nursing vol.71, no. 2.
McLean, S. et al., 2012. ‘Telehealthcare for chronic
obstructive pulmonary disease. Cochrane Review and
meta-analysis.’ British Journal of General Practice,
vol. 62, no. 604, pp. 739–749.
Ellis, D. G. et al., 2001. ‘A telemedicine model for
emergency care in a short-term correctional facility.’
Telemedicine journal and e-health, vol. 7, no. 2, pp.
87-92.
Chaiyachati, K. H. et al., 2014. ‘Continuity in a VA
Patient-Centered Medical Home Reduces Emergency
Department Visits.’ PLOS ONE vol. 9, no. 5.
Grabowski, D. C. and O’Malley, A. J., 2014. ‘Use Of
Telemedicine Can Reduce Hospitalizations Of
Nursing Home Residents And Generate Savings For
Medicare.’ Health Affairs (Millwood), vol. 33, no. 2,
pp. 244-250.
Moehr, J. R., et al. 2006. ‘Success factors for telehealth —
a case study.’ International Journal
of Medical Informatics, vol. 75, no. 10-11, pp. 755–63.
Murray, E., et al., 2011. ‘Why is it difficult to implement
e-health initiatives? A qualitative study.’
Implementation Science, vol. 6, no. 6.
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
96
