
ICT Solutions to Develop an Effective Motor and Cognitive Training
to Reduce Risk of Falls
The I-DONT-FALL Project
Francesco Barban
1
, Roberta Annicchiarico
1
, Alessia Federici
1
, Ilenia Debora Mazzù
1
,
Maria Giovanna Lombardi
1
, Simone Giuli
1
, Claudia Ricci
1
, Fulvia Adriano
1
, Ivo Griffini
1
,
Manuel Silvestri
1
, Massimo Chiusso
1
, Sergio Neglia
2
, Raquel Cuevas Perez
3
, Yannis Dionyssiotis
4
,
Georgios Koumanakos
5
, Milo Kovačeić
6
, Nuria Montero
7
, Oscar Pino
8
, Carmela Zincarelli
9
,
Niels Boye
10
, Cristian Barrué
11
, Peter Levene
12
, Stelios Pantelopoulos
13
, Roberto Rosso
14
,
Angelo Maria Sabatini
15
and Carlo Caltagirone
1,16
1
Clinical and Behavioral Neurology Laboratory, IRCCS Fondazione Santa Lucia, Rome, Italy
2
Engineering Ingegneria Informatica SpA, Rome, Italy
3
Hospital General de Granollers, Barcelona, Spain
4
Social Policy Center, Municipality of Kifissia, Greece
5
Frontida Zois Home Care Agency, Patras, Greece
6
Municipality of Stari Grad, Belgrade, Serbia
7
Hospital General Universitario Gregorio Marañón, Madrid, Spain
8
Benito Menni CASM, Sant Boi de Llobregat-Barcelona, Spain
9
IRCCS Fondazione Salvatore Maugeri, Telese Terme, Italy
10
Klinisk Informatik, Aarhus, Denmark
11
Knowledge Engineering & Machine Learning Group Computer Software Department,
Universitat Politècnica de Catalunya-Barcelona, Barcelona, Spain
12
Docobo Ltd, Bookham, Surrey, U.K.
13
Singular Logic, Athens, Greece
14
Tesan SpA, Vicenza, Italy
15
The BioRobotics Institute, Scuola Superiore Sant’Anna, Pontedera, Italy
16
Systems Medicine Department, University of Rome “Tor Vergata”, Rome, Italy
Keywords: ICT, Risk of Falls, Training, RCT.
Abstract: This study shows preliminary results of the multicenter and international I-DONT-FALL (IDF) project, co-
funded by the European Union, aiming to offer an integrated Information and Communication Technologies
(ICT) solution for fall prevention and detection. Here we assessed the efficacy of a motor and a cognitive
treatment delivered through the IDF ICT solution, aiming to reduce the risk of falls through a randomized
controlled trial. The outcome was measured with the Falls Efficacy Scale-International (FES-I) and the
subscales of the Tinetti Performance Oriented Mobility Assessment for balance (POMA-B) and gait
(POMA-G). We compared the effect of a 24-sessions period of motor training delivered through an i-
Walker vs. a comparable period of non-motor training in terms of frequency and duration of sessions. The
same comparison was performed for a period of cognitive training delivered though a touch-screen
computer interface vs. a comparable period of non-cognitive training in terms of frequency and duration of
sessions. Results showed that motor treatment alone or mixed with cognitive training reduces significantly
the fear of falling and the risk of falls. Both cognitive and motor treatments showed a nonspecific positive
effect on balance performance of participants. These preliminary results are consistent with previous
evidences.
259
Barban F., Annicchiarico R., Federici A., Mazzù I., Lombardi M., Giuli S., Ricci C., Adriano F., Griffini I., Silvestri M., Chiusso M., Neglia S., Cuevas
Perez R., Dionyssiotis Y., Koumanakos G., Kova
ˇ
cei
´
c M., Montero N., Pino O., Zincarelli C., Boye N., Barrué C., Levene P., Pantelopoulos S., Rosso R.,
Sabatini A. and Caltagirone C..
ICT Solutions to Develop an Effective Motor and Cognitive Training to Reduce Risk of Falls - The I-DONT-FALL Project.
DOI: 10.5220/0005490802590263
In Proceedings of the 1st International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AgeingWell-
2015), pages 259-263
ISBN: 978-989-758-102-1
Copyright
c
2015 SCITEPRESS (Science and Technology Publications, Lda.)

1 INTRODUCTION
It is estimated that about a third of community-
dwelling people over 65 years old fall each year
(Gillespie et al., 2012). Falls can have serious
physical consequences such as fractures and head
injuries (Peel et al., 2002) and psychological
consequences as well, particularly fear of falling and
loss of self-confidence, thus resulting in a restriction
in physical functions and social interactions
(Yardley et al., 2002). Moreover, as reported from
Peel and colleagues (2002), the rate of fall-related
injuries increases with age.
Among the several different definitions of fall, a
consensus definition has been suggested by Lamb
(2005). According to the author, fall should be
defined as ‘an unexpected event in which the
participants come to rest on the ground, floor, or
lower level’. The difficulty to formulate a consensus
definition of fall possibly derives from the
complexity of evaluating the risk factors for falls.
Indeed, risk factors are various and a few
comprehensive syntheses of them have been
provided (Campbell and Robertson, 2006; Deandrea,
2010). Particularly, it seems that only 15% of falls
have a single identifiable cause (e.g., syncopal falls
with cardiac pacing or falls related to neurological
disease; Campbell and Robertson, 2006) and a
similar percentage of falls results from an external
event that would cause falling, especially in younger
and intellectually able people (Campbell et al.,
1989). Interestingly, over 60% of falls result not just
from the additive effects of multiple pathologies but
from multiple interacting aetiological factors
(Fairweather and Campbell, 1991; Campbell and
Robertson, 2006). Research on risk factors for falls
has received an increasing attention as the evaluation
and detection of these are a keypoint to develop
effective intervention programs aimed to prevent
falls (Gillespie et al., 2012). Indeed, over the last 10
years, several attempts using Information and
Communication Technologies (ICT) aimed at falls
prevention and detection (Hawley-Hague et al.,
2014). Some of these studies delivered ICT-based
motor trainings for falls prevention and suggest
positive messages about the benefits.
Several studies investigated the possible link
between cognition and gait (Verlinden et al., 2014)
and its implication in falls (Amboni et al., 2013).
Indeed, gait is a complex motor behavior and
presents many different measurable facets besides
proper motor facets (e.g., velocity), such as an
important relationship to different aspects of
cognition (Holtzer et al., 2006). Particularly, pace
seems to be associated with attention and executive
functions and with general cognitive decline and
incident dementia as well (Verghese et al., 2007),
whereas rhythm seems to be associated to
information processing speed (Verlinden et al.,
2014). As suggested by Shumway-Cook and
Woollacott (2000), indeed, attentional demands for
postural control increase with aging whereas sensory
information decreases. Moreover, the declines in the
ability to allocate attention to postural control under
multi-task conditions might furtherly contribute to
increase the risk of falls.
Therefore, the development of effective
prevention programs should take into account not
only motor factors but also cognitive factors.
Particularly, it is agreeable that training programs
aimed to prevent risk of falls and to reduce number
of falls should be focused also on cognitive domains
such as attentional-executive functions, thus
providing effective results on motor behavior and
particularly in pace and rhythm of gait.
The findings that we report in this paper are
partial results of the I-DONT-FALL project which is
a multicenter and international project co-funded by
the European Union. This project aims to offer an
integrated system for fall management solution, both
in prevention and detection strategies. Moreover, the
project aims to assess the efficacy of a motor and of
a cognitive intervention and their combination to
reduce the risk of falls through an European
multicenter randomized controlled trial (RCT). The
assessment of treatment effects combined standard
scales and ICT assessment tools such as WIMU
(Mannini and Sabatini, 2014) and i-Walker (Cortés
et al., 2008).
The main aim of the present study was to assess
the differential effect of motor training and of a
cognitive training on risk of falls measured with the
Falls Efficacy Scale-International (FES-I) (Yardley
et al., 2005) and the subscales of the Tinetti
Performance Oriented Mobility Assessment for
balance (POMA-B) and gait (POMA-G) (Tinetti,
1986). Therefore, we compared the effect of a 24 –
sessions (twice-a-week) period of motor training vs.
a comparable period of non-motor training in terms
of frequency and duration of sessions. The same
comparison was performed for a period of cognitive
training vs. a comparable period of non-cognitive
training in terms of frequency and duration of
sessions.
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
260

2 METHODS
2.1 Subjects
The results reported in this paper come from the first
subset of 49 participants enrolled in the RCT study
of I-DONT-FALL project that completed the
assessment at T0 (pre-training) and T1 (post-
training). All participants were elderly (mean age 79
years, range 65-96 years), with formal education
(mean years 8.8, range 5-18), with high risk of falls
(POMA total score ≤ 20 and/or at least one previous
fall in the last year – mean score 19, range 10-28;
mean number of previous falls 1.2, range 0-9) and
without or with only a mild cognitive deficit (mean
MMSE 26.3, range 20-30). Moreover, they were free
of major behavioural disturbances and not receiving
any rehabilitative treatment. All participants gave
their written informed consent approved by local
ethics committees.
All participants were randomly enrolled in four
different kinds of training: a motor training, a
cognitive training, a mixed motor and cognitive
training and a placebo activity. The randomization
was double and stratified for pilot site: a first
randomization was done between cognitive
intervention or not. After that, a second
randomization was done between the motor
intervention or not. In this way, those receiving the
cognitive training might receive it mixed with the
motor (i.e., mixed training) or not (i.e., cognitive
training alone), whereas those not receiving the
cognitive treatment might receive the motor (i.e.,
motor training alone) or not (i.e., placebo). This
resulted in the four after mentioned conditions (see
figure 1). This kind of randomization was adopted to
balance the factors that were tested during the
analysis, i.e., cognitive (group A) vs. non-cognitive
(group B) and motor (group C) vs. non-motor (group
D).
2.2 Training and Placebo Activities
Each kind of training (cognitive, motor, mixed) and
placebo activity were executed through 2 sessions
per week for 12 weeks (24 sessions). Each session
lasted 1 hour for a total of 24 hours training. Motor
training was administered with an i-Walker (Cortés
et al., 2008) designed to help and support a user with
some mobility impairment. Specifically, it provides
assistance to compensate unbalanced muscle force
and lack of muscle force on climbs and descendents.
Motor training consisted in a set of warm-up
procedures followed by exercises dedicated for 1/2
of the session to balance and for 1/2 of the session to
gait. Cognitive training sessions consisted of a set of
exercises covering all the cognitive functions and it
was supported by surface computing (touchscreen-
enabled) equipment. Touchscreen computers could
be either large-format screens that could be used on
tables or standard PCs with touchscreen monitors.
Cognitive exercises were dedicated for the 2/3 of the
whole session to executive functions and attention
exercises and for 1/3 to other cognitive functions
(i.e., declarative memory, orientation, language,
constructional praxis, abstract reasoning). Executive
functions training consisted in exercises practicing
abstraction and planning such as sorting cards and
grouping them according with a covered criterion or
setting up a menu according with some rules and
working memory exercises. Attention was trained
with exercises of focused attention with distracters
or with exercises of sustained attention. Difficulty
level of exercises was increased according to
participant’s performance. Mixed training consisted
in the combination of 30 minutes of motor exercises
and 30 minutes of cognitive exercises during the
same training session. Placebo activity consisted in
entering data (i.e., words, names, codes) into a file
on the same computer used during the cognitive
training.
2.3 Outcome Measures
The risk of falls was measured with the Falls
Efficacy Scale-International (FES-I) (Yardley et al.,
2005) and the POMA-B and POMA-G subscales
(Tinetti, 1986).
We performed a total of 6 analyses of variance
ANOVA, resulting from each outcome measure (i.e.,
FES-I, POMA-B, POMA-G) by each kind of
treatment (i.e., motor, cognitive ). We used mixed
ANOVA with time (T0 vs. T1) as within factor, and
the kind of treatment, i.e., motor vs. non-motor and
cognitive vs. non-cognitive, as between factor. More
specifically, cognitive treatment was obtained
collapsing data from cognitive and mixed training
(group A) and non-cognitive training was obtained
collapsing data form motor and placebo treatment
Figure 1: Randomization of participants.
ICTSolutionstoDevelopanEffectiveMotorandCognitiveTrainingtoReduceRiskofFalls-TheI-DONT-FALLProject
261
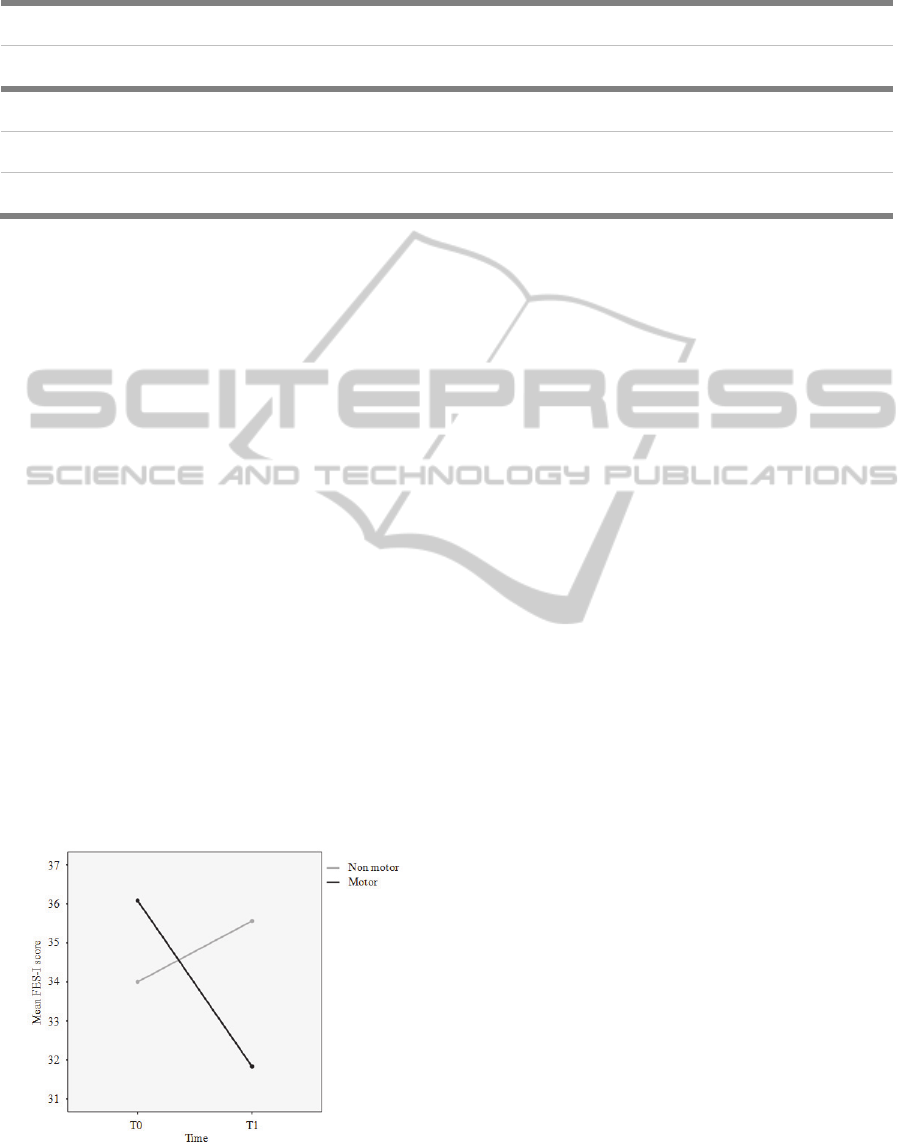
Table 1: Results.
MOTOR/NON MOTOR COGNITIVE/NON COGNITIVE
Scale TIME EFFECT TIME X TREATMENT TIME EFFECT TIME X TREATMENT
Fear of falling scale (FES-I) ns p< 0.012 ns ns
Tinetti Balance (POMA-B) p< 0.043 ns p< 0.047 ns
Tinetti Gait (POMA-G) ns ns ns ns
(Group B). Conversely, motor treatment was
obtained collapsing data from motor and mixed
training (Group C) whereas non-motor was obtained
collapsing data from cognitive and placebo training
(Group D) (Figure 1).
3 RESULTS
3.1 Fear of Falling (FES-I)
We found a significant reduction of the fear of
falling by the motor treatment alone or mixed with
cognitive training (Table 1). This was showed by the
significant interaction between time (T0 vs. T1) and
kind of treatment (motor vs. non-motor) on the FES-
I scores [F(1,47)= 6.772, p< 0.012] (Figure 2). Post-
hoc comparisons with paired t-test showed a
significant effect between T0 and T1 only for the
motor treatment (t(23)= 2.946, p< 0.007) and not for
the non-motor (t(24)= -.921, p< 0.366). The same
interaction between time and cognitive treatment
was not significant [F(1,47)= .751, p< 0.391]. Main
effects of time and group were not significant for
motor and cognitive treatments.
Figure 2: Effect of motor treatment on FES-I mean scores.
3.2 Balance and Gait (POMA-B,
POMA-G)
We found a general nonspecific effect of treatment
on balance. This was showed by a main effect of
time for both motor [F(1,47)= 4.340, p< 0.043] and
cognitive [F(1,47)= 4.158, p< 0.047] treatment on
the POMA-B subscale. Neither significant
interactions nor group effects emerged for both
treatments in both POMA subscales.
4 DISCUSSION
This study aimed at assessing the efficacy in
reducing the risk of falls of an ICT solution
providing a motor and cognitive treatment in a
sample of elderly participants at risk of falls. These
preliminary data showed that motor treatment alone
or mixed with cognitive training reduces
significantly the fear of falling and by consequence
the risk of falls. This was not the case of the
cognitive training focused on attentional-executive
functions when administered alone or mixed with
the motor one. However, both cognitive and motor
treatments showed a nonspecific positive effect on
balance performance of participants. These
preliminary results accord with the previous
published evidence (Huang et al., 2011; Segev-
Jacubovski et al., 2011; van het Reve and de Bruin,
2014) about the effect of the motor training in
combination with behavioral interventions on fear of
falling. To our knowledge, at present this study is
the first attempt to evaluate the reduction of risk of
falls through a cognitive training focused on
attentional-executive functions performed alone or
in association with a motor training. Previous
evidences (Smith-Ray et al., 2013) partially accord
with our results showing a positive effect of
cognitive training in elderly on balance when
compared with a rest period. Our preliminary data
ICT4AgeingWell2015-InternationalConferenceonInformationandCommunicationTechnologiesforAgeingWelland
e-Health
262

show that this effect is not specific of the cognitive
training.
5 CONCLUSIONS
Our preliminary results agree with previous
evidences (Huang et al., 2011; Segev-Jacubovski et
al., 2011; van het Reve and de Bruin, 2014) and are
motivating at pursuing with this study enlarging the
sample in order to better investigate the specific role
of the cognitive training alone or mixed with motor
training in the reduction of the risk of falls.
ACKNOWLEDGEMENTS
This study was co-funded by the EC funded project
I-DONT-FALL “Integrated prevention and
Detection sOlutioNs Tailored to the population and
Risk Factors associated with FALLs” (CIP-ICT-
PSP-2011-5-297225).
REFERENCES
Amboni, M., Barone, P., Hausdorff, J.M., 2013.
Cognitive contributions to gait and falls: evidence and
implications. Mov Disord. Sep 15;28(11):1520-33.
Campbell, A.J., Borrie, M.J., Spears, G.F., 1989. Risk
factors for falls in a community-based prospective
study of people 70 years and older. J Gerontol. 44:
M112–7.
Campbell, A.J., Robertson, M.C., 2006 Implementation of
multifactorial interventions for fall and fracture
prevention. Age Ageing. Sep;35 Suppl 2:ii60-ii64.
Cortés, U., Martínez-Velasco, A., Barrué, C., et al., 2008.
A SHARE-it service to elders’ mobility using the i-
Walker. Gerontechnology.7:95.
Deandrea, S., Lucenteforte, E., Bravi, F., Foschi, R., La,
V.C., Negri, E., 2010. Risk factors for falls in
community-dwelling older people: a systematic review
and meta-analysis. Epidemiology. 21(5):658–68.
Fairweather, D.S., Campbell, A.J., 1991. Diagnostic
accuracy. The effects of multiple aetiology and the
degradation of information in old age. J R Coll
Physicians Lond. 25: 105–10.
Gillespie, L.D., Robertson, M.C., Gillespie, W.J., et al.,
2012. Interventions for preventing falls in older people
living in the community. Cochrane Database Syst Rev.
Sep 12;9:CD007146.
Hawley-Hague, H., Boulton, E., Hall, A., Pfeiffer, K.,
Todd, C., 2014. Older adults' perceptions of
technologies aimed at falls prevention, detection or
monitoring: a systematic review. Int J Med Inform.
Jun;83(6):416-26.
Holtzer, R., Verghese, J., Xue, X., Lipton, R.B., 2006.
Cognitive processes related to gait velocity: results
from the Einstein Aging Study. Neuropsychology.
Mar;20(2):215-23.
Huang, T.T., Yang, L.H., Liu, C.Y., 2011. Reducing the
fear of falling among community-dwelling elderly
adults through cognitive behavioural strategies and
intense Tai Chi exercise: a randomized controlled trial.
J Adv Nurs. May;67(5):961-71.
Lamb, S.E., Jorstad-Stein, E.C., Hauer, K., Becker, C.,
Prevention of Falls Network Europe and Outcomes
Consensus Group, 2005. Development of a common
outcome data set for fall injury prevention trials: the
Prevention of Falls Network Europe consensus. J Am
Geriatr Soc. 53(9):1618–22.
Mannini, A., Sabatini, A.M., 2014. Walking speed
estimation using foot-mounted inertial sensors:
comparing machine learning and strap-down
integration methods. Med Eng Phys. 36(10):1312-21.
Peel, N.M., Kassulke, D.J., McClure, R.J., 2002.
Population based study of hospitalised fall related
injuries in older people. Inj Prev. 8(4):280–3.
Segev-Jacubovski, O., Herman, T., Yogev-Seligmann, G.,
Mirelman, A., Giladi, N., Hausdorff, J.M., 2011. The
interplay between gait, falls and cognition: can
cognitive therapy reduce fall risk? Expert Rev
Neurother. 11(7):1057-1075.
Shumway-Cook, A., Woollacott, M., 2000. Attentional
demands and postural control: the effect of sensory
context. J Gerontol A Biol Sci Med SciJan;55(1):M10-6.
Smith-Ray, R.L., Hughes, S.L., Prohaska, T.R., Little,
D.M., Jurivich, D.A., Hedeker, D., 2013. Impact of
Cognitive Training on Balance and Gait in Older
Adults. J Gerontol B Psychol Sci Soc Sci. Nov 5.
Tinetti, M.E., 1986. Performance-oriented assessment of
mobility problems in elderly patients. J Am Geriatr
Soc. Feb;34(2):119-26.
van het Reve, E., de Bruin, E.D., 2014. Strength-balance
supplemented with computerized cognitive training to
improve dual task gait and divided attention in older
adults: a multicenter randomized-controlled trial. BMC
GeriatrDec 15;14:134.
Verghese, J., Wang, C., Lipton, R.B., Holtzer, R., Xue, X.,
2007. Quantitative gait dysfunction and risk of
cognitive decline and dementia. J Neurol Neurosurg
Psychiatry. Sep;78(9):929-35.
Verlinden, V.J., van der Geest, J.N., Hofman, A., Ikram,
M.A., 2014. Cognition and gait show a distinct pattern
of association in the general population. Alzheimers
Dement. May;10(3):328-35.
Yardley, L., Beyer, N., Hauer, K., Kempen, G., Piot-
Ziegler, C., Todd, C., 2005. Development and initial
validation of the Falls Efficacy Scale-International
(FES-I). Age Ageing. Nov;34(6):614-9.
Yardley, L., Smith, H., 2002. A prospective study of the
relationship between feared consequences of falling
and avoidance of activity in community-living older
people. Gerontologist. 42(1):17–23.
ICTSolutionstoDevelopanEffectiveMotorandCognitiveTrainingtoReduceRiskofFalls-TheI-DONT-FALLProject
263
