
Towards an Access Control Model for Collaborative Healthcare Systems
Mohamed Abomhara and Geir M. Køien
Department of Information and Communication Technology, University of Agder, Grimstad, Norway
Keywords:
Access Control, Authorization, Electronic Health Records, Security, Privacy, Collaborative Healthcare
Systems.
Abstract:
In this study, an access control model for collaborative healthcare systems is proposed. Collaboration require-
ments, patient data confidentiality and the need for flexible access for healthcare providers through the actual
work they must fulfill as part of their duties are carefully addressed. The main goal is to provide an access
control model that strikes a balance between collaboration and safeguarding sensitive patient information.
1 INTRODUCTION
Healthcare services necessitate collaborative support
from multiple parties to fulfill the information re-
quirements of daily clinical care and provide rapid
patient care (Moonian et al., 2008). Collaborative
support is required within healthcare organizations
such as hospitals, where patient records must be
moved among healthcare professionals, laboratories
and wards, to name a few. Collaboration among
healthcare organizations is also essential for patients
being transferred from one healthcare provider to an-
other for specialized treatment. Such collaboration
within or among healthcare organizations has been
shown to provide cost-effective healthcare services
(Alshehri and Raj, 2013). However, collaboration and
information sharing raise security and privacy con-
cerns (Gajanayake et al., 2014). Patient records con-
tain sensitive information that calls for appropriate
access control mechanisms to ensure confidentiality
and protect integrity of data as well as filter out ir-
relevant information to reduce information overload
(Alhaqbani and Fidge, 2008).
Access control is defined as a mechanism through
which users are permitted access to resources accord-
ing to their identities (authentication) and associated
privileges (authorization) (Hu et al., 2006). Access
control mechanisms have undergone many develop-
ments in both academia and industries in order to
meet healthcare domain needs. However, progress to
date has not been sufficient to fulfill the security re-
quirements of a collaborative healthcare environment
(Alhaqbani and Fidge, 2008). The majority of mod-
els, such as Role-Based Access Control (RBAC) (Fer-
raiolo et al., 2001) and Attribute-Based Access Con-
trol (ABAC) (Hu et al., 2014) for instance, help re-
strict medical records to users based on certain roles
and attributes, but sensitive information can still be
compromised by authorized insiders (Alshehri et al.,
2013; Alshehri and Raj, 2013; Ferreira et al., 2007).
Such models and extensions have been employed in
specific applications to manage information access in
a controlled environment. Nevertheless, few stud-
ies have addressed the issue of managing informa-
tion access within the context of team collaboration
(Thomas, 1997; Georgiadis et al., 2001; Alotaiby and
Chen, 2004) and workflow (Le et al., 2012; Russello
et al., 2008). This study, proposes an access con-
trol model that is secure, flexible, easy to manage,
and supports cooperative engagements. Our focus is
mainly on collaborative activities that are best accom-
plished through organized groups of healthcare practi-
tioners within or among healthcare organizations with
the objective of accomplishing a specific work (treat-
ment of patient’s case).
1.1 Collaboration and Secure Sharing
of Healthcare Data
Healthcare providers deal with large amounts of sen-
sitive healthcare records which are shared and collab-
oratively used among different healthcare practition-
ers (Fabian et al., 2015). Collaboration occurs when
a healthcare provider such as primary care doctor re-
quests help from another healthcare provider to treat
a case. Figure 1 provides an example scenario of col-
laboration and sharing of healthcare data.
In this scenario, a 7-year old patient visited his pri-
mary care doctor with high body temperatures. The
Abomhara, M. and Køien, G.
Towards an Access Control Model for Collaborative Healthcare Systems.
DOI: 10.5220/0005659102130222
In Proceedings of the 9th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2016) - Volume 5: HEALTHINF, pages 213-222
ISBN: 978-989-758-170-0
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
213
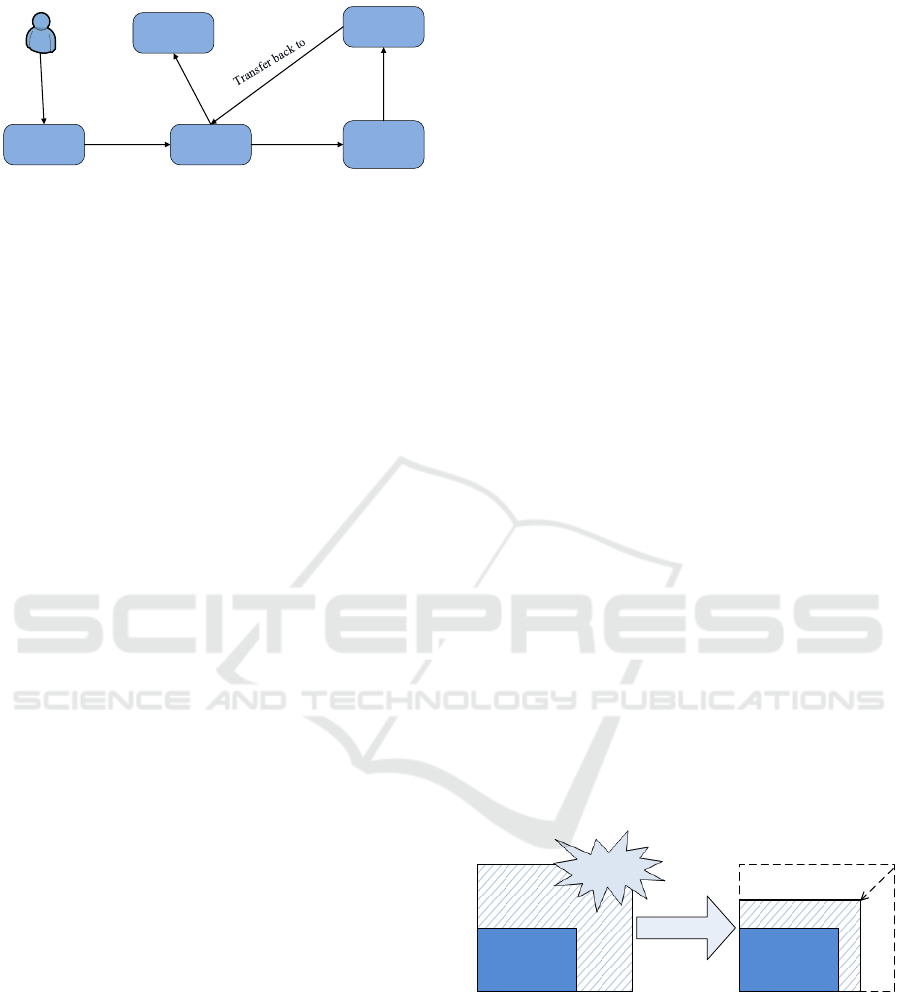
Patient
Primary care
doctor
Discharged
General
medicine ward
Infectious
diseases
consultation
Cardiology
consultation
Visit
Admit to
Request
consultation
Transfer
Share PHRs
PHRs : Patient Healthcare Records
Share PHRs
Share PHRs
Figure 1: An example scenario of collaboration and sharing
of healthcare data.
patient was quickly examined by the primary care
doctor and the cause of fever could not be found.
The patient was admitted to the general medicine
ward, where he was reassessed by the attending physi-
cian who requested some routine blood tests. Upon
admission, the attending physician subsequently re-
quested an infectious diseases consultation because
the patient begun to develop a skin rash. The infec-
tious diseases team investigated further and decided
to consult the cardiology team as they were concerned
about Kawasaki disease. The patient was immediately
transferred to the cardiology ward. Eventually, the pa-
tient made a substantial recovery and was transferred
back to general medicine ward. After spending a few
more days in the hospital, the patient has recovered,
then he was discharged, and advised to see his pri-
mary care doctor for follow-up.
In such group consultation, it is noticed that, sev-
eral healthcare professionals are involved in various
roles to provide patient care. That includes primary
care doctors, general physicians and specialists such
as the infectious diseases team and cardiologists. Ev-
ery participant needs to obtain the medical records
they request based on the health insurance portabil-
ity and accountability act (HIPAA) minimal disclo-
sure principle (Zhang and Liu, 2010; Fabian et al.,
2015). Therefore, sharing and accessing healthcare
records with efficient coordination between health-
care practitioners to perform collaborative work is a
critical function in access control models (Alotaiby
and Chen, 2004). The main concern is about los-
ing control over the sensitive healthcare records while
sharing them with multiple parties. Many researches
(Shen and Dewan, 1992; Thomas, 1997; Rubio-
Medrano et al., 2013) have developed access con-
trol models to support collaborative requirements by
defining a set of rules in the subject, objects and
access rights dimensions. However, these models
are general and quit complex. Additionally, they do
not present an applicable solution for collaborative
healthcare system.
The remaining parts of this study is structured as
follows: section 2 discusses the insider threat prob-
lem in the health domain and presents an overview of
the existing access control models. In section 3, the
proposed access control model is introduced. Conclu-
sions and future works are suggested in section 4.
2 BACKGROUND
In this section, a brief overview of the insider threat
problem in the healthcare domain is presented along
with existing access control models and their pros and
cons with respect to health systems.
2.1 Insider Threat
As shown in our scenrio (Fig.1), healthcare services
need the collaborative support of multiple healthcare
professionals and administrators in order to deliver
rapid patient care. Therefore, multiple users (e.g.
doctors and nurses) may require access to patient in-
formation to perform tasks. For this reason, insider
abuse or misuse of privileges (Probst et al., 2010) can
be a threat to patient information and a liability for
health care providers. One of the main causes of in-
sider threats in collaborative healthcare is information
leakage, which emerges when a supporting party is
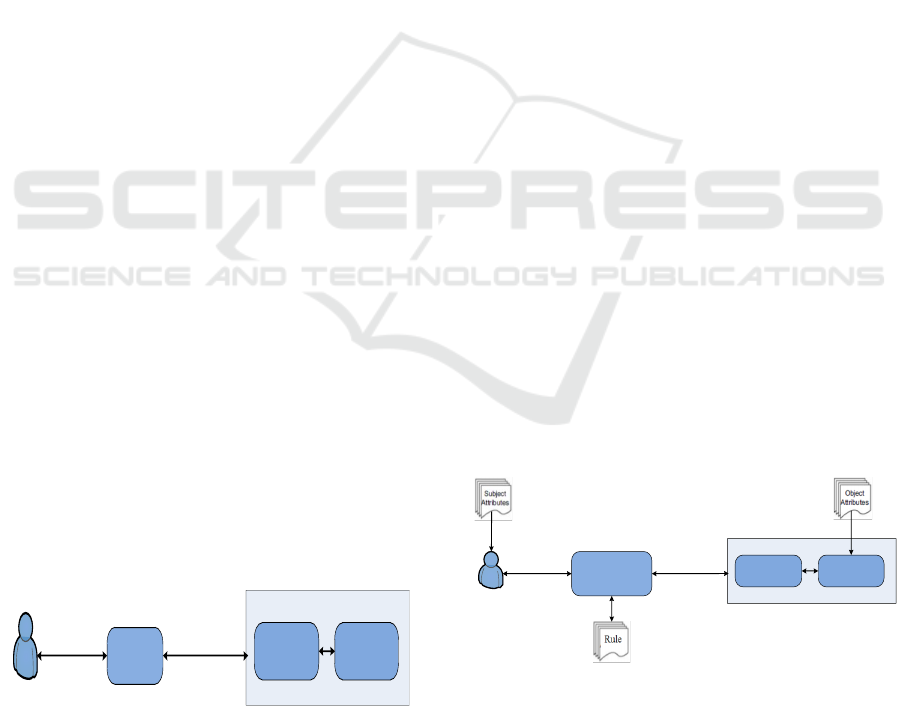
granted access beyond what is actually required (Fig-
ure 2 (a)). For instance, in treating a patient case, the
main practitioner consults a specialist from another
department. In doing so, improper information ac-
cess might occur if the specialist (e.g. cardiologist)
obtains more permission than required. The key to
solving this issue is to minimize the discrepancy (Fig-
ure 2 (b)) between the granted access and the required
access based on what is really needed.
Required
Granted
Required
Granted
Improper
Access
Figure 2: (a) Granted vs required information access and
(b) Minimization of access discrepancy.
2.2 Access Control Models
Research in security area has made every possible ef-
fort to address security challenges related to autho-
rization and access control. In this section, exist-
ing access control models are discussed, and their
strengths and weaknesses are identified with respect
to healthcare systems.
HEALTHINF 2016 - 9th International Conference on Health Informatics
214
2.2.1 Discretionary Access Control (DAC)
DAC (Hu et al., 2006; Kayem et al., 2010; Sama-
rati and Di Vimercati, 2001) defines access control
privileges based on the subject’s identity and the ac-
cess rules in place. It determines whether the subject
can or cannot execute particular actions on specific
resources (objects or files). DAC allows the subject
to own resources and for ownership to be transferred
to another subject (Majumder et al., 2014). Although
DAC policies tend to be flexible and are widely de-
ployed, DAC has several drawbacks when utilized in
healthcare systems (Alhaqbani and Fidge, 2008; Ga-
janayake et al., 2014). First, ownership and permis-
sion updating is not scalable, as the number of users
and medical records are continuously growing. Sec-
ond, DAC policies do not provide high security assur-
ance, because granting read access is transitive and,
DAC allows data to be copied from one resource to
another, which can result in unintentional information
flow in a system (Hu et al., 2006).
2.2.2 Mandatory Access Control (MAC)
In MAC (Samarati and Di Vimercati, 2001; Hu et al.,
2006; Majumder et al., 2014), a subject cannot change
the access rights to objects because access control
policy decisions are made by a central authority. Un-
like DAC, MAC controls information flow to en-
sure information confidentiality and integrity (Kayem
et al., 2010). However, enforcing MAC policies in
healthcare systems is often very difficult due to the
vast numbers of users, the wide range of data types,
and the requirements to give patients control owner-
ship of their own medical records.
2.2.3 Role-based Access Control (RBAC)
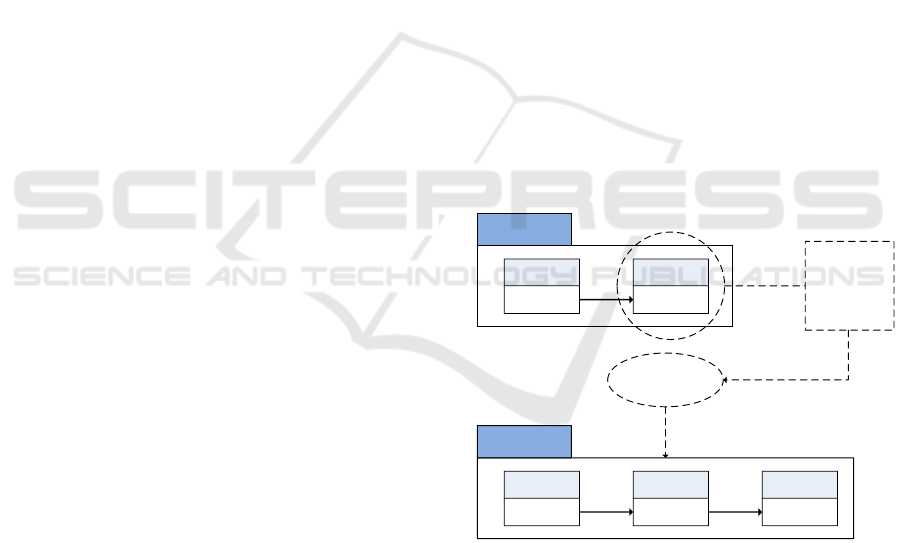
RBAC (Ferraiolo et al., 2001) allows organizations to
enforce access policies based on subjects’ roles (job
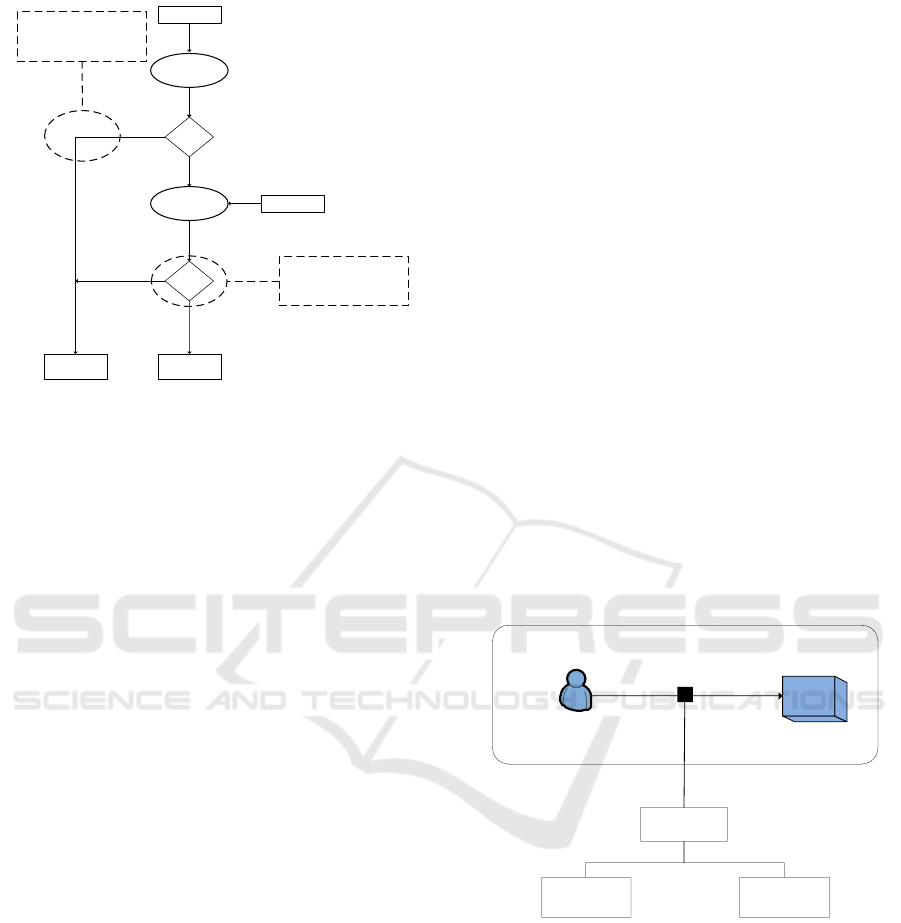
functions) rather than users or groups, as shown in
Figure 3.
Subject
Role
Subject Assignment
Operation Object
Permission Assignment
Permission
Activity
Attribute
Task
Collabrative
Context
Criteria
PolicySpace-time
Role
Discretionary
Environment
Request Permission
Figure 3: Overview of the RBAC model.
Subjects (users) are assigned roles (e.g. patient,
doctor, or nurse), permissions (or access rights) are
then grouped based on the roles. Access to resources
(medical records in this case) is restricted to au-
thorized individuals according to the assigned roles.
RBAC has a number of advantages, including flex-
ibility in terms of permission administration man-
agement, since roles can be updated without updat-
ing permissions for every user. Moreover, the use
of role hierarchies provides additional advantages, as
one role may implicitly include operations associ-
ated with another role. Also, the separation of du-
ties (SoD) principle ensures that no user is allowed
to execute two roles simultaneously. Although the
RBAC model has several advantages, it also has dis-
advantages. That is why it is not efficiently imple-
mented in healthcare environments. Insider threats
are a common problem faced by healthcare systems
due to RBAC’s lack of granularity (Alshehri and Raj,
2013). Roles are not sufficiently granular to restrict
data access to only the right (authorized) subjects.
For example, consider a role that is associated with
a set of permissions. Any subject in this role would
be allowed the permissions associated with this role
(Alshehri et al., 2013). Furthermore, RBAC does
not consider healthcare provider workflow (Russello
et al., 2008) nor separate task from role. Various
types of tasks with different access control character-
istics are dealt with in the same manner (Oh and Park,
2003).
2.2.4 Attribute Based Access Control (ABAC)
In ABAC (Hu et al., 2014), permissions to access the
objects are not directly given to the subject. It uses
attributes of the subject (e.g. name, age or role in
organization) and attributes of object (e.g. metadata
properties) to provide authorizations as shown in Fig-
ure 4. The permissions in ABAC depend on a com-
bination of a set of attributes and their relative values
(Ubale Swapnaja et al., 2014).
Subject
Policy Decision
Engine
Operation Object
Permission
Authorization
Figure 4: Overview of the ABAC model.
ABAC overcomes the user role assignment prob-
lem exist in RBAC and focuses on the attributes of
a user requiring to grant access. It is a very flex-
ible model that is considerably easier to administer
than RBAC. However, higher flexibility comes with
Towards an Access Control Model for Collaborative Healthcare Systems
215
higher complexity due to the specification and main-
tenance of the policies. The number of subjects and
objects in healthcare systems increases dynamically.
This requires maintaining database which contains all
attributes in same format (Verma et al., 2012).
2.2.5 RBAC Extensions
The strength of RBAC lies in its manageability. It is
fairly easy to assign authorization to users based on
their roles. Unfortunately, RBAC alone does not suf-
fice to handle various constraints that are required in
diverse domains. RBAC has been broadly extended
to support diverse domains in data authorization man-
agement with various constraints. Extensions in-
clude task-role based (Oh and Park, 2003), team-
based (Thomas, 1997; Georgiadis et al., 2001), con-
textual role-based (Motta and Furuie, 2003), context-
aware (Koufi and Vassilacopoulos, 2008) and so forth
(Tolone et al., 2005). However, these extended mod-
els would add additional complexity to healthcare
systems because they still face some problems (Moo-
nian et al., 2008). Granularity and manageability are
inversely proportional to one another. Higher gran-
ularity in security invariably implies more complex
management. This is apparent in attribute-based ac-
cess control (ABAC), which offers higher control or
granularity at the expense of lower manageability. On
the other hand, role-based access control (RBAC) ev-
idently provides lesser granularity for better manage-
ability. To combine the strengths of both approaches
without being hindered by their limitations, bilayer
access control (BLAC) has been devised (Alshehri
et al., 2013; Alshehri and Raj, 2013). BLAC enforces
a two-layer access control that initially applies RBAC
and ABAC. The model uses the concept of pseudo-
role, which is defined as a set of static attributes of
subjects. A pseudorole is not a real role, which is
traditionally defined as a job function. Subjects’ at-
tributes are categorized as static attributes (when at-
tribute values typically do not change) used to gen-
erate pseudoroles and dynamic attributes (when at-
tribute values change frequently). Static and dynamic
attributes are used in policies to constrain pseudoroles
(Alshehri and Raj, 2013).
Despite the advantages offered by BLAC, it is
not exclusively tailored for collaborative healthcare
system. BLAC focus has not been placed on sup-
porting collaboration and coordination work. Thus,
an additional policy can be defined at the 2
nd
layer
of BLAC to ensure more secure interaction between
cooperating parties. Although secure collaboration
is achievable via intricate policy management, doing
this would basically reduce the approach to ABAC.
Thus, the issue of low manageability may resurface
when using BLAC to secure a collaborative effort.
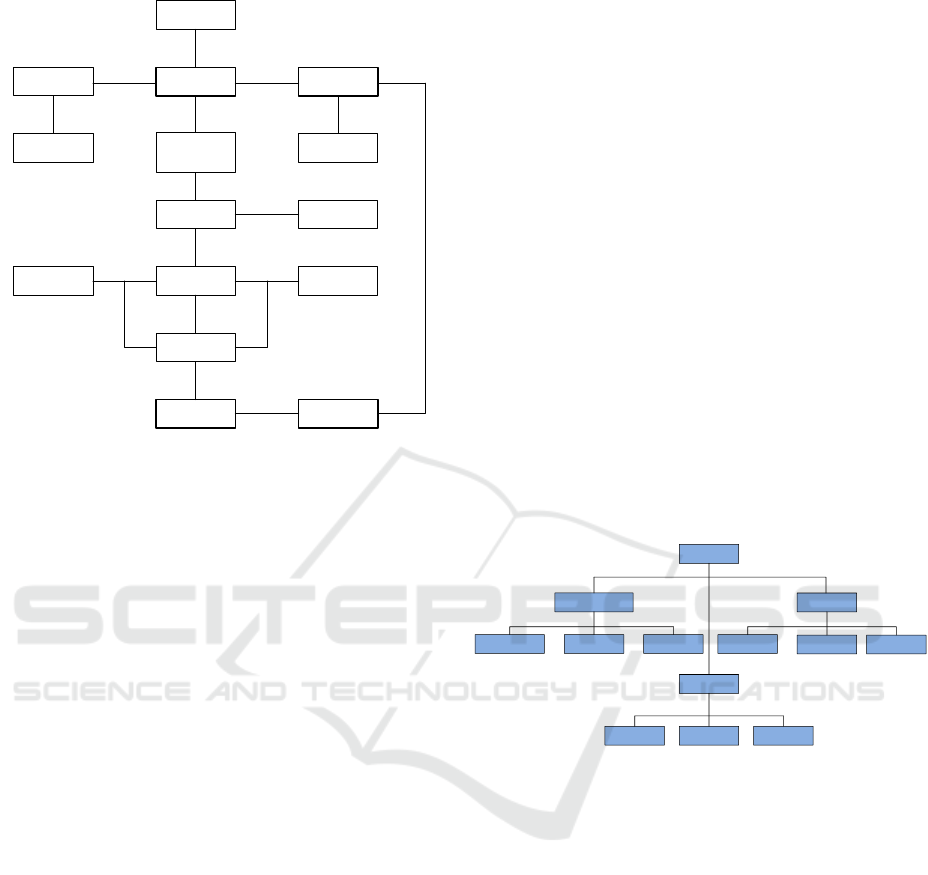
3 PROPOSED ACCESS CONTROL
MODEL
To alleviate the aforementioned limitation of BLAC
and satisfy access control requirements for collabo-
rative healthcare systems, work-based access control
(WBAC) model is proposed (Figure 5). In the pro-
posed model, a secondary RBAC layer, with extra
roles extracted from team work requirement, is added
to BLAC to manage the complexity of cooperative
engagements in the healthcare domain. Policies re-
lated to collaboration and team work are encapsulated
within this coordinating layer to ensure that the at-
tribute layer is not overly burdened. The main con-
cepts of our model are:
1. Subjects are assigned to pseudoroles and/or team
role (section 3.1) and objects are associated with
WBAC policies; main policy and collaboration
policy.
2. Access control is performed on three-step evalua-
tion procedure; pseudoroles evaluation, team role
evaluation and rule examination (section 3.3).
BLAC
First layer
RBAC
Second layer
ABAC
WBAC
First layer
Primary
RBAC
Second layer
Secondary
RBAC
Third layer
ABAC
Complex
coordination
of policies
at the
attribute level
Restructuring
Figure 5: BiLayer Access Control and Work Based Access
Control.
In this study, ”work” is defined as an entity com-
prising a collection of elements that interact with one
another for a particular outcome to be achieved suc-
cessfully. As shown in Figure 6, the fundamental idea
is that work itself demands completion, and it is di-
rectly linked to the patient, context, personnel and
goal.
A goal is directly linked to an objective and an
objective is broken down into a set of tasks. The
difference between a goal and an objective is that, a
HEALTHINF 2016 - 9th International Conference on Health Informatics
216
Patient
Context Work Personnel
Time
Long-term
goal
Role
Objective Purpose
Task (k)Task (1) Task (n)
Workflow
Resource Policy
Figure 6: Work Model for Collaboration.
goal consists of long-term aims that need to be ac-
complished (e.g. treatment of patient) and an ob-
jective comprises of concrete attainments that can be
achieved by following a certain number of steps. Per-
sonnel in the collaboration will have their own roles.
In performing a certain task, personnel must access
resources that are governed by policies.
3.1 Team Role
Team is defined as a collection of participants in spe-
cific role with objective of accomplishing a specific
work (Thomas, 1997). Each team has a responsible
team manager. Any of the participants joining a team
shares a common goal and may share a default set of
permissions for their cooperative work. The notion of
a team role is used to restrict access permissions to
those individuals who not only have the right organi-
zational roles but also are associated to the task via
team membership (Wang, 1999).
Regarding the process of collaboration and team
work, access control model must be able to provide
an efficient and secure platform for people to work
together in a hospital without being deterred by re-
strictive enforcement of access control policies (Le
et al., 2012). This can be a rather delicate situation
to handle, given the fact that the fluidity of team-
work within the medical domain is often incongru-
ent with technological security. To demonstrate this
notion, we consider a scenario (section 1.1) involv-
ing four medical practitioners who are working to-
gether on a patient’s case. For the sake of securing the
patient’s private (sensitive) data (e.g. mental illness,
etc.), the collaboration must be clearly defined. By
default, only the main practitioner should be aware
of the patient’s personal information (need-to-know
principle). The three other medical practitioners with
supporting roles are given information based on their
contributing roles. In order to achieve this, it is imper-
ative to determine the finer roles of each team mem-
ber. The team role of each member will subsequently
determine the extent of access given. For instance,
if the supporting party is included solely for consul-
tation purposes concerning the disease, only informa-
tion essential for diagnosis is provided. It is not neces-
sary to allow perusal of personal information related
to the patient. In this way, improper access to the pa-
tient’s sensitive information can be prevented.
Hospital personnel roles are often simplistically
split into medical practitioners, nurses and adminis-
trators. However, their roles in a team can be further
categorized using the team role theory (C
´
ordoba and
Piki, 2012). This theory contends a total of nine roles
per group, which are classified into thought, action
and management. For the purpose of this research,
they are rephrased and illustrated in Figure.7.
Role
Action
CheckerDoer Motivator
Management
NetworkerCoordinator Mediator
Thought
Evaluator
Thinker
Mentor
Figure 7: Taxonomy of Team Role.
Thought denotes a role that is dominated mostly
by thinking. To be a successful thought collabora-
tor, the person may need to understand the medical
predicament in detail without necessarily knowing the
patient. A worker in this role could be involved in de-
vising strategies to confront particular medical enig-
mas. Thus, a cardiology specialist may offer his/her
expertise regarding the best practices of performing a
heart transplant on a child without being involved in
the actual operation.
Action, as the labeling suggests, signifies being
involved in task-related collaboration, such as meet-
ing the patient for a medical check-up. Having an
action role usually implies close interaction with the
patient. Nevertheless, discretion is still feasible with
care. For instance, an anesthesiologist needs to only
know the patient’s physical characteristics to prepare
anesthetic. Who the patient is, or where the patient
lives is not relevant to completing this task.
The management category comprises personnel
Towards an Access Control Model for Collaborative Healthcare Systems
217
who are mostly involved in managing others. These
types of collaborators are adept at coordinating team-
work that is susceptible to social or psychological
challenges. For example, in conflict management,
they may have to resolve series of opposing diagnoses
made by medical practitioners and that may otherwise
escalate into serious altercations. In this regard, such
personnel’s need for information is inwardly oriented.
They have a greater need to know personal informa-
tion about others working at the hospital rather than
of patients.
3.2 Work-Based Access Control
Work-based access control (WBAC) combines the
pseudorole in BLAC (section 2.2.5) and team role to
enable a multilayered role facility that is driven by
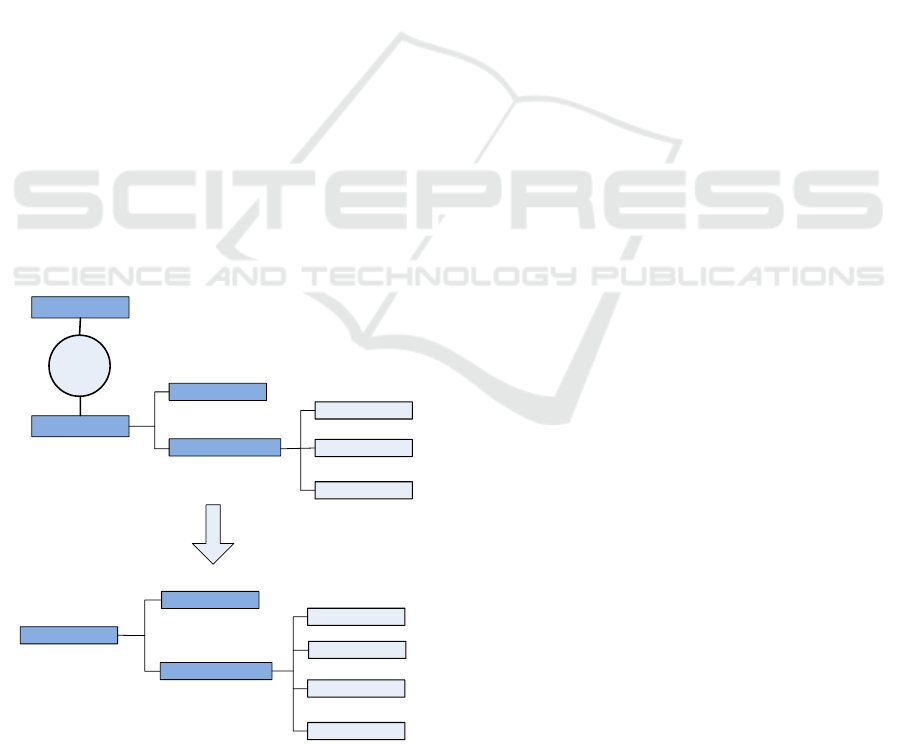
collaboration. Merging (Figure 8) is done by sim-
plifying the inherent classification of team roles into
four elementary roles, i.e. the main, thought, action
and management roles. Here, collaborative team roles
are combined with the main role and are placed in the
same group. This way, access control is enforced with
superior flexibility and it promotes abstraction of the
collaborative characterization of access control from
the main flow. This ensures more manageable im-
plementation as a whole. Process wise, the original
BLAC procedure is enhanced with an added decision
mechanism that provides an alternative route for par-
ties beyond the normally established policy.
Pseudorole
Team Role
Merging
Main
Collaborative
Thought
Action
Management
Pseudorole
Team Role
Main
Management
Action
Thought
Role
Figure 8: Merging of Pseudorole and Team Role.
Multiple role layers (Wen et al., 2009) segregate
access validation into two modes. Verification is done
sequentially, whereby normal validation in BLAC
gains precedence over WBAC. In other words, the
pseudorole is validated first, followed by team role
validation. Separating the roles is a delicate agenda
as the integrity of access control during collaboration
must be guaranteed.
consider the following scenario to appreciate the
limitation of BLAC in managing problems potentially
arising with regard to collaborative work. Suppose a
physician from the primary care unit requires the help
of another physician from the oncology department.
In the policy prior to collaboration (Figure 9), only
the physician in the primary care department has ac-
cess to reading the object or resource. Therefore, any
access request by the oncology department physician
would be denied.
The policy defined in Figure 9 can be visual-
ized better by studying the decision logic and pro-
cess in BLAC (Figure 10). The access decision en-
gine always checks the pseudorole’s validity first. The
physician from the oncology department would have
to pass the initial validation for being a physician.
However, when the engine discovers that the physi-
cian’s department is not primary care, access consid-
eration halts immediately. In order to solve this prob-
lem, BLAC recommends a modification to the origi-
nal policy. A possible modification that allows an on-
cology department physician to read data created by
the main, primary care physician, is shown in Figure
11.
To appreciate the limitation of BLAC in managing the issues that may emerge with
regard to collaborative work, consider the following hypothetical scenario. Supposed
that a physician from the primary care unit is requiring the help of another physician
from the oncology department. The policy prior to the collaboration is given below
(Figure ). In this policy, only the physician in the primary care department is given
accessed to reading the object or resource. Therefore, an access request made by the
physician from the oncology department would be denied.
<policy>
<pseudorole>
<(subject.provider = “physician”) AND
(subject.department = “primary care”)AND
(subject.hospital = “st mathew”)
</pseudorole>
<rule>
<subject>”any”</subject>
<object> <object.providerId=subject.Id></object>
<action><action.type=”read”></action>
<env><env.accessIP=”192.168.*.*”></env>
</rule>
</policy>
Figure : Original Policy Prior to Collaboration
The policy defined above can be visualized better by studying the decision logic and
its process (Mourad & Jebbaoui, 2015) in BLAC (Figure ). The access decision
engine would always check the validity of the pseudorole first. The physician from
the oncology department would pass the initial validation because he is a physician.
However, when it discovers that the department of the physician is not primary care,
the access consideration is halted immediately. In order to solve this problem, BLAC
recommends the modification of the original policy.
Figure 9: Original Policy Prior to Collaboration.
At first glance, the policy seems valid. It now of-
fers access to a new department called oncology. En-
abling proper access to the object based on the collab-
orator’s subject ID is somewhat complicated. It is dif-
ficult to define the implications of collaboration on the
rule itself because it is structured by subject, object,
action and environment. Therefore, a new attribute is
introduced known as the ’collaboratorId’. This new
collaboratorId attribute should be enforced only on
two conditions: the objects are created by the physi-
cian and are necessary for collaboration. However,
HEALTHINF 2016 - 9th International Conference on Health Informatics
218
Access request
Pseudorole
validation
valid?
Rule
examination
valid?
Access
granted
Access
denied
Yes
No
Yes
Policy
Difficult to manage length of
collaborative access (e.g. based
on dynamic time) . Also may
inflate original policy
No
Complete termination of access
consideration if valid pseudorole
is not available
Figure 10: Flow of BLAC for Invalid Pseudorole.
this is a rather tedious process because it involves the
additional task of security management. For conve-
nience, suppose that all objects created by the physi-
cian in the primary care department are updated with
the collaboratorId. Updating the objects with collab-
oratorId implies that the oncology department physi-
cian can now read every object created by the former
physician. This is true regardless of each one’s pur-
pose in the collaboration. Thus, if a confidential ob-
ject is created by the primary care physician for the
purpose of a crime investigation, it is visible to the
collaborating oncology physician as well.
Apart from difficulty controlling the scope of ac-
cess, employing BLAC for collaboration can also be
a source of additional complexity in constructing the
rules of a policy. It is worth noting that the modifi-
cation requires two changes. The first change is done
to the pseudorole and the second to the object of the
rule, which is not desirable. It is better to minimize
the changes.
In addition to the aforementioned dilemmas, an-
other issue must be addressed. Controlling the length
of collaboration is also a cumbersome endeavor. For
instance, in limiting the collaborating party’s access
based on the time factor, the rules must be modi-
fied intricately since time is fundamentally dynamic.
If not performed with care, access could be tem-
porally extended beyond necessity. Given the con-
straints faced by BLAC in managing collaborative ac-
cess control implementation, a more dynamic policy
with dual inclination is proposed as shown in Figure
12, whereby the normal policy of enforcing access
control is contained within the main policy. On the
other hand, any policy that mediates resource sharing
is covered by the collaboration policy. This way, bet-
ter access control management is achievable.
Below is the possible modification that allows a physician from the oncology
department to read the data created by the main physician in primary care (Figure ).
<policy>
<pseudorole>
<(subject.provider = “physician”)
AND
(subject.deparment = “primary care”)
AND
(subject.hospital = “st mathew”)
</pseudorole>
<rule>
<subject>”any”</subject>
<object> <object.providerId=subject.Id></object>
<action><action.type=”read”></action>
<env><env.accessIP=”192.168.*.*”></env>
</rule>
</policy>
<policy>
<pseudorole>
<(subject.provider = “physician”)
AND
(subject.department = “primary care”
OR subject.department=”oncology”)
AND
(subject.hospital = “st mathew”)
</pseudorole>
<rule>
<subject>”any”</subject>
<object>
<object.providerId=subject.Id
OR
object.collaboratorId=subject.Id>
</object>
<action><action.type=”read”></action>
<env><env.accessIP=”192.168.*.*”></env>
</rule>
</policy>
Figure : Modified Policy Due to Collaboration
Figure 11: Modified Policy Due to Collaboration.
Certain concerns may arise with a dual policy in
the access control model, the most apparent of which
would be priority. For instance, in situations where
one policy opposes the other, which would dominate?
It is therefore clearly defined that when two policies
are in conflict, the main policy is always given the
highest priority, regardless of context.
Subject
Environment
Object
Policy
Main policy
Collabration
policy
Figure 12: Dual Policy in WBAC.
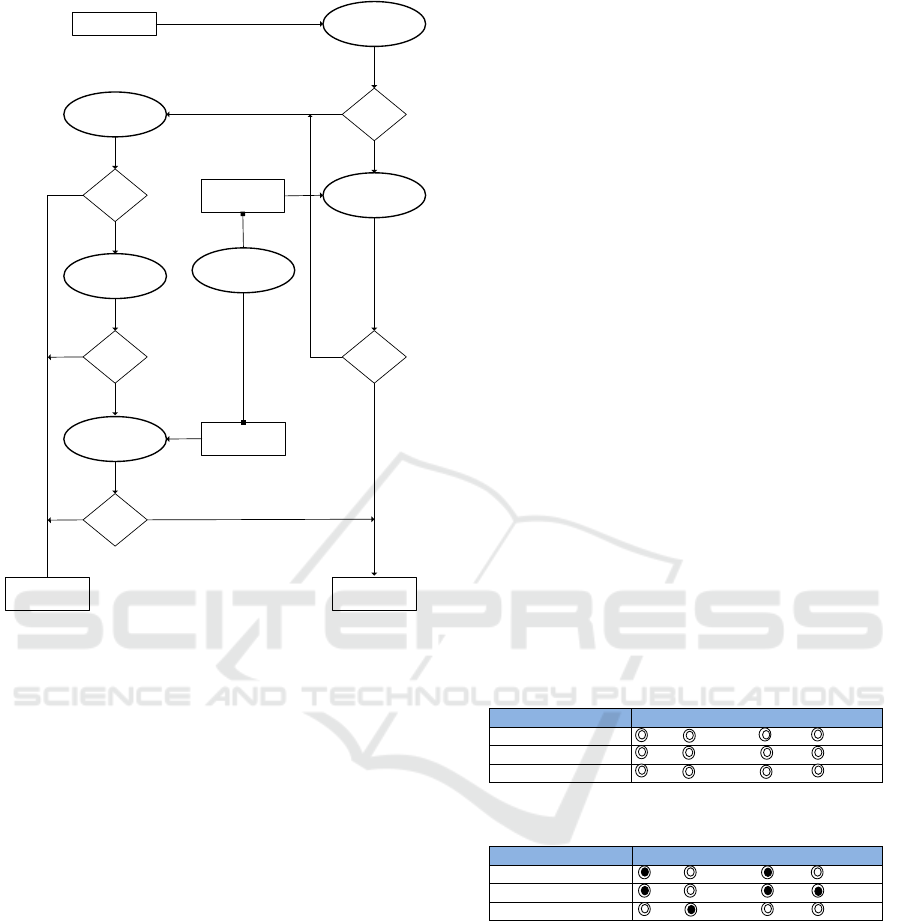
3.3 Flow model of WBAC
Similar to the core process of BLAC, access request
in WBAC first undergoes pseudorole validation as
shown in Figure 13. At this stage, the user’s pseudo-
role is compared against the one defined in the policy.
In BLAC, failing this step results in the complete ter-
mination of decision logic. WBAC, however, treats
this differently. If the request fails, the resource is in-
spected further to determine whether it is part of col-
laborative work. If it is, then the team role of the user
in question is properly extracted and examined.
Towards an Access Control Model for Collaborative Healthcare Systems
219
Access request
Pseudorole
validation
valid?
Collaborative
resource
No
Rule
examination
Team Role
validation
Coordination
Rule
examination
valid?
valid?
valid?
Main policy
valid?
No
Access
granted
Collaborative
policy
Access
denied
No
No
Yes
No
Yes
Figure 13: Flow of WBAC.
In cases where the user possesses a valid team role
over the resource, the extent of access is determined
by the collaborative policy. This policy controls the
granting of access according to the user’s purpose
within the team. For instance, users with the action
team role receive more access to a patient’s personal
information as compared to users with the manage-
ment team role. This is because the former type of
user is in greater need of the information to perform
their job than the latter.
Complications might arise in terms of coordinat-
ing the ramification of two different policies, i.e. the
main and collaborative policies. Considerable con-
cern would also pertain to whether a request initially
denied by the main flow should be granted access by
an alternative flow. In resolving this, it must be noted
that the nature of collaboration is never free from
risk. Sharing information always entails compromise
to certain parts of security. As such, it is impossible
to negate the danger altogether.
As mentioned in earlier sections 2.1, a realistic
way of handling collaboration risk is to minimize the
discrepancy between the granted and the required ac-
cess. This is where the coordination element becomes
vital. The delimiting principle of access restriction
must be balanced with the necessity for information
distribution. Excessive restriction can hamper coop-
eration while too much freedom can entirely defeat
the purpose of security.
A way of simplifying conflict resolution between
competing policies is to utilize a tabular representa-
tion in organizing shared resources and team roles.
Each resource contains four options that reflect the
team role involved. The options should not be exclu-
sive by nature and the administrator can select none
or all. Zero selection implies that the resource is not
open to collaborative access and can only be accessed
based on user-related pseudoroles and rules. In con-
trast, complete selection means the resource is pub-
licly available to everyone collaborating.
To concretize the possibility of using tabulariza-
tion in defining a collaboration policy, it would be
useful to consider the illustration below (Figure 14 ).
Here, the collaborative resources required for work
are enumerated in table form. Each shared resource
is tied to the set of collaborative roles or team roles
that can access it. In effect, the selected roles will de-
termine the extent of collaborative access. Note that
the collaborative role for a particular resource should
be set in accordance with its purpose (Figure 15). A
patient’s personal information is vital to the main col-
laborator and those with an action team role. How-
ever, medical information, which might be less sensi-
tive and fundamental to treatment than personal infor-
mation, should be made accessible to most team roles
except the people role.
Collaborative Resource
Collaborative Role
Resource (1)
Main Management Action Thought
Main Management Action Thought
Resource (N)
Main Management Action Thought
Collaborative Resource
Collaborative Role
Patient personal information
Main Management Action Thought
Patient medical information
Main Management Action Thought
Staff personal information
Main Management Action Thought
ABAC
In ABAC, permissions to access the objects are not directly given to the subject. It uses attributes
of the subjects such as subject’s name, age or role in organization and attributes of objects such
as metadata properties to provide authorizations. The permissions in ABAC are depending on the
combination of set of subject and object’ attributes and their relative values.
ABAC overcome the user role assignment problem which exist in RBAC and focuses on
the attributes of a user required to grant access. It very flexible model that is considerably easier
to administer than RBAC. However, higher flexibility comes along with the higher complexity
due to the specification and maintenance of the policies. The numbers of subjects and objects in
healthcare systems is dynamically increased, which require maintained database containing all
attributes in same format.
Figure 14: Simplification of Collaborative Role into Tabular
Form.
Collaborative Resource
Collaborative Role
Resource (1)
Main Management Action Thought
Main Management Action Thought
Resource (N)
Main Management Action Thought
Collaborative Resource
Collaborative Role
Patient personal information
Main Management Action Thought
Patient medical information
Main Management Action Thought
Staff personal information
Main Management Action Thought
ABAC
In ABAC, permissions to access the objects are not directly given to the subject. It uses attributes
of the subjects such as subject’s name, age or role in organization and attributes of objects such
as metadata properties to provide authorizations. The permissions in ABAC are depending on the
combination of set of subject and object’ attributes and their relative values.
ABAC overcome the user role assignment problem which exist in RBAC and focuses on
the attributes of a user required to grant access. It very flexible model that is considerably easier
to administer than RBAC. However, higher flexibility comes along with the higher complexity
due to the specification and maintenance of the policies. The numbers of subjects and objects in
healthcare systems is dynamically increased, which require maintained database containing all
attributes in same format.
Figure 15: Collaborative Resource and RoleC.
4 CONCLUSIONS AND FUTURE
WORK
In this work, an access control model was proposed
that is suitable for collaborative healthcare systems to
address the issue of information sharing and informa-
tion security. The aim is to provide a flexible access
control model without compromising the granularity
of access rights. The major contributions of this work
are as follows. First, the proposed model offers fine-
grained control of access rights granting. Healthcare
HEALTHINF 2016 - 9th International Conference on Health Informatics
220

providers are granted access only to the specific re-
source (patient records) instances that are bound to
work task execution. Secondly, WBAC corresponds
to the least privilege principle, whereby healthcare
providers are granted minimal access rights for car-
rying out duties, or tasks. Third, the WBAC model
ensures that access rights are dynamically adapted to
the actual needs of healthcare providers. Healthcare
providers can access the resources associated with a
work task, but only while the work task is active.
Once the work is completed the access rights are in-
validated.
4.1 Verification and Validation
The WBAC scheme will be further investigated at the
”Center for eHealth and Health Care Technology” at
the University of Agder. The plan is to formalize
the proposed event and policy, develop and proto-
type the functionality to be implemented as well as
evaluate the validity of the model. In order to eval-
uate the model’s validity, three main dimensions are
evaluated: security, efficiency and practicality. Secu-
rity refers to the model’s capacity to facilitate confi-
dentiality and integrity in healthcare systems. Prac-
ticality denotes the possible difficulties in managing
the model during actual implementation. Finally, ef-
ficiency is the model’s performance in terms of re-
source consumption, e.g. time. Moreover, the prob-
lems of inconsistency and incompleteness (Shaikh
et al., 2010; Aqib and Shaikh, 2014) of the access
control policy set will be validated and verified.
Formal specification and verification of WBAC
policies is important. We consider using linear tem-
poral logic (LTL) (Rozier, 2011) as formalism for
specifying WBAC policies. LTL allows a conve-
nient and concise formalism for specific policies as
well as used for verifying properties of reactive sys-
tems. In additions, NIST’s (National Institute of
Standards and Technology) generic model checking
technique (ACPT (Access Control Policy Testing))
(Hwang et al., 2010) will be used to model and ver-
ify policies during policy modeling to assures that
WBAC policies satisfy the security properties in-
tended by the model.
Use of formal methods, while important, cannot
verify usefulness and properties that are not captured
within the model and the formalism. We therefore see
formal verification as a necessary, but not sufficient,
condition for validation of WBAC in eHealth scenar-
ios.
The plan is also to analyze the insider threat in
the domain of healthcare information sharing and ex-
amine whether WBAC will perform effectively and
efficiently on identified threats. Furthermore, access
control policies, compliance and human factors will
be considered. The access control policies need to be
shaped and evaluated in term of their human impact
(Probst et al., 2010). The idea is how to define a set
of consistent access control policies related to human
behaviors, and fit it to healthcare processes and the
way people work, including in emergency situations.
ACKNOWLEDGEMENTS
We would like to thank the ”Center for eHealth and
Health Care Technology” at the University of Agder
for the support in investigating WBAC.
REFERENCES
Alhaqbani, B. and Fidge, C. (2008). Access control re-
quirements for processing electronic health records.
In Business Process Management Workshops, pages
371–382. Springer.
Alotaiby, F. T. and Chen, J. X. (2004). A model for team-
based access control (tmac 2004). In Information
Technology: Coding and Computing, 2004. Proceed-
ings. ITCC 2004. International Conference on, vol-
ume 1, pages 450–454. IEEE.
Alshehri, S., Mishra, S., and Raj, R. (2013). Insider threat
mitigation and access control in healthcare systems.
Alshehri, S. and Raj, R. K. (2013). Secure access control
for health information sharing systems. In Healthcare
Informatics (ICHI), 2013 IEEE International Confer-
ence on, pages 277–286. IEEE.
Aqib, M. and Shaikh, R. A. (2014). Analysis and compari-
son of access control policies validation mechanisms.
International Journal of Computer Network and In-
formation Security (IJCNIS), 7(1):54.
C
´
ordoba, J.-R. and Piki, A. (2012). Facilitating
project management education through groups as sys-
tems. International Journal of Project Management,
30(1):83–93.
Fabian, B., Ermakova, T., and Junghanns, P. (2015). Collab-
orative and secure sharing of healthcare data in multi-
clouds. Information Systems, 48:132–150.
Ferraiolo, D. F., Sandhu, R., Gavrila, S., Kuhn, D. R., and
Chandramouli, R. (2001). Proposed nist standard for
role-based access control. ACM Transactions on In-
formation and System Security (TISSEC), 4(3):224–
274.
Ferreira, A., Ricardo, C.-C., Antunes, L., and Chadwick, D.
(2007). Access control: how can it improve patients
healthcare? Medical and Care Compunetics 4, 4:65.
Gajanayake, R., Iannella, R., and Sahama, T. (2014).
Privacy oriented access control for electronic health
records. electronic Journal of Health Informatics,
8(2):15.
Towards an Access Control Model for Collaborative Healthcare Systems
221

Georgiadis, C. K., Mavridis, I., Pangalos, G., and Thomas,
R. K. (2001). Flexible team-based access control us-
ing contexts. In Proceedings of the sixth ACM sym-
posium on Access control models and technologies,
pages 21–27. ACM.
Hu, V. C., Ferraiolo, D., and Kuhn, D. R. (2006). Assess-
ment of access control systems. US Department of
Commerce, National Institute of Standards and Tech-
nology.
Hu, V. C., Ferraiolo, D., Kuhn, R., Schnitzer, A., Sandlin,
K., Miller, R., and Scarfone, K. (2014). Guide to at-
tribute based access control (abac) definition and con-
siderations. NIST Special Publication, 800:162.
Hwang, J., Xie, T., Hu, V., and Altunay, M. (2010). Acpt:
A tool for modeling and verifying access control poli-
cies. In Policies for Distributed Systems and Networks
(POLICY), 2010 IEEE International Symposium on,
pages 40–43. IEEE.
Kayem, A. V., Akl, S. G., and Martin, P. (2010). Adaptive
cryptographic access control, volume 48. Springer
Science & Business Media.
Koufi, V. and Vassilacopoulos, G. (2008). Context-aware
access control for pervasive access to process-based
healthcare systems. Studies in health technology and
informatics, 136:679.
Le, X. H., Doll, T., Barbosu, M., Luque, A., and Wang,
D. (2012). An enhancement of the role-based access
control model to facilitate information access manage-
ment in context of team collaboration and workflow.
Journal of biomedical informatics, 45(6):1084–1107.
Majumder, A., Namasudra, S., and Nath, S. (2014). Tax-
onomy and classification of access control models for
cloud environments. In Continued Rise of the Cloud,
pages 23–53. Springer.
Moonian, O., Cheerkoot-Jalim, S., Nagowah, S. D., Khedo,
K. K., Doomun, R., and Cadersaib, Z. (2008).
Hcrbac–an access control system for collaborative
context-aware healthcare services in mauritius. Jour-
nal of Health Informatics in Developing Countries,
2(2).
Motta, G. H. and Furuie, S. S. (2003). A contextual role-
based access control authorization model for elec-
tronic patient record. Information Technology in
Biomedicine, IEEE Transactions on, 7(3):202–207.
Oh, S. and Park, S. (2003). Task–role-based access control
model. Information systems, 28(6):533–562.
Probst, C. W., Hunker, J., Gollmann, D., and Bishop, M.
(2010). Insider Threats in Cyber Security, volume 49.
Springer Science & Business Media.
Rozier, K. Y. (2011). Linear temporal logic symbolic model
checking. Computer Science Review, 5(2):163–203.
Rubio-Medrano, C. E., D’Souza, C., and Ahn, G.-J. (2013).
Supporting secure collaborations with attribute-based
access control. In Collaborative Computing: Net-
working, Applications and Worksharing (Collaborate-
com), 2013 9th International Conference Conference
on, pages 525–530. IEEE.
Russello, G., Dong, C., and Dulay, N. (2008). A workflow-
based access control framework for e-health applica-
tions. In AINAW 2008-Workshops. 22nd International
Conference on, pages 111–120. IEEE.
Samarati, P. and Di Vimercati, S. D. C. (2001). Access con-
trol: Policies, models, and mechanisms. Lecture notes
in computer science, pages 137–196.
Shaikh, R. A., Adi, K., Logrippo, L., and Mankovski, S.
(2010). Inconsistency detection method for access
control policies. In Information Assurance and Se-
curity (IAS), 2010 Sixth International Conference on,
pages 204–209. IEEE.
Shen, H. and Dewan, P. (1992). Access control for collabo-
rative environments. In Proceedings of the 1992 ACM
conference on Computer-supported cooperative work,
pages 51–58. ACM.
Thomas, R. K. (1997). Team-based access control (tmac):
a primitive for applying role-based access controls in
collaborative environments. In Proceedings of the
second ACM workshop on Role-based access control,
pages 13–19. ACM.
Tolone, W., Ahn, G.-J., Pai, T., and Hong, S.-P. (2005). Ac-
cess control in collaborative systems. ACM Comput-
ing Surveys (CSUR), 37(1):29–41.
Ubale Swapnaja, A., Modani Dattatray, G., and Apte Sula-
bha, S. (2014). Analysis of dac mac rbac access con-
trol based models for security. International Journal
of Computer Applications, 104(5).
Verma, S., Kumar, S., and Singh, M. (2012). Comparative
analysis of role base and attribute base access control
model in semantic web. International Journal of Com-
puter Applications, 46(18).
Wang, W. (1999). Team-and-role-based organizational con-
text and access control for cooperative hypermedia en-
vironments. In Proceedings of the tenth ACM Confer-
ence on Hypertext and hypermedia: returning to our
diverse roots: returning to our diverse roots, pages
37–46. ACM.
Wen, Z., Zhou, B., and Wu, D. (2009). Three-layers role-
based access control framework in large financial web
systems. In Computational Intelligence and Software
Engineering, 2009. CiSE 2009. International Confer-
ence on, pages 1–4. IEEE.
Zhang, R. and Liu, L. (2010). Security models and re-
quirements for healthcare application clouds. In Cloud
Computing (CLOUD), 2010 IEEE 3rd International
Conference on, pages 268–275. IEEE.
HEALTHINF 2016 - 9th International Conference on Health Informatics
222
