
Building а National Clinical Data Warehouse
Ustun Yildiz
1
and Ayse Keles
1,2
1
Agency of Health Informatics, Ankara, Turkey
2
Yildirim Beyazit University, Ankara, Turkey
{ustun.yildiz, ayse.keles}@saglik.gov.tr
Keywords: EHR, Clinical Data Warehouse, Data Privacy, Health Transformation Program
Abstract: Turkey has created an e-health vision along with the Health Transformation Program. In this framework,
standard coding systems such as standard definitions of the institutions, databank of healthcare providers,
standard disease, drug and medical supplies classifications have been developed and a national clinical data
warehouse (Health-NET) was established. Health-NET is an integrated, safe, fast and expandable health
information system which aims to improve efficiency and quality of health services by collecting all kinds of
data produced in the health institutions in line with the standards and generating information adequate for all
stakeholders of the collected data.
1 INTRODUCTION
Access to healthcare is regarded as a fundamental
element of social development. While classic theories
of development explain development in terms of
many socio-economic and cultural indicators such as
GNP per capita, level of industrialization and
employment, and consumption level of primary
goods and services, today, it is explained primarily in
terms of indicators related to the access to education
and healthcare. At the end of 2002, the status of the
Turkish health system made it necessary to undertake
radical changes in many areas from service delivery
to financing and from human labor to information
systems. In order to improve the quality of service in
these areas, Turkey has gone through a Health
Transformation Program (HTP) started as early as
2003(OECD, 2014)(Akdag, 2008)(Akdag, 2011). As
a result of the health infrastructure rehabilitation
efforts, Turkey has observed a rapid decline in the
Under-5 Mortality Rate (U5MR) from 29 in 2003 to
7.7 in 2011 per 1000 births (T.D., 2010) Similarly, the
life expectancy at birth has increased to 75 in 2011
from 70 in 2004. Consequently, the satisfaction with
the government provided health services was
measured 75.9% in 2011 comparing to 39.5% in
2003(WHO, 2012). In the context of HTP, the
effective collection and use of nation-wide Electronic
Health Records (EHR)s became a primordial goal. In
parallel with the development of the relevant
legislative framework, a national clinical warehouse
(CDW) that collects EHR and other operational data
from all health organizations in the country had been
established in 2012 and became operational. As
analogous to the worldwide approach of putting the
health information at the center of decision processes
along with the patient, the data collected from the
healthcare facilities are used to structure and manage
the new health infrastructure of the country (De Mul,
2012)(Yoo, 2014). Generally speaking, CDW is used
to empower traditional application software in order
to analyze public health behavior and support several
different decision workflows such as clinical quality
improvement (Weiner, 2012), pay-for-performance(
Van Herck, 2010) and evidence-based medicine
systems (Sacklett, 2000). The integration and use of
diverse healthcare data from various sources into the
same clinical repository is a challenging problem
when implemented at a nation-size level. The
problem becomes even more complex when Hospital
Information Systems (HIS) that create the collected
data are autonomous and implemented with different
technologies. The current HIS market in Turkey
includes more than 150 private firms that implement
their customized software in more than 1500
healthcare facilities operating with more than 200.000
beds capacity (Kose, 2013). In this paper, we share
our experience in implementing CDW and its use in
the critical decision processes of the Ministry of
93
Yildiz U. and Keles A.
Building Ð
ˇ
r National Clinical Data Warehouse.
DOI: 10.5220/0005890000930097
In Proceedings of the Fourth International Conference on Telecommunications and Remote Sensing (ICTRS 2015), pages 93-97
ISBN: 978-989-758-152-6
Copyright
c
2015 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Health of Turkey. We summarize the design and
operation processes, the software architecture, its use
in Health Transformation Program and the lessons
learned.
2 BACKGROUND
In this section, we describe some of the main aspects
of a large-scale CDW that needs conceptual and
technical considerations.
2.1 Data Collection
The health institution that provides CDW with data is
composed by Level I Family Practitioners, Level II
Public and Private Hospitals and Level II University
Hospitals and Research Centers. It is obvious that the
data collection might not be achieved with 100\%
accuracy due to the complexity of data and the
widespread use of the system. Data collection
services are frequently updated due to the updates in
the data packages definitions. This continuous
process requires a tight coordination with Hospital
Information System (HIS) providers that will
implement client component for data upload to
collection services. Due the difficulties in the
integration process that needed continuous support, a
help desk has been established by the Ministry of
Health. The help desk provided regular data on the
amount of data collected by CDW, the amount and
type of upload errors to HIS firms. It has been
recognized that the success of integration capabilities
of institutions that belong to different levels are
different. Level I institutions were 99% successful in
uploading their data as described in the integration
kits of CDW public website. Level II institutions were
less successful in sharing their data. The main reason
behind the successful integration of Level I
institutions was based on the underlying business
model which makes possible the calculation of
practitioners salaries based on the collected data by
CDW. While Level I data collection was successful,
Level II data collection had not been as expected and
it was below 60% average for the first year. The main
reason for the lack of data was that Level II
institutions were not subject to any business model
implemented by CDW. The second year of the
implementation of CDW, the data collection rate was
increased to 77% as the parameters for Service
Quality Standards were started to be calculated with
CDW data. The integration of Level III research
institutions were even less successful given that they
were not managed by the Ministry but by independent
universities. During the third year, the integration of
Level II has improved by the increasing calculation
of different healthcare service parameters using
available CDW data.
2.2 Data Quality
It is important that we should not confuse the concept
of 'data quality' to the aforementioned concept of
'clinical quality data'. While 'clinical quality data' is
specific data based on clinical quality indicators
which help to understand the clinical quality of the
services provided to patients with specific diseases
e.g. diabetes, stroke etc. On the other hand, 'data
quality' is about the quality of any data collected by
CDW and based on certain criteria sets e.g. complete,
valid/correct, timely, without duplication (Kahn,
2012)(Arts, 2002). In this section, we detail the issues
and our solutions to improve the ‘data quality’ of the
‘clinical quality indicators’ collected for CDW. The
major issue that has been encountered in establishing
the data quality was the data wrongly packed that do
not fulfill data package acceptance rules. We
identified the main reason was the difficulties
associated with the establishment of data packages to
be sent to CDW. On the other hand, we identified HIS
users use different ICD-10 (WHO, 2004) codes for
certain diagnosis and diseases because HIS require
sophisticated data input interfaces for the latters. One
particular aspects that needs special attentions is the
geographic and temporal properties of the clinical
data. It is observed that public health indicators could
be misleading based on certain periods and on
locations (e.g. Temporary Refuge Spaces), these
problems are configured by expert knowledge.
2.3 Data Privacy
The privacy of EHR had been a high priority concern
in the implementation of CDW and the tools that
manage its data. In the collection process of EHR, the
definition of data packages was mainly defined by the
public health surveillance necessities and the
establishment of personal health records. The idea
behind the establishment of personal health records is
to support the continuity of healthcare and prevent
redundant services such as radiology. One other
advantage of the involvement of patients in the
structuring the records is the elimination of
inconsistencies. Turkish citizens have a unique and
publicly available 10 digit number. The use of this
number considerably facilitates the consolidation and
access of personal health records but in the same time
could be a major privacy concern.
Fourth International Conference on Telecommunications and Remote Sensing
94
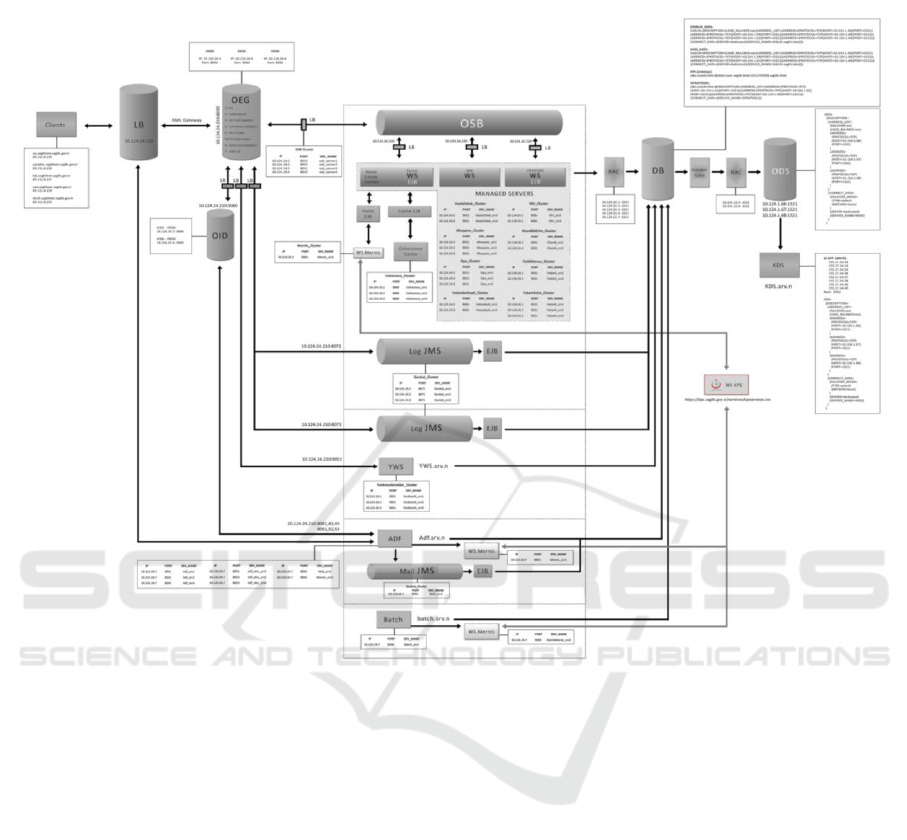
Figure 1: Overview of Architecture
In order to overcome with privacy concerns, an
electronic consent form has been implemented in
personal health record system (MoH, 2015). Patients
can login and configure their preferences on the use
of their records. The preferences are overwritten only
in the case of emergency room services. It is
recognized that the collection private health
information and its computation after de-
identification of data still can be a privacy concern as
the identification of patient is possible with the
combination of different queries (Fernandez, 2013)
For certain diagnosis and diseases codes (e.g. HIV),
we have decided to collect the records without
identifiable information and a cryptic number without
publicly available citizenship number
3 SOFTWARE ARCHITECTURE
Figure 1 describes the overview of the architecture of
CDW with components related to data collection
through web services, storage and data analyze
modules. Messages coming from healthcare facilities
are collected under HL7 form by Load Balancer
component. Received messages are forwarded to an
available XML Gateway. In parallel, HL7 messages
are processed asynchronously by the JMS log queue.
During its flow throughout the XML Gate way, the
Authentication happens with LDAP on OID. Next,
HL7 message is validated against XSD schema and
Schematron processes business rules (mandatory and
optional fields in data packages). After the validation,
HL7 messages are transformed to a local data format
to be saved in the database. The transformed
messages are also validated against XSD Entity.
Building а National Clinical Data Warehouse
95

Figure 2: Functions available on dashboard
Collected messages are transferred to Service
Bus. In the latter, the data is unpacked and the patient
ID is verified through an external ID verification
service (WS-Mernis). Figure 2 describes some of the
functions available to users.
4 CONCLUSIONS
This paper has presented a small set of lessons learned
from the establishment of a National Data
Warehouse. The main research problems that we took
the challenge on were: Data quality, data collection
and data privacy issues. Although the patient count
and basic computational problems were manageable
with relation data models and systems, the advanced
computation of patient records such as disease
correlation analysis, organization of cohorts for
evidence-based medicine applications require the use
of big data solutions.
REFERENCES
OECD, Oecd reviews of health care quality: Turkey
2014doi:http://dx.doi.org/10.1787/9789264202054-en.
URL /content/book/9789264202054-en
R. Akdag, Turkey health transformation program 2003-
2010, Tech. Rep. 839, Re- public of Turkey, Ministry
of Health (June 2011).
R. Akdag (Ed), Health transformation program in turkey
and primary health care services, Tech. Rep. 770,
Republic of Turkey, Ministry of Health (November
2008).
T. D. V. D. Lilia Jelamschi, Decline in the under-5 mortality
rate (u5mr) in turkey: A case study, Tech. rep.,
UNICEF,
http://www.unicef.org.tr/files/bilgimerkezi/doc/declin-
in-the-under-5-mortality-rate-u5mr-in-turkye-a.pdf
(March 2010).
W. H. O. R. O. for Europe, Successful health system
reforms: The case of turkey, Tech. Rep. WHO LIS
e96508, World Health Organization: Regional Office
for Europe (May 2012).
M. De Mul, P. Alons, P. Van der Velde, I. Konings, J.
Bakker, J. Hazelzet, Development of a clinical data
warehouse from an intensive care clinical information
system, Computer methods and programs in
biomedicine 105 (1) (2012) 22–30.
S. Yoo, S. Kim, K.-H. Lee, C. W. Jeong, S. W. Youn, K. U.
Park, S. Y. Moon, H. Hwang, Electronically
implemented clinical indicators based on a data ware-
house in a tertiary hospital: its clinical benefit and
effectiveness, International journal of medical
informatics 83 (7) (2014) 507–516.
J. P. Weiner, J. B. Fowles, K. S. Chan, New paradigms for
measuring clinical performance using electronic health
records, International Journal for Quality in Health
Care 24 (3) (2012) 200–205.
Fourth International Conference on Telecommunications and Remote Sensing
96

P. Van Herck, D. De Smedt, L. Annemans, R. Remmen, M.
B. Rosenthal, W. Sermeus, Systematic review: effects,
design choices, and context of pay-for- performance in
health care, BMC health services research 10 (1) (2010)
247.
D. L. Sackett, Evidence-based medicine, Wiley Online
Library, 2000.
R. Kose, Health statistics year book, Yearbook 978-975-
590 509-9, Agency of Health Research (2013).
M. G. Kahn, M. A. Raebel, J. M. Glanz, K. Riedlinger, J. F.
Steiner, A pragmatic framework for single-site and
multisite data quality assessment in electronic health
record-based clinical research, Medical care 50.
D. G. Arts, N. F. De Keizer, G.-J. Scheffer, Defining and
improving data quality in medical registries: a literature
review, case study, and generic framework, Journal of
the American Medical Informatics Association 9 (6)
(2002) 600–611.
W. H. Organization, et al., International statistical
classification of diseases and health related problems
(the) icd-10, Ph.D. thesis, World Health Organization
(2004).
T. M. of Health, E-nabiz personal health records system, ,
https://enabiz.gov.tr/Giris.aspx (2015).
J. L. Ferna ́ndez-Alema ́n, I. C. Sen ̃or, P. A ́. O. Lozoya, A.
Toval, Security and privacy in electronic health
records: A systematic literature review, Journal of
biomedical informatics 46 (3) (2013) 541–562.
Building а National Clinical Data Warehouse
97
