
User Perceptions of the Telemedicine Programme in Nursing Homes
The Singapore Perspective
H. J. Toh
1
, J. Chia
1
, E. Koh
2
, K. Lam
1
, G. C. Magpantay
1
, C. M. De Leon
1
and J. A. Low
3
1
GeriCare@North, AHS Programme Office, Khoo Teck Puat Hospital, Singapore, Singapore
2
Ageing-In-Place, AHS Programme Office, Khoo Teck Puat Hospital, Singapore, Singapore
3
Department of Geriatric Medicine and Palliative Care, Khoo Teck Puat Hospital, Singapore, Singapore
Keywords: Telemedicine, User Satisfaction, Perceptions, Healthcare, Telecommunications Technology, Focus Group
Discussion, Semi-structured Interviews.
Abstract: Geriatric care is a holistic approach to caring for older persons with complex health problems, so as to meet
their long term care needs and maintain their independence for as long as possible. Due to a scarcity of
geriatricians, Telegeriatrics was piloted in December 2010 by an acute hospital in Singapore to improve
access to geriatric specialists for nursing homes. This preliminary study explores the perspectives of users
from the NHs and the acute hospital on two aspects of Telegeriatrics – the telemedicine consultation and the
nurse training programme. Seven focus group discussions and two semi-structured moderate interviews
were conducted with a total of 24 participants. Thematic content analysis was applied to identify
important themes and new themes that emerged during the coding process. The most commonly recognised
benefits were increased access to specialist care, reduced need for hospitalizations, improved quality of care,
and enhanced nursing skills and knowledge. However, the greatest barriers as perceived by the users were
the lack of personal touch, technical issues, and medico-legal issues. The users expressed general
acceptance of Telegeriatrics in providing geriatric care. They were aware of its limitations and challenges,
but also recognized it as a promising way of providing consultation and strengthening nursing skills.
1 INTRODUCTION
Telemedicine, a combination of telecommunications
technology and medicine, is seen as a solution to
delivering healthcare services when distance
becomes a crucial element of consideration
(Armstrong and Haston, 1997; Bashshur et al., 2000;
Clark et al., 2007). In some countries, the ageing
population has resulted in an increase in the
development of telemedicine for older people (Goins
et al., 2001; van den Berg et al., 2012).
Telemedicine can also bridge knowledge and skills
gaps in nursing home (NH) care by introducing
continuous nurse training and education. As a result
of Singapore’s rapidly ageing population and severe
bed crunch (Cheah and Heng, 2001; Ong et al.,
2014), ‘remote’ medicine could be the key to
improving outcomes for the elderly without
requiring emergency department (ED) use (Shah et
al., 2007; Trief et al. 2007). Telemedicine
consultations that provide timely specialist access to
the NHs can be instrumental in detecting and
treating symptoms early, thereby enabling NH
residents to be managed in the NHs and preventing
unnecessary transfers to the acute hospitals (Ellis et
al., 2001; McLean et al., 2012; Grabowski and
O’Malley, 2014). Furthermore, telemedicine
provides NH nurses with additional training and
educational opportunities (Janet et al., 2011).
Increased access to knowledge, enhanced
understanding of medical conditions and improved
decision making capacity can improve the quality of
care and decrease transfers to the acute hospital.
Telegeriatrics is an on-going programme that
was started in December 2010 by an acute hospital
in Singapore. It is targeted at providing geriatric
specialist services for the elderly in three partnering
NHs. Prior to the programme, the NHs had limited
access to specialist care. There was heavy reliance
on nursing care and physical visits by general
practitioners. Limited by an inadequate supply of
geriatricians, video-conferencing between the patient
and the geriatrician enables the provision of timely
and accessible care, while reducing
97
Toh H., Chia J., Koh E., Lam K., Magpantay G., De Leon C. and Low J..
User Perceptions of the Telemedicine Programme in Nursing Homes - The Singapore Perspective.
DOI: 10.5220/0005436900970105
In Proceedings of the 1st International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AgeingWell-
2015), pages 97-105
ISBN: 978-989-758-102-1
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

unnecessary travel and associated costs.
One main aspect of the programme was for NH
residents to receive real-time telemedicine
consultation with a geriatrician. A high-resolution
camera and high-definition video monitor were
installed in the acute hospital and the NHs. The
mobile videoconferencing unit ensures that
telemedicine consultations can be held at either the
consultation room or the resident’s room.
Before consultation, the nurse refers residents
requiring specialist care for consultation. In a typical
telemedicine consultation, a nurse from the NH
describes the presenting symptom(s) or problem(s),
while the geriatrician identifies the nature of the
problem and prescribes the appropriate treatment.
The consultation is documented in a form. This form
is used to document elements of the resident’s visit
such as the name of consulting doctor, any
assessments completed by the nurse and any
information received from other healthcare facilities.
After consultation, the form is emailed to the NH for
the nurses to follow up with the management plan.
Both the nurse and geriatrician play important roles
in representing the effectiveness of telemedicine to
provide care as this could influence user perceptions
to a certain extent.
Another arm of the programme was continuous
education and training for the NH nurses, who are
the main carers of NH residents. Before
telemedicine consultations can be facilitated by the
geriatrician and the nurse, selected staff and enrolled
nurses from the NHs need to undergo training. The
aim of the 9-month Telegeriatrics Nurse Training
Course (TNTC) is to equip these nurses with a
specific set of knowledge and skills targeted at
managing NH residents. The nurses were also taught
how to perform simple assessments and physical
examinations to enable them to assist the
geriatricians during telemedicine consultations. In
order to ensure coordinated and integrated care,
multi-disciplinary meetings and mortality audits
were also held via videoconferencing.
The acute hospital’s administrators were the
indirect users of Telegeriatrics as they provided the
on-going support for the programme’s operations. In
particular, they manage matters such as
administrative support, partnering NHs’ feedback,
and process improvements.
In several studies, effectiveness of telemedicine
in providing care has been explored using user
satisfaction as the main outcome, and these users
have reported high levels of acceptability and
willingness to adopt this technology into their
practices (Linassi and Li, 2005; Mair and Whitten,
2000; Yip et al., 2003). However, to date, emphasis
is placed solely on how useful the telemedicine
consultation is, over general satisfaction with the
intervention that is required for knowledge
development and quality improvement in the area of
telemedicine (Demiris et al., 2004; Whitten et al.,
2005). In addition, user readiness in integrating
telemedicine into both clinical practice and
continuous nursing education has not been assessed
in a Singapore context.
This study was designed with the aim of
examining user perceptions and experience of the
telemedicine system as well as the influence of
education on the NH nurses in Singapore. By
reporting on the users’ experiences of Telegeriatrics,
it is hoped that the hospital’s administrators can
develop targeted improvement measures to address
gaps identified in the Telegeriatrics’ training
curriculum, processes and resources.
2 METHODS
2.1 Ethics Approval
Ethics approval was obtained from the National
Healthcare Group Domain Specific Review Board
(DSRB).
2.2 Setting and Recruitment
Three existing NH partners of the acute hospital’s
Telegeriatrics programme were recruited for this
study.
An interview guide was developed to elicit
responses on the impact of Telegeriatrics on the
quality of resident care, cost-effectiveness, user’s
ability to express clearly in a virtual visit, ease of
equipment use, challenges, sense of intimacy, and
potential for long-term use.
Staff who have used the videoconferencing
system for consultations, multidisciplinary meetings
and mortality audits, were recruited. All the nurses
who were included in this study had completed
TNTC.
To grasp a more holistic, integrated view of the
Telegeriatrics experience, both direct and indirect
users were recruited for this study:
i. Nurses of each NH
ii. Nurse managers of each NH
iii. Geriatricians of the acute hospital
iv. Administrators of the acute hospital
The initial plan for this study was to conduct
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
98

only focus group discussions (FGDs) with the users.
However, during the plan’s execution, we conducted
two semi-structured interviews in addition to the
FGDs. For one of the NHs, only one nurse manager
was involved in Telegeriatrics and hence was
scheduled for a semi-structured interview. For one
NH, a nurse who was not available on the day of the
FGD was scheduled for a semi-structured interview.
The FGDs with the geriatricians and the
hospital’s administrators were held at the acute
hospital while those with the nursing staff and nurse
managers were conducted at the three respective
NHs.
2.3 Procedures
Seven FGDs and two semi-structured interviews
were conducted between February 2014 and July
2014.
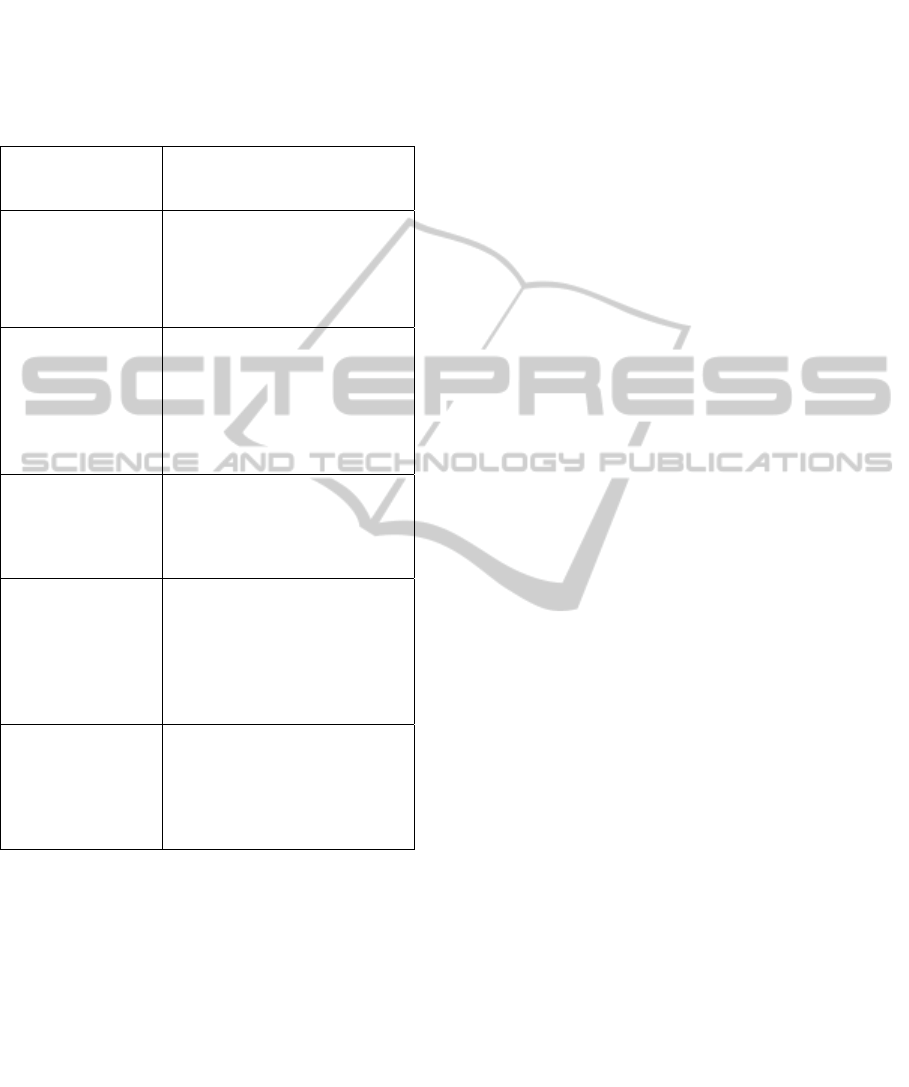
Table 1: Composition of FGDs and semi-structured
interviews.
Composition
Participants,
N = 24
n
FGDs
NH1’s staff and enrolled nurses
NH2’s staff and enrolled nurses
NH3’s staff nurses
NH1’s nurse managers
NH2’s nurse managers
Hospital’s geriatricians
Hospital’s administrators
Semi-structured interviews
NH2’s enrolled nurse
NH3’s nurse manager
5
3
5
2
2
2
3
1
1
Each FGD and semi-structured interview lasted
approximately 1 hour and 30 minutes respectively.
The FGDs and the individual semi-structured
interviews were conducted face-to-face by the first
author. Prior to the FGDs and semi-structured
interviews, the moderator briefed the participants on
the purpose of the study, the expected duration of
the session, and their responsibility as a participant
in the session. They were also given sufficient time
to ask questions, and signed a standardized informed
consent form specifying the benefits and risks of the
study. An interview guide which consisted of
structured, open-ended questions was used to
encourage the participants to express their unique
perspectives of the programme. Field notes were
taken during the sessions which allowed for
triangulation of data (Burns and Grove, 2001).
2.4 Data Analysis
Responses from all the FGDs and semi-structured
interviews were audio recorded and were also
documented in detailed, word-for-word transcripts
by the first author. This study used an explorative
and descriptive design, in which qualitative content
analysis (Hsieh and Shannon, 2005)
was used to
search for contexts, meanings, interpretations, and
consequences.
Both inductive and deductive approaches were
employed in the process of the categorization. The
main categories were formed mainly based on the
concepts derived from literature reviews (Dansky et
al., 1999; Greater Southern Area Health Service,
2009).
The Miles and Huberman (1994) framework was
used for management of the data. The transcripts
were first read in detail to obtain a general view of
the main categories. They were then reviewed and
coded where supplementary notes on the ideas that
emerged were made, to form the main categories.
The main categories were presented in a table in
Microsoft Excel to allow for further thematic
description, and combination of main categories and
sub-categories to emerge as themes and sub-themes.
Supporting comments explain these themes in the
participants’ own words. Identification of links and
patterns between themes and sub-themes resulted.
3 RESULTS
The study group primarily comprised of females,
who are mainly nurses (Table 2). 79% of the users
were from the NHs, and hence the NH users’
perceptions are more representative of the interview
responses. All participants had no prior
experience with facilitating consultations via the
Table 2: Characteristics of focus group and semi-
structured interviews participants.
Characteristics
Participants,
N = 24
n (%)
Gender
Female
17 (71)
Designation
Administrator
Geriatrician
Nurse Manager
Senior Staff Nurse
Staff Nurse
Enrolled Nurse
3 (13)
2 (8)
5 (21)
1 (4)
9 (38)
4 (17)
UserPerceptionsoftheTelemedicineProgrammeinNursingHomes-TheSingaporePerspective
99
video-conferencing system.
The five themes that emerged from the FGDs
and semi-structured interviews were: (1)
Accessibility; (2) Continuity of care; (3) Impact on
nursing; (4) Technology; and (5) Ethics.
Table 3: Themes and sub-themes that emerged from FGDs
and semi-structured interviews.
Themes
Sub Themes
Accessibility
(i) Increased access to
specialist care
(ii) Reduced waiting and
travelling time
Continuity of care
(i) Reduced need for hospital
admissions
(ii) Dying & quality of death
(iii) Joint decision making
(iv) Inadequacies of NHs
Impact on nursing
(i) Positive effects on nurses
(ii) Increased expectations
(iii) Negative impacts
Technology
(i) Receptiveness of
residents’
(ii) Technical issues
(iii) Decreased social presence
(iv) Personal touch
Ethics
(i) Distrust in nurses
(ii) Medico-legal issues
(iii) Risk of confidentiality
breach
3.1 Accessibility
NH residents could reap the benefits from prompt
specialist attention, especially from ad-hoc
consultations. This allowed for the prevention and
treatment of complications so to prevent
emergencies and hospitalizations.
“Through telemedicine, we can start treatment
straight away so [that] patients can get better…
Secondly, if residents are not well, then doctor will
advise sending [residents] to hospital straight away,
so you administer treatment early… They also stay
in hospital [for a] shorter time.” (Nurse Manager)
The frequency of visits to the specialist clinics
was also reduced, as residents may not require
additional specialist medical advice after
telemedicine consultations. Other cited benefits were
related to the reduction of costs including travel
expenses for specialists and hospital transfers; and
reduction in stress levels associated with transferring
of residents.
“Reduces doctor’s travelling. Reduces the need
to travel to a site, and the time involved is money.”
(Geriatrician)
3.2 Continuity of Care
Increased specialist access has resulted in managing
residents on-site, therefore avoiding a trip to the ED
and/or a hospital admission.
“In [the] case they (the residents) are sick, we
just can call the hospital for a tele-consultation...
Our admission rates are lesser now...” (Staff
Nurse)
The use of telemedicine presents an opportunity
for the residents to achieve better quality of death, as
end-of-life care preferences were discussed during
telemedicine consultations. The NH nurses could
then tailor their care according to these preferences.
“They (the residents) want to die in a place
where they are familiar with, with the familiar
surroundings and people around them.” (Nurse
Manager)
Coordination of care through multidisciplinary
meetings to address complex problems assured
consistency in delivering holistic, better quality
clinical care.
“I think it’s very beneficial, because how can
you get al.l the professionals together just for one
case? That will be time-consuming. I think
sometimes we have to maximize the use of
technology.” (Nurse Manager)
A limiting factor of continuing care in the NH
was the inadequacy of resources in the NHs. This
resulted in referrals to ED, even though the
geriatrician and the nurse could coordinate resident
care and manage conditions in the NH.
“Nursing homes have no access to equipment
like [one with] diagnostic capability, for example, so
to manage the patient better… Consultation alone is
only one aspect.” (Nurse Manager)
3.3 Impact on Nursing
Nurses felt a deep sense of commitment and
dedication in caring for their residents. They were
proud of their expanded role and appreciated that the
TNTC has equipped them with confidence,
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
100

knowledge, and skills. After the course, they could
detect signs and symptoms early, as well as perform
physical examinations. The course has also helped
them to better identify and escalate changes in
residents’ medical conditions to the nurse manager
or doctor.
“It [the TNTC] makes us, all of us, more
confident, more systematic in doing assessment and
delivering system of care toward the patient.” (Staff
Nurse)
A number of users felt that with Telegeriatrics in
place, nurses must play a more active role. For
example, nurses must be able to distinguish medical
conditions that require specialist care from the
others, present and document accurately residents’
case history, and manage more diverse conditions in
the NHs.
“The tool (consultation via videoconferencing to
provide care) actually forces the nurses to step up
because you are trying to limit the amount of
doctoring that is occurring in the nursing homes.”
(Hospital’s Administrator)
Language differences were one of the barriers to
effective communication during telemedicine,
affecting the quality of consultations. Language
barriers were significant, particularly between
foreign nurses and the local doctors.
“I still have some problems hearing the nurses
properly, especially the foreign ones…”
(Geriatrician)
Another negative impact of telemedicine was the
lack of comfort and unfamiliarity with technology
when the telemedicine consultations were first
implemented in the NHs.
“They (the nurses) were not comfortable, having
to tell the case [is] like talking to a wall.” (Nurse
Manager)
However, over time, the nurse managers
observed an improvement in the nurses’ confidence
and competency in communication skills, and ability
to facilitate consultations independently.
“They are more confident and their flair for the
case presentation is much better than initially. Now
they even own the whole consultation without my
involvement most of the time.” (Nurse Manager)
3.4 Technology
The nurses expressed concerns about the residents’
ability to readily adopt telemedicine as a form of
technology-enabled care. A nurse described how the
residents exhibited initial unfamiliarity during
consultations.
“Sometimes we need to repeat [our
explanations] to the residents, because residents
didn’t know where to focus on. They didn’t know
about telemedicine, but they knew the doctor is with
them… Sometimes they didn’t know that he (the
doctor) is talking to them.” (Nurse Manager)
However, the residents were observed to adapt
well to the new technology. They were receptive
towards the experience and felt assured by the
geriatrician’s words. A nurse manager described the
residents’ experience as mainly positive:
“They actually acknowledge [the doctors] and
they are quite happy and will wave at the doctors
and they follow the instructions from the doctors.”
(Nurse Manager)
The most frequently identified challenge was the,
sometimes, unfriendly medium of technology.
Delays or problems with transmissions, and visual
and audio quality have reportedly hindered flow of
information delivery, lengthened consultation
duration and made the experience a dissatisfying
one.
“The reception is so poor that we have to stop
because it doesn’t help us at all. If we are going to
have this type of reception, I say, it doesn’t serve
any purpose. We can’t hear what is going on, we
can’t see [too], so it’s not useful for us.” (Nurse
Manager)
Decreased social presence was also another
barrier to using telemedicine. Social presence is the
social degree of person-to-person awareness, which
occurs in a mediated environment (Tachakra and
Rajani, 2002). A common example quoted by the
users was the tendency to assume that the user at the
remote end could not hear them and in response,
they spoke louder over the system.
“I have a habit of speaking very loudly during
telemedicine. Actually they (the hospital’s
administrators) say I don’t have to talk so loudly but
then naturally, I tend to speak louder than usual.”
(Geriatrician)
The geriatrician’s physical presence was
perceived by some as primacy as it serves as a form
of emotional support for the residents. Digital
interaction was reported to be “different” from a
physical consultation.
“There’s this article about this ritual of
examining the patient; it means a lot to patients. It’s
not necessary to listen to the lungs; you still have to
put the stethoscope there.” (Geriatrician)
However, they expressed understanding that
although telemedicine can never replace personal
touch, a key solution will be continued medical
oversight. Physical visit as a follow-up to a
telemedicine consultation was suggested to provide
UserPerceptionsoftheTelemedicineProgrammeinNursingHomes-TheSingaporePerspective
101

the right balance, asserting that the traditional
method of face-to-face consultation should never be
relinquished.
“You still need physical visits interspersed with
the tele-consultation. This is to supplement the
completeness, where you have one physical
examination of this patient regularly…”
(Geriatrician)
3.5 Ethics
The main ethical concern is related to trust issues
between doctors and the nurses during the
telemedicine consultations. Lack of trust by doctors
in the nurse’s ability to perform accurate physical
examinations exists and this could possibly
compromise the quality of resident care.
“There will come a time where we are so good
that we don’t have a clinical educator here, so the
doctor there will have to really take us seriously,
and whether he is going to trust that info given to
him, really that decision he has to decide…” (Nurse
Manager)
The other potential risk associated with
technology-enabled care includes potential liabilities
of the health professional. With medical tele-
diagnosis, medical liability is the main risk.
Insecurities were expressed regarding this grey area:
“For some conditions, it’s just not safe enough
to just have telemedicine. You need to see the patient
and examine the patient...” (Geriatrician)
4 DISCUSSION
There was a general positive response to this new
way of accessing geriatric care. According to the
users, the programme reduced the need for
unnecessary travel and provided timely diagnosis
and treatment. The users identified with the benefits
of using telemedicine to manage residents
and improve adherence to care plans and clinical
outcomes, thereby avoiding hospital transfers.
The nurse managers and nurses felt the benefits
brought about by TNTC. TNTC taught the nurses to
improve on their existing skill set and to apply it not
only in telemedicine consultations, but also in their
routine nursing practices. The nurse managers
particularly expressed that the education aspect of
the programme, including multidisciplinary
meetings, was useful, as care for the residents was
coordinated among health care professionals.
According to a study by Gagnon et al. (2010),
telemedicine applications can facilitate
communication among health care professionals,
and lead to a more coordinated and effective
management. Also, mortality audits have helped the
nurse managers and nurses recognize factors that
contribute to the immediate and underlying cause of
death. They could address suboptimal care practices,
and take steps to prevent such factors that could lead
to similar deaths in the future. Such audits if
conducted consistently have the potential to decrease
morbidity and mortality, leading to standardized and
improved care (Pattinson et al., 2009). Telegeriatrics
has empowered the NHs to conduct after-death
reviews, which have recently been introduced by
Ministry of Health as a criterion for the enhanced set
of nursing home licensing standards (Siau, 2014).
In addition, the nurse managers reported the
success of Telegeriatrics in empowering nurses, and
were keen to continue providing support needed to
sustain the programme. The successful incorporation
of telemedicine was reported to be mainly
contributed by a supportive management that sees
the need for its use (Moehr et al., 2006; Murray et
al., 2011).
The nurses reported that their roles have
expanded from the traditional nursing care. Prior to
the programme, nurses were not required to present
cases to geriatricians during their physical visits.
Furthermore, they did not perform any physical
examinations on the residents. During the
programme, increased expectations were placed on
the nurses in providing resident care. Nurses were
expected to carry out specific roles in the assessment
and management of patients with specific
conditions. Nurses were also expected to bring forth
their suggestions in the management of the resident.
On top of this, they had to learn how to operate the
videoconferencing equipment.
Despite increased expectations, nurses expressed
that they have acquired more knowledge and
confidence in coordinating care. They were proud of
being entrusted with this expanded role. Although
there was initial resistance in facilitating the
telemedicine consultations and frustrations with the
technological disruptions, the nurses accepted these
challenges. They added that this new way of
delivering care has been integrated into their day-to-
day nursing practice. Nurses’ attitudes toward
telemedicine are the key determinant to the
successful implementation of a technology-related
programme (Gamm et al., 1998). Therefore, it is
important to ensure that nurses are prepared to
accept new operational changes, which will not only
alter current medical practice but also attitudes
towards a programme that involves technology. In
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
102

addition, training and the presence of a support
system assist the adoption and use of a new
technology (Ash et al., 2003).
The geriatricians felt that it was plausible to use
telemedicine consultations to manage some
conditions on-site. However, they appeared to be
more reserved in their acceptance of the programme.
They found that the care provided over telemedicine
was less satisfactory than traditional encounters’, as
they faced difficulties in building therapeutic
relationships with the residents. Similarly,
complications in clinician–patient relationships
created by communication technology were
observed in other studies (Weiner and Biondich,
2006). In relation to this, they and the hospital’s
administrators suggested that the telemedicine
consultation should be a form of “relationship
medicine” (Hixon, 2014). Telemedicine encounters
should be remote only when trust between the doctor
and the patient is established.
The geriatricians also articulated that not seeing
the patients in person and their heavy reliance on the
nurses were potential medical risks. These concerns
reflect a sense of insecurity in relying on a medical
system that has been prone to errors (Rowthorn and
Hoffman, 2001; Sao et al., 2012). A study reported
that the doctor took greater care in communicating
with the patient in a telemedicine consultation than
in a face-to-face consultation (Tachakra and Rajani,
2002). In the study, verbal cues were more
frequently used to allow coordination of beliefs
between both parties. Although telemedicine
services have been piloted in a number of clinical
domains, one of the main challenges in adopting
these services includes the lack of clarity over legal
liabilities (Commission Staff Working Paper on
Telemedicine, 2009).
The main limitation of this study is its inability to
assess patient satisfaction as most of the NH
residents were either cognitively impaired,
uncommunicative or both.
Another major limitation of this study is that due
to its exploratory nature, some concepts that were
not mentioned in the FGDs or the semi-structured
interviews were not captured in this study. Further
quantitative analysis can be explored to allow a
clearer understanding of the relationships among
individual factors. In addition, the moderator is a
member of the acute hospital team providing the
telemedicine services. Hence, there is a possibility
that the users may provide responses that the
moderator would like to hear. In order to minimize
this form of bias, an acknowledgement of
participation which clarifies the process and creates
a common expectation among participants was given
before the discussion.
5 CONCLUSIONS
This study offers a better understanding of the ways
in which Telegeriatrics had influenced the users,
including its benefits and drawbacks in providing
geriatric care. It identifies specific issues that can
affect the user perception, and thus, it provides
better guidance on how to proceed with subsequent
quality improvement initiatives in order to ensure
better care for NH residents.
Favourable attitudes towards the programme
have made it possible to coordinate treatment plans
for patients on-site, and to strengthen nurses’
knowledge and skills in providing better nursing
care. Telegeriatrics could be one of the solutions to
compensate for the inadequate supply of
geriatricians in Singapore, and play a part in the
continuity of care between hospital and NHs.
While the nurses and nurse managers appreciate
the programme and acknowledge that NH residents
were better cared for, the geriatricians appeared to
be less convinced. In many studies, the successful
adoption of using telemedicine has been limited by
the doctors’ conservative perceptions (Siwicki,
1997; Coiera, 2003). As adoption of telemedicine
mainly relies on the readiness and attitudes of
healthcare professionals, efforts to actively engage
the geriatricians are necessary for the continued
operations of Telegeriatrics. In order for the
hospital’s administrators to achieve a user-driven
design that will increase usability and acceptance,
these professionals need to closely assess the
geriatricians’ needs and expectations.
The concern with the potential medical risks that
comes along with the use of telemedicine highlights
the need to ensure that professional practice
standards are followed through and ethical standards
upheld. The safety issues associated with
telemedicine are more complicated and include not
only anxiety about operating an equipment, but also
concerns regarding possible adverse effects on
patient management decisions through delayed or
missing information, misunderstood advice, or
inaccurate findings. Further research is needed in the
area of patient safety as it is directly related to
telemedicine practice.
Despite these concerns, the users believed that
using communication technologies to provide health
care is expected, and will be more often in the near
future. The use of telemedicine has the feasibility to
UserPerceptionsoftheTelemedicineProgrammeinNursingHomes-TheSingaporePerspective
103

extend specialist access to more areas of the
community in the north of Singapore. The provision
of continuous nurse education to prepare for
technology use is also viable. As NH nurses play an
integral part in caring for residents throughout the
course of their illness, enhanced nursing knowledge
and skills could lead to higher standards in the
provision of long-term geriatric nursing care.
However, it is emphasized that the use of
telemedicine is a useful alternative to availing expert
opinion, but will never replace traditional care.
ACKNOWLEDGEMENTS
The authors would like to thank all the participants
of this study for their time and insights.
REFERENCES
Armstrong, I. J. and Haston, W. S., 1997. Medical
decision support for remote general practitioners using
telemedicine. Journal of Telemedicine and Telecare,
vol. 3, pp. 27–34.
Bashshur, R. L. et al., 2000. Telemedicine: A new health
care delivery system. Annual Review of Public Health,
vol. 21, pp. 613–37.
Clark, R.A. et al., 2007. Telemonitoring or structured
telephone support programmes for patients with
chronic heart failure; systematic review and meta-
analysis, vol. 334, pp. 942-945.
Goins, R.T. et al., 2001. ‘Telemedicine, rural elderly, and
policy issues.’ Journal of Aging Society Policy, vol.
13, no. 4, pp. 53-71.
van den Berg, N. et al., 2012. Telemedicine and telecare
for older patients--a systematic review. Maturitas, vol.
73, no. 2, pp. 94-114.
Cheah, J and Heng, B. H., 2001. ‘Implementing chronic
disease management in the public healthcare sector in
Singapore: the role of hospitals.’ World Hospitals and
Health Services, vol. 37, no. 3, pp. 19-23, 40-43.
Ong, J., 2014. Singapore Budget 2014: Hospital bed
crunch comes under fire. The Straits Times, Available
from: <http://www.straitstimes.com/>. (12 March
2014).
Shah, M. N., 2007. ‘High-Intensity Telemedicine-
Enhanced Acute Care for Older Adults: An Innovative
Healthcare Delivery Model.’ Journal of American
Geriatrics Society, vol. 61, no. 11, pp. 2000–2007.
Trief, P. M. et al., 2007. ‘Psychosocial Outcomes of
Telemedicine Case Management for Elderly Patients
With Diabetes The randomized IDEATel trial.’
Diabetes Care, vol. 30, no. 5, pp. 1266-268.
Ellis, D.G. et al., 2001. ‘A telemedicine model for
emergency care in a short-term correctional facility.’
Telemedicine journal and e-health, vol. 7, no. 2, pp. 87-92.
McLean, S. et al., 2012. ‘Telehealthcare for chronic
obstructive pulmonary disease. Cochrane Review and
meta-analysis.’ The British Journal of General
Practice, vol. 62, no. 604, pp. 739–749.
Grabowski, D. C. and O’Malley, A. J., 2014. ‘Use Of
Telemedicine Can Reduce Hospitalizations Of
Nursing Home Residents And Generate Savings For
Medicare.’ Health Affairs (Millwood), vol. 33, no. 2,
pp. 244-250.
Janet, L. G., 2011. ‘The Virtual Clinical Practicum: An
Innovative Telehealth Model for Clinical Nursing
Education. Nursing Education Perspectives.’ National
League for Nursing, vol. 32, no. 3, pp. 189-194.
Linassi, A. G. and Li, P. S. R., 2005. ‘User satisfaction
with a telemedicine amputee clinic in Saskatchewan.’
Journal of Telemedicine and Telecare, vol. 11, no. 8,
pp. 414-418.
Mair, F
and Whitten, P., 2000. ‘Systematic review of
studies of patient satisfaction with telemedicine.’ BMJ,
vol. 320, no. 7248, pp. 1517-520.
Yip, M. P. et al., 2003. ‘Development of the Telemedicine
Satisfaction Questionnaire to evaluate patient
satisfaction with telemedicine: a preliminary study.’
Journal of Telemedicine and Telecare, vol. 9, no. 1,
pp. 46-50.
Demiris, G. et al., 2004. ‘Assessment of Patients’
Acceptance of and Satisfaction.’ Journal of Medical
Systems, vol. 28, no. 6, pp. 575-579.
Whitten, P. and Love, B., 2005. ‘Patient and provider
satisfaction with the use of telemedicine: Overview
and rationale for cautious euthusiasm.’ Journal of
Postgraduate Medicine, vol. 51, pp. 294-300.
Burns, N. and Grove, S. K., 2001. The practice of nursing
research: Conduct, critique, and utilization (4th ed.).
Philadelphia: W. B. Saunders.
Hsieh, H. F. and Shannon, S. E., 2005. ‘Three Approaches
to Qualitative Content Analysis.’ Qualitative Health
Research vol. 15, no. 9, pp. 1277-288.
Dansky, K. H. et al., 1999. ‘Nurses’ Responses to
Telemedicine in Home Healthcare.’ Journal
of Healthcare Information Management, vol. 13, no.
4.
Greater Southern Area Health Service (GSAHS), 2009.
User satisfaction and experience with a telemedicine
service for diabetic foot disease in an Australian rural
community, Devine Research Report. Available from:
Greater Southern Area Health Service. (December
2009).
Miles, M. B. and Huberman, A. M., 1994. Qualitative
data analysis: An expanded source book. Thousand
Oaks, CA: Sage Publications.
Tachakra, S. and Rajani, R., 2002. ‘Social presence in
telemedicine.’ Journal of Telemedicine and Telecare,
vol. 8, no. 4, pp. 226-230.
Gagnon, M-P. et al., 2010. ‘Systematic Review of Factors
Influencing the Adoption of Information and
Communication Technologies by Healthcare
Professionals.’ Journal of Medical Systems, vol. 36,
no. 1, pp. 241–277.
Pattinson, R. et al., 2009. ‘Perinatal mortality audit:
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
104

Counting, accountability, and overcoming challenges
in scaling up in low- and middle-income countries.’
International Journal of Gynecology & Obstetrics,
vol. 107, no. 1, pp. 113-121, 121-122.
Siau, M. E., 2014. MOH unveils new standards for
nursing homes. Available from:
<http://www.todayonline.com/singapore/moh-unveil-
new-standards-nursing-home>. (9 January 2014).
Moehr, J. R. et al., 2006. ‘Success factors for telehealth—
a case study.’ International Journal of Medical
Informatics, vol. 75, no. 10-11, pp. 755–763.
Murray E, et al., 2011. ‘Why is it difficult to implement e-
health initiatives? A qualitative study.’
Implementation Science, vol. 6, no. 6.
Gamm, L. et al., 1998. ‘Investigating Changes in End-
User Satisfaction with an Electronic Medical Record
in Ambulatory Care Settings.’ Journal of Healthcare
Information Management, vol. 12, no. 4, pp. 53–65.
Ash, J.S. et al.., 2003. ‘A consensus Statement on
Considerations for a Successful CPOE
Implementation.’ Journal of the American Medical
Informatics Association, vol. 10, no. 3, pp. 229-234.
Weiner, M., and Biondich, P., 2006. ‘The Influence of
Information Technology on Patient-Physician
Relationships.’ The Journal of General Internal
Medicine, vol. 21, no. 1, pp. 35–39.
Hixon, T., 2014. Why is Telemedicine suddenly hot?
Available from: <http://www.forbes.com/sites/
toddhixon/2014/10/22/why-is-telemedicine-suddenly-
hot/>. (22 October 2014).
Rowthorn, V. and Hoffmann, D., 2001. ‘Legal
Impediments to the diffusion of telemedicine.’ Journal
of Health Care Law and Policy, vol.14, pp.1–54.
Sao, D. et al., 2012. Chapter 20: Legal and Regulatory
Barriers to Telemedicine in the United States: Public
and Private Approaches toward Health Care Reform.
In: Cohen I.G., editor. The Globalization of Health
Care: Legal and Ethical Issues. (I.Glenn Cohen ed.,
Oxford University Press 2013). Available from:
<http://ssrn.com/abstract=2176764>.
Commission Staff Working Paper on Telemedicine. 2009.
Available from: <http://ec.europa.eu/information_
society/activities/health/docs/policy/telemedicine/tele
medecineswp_sec-2009-943.pdf>
Siwicki, B., 1997. ‘Telemedicine. Providing Proof to
Payers.’ Health Data Management, vol. 5, no. 7, pp.
56-58.
Coiera, E., 2003. The guide to health informatics. Madison
Avenue, New York: Oxford University Press.
UserPerceptionsoftheTelemedicineProgrammeinNursingHomes-TheSingaporePerspective
105
