
A Robust Multichannel Lung Sound Recording Device
Elmar Messner
1
, Martin Hagm¨uller
1
, Paul Swatek
2
and Franz Pernkopf
1
1
Signal Processing and Speech Communication Laboratory, Graz University of Technology, Graz, Austria
2
Division of Thoracic and Hyperbaric Surgery, Medical University of Graz, Graz, Austria
Keywords:
Lung Sounds, Lung Sound Transducer, Air-Coupled Microphone, Multichannel Recording Device, Sound
Classification.
Abstract:
This paper presents a robust multichannel lung sound recording device (LSRD) for automatic lung sound
classification. Compared to common approaches, we improved the usability and the robustness against body
sounds and ambient noise. We developed a novel lung sound transducer (LST) and an appropriate attachment
method realized as a foam pad. For analogue prefiltering, preamplification, and digitization of the lung sound
signal, we use a composition of low-cost standard audio recording equipment. Furthermore, we developed a
suitable recording software. In our experiments, we show the robustness of our LSRD against ambient noise,
and we demonstrate the achieved signal quality. The LST’s microphone features a signal-to-noise ratio of
SNR = 80 dB. Therefore, we obtain a bandwidth of up to a frequency of f ≈ 2500 Hz for vesicular lung
sound recordings. Compared to the attachment of the LST with self-adhesive tape, the foam pad achieves
an attenuation of ambient noise of up to 50 dB in the relevant frequency range. The result of this work is
a multichannel recording device, which enables a fast gathering of valuable lung sounds in noisy clinical
environments without impeding the daily routines.
1 INTRODUCTION
Computer-aided lung sound analysis offers advan-
tages for medical diagnosis, such as digital stor-
age, monitoring in critical care settings, computer-
supported analysis, and comparison among different
sound recordings. Despite these advantages, it is far
away from being used in clinical settings. One rea-
son is the lack of efficiency and performance due
to the variability in the recordings (Reichert et al.,
2008; Gurung et al., 2011). Recently, lung sound
research mainly focused on the classification task.
Researchers either performed lung sound recordings
independently or used appropriate databases in their
experiments (Palaniappan et al., 2013). Sensors ap-
plied to lung sound recording are air-coupled mi-
crophones, contact sensors and modified stethoscope
chest pieces (Pasterkamp et al., 1993; Kraman et al.,
2006). The most common recording technique em-
ploys air-coupled microphones attached with self-
adhesive tape. This approach lacks of sensitivity
against body sounds and ambient noise (Zanartu et al.,
2009; Pasterkamp et al., 1999; Liu et al., 2013).
Moreover, for multichannel usage the attachment
of several lung sound transducers (LSTs) with self-
adhesive tape results in a poor usability and increases
the sensitivity against measurement errors.
In this paper, we introduce a robust lung sound
recording device (LSRD) to circumvent the afore-
mentioned drawbacks. It supports a reliable record-
ing of a high quality lung sound database for mul-
tichannel lung sound classification. To obtain clean
lung sound recordings, we focused on the recording
stage and reduced post-processing. Furthermore, it
was important that the LSRD is suitable to record
lung sounds for a large number of diseases. This
is reflected in the distribution and position of the
LSTs. Beside distinct adventitious lung sounds (So-
vijarvi et al., 2000), it should reliably allow the esti-
mate of changes in amplitude of lung sounds, which
is necessary for the detection of, e.g., pneumotho-
rax (Hayashi, 2011).
Based on the approach with air-coupled micro-
phones (Pasterkamp et al., 1993), we developed a
novel lung sound transducer ensuring a high signal
quality. For the attachment of the LSTs, we designed
a foam pad similar to the Stethographics STG 16
(Murphy, 2007). It records lung sounds in supine
position. We implemented the analog prefiltering,
preamplification, and digitization of the lung sound
signal with a composition of standard audio record-
ing equipment. The entire LSRD consists of the foam
34
Messner, E., Hagmüller, M., Swatek, P. and Pernkopf, F.
A Robust Multichannel Lung Sound Recording Device.
DOI: 10.5220/0005660200340039
In Proceedings of the 9th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2016) - Volume 1: BIODEVICES, pages 34-39
ISBN: 978-989-758-170-0
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

pad (our so called auscultation pad) and a pneumota-
chograph, both working with an appropriaterecording
software on a personal computer.
We organized the paper as follows. Section 2
presents our LST design and the auscultation pad.
Section 3 gives an overview on the remaining compo-
nents of the LSRD. The achieved signal quality and
the robustness against ambient noise is treated in Sec-
tion 4. Section 5 describes the measurement proce-
dure and Section 6 concludes the paper.
2 AUSCULTATION PAD
The core of our LSRD is the auscultation pad. It is a
foam pad with 16 LSTs distributed on its surface. We
adapted our LST design for this attachment method.
In the following subsections, we separately describe
the LST design and the foam pad.
2.1 Lung Sound Transducer
We developed a novel LST according to the ap-
proach with air-coupled electret-condenser micro-
phones (Pasterkamp et al., 1993). Figure 1 shows our
final LST. We use a Littmann Classic II chest piece
as coupler. We inserted an electret-condenser micro-
phone capsule (ECMC) in such a way that the stetho-
scope chest piece is acting as a conical coupler be-
tween the microphone capsule and the human skin.
The depth of the conical coupler is d = 2.2 mm, and
the width is w = 33 mm. Its shape corresponds to
the recommendations in (Wodicka et al., 1994; Kra-
man et al., 1995). We used the diaphragm of the
chest piece to cover its opening. It prevents the fill-
ing of the coupler cavity with skin, and, thus, it en-
sures its acoustic effect. This is important for varying
contact pressure, and, therefore, it is relevant for our
attachment method discussed in Section 2.2. The di-
aphragm further enables a convenient disinfection of
the LST, and it protects the ECMC from scratching
Sealing Ring
Diaphragm
Venting
Chest Piece
ECMC
Figure 1: Lung sound transducer consisting of an electret-
condenser microphone capsule (ECMC) inserted in a
Littmann Classic II chest piece.
body hair and dirt.
To allow static pressure equalization between the
coupler chamber and the surrounding air, we inserted
a small vent into the chest piece. We used a thin-wall
23-g needle with a length of l = 11.5 mm and with an
inner diameter of d = 0.35 mm, according to the rec-
ommendations in (Kraman et al., 1995). As ECMC,
we used the Primo EM172, which features a very high
signal-to-noise ratio of SNR = 80 dB and a sensitivity
of −27 dB (re 1V/Pa). These specifications are dis-
tinctly better than those of widely used microphones,
like the Sony ECM-44BPT (Sen and Kahya, 2006) or
the Sony ECM-77B (Dokur, 2009), which feature an
SNR ≤ 64 dB.
2.2 Pad
The attachment of the LST is a crucial part, because
of its high sensitivity against air- and tissue-borne
sounds (Zanartu et al., 2009; Pasterkamp et al., 1999).
Therefore, we developed a foam pad, the auscultation
pad shown in Figure 2. It consists of several foam lay-
6 cm
6 cm6 cm
7 cm
1 2
3
4
5 6
7
8
9
10
11 12
13
14
15 16
Figure 2: Arrangement of the lung sound transducers on the
auscultation pad. The center line represents the spine.
ers and a cover of artificial leather. The topmost lay-
ers holds the LSTs. There is a small cavity beneath
each LST, which avoids increasing contact pressure
due to the underlying foam. Furthermore, the cavity
prevents the foam from touching the venting of the
LST or even clogging it. By using different kinds of
foam, we designed a shape that adapts to almost ev-
ery physique. This construction provides a symmet-
ric contact pressure with respect to the spine. We ar-
A Robust Multichannel Lung Sound Recording Device
35

ranged the LSTs on the surface of the auscultation pad
with a fixed pattern, which almost matches the one
proposed in (Sen and Kahya, 2006). The pad enables
a fast attachment of the LST on the posterior chest by
simply placing the auscultation pad under the back of
the patient in supine position. To further stabilize the
patient, we extendedthe auscultation pad with two ad-
ditional pads, one for the head and another one for the
buttocks, as shown in Figure 3. We are able to achieve
a high robustness against body sounds and ambient
noise with an overall high lung sound signal quality.
Further details are presented in Section 4. The attenu-
ation of ambient noise is due to the surrounding foam.
We achieve the robustness against body sounds due to
the reliable attachment and almost no movement of
the back during breathing in the supine position. The
surrounding foam further prevents the interspersal of
body-borne noise in the LST cable. Another advan-
tage is the balanced audio connection from the aus-
cultation pad to the microphone preamplifiers, which
reduces the susceptibility to external noise.
3 REMAINING SETUP
COMPONENTS
We use the auscultation pad as part of a mobile
recording setup (Figure 3). The setup consists of an
equipment cart, which includes the recording hard-
ware, two screens, a pneumotachograph,and the pads.
The following subsections contain some details about
the remaining components.
Main Screen
Patient Screen
Auscultation Pad
Additional
Pads
Pneumotachograph
Figure 3: Mobile lung sound recording device containing
the auscultation pad and the remaining components.
3.1 Recording Hardware
We implemented the analogue prefiltering, preampli-
fication, and digitization of the lung sound signal with
low-cost standard audio recording equipment. The
composition of the appropriate hardware fulfills the
requirements of the CORSA guidelines (Vannuccini
et al., 2000).
We use two SM Pro Audio EP84 8-channel mi-
crophone preamplifiers with the integrated ADAT in-
terface SM Pro Audio PR8IIA. Beside the high-pass
filtering (cutoff frequency f
c
= 80 Hz, with a slope
of 18 dB/oct), the preamplification, and the analog-
to-digital conversion of the LST signal, the SM Pro
Audio PR8IIA provides the supply voltage (phantom
power) for the ECMCs. For the appropriate operat-
ing voltage of the ECMCs, we further use AKG MPA
VL phantom power adapters. They convert the phan-
tom power of 48V to the required 3V~10V. The AKG
MPA VL phantom power adapter features a high-pass
characteristic with a cutoff frequency of f
c
= 80 Hz
and a slope of 6 dB/oct. In a series-connection with
the microphone preamplifier, an overall high-pass
characteristic with a slope of 24 dB/oct is achieved.
The high-pass filters of the microphone preamplifiers
and the phantom power adapters are implemented as
Bessel filters. Therefore, they feature an approxi-
mately linear phase response. The two SM Pro Au-
dio EP84 are connected with an RME Fireface 800
audio interface. This represents a firewire multichan-
nel audio recording device for a computer. For the
lung sound recordings we use a sampling frequency
of f
s
= 16 kHz and a resolution of 24 Bit.
3.2 Pneumotachograph
The simultaneous recording of the velocity of respired
air and the lung sounds makes the distinction between
inspiratory and expiratory phases possible. Further-
more, we almost reach a uniform lung sound signal
intensity profile by specifying the respiratory behav-
ior of the patient, resulting in a high quality database.
We use a Schiller SP 260 pneumotachograph con-
nected via the USB port.
3.3 Recording Software
We developed a MATLAB GUI for the simultaneous
recording of the air flow and the lung sounds. Beside
the recording task, it enables the gathering of meta-
data and the clinical report.
We use Playrec for the multichannel recording of
the lung sound signals with MATLAB. For the flow
signal, we read the serial port of the pneumotacho-
BIODEVICES 2016 - 9th International Conference on Biomedical Electronics and Devices
36
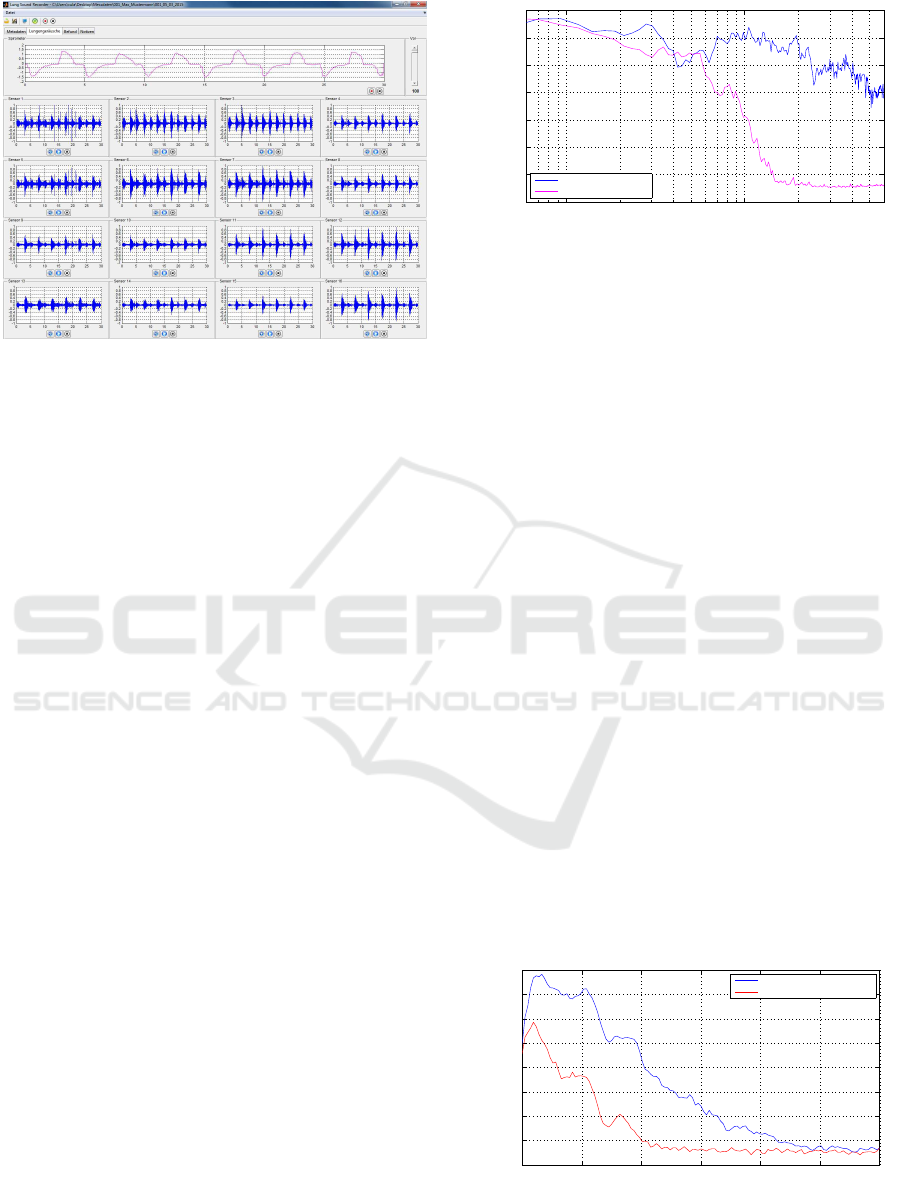
Figure 4: MATLAB GUI for the recording of the air flow
and the lung sounds signals.
graph. Figure 4 shows the main screen of the soft-
ware, featuring simultaneously recorded air flow and
lung sounds. Furthermore, we have a patient screen
to display the measured air flow in real time.
4 ROBUSTNESS AND SIGNAL
QUALITY
In this section, we show the achieved signal quality
by means of the SNR and the frequency range of the
recording setup. We further demonstrate the robust-
ness against ambient noise with a simple experiment.
4.1 Robustness Against Ambient Noise
The CORSA guidelines (Rossi et al., 2000) recom-
mend to have environmental condition with a back-
ground noise level of preferably < 45 dB(A) during
lung sound recordings. These requirements are not
always given in clinical setting.
We compared the performance of our auscultation
pad in a noisy setting with the attachment-method of
the LST with self-adhesive tape (Pasterkamp et al.,
1993). The experiment took place in a small room.
We considered two measurement scenarios. In the
first scenario we centered the auscultation pad on the
floor with a test person lying on it. In the second sce-
nario, we placed a chair in the center of the room, with
the test person in a sitting position.
With self-adhesive tape, we attach an LST on the
persons posterior chest, at the same position where it
was attached with the auscultation pad. The resid-
ual signal acquisition chain remained the same for
both scenarios, as introduced in Section 3. As noise
10
2
10
3
−120
−110
−100
−90
−80
−70
−60
−50
Frequency [Hz]
PSD [dB]
Self-adhesive tape
Auscultation pad
Figure 5: Attenuation of background noise of the ausculta-
tion pad compared to the attachment method of lung sound
transducers with self adhesive tape.
sources, we used five loudspeakers, which played
back white Gaussian noise. The loudspeakers fea-
ture a flat frequency responce from f = 80 Hz to
f = 20 kHz. We measured the A-weighted equiva-
lent sound level for both scenarios at the position of
the sensor over 30 seconds with L
Aeq
= 68 dB. During
the recording of the LST signal, we instructed the test
person to hold its breath for 15 seconds and played
back the white Gaussian noise.
Figure 5 shows the power spectral density (PSD)
for the LST signal in both scenarios in the relevant
frequency range. We see a distinct attenuation com-
pared to the attachment with self-adhesive tape, start-
ing above a frequency of f = 500 Hz. At a frequency
of f ≈ 2 kHz the difference is up to 50 dB.
4.2 Signal Quality
In Figure 6 we show the SNR of our recording setup
by illustrating the spectral characteristics of the vesic-
ular lung sound of a healthy adult person. The blue
line shows the spectral characteristics during the in-
spiratory phase. The red line shows the background
noise recorded at breath hold; the frequency compo-
nents in the low-frequency range are mainly caused
by body sounds.
0 500 1000 1500 2000 2500 3000
−120
−110
−100
−90
−80
−70
−60
−50
−40
Frequency [Hz]
PSD [dB]
Inspiratory lung sound
Background noise
Figure 6: Spectral characteristics of normal breath sounds
and background noise at breath hold, recorded at the poste-
rior chest of a healthy adult.
A Robust Multichannel Lung Sound Recording Device
37

We achieve a signal-to-noise ratio of up to SNR =
75 dB with an additional head room of around 5 dB.
Due to the high SNR value, we reach a bandwidth up
to a frequency of f ≈ 2500 Hz.
5 MEASUREMENT PROCEDURE
The lung sounds are recorded in the supine position
on an examination table. The auscultation pad is
placed under the back of the patient. For the orien-
tation of the patient on the pad, we use a defined dis-
tance between the the 7th cervical (C7) vertebra and
the topmost row of sensors. The patient is instructed
to lie quietly on the table and to breath with a max-
imum inspiratory flow of 1.5 l/s. This corresponds
to values used from the authors in (Jones et al., 1999;
Malmberg et al., 1995) and also the recommendations
in the CORSA standard (Vannuccini et al., 2000). The
recording time can be specified in the recording soft-
ware.
6 CONCLUSIONS
We developed a robust lung sound recording device
(LSRD), which reliably records a high quality lung
sound database for multichannel lung sound classifi-
cation. With preliminary measurements, we success-
fully underline the robustness of our newly designed
auscultation pad with respect to ambient noise. Com-
pared to the attachment of the LST with self-adhesive
tape, we achieve an attenuation of ambient noise of
up to 50 dB in the relevant frequency range. Due
to the high signal-to-noise ratio of our LST’s micro-
phone of SNR = 80 dB, we obtain a bandwidth of up
to f = 2500 Hz for vesicular lung sounds. For care-
fully performed measurements, our LSRD reduces
the post-processing to band-pass filtering and heart
sound reduction.
As future work, we plan to record a lung sound
database for several lung diseases. Furthermore, we
will focus on the classification of lung sounds.
ACKNOWLEDGEMENTS
This project was supported by the govern-
ment of Styria, Austria, under the project call
HTI:Tech
for Med. The authors acknowledge 3M
TM
for providing Littmann® stethoscope chest pieces
and Schiller AG for the support with a spirometry
solution.
REFERENCES
Dokur, Z. (2009). Respiratory sound classification by us-
ing an incremental supervised neural network. Pattern
Analysis and Applications, 12(4):309–319.
Gurung, A., Scrafford, C. G., Tielsch, J. M., Levine, O. S.,
and Checkley, W. (2011). Computerized lung sound
analysis as diagnostic aid for the detection of ab-
normal lung sounds: a systematic review and meta-
analysis. Respiratory medicine, 105(9):1396–1403.
Hayashi, N. (2011). Detection of pneumothorax visualized
by computer analysis of bilateral respiratory sounds.
Yonago acta medica, 54(4):75.
Jones, A., Jones, R. D., Kwong, K., and Burns, Y. (1999).
Effect of positioning on recorded lung sound intensi-
ties in subjects without pulmonary dysfunction. Phys-
ical Therapy, 79(7):682–690.
Kraman, S. S., Wodicka, G. R., Oh, Y., and Pasterkamp,
H. (1995). Measurement of respiratory acoustic sig-
nals. Effect of microphone air cavity width, shape, and
venting. CHEST Journal, 108(4):1004–1008.
Kraman, S. S., Wodicka, G. R., Pressler, G. A., and
Pasterkamp, H. (2006). Comparison of lung sound
transducers using a bioacoustic transducer testing sys-
tem. Journal of Applied Physiology, 101(2):469–476.
Liu, S., Gao, R. X., John, D., Staudenmayer, J., and Freed-
son, P. (2013). Tissue artifact removal from respira-
tory signals based on empirical mode decomposition.
Annals of biomedical engineering, 41(5):1003–1015.
Malmberg, L. P., Pesu, L., and Sovij¨arvi, A. (1995). Sig-
nificant differences in flow standardised breath sound
spectra in patients with chronic obstructive pulmonary
disease, stable asthma, and healthy lungs. Thorax,
50(12):1285–1291.
Murphy, R. (2007). Development of acoustic instruments
for diagnosis and management of medical condi-
tions. Engineering in Medicine and Biology Maga-
zine, IEEE, 26(1):16–19.
Palaniappan, R., Sundaraj, K., and Ahamed, N. U. (2013).
Machine learning in lung sound analysis: a systematic
review. Biocybernetics and Biomedical Engineering,
33(3):129–135.
Pasterkamp, H., Kraman, S., DeFrain, P., and Wodicka,
G. (1993). Measurement of respiratory acoustical
signals. Comparison of sensors. CHEST Journal,
104(5):1518–1525.
Pasterkamp, H., Wodicka, G., and Kraman, S. (1999). Ef-
fect of ambient respiratory noise on the measurement
of lung sounds. Medical & Biological Engineering &
Computing, 37(4):461–465.
Reichert, S., Gass, R., Brandt, C., and Andr`es, E. (2008).
Analysis of respiratory sounds: state of the art. Clini-
cal medicine. Circulatory, respiratory and pulmonary
medicine, 2:45.
Rossi, M., Sovijarvi, A., Piirila, P., Vannuccini, L., Dal-
masso, F., and Vanderschoot, J. (2000). Environmen-
tal and subject conditions and breathing manoeuvres
for respiratory sound recordings. European Respira-
tory Review, 10(77):611–615.
BIODEVICES 2016 - 9th International Conference on Biomedical Electronics and Devices
38

Sen, I. and Kahya, Y. (2006). A multi-channel device for
respiratory sound data acquisition and transient detec-
tion. In Proceedings of the 27th Annual International
Conference of the IEEE Engineering in Medicine and
Biology Society (EMBS’06), pages 6658–6661.
Sovijarvi, A., Malmberg, L., Charbonneau, G., Vander-
schoot, J., Dalmasso, F., Sacco, C., Rossi, M., and
Earis, J. (2000). Characteristics of breath sounds and
adventitious respiratory sounds. European Respira-
tory Review, 10(77):591–596.
Vannuccini, L., Earis, J., Helisto, P., Cheetham, B., Rossi,
M., Sovijarvi, A., and Vanderschoot, J. (2000). Cap-
turing and preprocessing of respiratory sounds. Euro-
pean Respiratory Review, 10(77):616–620.
Wodicka, G. R., Kraman, S. S., Zenk, G. M., and
Pasterkamp, H. (1994). Measurement of respira-
tory acoustic signals. Effect of microphone air cavity
depth. CHEST Journal, 106(4):1140–1144.
Zanartu, M., Ho, J. C., Kraman, S. S., Pasterkamp, H., Hu-
ber, J. E., and Wodicka, G. R. (2009). Air-borne and
tissue-borne sensitivities of bioacoustic sensors used
on the skin surface. IEEE Transactions on Biomedi-
cal Engineering, 56(2):443–451.
A Robust Multichannel Lung Sound Recording Device
39
