
Agent-based Modeling and Simulation Software Architecture
for Health Care
Karam Mustapha and Jean-Marc Frayret
Polytechnic University of Montreal, Mathematical and Industrial Engineering Department
2500, Chemin de Polytechnique, Montreal, H3T 1J4, Canada
Keywords: Health Care, Agent-based Simulation, Colon and Colorectal Cancer.
Abstract: Health Care (HC) organizational structure and related management policies are essential factors of HC sys-
tem. They can be tested through simulations in order to improve HC performance. To simplify the design of
these simulations we have proposed a modelling approach based on an additional structure. The modelling
approach considers the complexity of the modelling process, where in the various models are developed.
This approach is organized according to two main abstraction levels, a conceptual level and a simulation
level. We developed a computer simulation environment of patient care trajectories using the agent in order
to evaluate new approaches to increase hospital productivity and adapt hospital clinical practice conditions
for the elderly and patients with multiple chronic diseases. For that, we have developed a multi-agent
framework to simulate the activities and roles in a HC system. This framework can be used to assist the col-
laborative scheduling of complex tasks that involve multiple personals and resources. In addition, it can be
used to study the efficiency of the HC system and the influence of different policies.
1 INTRODUCTION
Health Care (HC) is a rich domain for multifaceted
simulation studies. The conceptual and architectural
modeling is challenging due to the diverse and com-
plex dimensions. In this domain, simulation general-
ly aims at experimenting and testing management
policies or organizational designs in a controlled
environment in order to understand their economi-
cal, human and environmental consequences. This
paper deals with the simulation of cancer patients’
pathways.
Almost 88% of the Canadian population over the
age of fifty1 (41 % women and 46 % men) will de-
velop some form of cancer during their lifetime.
Lung, breast, colon, rectal and prostate cancers rep-
resent more than half of all new cancer cases (52 %).
Colon and rectal cancers are the third most common
cancers among men and women and are considered
the second leading cause of cancer death among men
and the third among women.
With the aging population and the intricacy of
1
http://www.cancer.ca/~/media/cancer.ca/CW/cancer%20informat
ion/cancer%20101/Canadian%20cancer%20statistics/canadian-
cancer-statistics-2013-FR.pdf
the medical system, the management of HC activi-
ties has become increasingly complex. Therefore,
simulation is a relevant tool to model this complexi-
ty and improve its operations. In particular, agent-
based modeling and simulation significantly extend
the capabilities of simulation approaches such as
discrete-event simulation as discussed in the next
section.
Providing high-quality care is a priority among
health professionals. However, resources are limited
and their utilization must be optimized in order to
meet high quality standards and patients’ unique pro-
files. Therefore, the challenge faced by HC providers
and managers is to design organizational and medical
processes that deliver the right treatment, to the right
patient, at the right time using the right resources.
Factors, such as socio-demographic and environmen-
tal characteristics, as well as the characteristics of the
organizational and decision-making systems, can be
used to simulate patient care trajectories, from their
diagnosis to the end of the treatment.
In this paper, we propose to study the efficiency
of organization decisions which aims at: i) describ-
ing the HC organization; ii) modelling and simulat-
ing the behaviours and decisions of its actors and iii)
implementing these decisions and observe their local
Mustapha, K. and Frayret, J-M.
Agent-based Modeling and Simulation Software Architecture for Health Care.
DOI: 10.5220/0005972600890100
In Proceedings of the 6th International Conference on Simulation and Modeling Methodologies, Technologies and Applications (SIMULTECH 2016), pages 89-100
ISBN: 978-989-758-199-1
Copyright
c
2016 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
89

and global effect on the HC, and iv) supporting each
step with specific conceptual and software support.
This paper presents different objectives, the first
objective presented requires the agent-based model-
ling and simulation of complex behaviours, decision-
making processes and interactions between hospital
staff and patients. The most appropriate technology to
simulate these complex mechanisms is Agent-Based
modelling and Simulation (ABS). The second objec-
tive is therefore to create and validate the patient
agent model, which includes a physiological model of
how the cancer evolves in time in response to specific
treatments. Also, to simulate a large number of pa-
tients treated simultaneously with the same resources
of the hospital; this step of the project is only con-
cerned with the general behaviour of the patient agent,
and how well it can be configured in order to simulate
colon and colorectal cancer patients with different
attributes. As for third objective, healthcare decision
makers need reliable tools to support them in decision
making for adapting policies to help cut costs or re-
duce waiting time, and to provide visualization which
allows them to rehearse innovative ideas before they
are implemented.
Contributing to aforementioned objectives, we
aim to developing a computer simulation environ-
ment of patient care trajectories using the agent in
order to evaluate new approaches to increase hospi-
tal productivity and adapt hospital clinical practice
conditions for the elderly and patients with multiple
chronic diseases. Ultimately, the simulation model
will include: the physical health of the patient; the
cognitive state of the patient; the psychosocial state
of the patient; the hospital resources, staff and phy-
sicians. For that, we have developed a multi-agent
architecture to simulate the activities and roles in a
HC system. This architecture can be used to assist
the collaborative scheduling of complex tasks that
involve multiple personals and resources. In addi-
tion, it can be used to study the efficiency of the HC
system and the influence of different policies.
First, this paper describes the general scope of
this simulation project and presents an up to date
ABS. Next, the general conceptual model of the
simulation is described and finally simulation results
are presented.
2 LITERATURE REVIEW
Many research projects are based on the agent para-
digm to model and/or simulate complex systems.
Indeed, this paradigm provides a tailored approach
to model complex systems by explicitly addressing
the study of the interactions and behaviours of their
components. The design of HC agent-oriented mod-
els is a difficult task that requires the use of specific
knowledge and skills. This section defines ABS and
introduces a detailed analysis of ABS applications in
the medical domain. Finally, this section also pre-
sents different ABS development framework.
2.1 Agent-based Simulation
ABS is an abstract representation of reality that in-
volves the elaboration of a descriptive model, which
reproduces the behaviour of the system by modelling
its components, including their decision-making
capabilities and interactions patterns, as agents. An
agent can be defined as an entity, theoretical, virtual
or physical, capable of acting on itself and on the
environment in which it evolves, and capable of
communicating with other agents (Jennings et al.,
1998).
Research in ABS is prolific. It is known under
different labels, including multi-agent simulation,
individual-based models and agent-based models.
These tools are part of a more generic technology
known as multi-agent systems; this domain of appli-
cations is much larger than simulation. In the litera-
ture, the concept of agent is generally defined as
(Jennings et al., 1998) "…a computer system situat-
ed in an environment, which is a way autonomous
and flexible to achieve the objectives for which it
was designed."
In practice, the multi-agent paradigm is used at
two levels: for modelling and for simulating. At the
first level, it is required to create multi-agent models
that (1) reproduce the naturally distributed structure
of the studied systems, or (2) propose a representa-
tion of complex problems. Such models can be used
for developing reactive, deliberative or hybrid agent
models. The second level involves the simulation
(i.e. experimentation with these models). Such a
simulation may or may not be based on distributed
software architecture. In other words, the operational
simulation model is not necessarily multi-agent. It
may be object-oriented or translated into other simu-
lation languages (e.g. DEVS) (Quesnel et al., 2007)
2.2 Agent-based Simulation in the
Health Care Domain
HC operation management is a domain that is well
suited to ABS because it involves many people in-
teracting with their own decision-processes. With
agent-based modelling, it is possible to explicitly
model these individuals and their interactions. How-
SIMULTECH 2016 - 6th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
90

ever, although ABS is growing in the medical do-
main, applications to the real world are still rare
((Nealon and Moreno, 2003), (Devi and Mago,
2005)).
In the medical domain, (Mustafee et al., 2010)
identifies 200 papers, in which simulation is used.
More than 70% of these applications used Monte
Carlo simulation, while 20% used Discrete-Event
Simulation, less than 9% used System Dynamics,
and finally only 1% used ABS.
For instance, (Stainsby et al., 2009) uses ABS to
reorganize hospital emergency departments. Recent-
ly, several simulation techniques have been used in
conjunction to capture different dimensions. (Knight
et al., 2012) use DES and ABS to model a healthcare
system, in which patients choose their hospital based
on a linear additive service function of three factors
(i.e., hospital reputation, travel distance, waiting
time). Finally, (Figueredo and Aickelin, 2011) pro-
poses one of the first systematic studies aiming at
comparing SD and ABS based on a simple mathe-
matical model of interactions between a tumour and
immune cells. The authors concluded that both mod-
elling paradigms are not always equivalent.
In most organizational simulations in the medical
field, agents, whether patients, doctors or nurses are
of reactive type and their behaviour is very specific
to the purpose of the simulation. In (Kazar et al.,
2008), the author discussed the introduction of a
multi-agent system into the medical field, which
helps the management take decisions and actions,
and also ensures the communication and coordina-
tion by reducing the errors of diagnosis and treat-
ment, and by improving time required for the medi-
cal resources, and other medical departments. How-
ever, (Kanagarajah et al., 2010) (Laskowski et al.,
2009) use simulation in order to analyse the perfor-
mance of an emergency department in different con-
figurations. In these studies, agents are used to mod-
el resources that move through the hospital with
predefined process time. In (Jones and Evans, 2008),
modelling deals mainly with the different types of
treatment associated with their time and resource
requirements, which then become predefined in the
simulation. Only patient’s arrival time and resource
availabilities change dynamically. In these models,
the agents travelling times within the hospital is pre-
defined. However, it can also be dynamically com-
puted in the simulation as in (Zhang and Yao, 2010),
which models the evacuation of a hospital undergo-
ing a fire, or in (Krizmaric et al., 2005) that use sim-
ulation to study different transport configurations for
clean and dirty equipment in the hospital.
Also, some authors proposed the concept of an
online medical service system for internet users using
a multi agent system, the user can get access to the
details of the closest and best health care system such
as hospital, medical clinic, etc. (Gupta et al., 2012).
However, (Han et al., 2006) used the medical sensor
modules with combinations of wireless telecommuni-
cation technology based in the multi-agent system.
The papers (Iantovics, 2008) (Gupta and Mukho-
padhyay, 2012), proposed a hybrid system with hu-
man and artificial agent members. (Gupta and
Mukhopadhyay, 2012) proposed an operational algo-
rithm to describe the operations of a hybrid multi
agent system based intelligent medical diagnosis sys-
tem called Clinical Diagnosis System (CDS) (Gupta
and Pujari, 2009). Also, (Mahmud et al., 2009) pre-
sented hybrid architecture of a multi-agent consulta-
tion system for obesity oriented health problems.
Some authors propose a multi-agent oriented
learning environment aimed at learning using a posi-
tive approach to perform diagnostic reasoning and
modelling of a domain (Rosa et al., 2003). In (Chao
and Wong, 2009), the authors proposed the model of
practical data mining diagnostic which intends to
support real medical diagnosis by two emerging
technologies - data mining (Zhang et al., 2005) and
multi-agent system (Foster et al., 2005)(Klusch et
al., 2003). In the next section we present the patient
agent models.
3 PATIENT AGENT MODELS
In the literature review, we have presented various
research based on the definition of methodologies to
guide the designers in the development of multi-
agent models in general. However they present a
number of weaknesses related to modelling HC, and
their simulation, for example, at present, there is no
generally accepted health care ontology for generat-
ing and analysis of medical or health care infor-
mation. This makes it difficult to communicate be-
tween several systems developed in different areas.
Also, other limitations related to the framework can
be synthesized by the following: (i) the absence of
an approach which ensures the passage of the con-
ceptual level to the implementation level; (ii) the
transition from design to implementation is costly in
time and development efforts; (iii) consideration of
the organization; (iv) multi-modelling and v) time
management.
In this study we proposed a modelling approach
based on an additional structure to consider the
complexity of the modelling process, where in the
various models is developed. The real system is first
Agent-based Modeling and Simulation Software Architecture for Health Care
91
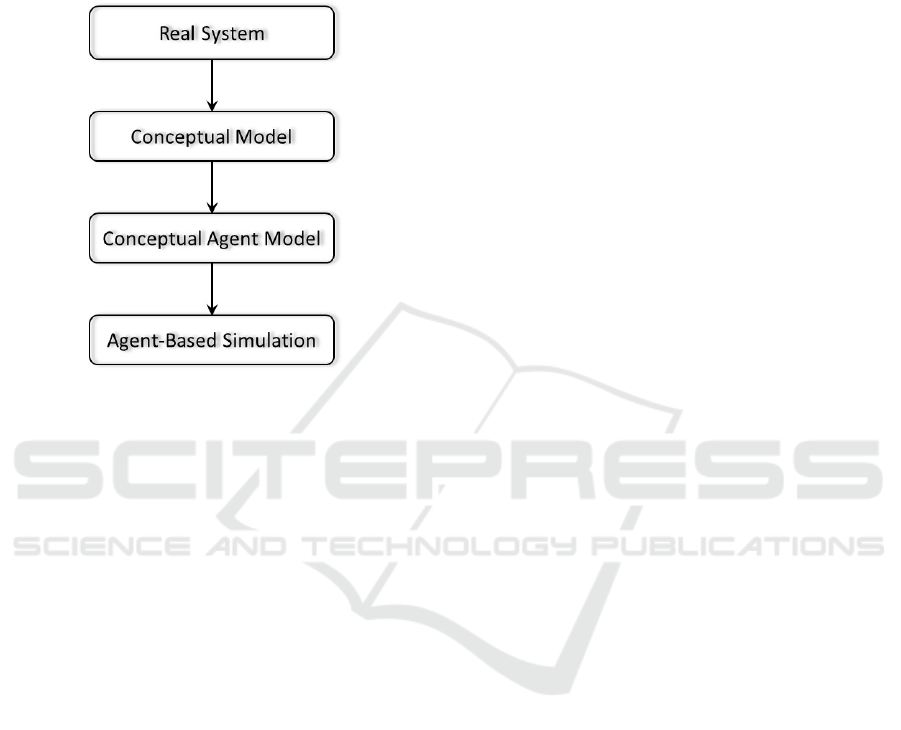
represented by the HC domain and then the overall
modelling approach is based on an incremental ap-
proach in which different models are developed. As
shown in Figure 1, the expert’s fields of intervention
are specified including different models: conceptual
modelling and simulation oriented agents.
Figure 1: A schematic of the Modelling Process.
In the process of modelling and simulation patient
trajectory, the model distinguishes three main steps:
the conceptual modelling, the conceptual agent
modelling, and operation modelling (Simulation
Oriented Agents - SOA).
The patient is the central actor of the HC system
or real system. It interacts with many resources, in-
cluding physicians, nurses and equipment. Its dy-
namic condition is the main driver of resource utili-
zation, and its reaction to treatment defines the sys-
tem quality level. In order to design such an agent,
different models are proposed to describe its place in
the overall system, and its complex behaviour.
Conceptual modelling is based on several mod-
els specifying the nature of the agents and the archi-
tecture of multi-agent system. In the following, it is
for the programmer to operationalize the conceptual
model agent. Each agent identified at the conceptual
level is specified and implemented according to the
constraints related to the development environment.
It is always for the programmer, to take into account
the technical constraints ignored at the simulation.
Thus, the multi-agent system will be deployed in a
software environment enabling its execution to con-
duct simulation experiments.
The conceptual modelling and conceptual agent
modelling are described next. With regard to operat-
ing step, it will be addressed in the next section on
the architecture simulation support.
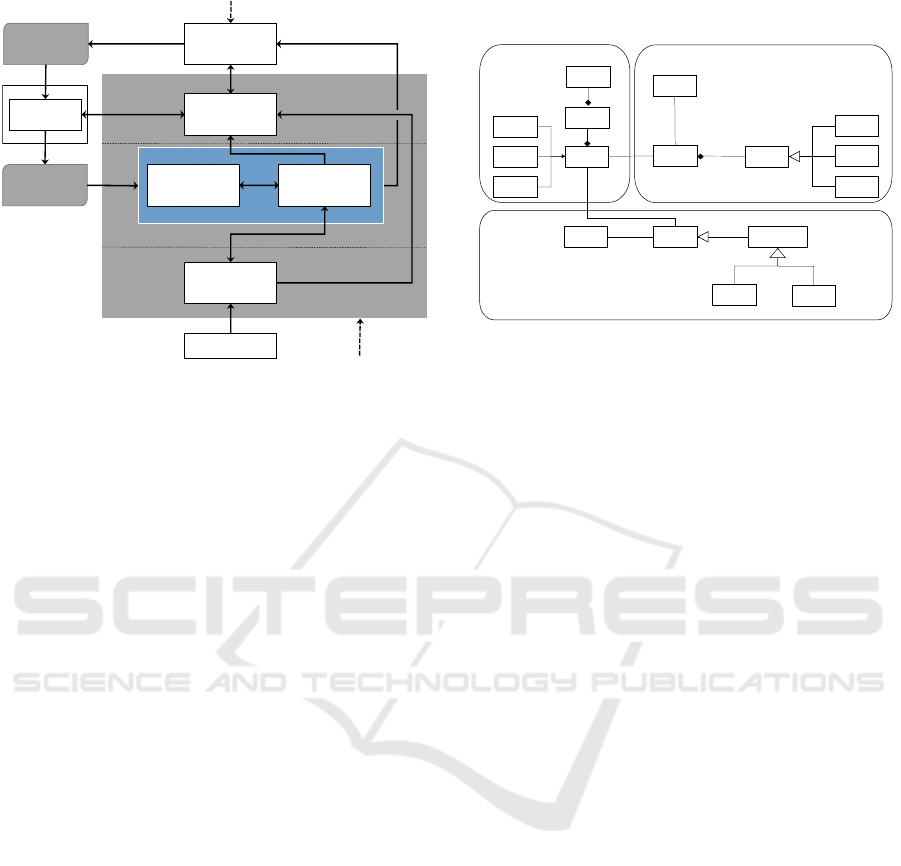
3.1 Conceptual Model
The general conceptual model proposed in this study
defines the main interactions between the patient and
its environment (Figure 2). It is composed of four
dimensions and includes different aspects of the
patient, its environment, and the HC system. These
dimensions are related to physiology of the patient,
the psychosocial state and support of the patient, the
decision processes and the resources used to treat the
patient. The links between the different aspects iden-
tified within these four dimensions represent their
mutual dependencies. The central part represents the
patient agent. The other parts represent the hospital
staff involved in the treatment selection, as well as
patient support (e.g., family members, nurses) (for
more details see the reference (Gilli et al., 2014)).
Psychosocial dimension: The psychological
dimension includes an emotional model of the pa-
tient agent and its social influences, especially in the
form of support from family members and nurses.
This model describes a response to specific situa-
tions and will eventually contribute to measuring the
patient quality of life during treatment.
Physiological Dimension: this dimension in-
cludes both the patient’s health model (its general
physical and health condition) and its cancer evolu-
tion model. Both are affected by treatment in differ-
ent manners, while influencing each other. In prac-
tice, this dimension includes on the one hand, the
absolute physiological state of the patient and can-
cer, and, on the other hand, the perception of this
state obtained from observations (e.g., analysis,
scans, and biopsies). While the initial information is
not necessarily known, the subsequent information
can be out-dated, and more or less accurate. Finally,
in this model, the patient health model is influenced
by his or her emotional model.
Decision Dimension: This dimension includes
both the patient’s and the physician’s decision mod-
els. It represents the main actors’ decision-making
processes and preferences that contribute to treat-
ment selection and treatment implementation. It is
the part of the conceptual model that directly con-
tributes to the decision and implementation of pa-
tient care trajectories. Here, the patient decision
model is influenced by its health and emotional
models, while the physician decision model is influ-
enced by the patient cancer and health models. The
patient decision model also contributes to plan each
individual treatment according to the system re-
source availabilities.
System Dimension: The system dimension rep-
resents the virtual hospital resources and processes.
SIMULTECH 2016 - 6th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
92
Treatment
plan
Resource
Model
Physician decision
model
Patient decision
model
Cancer evolution
model
Patient health
model
Patient emotional
model
Support
Treatment
implementation
Decision
Physiology
Psychosocial
Patient a
g
ent
Physician agent
System
Figure 2: General conceptual model.
When a physician requests a type of treatment,
it must be planned according to the hospital priority,
the workload of the resources required for this kind
of treatment, as well as the preferences of the pa-
tient. The different sub-models of these dimensions
influence each other in order to emulate the general
relationships between the patient, his/her cancer, the
medical staff, and the patient's support. The relation-
ship between the patient and the hospital processes
and resources are addressed through the dynamic
specification of the treatment program into the care
trajectories, which defines how the patient interacts
with the different resources for his/her treatment and
tests/scans. The next section focuses on the concep-
tual agent model.
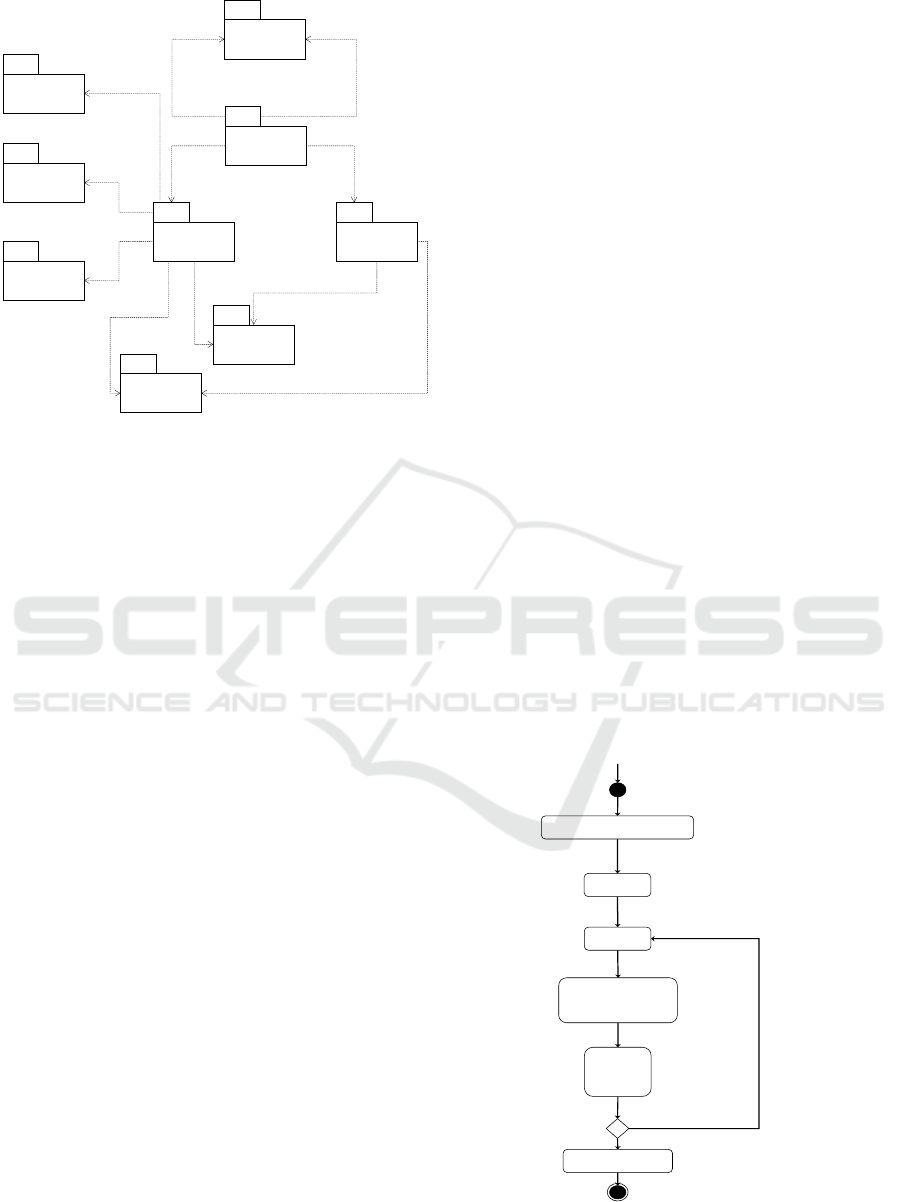
3.2 Conceptual Agent Model
The conceptual agent model must determine a num-
ber of properties of the previous conceptual model.
Focusing mainly on aspects of design and analysis,
the conceptual agent model integrates the major
concepts of agent, role, service and relationship,
defined as:
The agent is an active entity of the environment;
The role is played by the concept of an agent;
A service is a function performed by an agent;
A relationship is an interaction between entities.
The concepts behind the conceptual agent mod-
el are defined through a meta-model. This meta-
model defines as precisely as possible all the con-
cepts involved in a conceptual agent model and se-
mantic relationships. The conceptual agent meta-
model is formalized by the UML class diagram
shown in Figure below.
Environment
Agent
*
1
Reactive
Deliberative
Hybrid
Role
*
*
Service
Physician
Patient
Nurse
*
*
Informational
Simple
Complex
Active entities
Interaction
Role Description
Behavior
*
1
Interactionprotocol
*
*
1
Tas k
*
*
1
Figure 3: Conceptual agent model.
In this conceptual model an agent plays different
roles. The same role can be played by several agents.
A role provides services, while a service may require
a task. Relationships can develop between roles.
There are two sub-types of interactions, simple and
complex interactions (informational). The simple rela-
tionship is an exchange of information to complete
tasks, the distribution of tasks or the sharing of
knowledge and the complex relationship for example
assumes that agents must coordinate their actions in
order to combine their skills to solve complex tasks.
An interaction composed protocol. Finally, there are
several types of agents: reactive (If the simple behav-
iour is required, a type of stimulus-response behav-
iour is sufficient), deliberative (If decision making
and negotiation are needed, it will be the capacities of
a deliberative agent to perceive its environment and
the behaviour of other agents), hybrid (Reactive be-
haviour and deliberative behaviours are needed. For
example, an agent "smart" capable of interacting with
another agent when disruptive events occur). In the
next section we present the Simulation of Care Path-
ways for Patients (SiCaPP).
4 SIMULATION
METHODOLOGY (SICAPP)
The objective of this section is to present the soft-
ware solution restraint to accompany the process
design and Simulation of Care Pathways for Patients
(SiCaPP) for colon and rectal cancer treatment by
integrating the functional and software requirements,
and based on multi-agent modelling.
SiCaPP represents an implementation solution for
the conceptual agent model and is characterized by:
Agent-based Modeling and Simulation Software Architecture for Health Care
93

Specification, the agents’ behaviour in appro-
priate languages to the granularity of agents, it
is to describe how the agent should behave dur-
ing the simulation without prejudging how they
will actually be implemented (language pro-
gramming, simulation language, environment,
etc.)
The specification of interactions between
agents which results in dynamic simulation.
These interactions will have different imple-
mentation issues that are involved as agents of
a same environment.
The simulation environment aims both to facilitate
the handling of models and supervise their imple-
mentation in order to exploit their results. To support
the simulation design process different conceptual
software needs should be treated. These needs can
be summarized into two main categories:
Needs related to the field study of HC
As mentioned in the previous section, the HC
complex systemimpose many constraints. It in-
volves modelling and simulating the system ac-
cording to their decision-making level and opera-
tional implementation. In fact, the processes na-
ture, calculations or decision-making implement-
ed processes method requires a large variability
of representation behavioural of entities in a HC.
This is translated by expressed models in adapted
modelling languages, which must be possible to
integrate, that is to say make or consistently
maintain at a conceptual and simulation level.
The multi-agent paradigm seems affordable.
Needs related to simulation
The nature of the simulation of HC, as well as
taking into account the foregoing need, leads to a
distributed simulation load on one or more simu-
lators. Since the simulation word is set, the time
issue becomes unavoidable and is necessary in a
simulator. We need to synchronize the agents in
the simulator to avoid inconsistent behaviour of
the simulation as a whole and therefore the re-
sults of simulations erroneous (Fujimoto, 2000).
This problem is not specific to the simulation of
HC and has already been posed.
5 SICAPP ARCHITECTURE
SiCaPP architecture presents different services,
these services includes the following information:
agents’ management, time management, and inter-
agent communication.
The agents’ management provides all the func-
tions needed to manage the life cycle of agents ad-
dressing, functions such as launch and stop. It allows
for example, adding, changing, or deleting the
agents dynamically, it maintains a directory of these
agents taking particular account of the simulator in
which they operate. Secondly, the inter-agent com-
munication presents different communication lan-
guages like ACL message and provides the commu-
nication between agents in the environment. It can
also manage a directory like yellow pages integrat-
ing information on the capabilities and/ or agent
played roles of the simulation. Finally, the time
management is rarely mentioned in mutli-agent, of
the fact that the distributed nature of the simulation
is often more conceptual than software. Thus, time
management is implicitly centralized on the reactive
multi agent system and is not managed in the delib-
erative systems if not in relative terms.
In this architecture, we also define a different role
that includes the following information:
A set of actions that can be performed, i.e. a pa-
tient role is to approve action prescribed by
physician.
A set of protocols, which describe how this role
should interact with other roles.
A set of goals.
The SiCaPP system is organized into different
packages (Figure 4), packages include:
User interface: It is a GUI-based logic which
enables the user to generate, simulate patients
and show simulation results graphically.
Database: It is used to register generated pa-
tients and the simulation results.
Patient population: It generates patient’s popu-
lation; this information includes aspects of a
patient’s personnel information and physical
health such as treatment plan, medication and
diagnosis.
Patient simulation: Controlled by physicians
who decide whether diagnostics are to be ac-
cepted, perform medical and surgical interven-
tions, provide prescriptions, and perform
chemotherapy and radiotherapy treatment in
collaboration with nurse.
Treatments protocols: It describes a method to
be used during the treatment (e.g. drug, medi-
cal treatment) or a medical research study.
Treatment plan: This package is used to choose
a treatment trajectory plan for patients based
on the epidemiological studies and real data.
SIMULTECH 2016 - 6th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
94
UserInterface
PatientPopulation
DataBase
PatientSimulation
TreatmentProtocols
EquationMethods
Gompertz and
Iwata
ClinicalProfil
Graphiccal/Results
Access
Access
Access
Access
Access
Access
Access
Access
Access
Access
TreatmentPlan
Access
Figure 4: SiCaPP Architecture Diagram.
Equation methods: it contains different sets of
mathematical equations used in our model,
e.g. gompertz model which describes the evo-
lution of the main tumour from the appearance
of the first cancerous cell to a larger tumour,
iwata (Iwata et al., 2000) (Gilli et al., 2014)
model which is used to describe the evolution
of metastases.
Clinical profile: It is used to check the physical
and psychological state of the patient, it is
based on different notions e.g. depression, sta-
tus performance, sleep disturbance and fa-
tigue. We are using the epidemiological stud-
ies and Jewish Hospital real data.
6 SICAPP KERNEL
Medical information of a patient is one of the most
sensitive types of information; this information in-
cludes aspects of patient’s personnel information
and physical health such as treatments, medicines
and diagnosis. A patient may be treated by any
number of physicians or nurses but they must all
belong in the team which is responsible for this pa-
tient. A physician can treat any number of patients
and maintain the medical history for each patient.
The patient is considered as a composed class to
calculate tumour evolution using mathematical mod-
els. Tumour growth is based essentially on popula-
tion-based models (Verga, 2010). Also this class is
used to verify the stage before and during the treat-
ment (diagnosis step). Each patient has a medical
profile; this profile contains a record of all treat-
ments used within the medical group. If the patient
has been treated in any facility within the same med-
ical group, we will have an existing patient record
and a medical history for the patient; this may need
to be updated. A treatment instance is created for all
patients admitted and updated throughout the pa-
tient’s stay. The treatment will subsequently be add-
ed to the patients’ medical record upon patient dis-
charge.
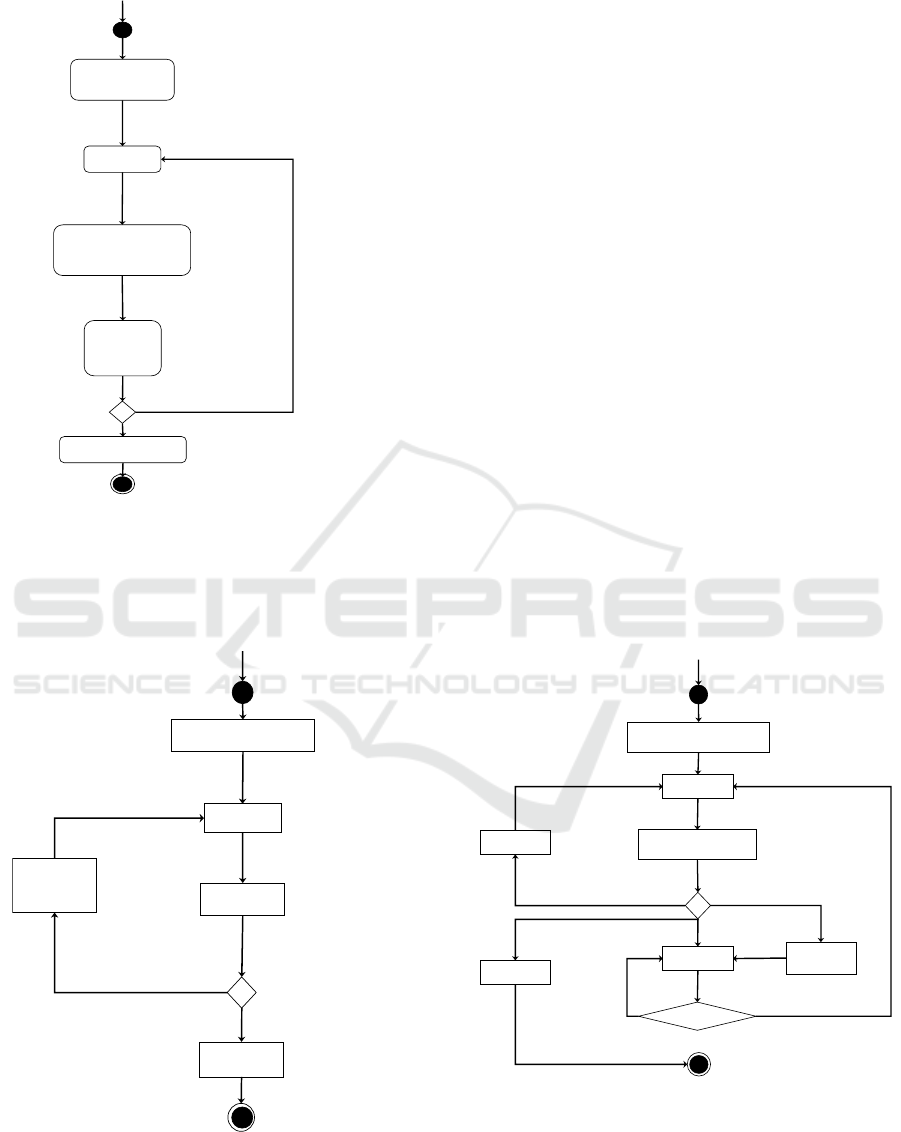
6.1 Generate Population of Patients
using SiCaPP
Based on epidemiological studies and the real data,
two different methods are used to generate the popu-
lation of patient. Figures below show a state chart
for the class to generate a virtual patient population.
Firstly this class generates the age and gender using
the epidemiological studies (Figure 5) alternatively
we can extract this information from real data
(Figure 6). Secondly, based on the age and gender
we choose the cancer type (two types are available:
colon and rectal) and stage. Alternatively we can
also extract this information from real data. Finally,
we use the gompertz model to determine the tumour
size in mm and we can calculate the stage using the
iwata model. If the stage obtained is different using
both models we have to re-determine the stage again
and repeat the same procedures. In case stage results
are matching, population generated is registered in
the data base.
Star
t
Generate Age and Gender using
epidemiological studies
Determine
Cancer Type
Determine
Stage
Calculate
Tumor Size
Using Gompertz Model
(Free evolution)
[If stage
obtained is
different the
generated
Stage]
Population registered
in the data base
[If no]
Verify the
stage
Using Iwata
Model
Figure 5: Generate population using the epidemiological
studies.
Agent-based Modeling and Simulation Software Architecture for Health Care
95
Start
Extract patient
information from
data base
Extract Stage
[If simulated
stage different
the Stage of
patient]
[If no]
Ver i f y t h e
stage
Using Iwata
Model
Access
Calculate
Tumor Size
Using Gompertz Model
(Free evolution)
Population registered
in the data base
Figure 6: Generate population using the real data.
6.2 Select Treatment Plan using
SiCaPP
Diagnosis
Treatment
Start
Extract Patient
Information
Patient
Proposition
Treatment
If patient accept the treatment
If no
Treatment
selected
Select a
Figure 7: Select treatment plan.
Figure 7 shows a state chart for the treatment class
which is responsible for generating a treatment plan
for each patient. This treatment is defined by the
physician. The patient has to perform some diagno-
sis which enables treatment plan choosing. When the
patient approves the treatment, the following infor-
mation must be stored in the generated file to be
used in the simulation step. In case the patient re-
jects the treatment, the physician has to choose an-
other type of treatment in collaboration with the
medical team and patient.
6.3 Treatment Trajectory using
SiCaPP
The figure below shows a state chart of class used to
treat patients who have colon or rectal cancer. This
treatment is created by the physician. First of all, the
patient should be examined prior each treatment or
session of treatments such as radiotherapy or chemo-
therapy. This is needed to evaluate the physical and
psychological state of this patient and determine the
stage of the cancer. After this evaluation the physi-
cian will be able to verify the patient’s ability to
continue treatment or suspend it for some period
until the patients state is re-evaluated or the treat-
ment is adjusted ( for example change the dose of
the medication). During treatment, the patient may
need to undergo more examinations if it is necessary
or if the physician has any concerns.
Exam
Evaluation
and determine stage
Start
Extract Patient and
Treatment Information
Suspend
Discharged
Treatment
Exam required?
Yes
No
Adjust
treatment
Figure 8: Treatment phase.
7 VA L I D AT I O N
The first objective was to validate our modelling and
SIMULTECH 2016 - 6th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
96
simulation oriented agents; the results of the simula-
tion are presented above in figure 8. These simula-
tions should allow us to validate our simulation plat-
form for executing further simulations that involve
treating patients with colon and rectal cancer. The
input data of the simulation and the results are stored
in a database, which was added into our simulation
platform.
To do that, we carried out different experiments,
using the Java eclipse software package with a
3,5GHz Intel Core i7 processor and 32 Go of RAM.
More specific, we used the JADE platform (Java
Agent Development Framework). JADE it’s a MAS
development environment complies with the FIPA
very diffused and included a set of tools included
facilitating various MAS development phases (Ri-
massa et al., 1999). The experiment aims at as-
sessing the ability of the model to replicate the re-
sults of real studies with specific treatment proto-
cols. In order to compare the simulation results with
actual data, we used the results for the real patients
after treatments. The treatments results are classified
by survived or not.
7.1 Experiment and Generate the
Virtual Population
In this experiment, we must calibrate the model’s
parameters. In order to do this ABS, we use the Jew-
ish Hospital real data, which allows us to validate
our model during the different type of treatment. The
real data include 773 patients who have colon and
colorectal cancer. However, among these patients
there are just 56 patients that have a complete pro-
file, more precisely that they have the stage, type of
treatments, and the results after treatments which
characterized by survived or not. Each of these pa-
tients have different types of information (or differ-
ent profile), like stage, age, cancer type, type of
treatment, and the protocol received by patients for
different treatments. Patients in the protocol received
two daily doses of chemotherapy treatment continu-
ously without rest periods.
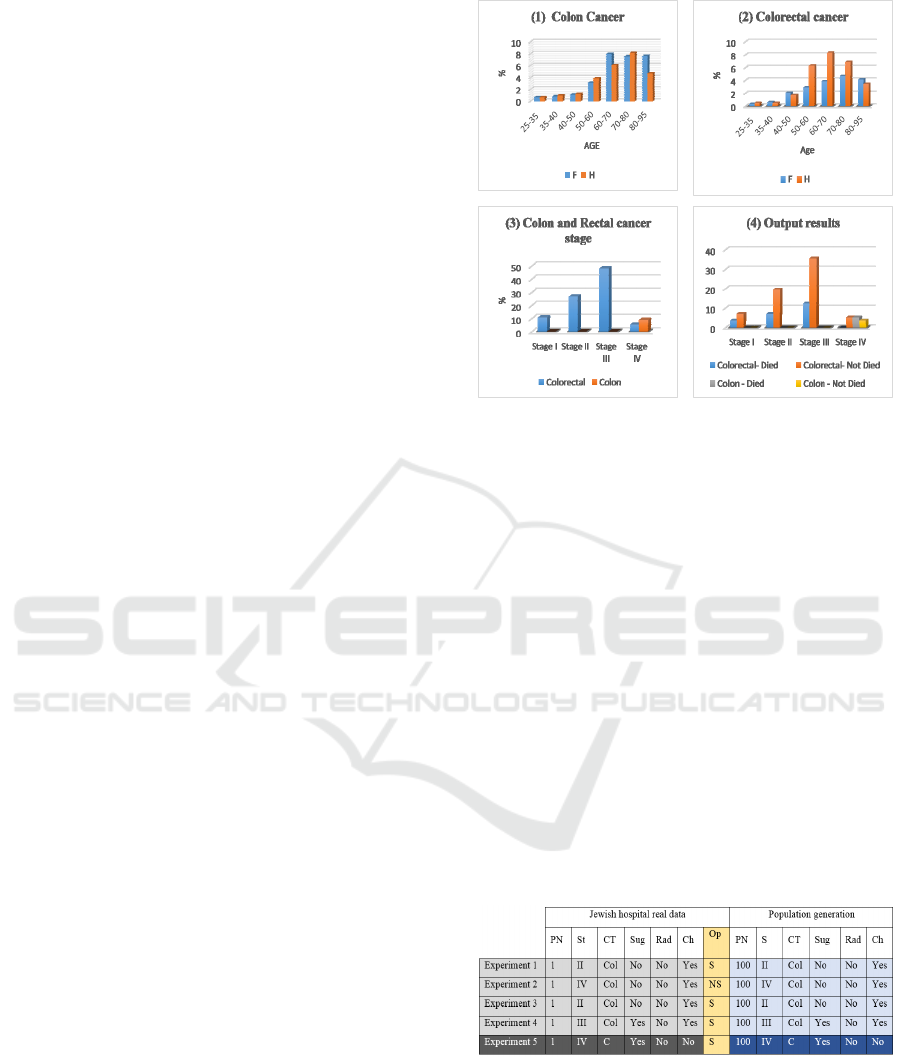
Figure 9 explains the contents presented in the
Jewish Hospital real data. Firstly we present the
percentage of patients (male and female) who have
Colon and Rectal Cancer in our real data, secondly
we present just the percentage of patients who have
a colon and rectal cancer with complete profile and
output results, and finally we present the percentage
of output results which is classified by Survived or
not.
To start our simulation, we must create several
populations of virtual patients based on the Jewish
Figure 9: Real Data Analyses.
Hospital real data. Firstly the user can be select
one real patient from the data base to generate the
following 100 virtual patients (or more) who have a
similar real patient profiles and same treatment plan.
During the generation of patient profiles we used the
Gompertz model which describes the evolution of
the main tumor from the appearance of the first can-
cerous cell to a larger tumor (we determine the stage
and the tumor size of the population generation).
Then, we use the iwata model to describe the evolu-
tion of metastases. In case the stage obtained and
real patient stages are matching, the population gen-
erated is registered in the data base and we can pre-
pare the simulation step. However, we must generate
the various parameters used by mathematics equa-
tions as Gompertz model and iwata model. The
model was calibrated for one protocol.
Table 1: Real data and Population generation information.
To validate our work, we select five patients with
different profiles to show the effectiveness of our
model. The table below represents the Jewish Hospi-
tal (patients selected) and the population generation.
This table presents the patient Number (P), the stage
(St), the type of cancer (CT: Colon (C) or Colorectal
(Col)), the different treatments (like surgery (Sug),
Radiotherapy (Rad) and Chemotherapy (Ch)) and
Agent-based Modeling and Simulation Software Architecture for Health Care
97
the Output results (Op) (Survived (S), or Not Sur-
vived (NS)). However, the real data and the popula-
tion generation have the same profile.
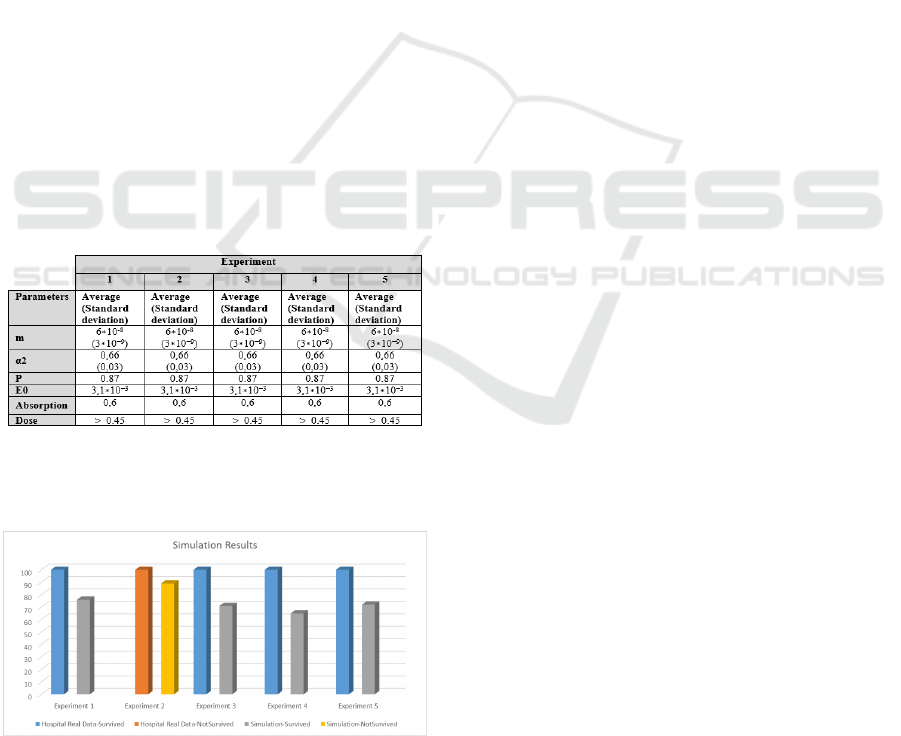
7.2 Calibration and Simulation Results
In order to calibrate the model for the configuration
of the real hospital data, we first need to estimate the
impact of each parameter on the results based on
their role in the model. For example, the percentage
of progressive disease is only defined by the pa-
rameter of the Gompertz evolution, the parameters
of the chemotherapy E0, and Absorption and Dose.
There are other parameters such as m, α and the
maximum and minimum size of the tumor in the
selection of the virtual population (Gilli, et al.,
2014). Thus, to calibrate the model, we proceed by
trial-and-error, using a dichotomy approach to set
each parameter and replicate the results of the hospi-
tal data as best as possible. Concerning the duration
of the simulated treatments, the median duration
reported in both studies was used for the correspond-
ing tests. The final values of the parameters for each
calibration are shown in Table 2. Concerning the
parameter Absorption, it has been set equal to its
defined in (Van Cutsem et al., 2000) value, while the
average value of α2 was taken in (Heun et al., 2011).
Table 2: Calibration Parameters.
In figure 10 below we compare our simulation
results with the results presented in the real hospital
data which are classified by survived or not.
Figure 10: Comparative analysis.
8 CONCLUSION AND FUTURE
WORK
The HCs is becoming increasingly complex. In the
search for their performance, modelling/simulation
becomes necessary. This modelling/simulation of
HCs needs multi-modelling with the use of different
formalisms or representation paradigms. The agent’s
oriented approach we showed to be relevant, includ-
ing the consideration of behaviour of various actors of
HC. Our research has focused on the definition of a
modelling approach for agent’s oriented simulation of
HC, with the main objective to allow a more organi-
zational modelling/agents oriented simulation of HC.
For this we have developed a simulation plat-
form for the implementation of the conceptual model
and implementation of multi-agent system. This
platform used a simulation platform based on a spe-
cific simulation environment (JADE). This simula-
tion allowed us to analyse the presented simulation
behaviour in the HC system. We have conducted
with our simulation platform several simulations of
the HC allowing the study of several relevant sce-
narios.
The validation phase described in this paper gives
very important results to reality reproduce, but it is
preliminary. Indeed, validation must be detailed with
more specific data for each patient and have a better
model calibrated than just on population averages,
before integration in the simulation platform. Thus,
validation with a more specific method, reflecting the
better use of the model in the simulation platform, is
required. This requires much more detailed data in the
treatment of each patient, to be provided by the Jew-
ish General Hospital in Montreal.
To complete the simulation platform, it will take
the next step in this focus on the most important part
will be the "Patient health model", because it will
determine the impact of patient treatment side ef-
fects that is an important aspect of treatment against
cancer. Indeed, the fight against cancer advanced by
chemotherapy can be seen as a balance between
enough drugs for reducing cancer, but not too much
to not kill the patient.
REFERENCES
Bernon C., Gleizes M. P., Picard G. and Glize P., 2002.
The Adelfe Methodology for an Intranet System De-
sign. In Proc. of the Fourth International Bi-
Conference Workshop on Agent-Oriented Information
Systems (AOIS), Toronto, Canada.
SIMULTECH 2016 - 6th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
98

Chao S. and Wong F., 2009. A Multi-Agent Learning
Paradigm for Medical Data Mining Diagnostic Work-
bench.
Devi M. S. and Mago V., 2005. "Multi-agent model for
Indian rural health care," Leadership in Health Ser-
vices, vol. 18, pp. 1-11.
Ferber J., Stratulat T. and Tranier J., 2009. Towards an
integral approach of organizations in multi-agents sys-
tems: the MASQ approach. Semantics and dynamics of
organizational models in Virginia Dignum.
Foster D., McGregor C. and El-Masri S., 2005. A Survey
of Agent-Based Intelligent Decision Support Systems
to Support Clinical Management and Research. In:
Proceedings of the 2nd International Workshop on
Multi-Agent Systems for Medicine, Computational Bi-
ology, and Bioinformatics, 16–34.
Figueredo G. P. and Aickelin U., 2011. "Comparing sys-
tem dynamics and agent-based simulation for tumour
growth and its interactions with effector cells," in Pro-
ceedings of the 2011 Summer Computer Simulation
Conference, pp. 52-59.
Fujimoto R., 2000. Parallel and distributed simulation
systems. John Wiley & Sons, Inc. USA.
Gaud N., Galland S. and Koukam A., 2008. Towards a
Multilevel Simulation Approach based on Holonic
Multi-agent. Published in the 10th International Con-
ference on Computer Modeling and Simulation
(EUROSIM/ UKSiM‟08), pp. 180–185, England. April
1–3.
Gilli Q., Mustapha K., Frayret J. M., Lahrichi N., and
Karimi E., 2014. Agent-Based Simulation of Colorec-
tal Cancer Care Trajectory: Patient Model. CIRRELT
(Interuniversity Research Centre on Enterprise Net-
works, Logistics and Transportation).
Gupta S., Sarkar A., Pramanik I., and Mukherjee B., 2012.
Implementation Scheme for Online Medical Diagnosis
System Using Multi Agent System with JADE.
Intemational Journal of Scientific and Research Publi-
cations, Volume 2, Issue 6,.ISSN 2250-3153, June.
Gupta S. and Mukhopadhyay S.. 2012 Multi Agent Sys-
tem Based Clinical Diagnosis Systm: An Algorithmic
Approach. International Journal of Engineering Re-
search and Applications (IJERA) ISSN: 2H8-9622.
Vol.2. Issue 5, pp. 1474-1477, September- October.
Gupta S. and Pujari S., 2009. A Multi-Aged: Based
Scheme for Heath Care and Clinical Diagnosis Sys-
tem, IAMA-09. ieeexplore. ISBN: 978-1-4244-4710-7.
July.
Han B-M., Song S.-J., Kyu Min Lee, Jang Kyung-Soo and
Shin Dong-Ryeol, 2006. Multi Agent System based
Efficient Healthcare Service. ICACT 2006, ISBN 89-
551 9-1 29-4.Feb. 20-22.
Heun J. M., Grothey A., Branda M. E., Goldberg R. M.,
and Sargent D. J., "Tumor status at 12 weeks predicts
survival in advanced colorectal cancer: Findings from
NCCTG N9741," The oncologist, vol. 16, pp. 859-867,
2011.
Hübner J. F., Sichman J. S., and Boissier O., 2007. Devel-
oping Organised Multi-Agent Systems Using the Moi-
se+ Model: Programming Issues at the System and
Agent Levels, Int. J. Accounting, Auditing and Per-
formance Evaluation, 1(3/4):370–395.
Iantovics B. 2008. The CMDS Medical Diagnosis System.
Ninth International Symposium on Symbolic and Nu-
meric Algorithms for Scientific Computing, IEEE.
Iwata K., Kawasaki K., and Shigesada N., 2000. "A dy-
namical model for the growth and size distribution of
multiple metastatic tumors," Journal of theoretical bi-
ology, vol. 203, pp. 177-186.
Jennings N. R., Sycara K., and M. Wooldridge, 1998. "A
roadmap of agent research and development," Autono-
mous agents and multi-agent systems, vol. 1, pp. 7-38.
Jones S. S. and Evans R. S., 2008 "An agent based simula-
tion tool for scheduling emergency department physi-
cians," in AMIA Annual Symposium Proceedings, p.
338.
Kanagarajah A., Parker D., and Xu H., 2010. "Health care
supply networks in tightly and loosely coupled struc-
tures: Exploration using agent-based modelling," In-
ternational Journal of Systems Science, vol. 41, pp.
261-270.
Kazar O., Sahnoun Z. and Frecon L.. 2008. Multi-agents
system for medical diagnosis. International Confer-
ence on Intelligent System and Knowledge Engineer-
ing, Vol. 1, Pages1265 – 1270.
Klusch M., Lodi S. and Moro G., 2003. The Role of
Agents in Distributed Data Mining - Issues and Bene-
fits. In: Proceedings of IEEE/WIC International Con-
ference on Intelligent Agent Technology (IAT’03),
211–217.
Knight V. A., Williams J. E., and Reynolds I., 2012.
"Modelling patient choice in healthcare systems: De-
velopment and application of a discrete event simula-
tion with agent-based decision making," Journal of
Simulation, vol. 6, pp. 92-102.
Krizmaric M., Zmauc T., Micetic-Turk D., Stiglic G., and
Kokol P., 2005. "Time allocation simulation model of
clean and dirty pathways in hospital environment," in
Computer-Based Medical Systems, 2005. Proceedings.
18th IEEE Symposium on, pp. 123-127.
Laskowski M., McLeod R. D., Friesen M. R., Podaima B.
W., and Alfa A. S., 2009. "Models of emergency de-
partments for reducing patient waiting times," PLoS
One, vol. 4, p. e6127.
Mahmud R., Aysa Abdul Halim Sithiq H., and Taharim H.
M., 2009. A Hybrid Technology for a Multi agent
Consultation System in Obesity Domain. World Acad-
emy of Science, Engineering and Technology.
Mustafee N., Katsaliaki K., and Taylor S. J. E., 2010.
"Profiling literature in healthcare simulation," Simula-
tion, vol. 86, pp. 543-558.
Nealon J. and Moreno A., 2003. "Agent-based applica-
tions in health care," in Applications of software agent
technology in the health care domain, ed: Springer,
pp. 3-18.
Picard G., 2004. Méthodologie de développement de sys-
tèmes multi-agents adaptatifs et conception de logi-
ciels à fonctionnalité émergente, thèse de doctorat,
Université Paul Sabatier de Toulouse III.
Agent-based Modeling and Simulation Software Architecture for Health Care
99

Quesnel G., Duboz R., Ramat E., and Traoré M.K., 2007.
VLE: A Multimodeling and Simulation Environment.
Proceedings of the Summer Simulation Multiconfer-
ence (SummerSim‘07), San Diego, California, USA,
July 15-18, pp. 367-374.
Rosa M. V., Cecilia D. Flores, Andre M. S., Louise J. S.,
Ladeira M. and Coelho H., 2003. A multi agent intel-
ligent environment for medical knowledge. Artificial
Intelligence in medicine, 335-366, Elsevier science
B.V.
Rimassa G., Bellifemine F., and Poggi A., JADE - A FIPA
Compliant Agent Framework, PMAA`99, p. 97-108,
Londres, 1999.
Stainsby H., Taboada M., and Luque E., "Towards an
agent-based simulation of hospital emergency depart-
ments," in SCC IEEE International Conference on
Services Computing, September 21, 2009 - September
25, 2009, Bangalore, India, 2009, pp. 536-539.
Verga F., 2010. "Modélisation mathématique de processus
métastatiques," Université de Provence-Aix-Marseille I.
Van Cutsem E., Findlay M., Osterwalder B., Kocha W.,
Dalley D., Pazdur R., et al., "Capecitabine, an oral
fluoropyrimidine carbamate with substantial activity in
advanced colorectal cancer: results of a randomized
phase II study," Journal of Clinical Oncology, vol. 18,
pp. 1337-1345, 2000.
Wooldridge M., Jennings N. and Kinny D., 2000. ‘The
Gaia methodology for agent –oriented analysis and de-
sign’, Autonomous Agents and Multi-Agent Systems,
vol. 3, n° 3, pp. 285-312.
Zambonelli F., Jennings N.R. and Wooldridge M., 2003.
‘Developing Multiagent Systems: The Gaia Method-
ology’, ACM Transactions on Software Engineering
and Methodology, vol. 12, n° 3, pp. 317-370.
Zhang W. and Yao Z., 2010. "A reformed lattice gas mod-
el and its application in the simulation of evacuation in
hospital fire," in IEEE International Conference on
Industrial Engineering and Engineering Management,
IEEM2010, December 7, Macao, China, pp. 1543-
1547.
SIMULTECH 2016 - 6th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
100
