
Computer-Aided Diagnosis for Endotracheal Intubation
Confirmation using Video-image Classification
Dror Lederman
Holon Institute of Technology, Holon, Israel
drorl@hit.ac.il
Keywords: Computer-Aided Diagnosis, Intubation Confirmation, Neural Networks.
Abstract: In this paper, a Computer-Aided Diagnosis (CAD) system for endotracheal tube position confirmation, and
detection of errors in intubation positioning is presented. Endotracheal intubation is a complex procedure
which requires high skills and the use of secondary confirmation devices to ensure correct positioning of the
tube. Our novel confirmation approach is based on video images classification and specifically on
identification of specific anatomical landmarks, including esophagus, upper trachea and main bifurcation of
the trachea into the two primary bronchi (“carina”), as indicators of correct or incorrect tube insertion and
positioning. Classification of the images is performed using a neural network classifier. The performance of
the proposed approach was evaluated using a dataset of cow-intubation videos and a dataset of human-
intubation videos. Each one of the video images was manually (visually) classified by a medical expert into
one of three categories: upper tracheal intubation, correct (carina) intubation and esophageal intubation. The
image classification algorithm was applied off-line using a leave-one-case-out method. The results show that
the system correctly classified 15
67 out of 1600 (97.9%) of the cow intubations images, and 349 out of the
358 human intubations images (97.5%).
1 INTRODUCTION
Intubation is a common medical procedure in
hospitals as well as in emergency medical units.
During intubation, a flexible tube is used to secure
passage of air to and from the lungs. The procedure is
performed by manually opening the mouth, lifting the
tongue using a device called laryngoscope in order to
reveal the vocal cords, and inserting an endotracheal
tube (ETT) through the vocal cords. The ETT should
be positioned between 2 and 5 cm above the
bifurcation of the trachea into the two primary
bronchi (“carina”).
The anatomy of the patient does not always allow
easy insertion of the ETT and consequently it might
be incorrectly positioned, usually either in the
esophagus or in the right main bronchus. Both of
these conditions can produce catastrophic results, as
the patient might be deprived of oxygen.
Unintentional esophageal intubation has been
associated with high mortality rate (Silvestri et al.,
2005; Timmermann et al., 2007). In cases of right
lung intubation (also termed one-lung intubation
(OLI)), only one lung is ventilated. Prolonged one
lung ventilation might cause serious pulmonary
complications such as collapse of the contralateral
lung and hyperinflation of the ventilated lung, which
might eventually result in hypoxia and
pneumothorax, respectively, and has been associated
with a significant increase in morbidity (Owen et al.,
1987; Zwillich et al., 1974) and Pneumonia (Wang et
al., 2009). Both esophageal and OLI may occur after
the ETT was positioned correctly (“dislodgement”)
from many reasons, for example, due to neck flexion
during general anesthesia (Vergese et al., 2004; Yap
et al., 1994).
Confirmation of correct tube positioning is a
challenging task. It requires high skills and the use of
secondary objective devices.
Numerous studies, which investigated
endotracheal misplacement rates in hospital and pre-
hospital settings, reported rates between 0% and 25%,
depending among others, on study design (Jacobs et
al., 1983; Jemmet et al., 2003; Jones et al., 2004; Katz
et al., 2001; Pointer, 1988; Silvestri et al., 2005;
Steward et al., 1984; Timmermann et al., 2007; Wang
et al., 2009).
In this paper, we present a computer-aided
diagnosis (CAD) system for endotracheal intubation
confirmation. The system is based on identification of
534
Lederman, D.
Computer-Aided Diagnosis for Endotracheal Intubation Confirmation using Video-image Classification.
DOI: 10.5220/0006200505340540
In Proceedings of the 6th International Conference on Pattern Recognition Applications and Methods (ICPRAM 2017), pages 534-540
ISBN: 978-989-758-222-6
Copyright
c
2017 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
specific anatomical landmarks as indicators of correct
or incorrect tube positioning.
Based on our previous preliminary work (e.g.
(Lederman, 2011)), we further developed and tested
our novel approach for automatic endotracheal
intubation confirmation. The approach is based on
direct visual cues, i.e., identification of specific
anatomical landmarks as indicators of correct or
incorrect tube positioning. In this study, the system
is further developed and evaluated using animal and
human tissue model.
The paper is arranged as follows. Section 2
reviews the relevant work in this field. Section 3
presents the proposed confirmation system. The
experimental results are presented in Section 3. The
results appear in Section 4, followed by discussion.
The conclusions appear in Section 5.
2 RELATED WORK
There are various methods and techniques for
endotracheal intubation confirmation. The most
common technique is auscultation to lung sounds
using a stethoscope. This technique requires high
attention, and its reliability has been questioned in
many studies (Brunel et al., 1989; Howells, 1985;
Klepper et al., 1993; Linko et al., 1983; Peterson et
al., 1973; Wang et al., 2006; Wodicka et al., 1994).
The use of exhaled carbon dioxide detection (CO2)
measurements (termed end-tidal CO2 (ETCO2)), has
become the gold standard-de-facto for confirming
correct tube positioning. However, the method has
been found to be unreliable in many emergencies
(Bhende et al., 1995; Gravenstein et al., 2004; Li,
2001; Nolan et al., 2005; Webb et al., 1993). In
addition, the method can not be used to detect OLI
incidents as in such cases the capnogram is generally
typical in shape and shows normal ETCO2 values
(Gravenstein et al., 2004; Webb et al., 1993). Other
techniques have been proposed (e.g., (Lederman,
2006; O'connor et al., 2005; Tejman-Yarden et al.,
2006; Tejman-Yarden et al., 2007; Weizman et al.,
2008)), but none of them has been proven effective.
Therefore, attempts to find the ultimate technique for
correct tube position confirmation have been
continued.
Our proposed approach is based on direct visual
cues, i.e., identification of specific anatomical
landmarks as indicators of correct or incorrect tube
positioning. In the following, we describe the method
and report its performance, evaluated using intubation
videos acquired on animals and human beings.
3 MATERIALS AND METHODS
The correct position of an ETT tip is 2-5 cm above
the carina. The image of the carina is therefore used
as the definitive anatomical landmark for confirming
correct endotracheal intubation. Hence, identifying
the carina in the acquired video images, and
discriminating between the carina and other
anatomical structures, is the main idea of the
proposed method. The method combines an artificial
neural network scheme which is employed in a
textural-based feature space. A general block diagram
of the proposed system appears in Figure 2.
3.1 The Video-stylet
Intubation is usually performed using an intubating
stylet, used to control and guide the ETT. We
designed and assembled a designated video-stylet.
The tip of the stylet comprises a miniature
complementary metal oxide silicon (CMOS) sensor.
The inner part of the stylet contains wires to transfer
the image and a narrow lumen to spray water or air in
order to clear blood and secretions away from the
camera sensor (Figure 1).
Figure 1: A schematic drawing of the video-stylet which
includes the stylet and complementary metal oxide silicon
(CMOS) sensor connected to a digital signal processor
(DSP).
The image sensor is connected to a processor with
an integrated image acquisition component. During
intubation, this rigid stylet is inserted into a standard
ETT with its camera at the tip. Video signals are
continuously acquired and processed by the
confirmation algorithm implemented on the
processor.
PC/
DSP
Stylet
CMOS
Air/water
lumen
Computer-Aided Diagnosis for Endotracheal Intubation Confirmation using Video-image Classification
535
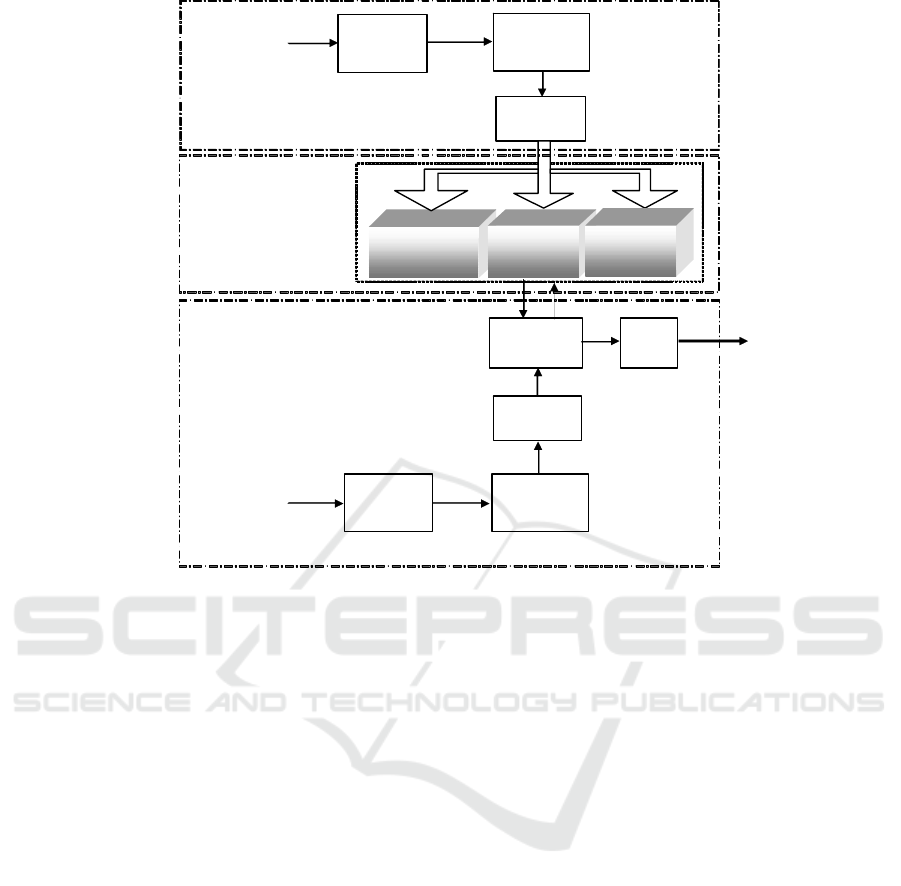
Figure 2: A general scheme of the proposed confirmation system. The system consists of three classes, one representing the
upper-trachea, one representing the carina and one representing the esophagus.
3.2 Pre-processing and Features
Extraction
The confirmation algorithm is based on classification
of specific anatomical landmarks, including the
carina, tracheal rings (upper trachea) and esophagus.
We use textural features (Haralick et al., 1973) that
contain important information about the structural
arrangement of surfaces and their relationship to the
surrounding environment. In particular, features
based on grey level co-occurrence matrices (GLCM)
are utilized. These features are based on the
assumption that texture information on an image is
contained in the overall or “average” spatial
relationship, which the grey tones in the image have
to one another. More specifically, it is assumed that
this texture information is adequately specified by a
set of grey tone spatial dependence matrices which
are computed for various angular relationships and
distances between neighboring resolution cell pairs
on the image. One of the advantages of these features
is that they are robust to imaging angles and scaling.
This property is of great importance to the task in
hand, as during intubation the tube may be inserted in
different angles and directions, depending on the
technique employed by the person performing the
procedure. It was therefore hypothesized that textural
features will allow reliable classification of the
images, independently of the angle at which the tube
was inserted.
A brief description of the textural features is now
given. Let
:*
f
Lx Ly I be an image with
dimensions
L
x and
L
y
, and grey levels
=0,1, , 1gG
. Let d be the distance (offset) between
two pixel positions
11
(,)
x
y
and
22
(,)
x
y
. Angles
quantized to
45
intervals are considered, such that
the neighbors of any pixel can lie on four possible
directions:
= 0 ,45 ,90 and 135
. A resolution cell is
considered to have eight nearest-neighbor resolution
cells. The co-occurrence matrix is constructed by
observing pairs of image cells at distance
d
from
each other and incrementing the matrix position
corresponding to the grey level of both cells. The un-
normalized frequencies for direction of
45
, for
instance, are defined by:
,
,,45
∘
=#{
,
,
,
∈
,
∗
,
|
−
|
=,
|
−
|
=−
−=−,−
=
,
,
=,
,
=
},
(1)
Upper Trachea
Model
Carina (TR)
Model
Feature
Extraction
Segmentation
to blocks
adaptation
Esophagus
Mod el
Identification
Decision
Memory
Single
-
frame Classification
Pre-
processing
Labeled images o
f
carina, vocal
cords and others
Training
Pre-
processing
Feature
Extraction
Segmentation
to blocks
Unknown ima
g
e
ICPRAM 2017 - 6th International Conference on Pattern Recognition Applications and Methods
536
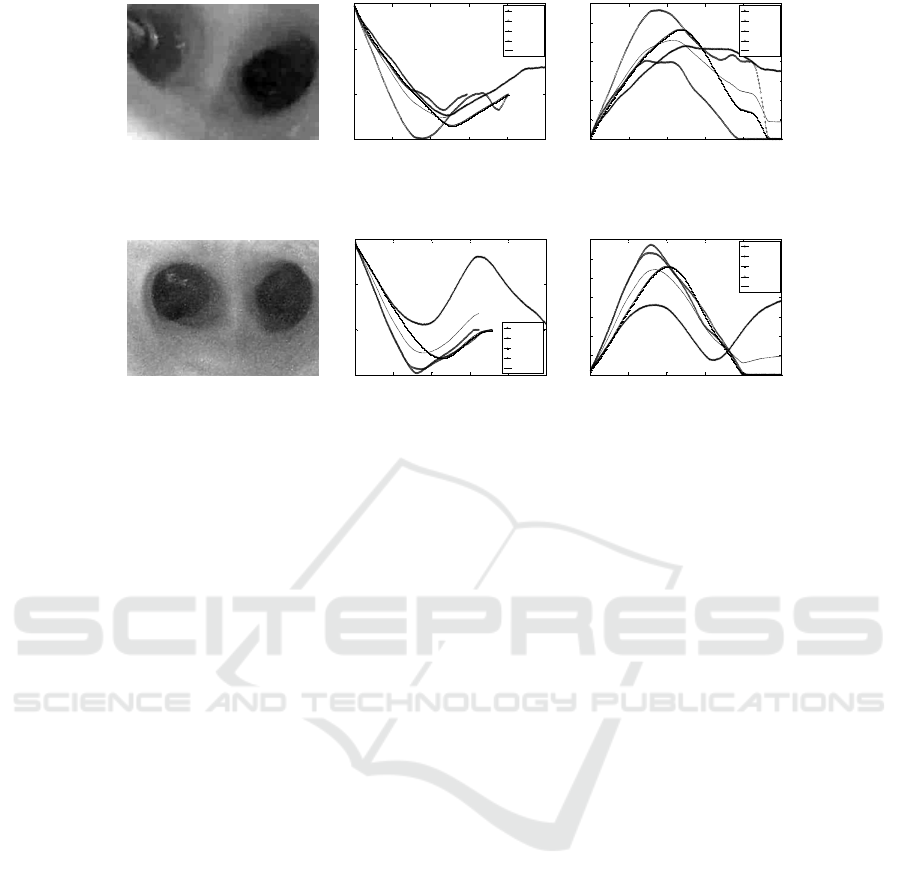
Figure 3: Two examples of carina images (left column) and the calculated textural features: correlation (middle column) and
contrast (right column).
where
#
denotes the number of elements in the set.
Measures of the other directions, as well as the
normalized measures, can be easily obtained
(Haralick et al., 1973).
To construct the feature set utilized in the
proposed system, various textural features were
extracted from the GLCM. Let
(, )
p
ij
denote the
(, )ij
th
entry in a normalized grey-tone spatial
dependence matrix, such that
(, ) (, )/
p
ij Pij R
,
where
R
is a normalization constant, which was set
in this work to the sum of all values of
(, )
P
ij
, i.e.,
11
=(,)
GG
ij
R
Pi j
, and
()
x
p
i
and
()
y
pi
denote the
i
th
entry in the marginal-probability matrix, obtained
by summing the rows and columns of
(, )
p
ij
,
respectively, i.e.
1
() (, )
G
x
j
pi Pij
,
1
(, )()
G
i
y
P
ijpj
. Then, the following features are
used to construct the feature set:
Contrast:
1
2
1
011
||=
=(,)
GGG
nij
ijn
fn pij
.
Correlation:
2
=1/ (,)
x
yxy
ij
fijpij
,
where
x
and
y
are the means,
x
and
y
are the
standard deviations of the marginal distributions
associated with
(, )pi j
.
Two information measures of correlation:
31
=/max{,}
f
HXY HXY HX HY
and
1/2
42
=1 exp 2.0fHXYHXY
, where
H
X
and
H
Y
are the entropies of
x
p
and
y
p
,
(, )log (, )
ij
H
XY p i j p i j
,
1
(, )log () ( )
xy
ij
HXY p i j p i p j
and
2
() ( )log () ( )
xy xy
ij
HXY p i p j p i p j
.
Maximal correlation coefficient:
1/2
5
second largest eigvenvalue of fQ
, where
(, ) (, ) ( , )/ () ( )
xy
k
Qi j pik p jk p ip j
.
The four values that each feature takes on in the four
directions are averaged to produce a rotation-
invariant feature which is employed by the
classification system. Figure 3 shows typical
examples of carina images and the corresponding
calculated features.
3.3 Classification
In order to classify the video frames, we utilized a
feed-forward artificial neural network classifier
(ANN) which consists of three layers. The first
(input) layer includes neurons that connect to selected
features, the second layer includes hidden neurons,
and the third (decision) layer includes one neuron that
generates a likelihood score of a test case belonging
to one of the three categories. To minimize over-
fitting and maintain robustness of the ANN
performance, a limited number of training iterations
(1000), and a large ratio between the momentum (0.9)
and learning rate (0.01), is used. The likelihood scores
obtained by the ANN classifier in leave-one-subject-
0 50 100 150 200 25 0
-0.5
0
0.5
1
Offset
Correlation
0 offset
45 offset
90 offset
135 offset
average
0 50 100 150 200 25 0
0
0.1
0.2
0.3
0.4
0.5
0.6
0.7
Offset
Contrast
0 offset
45 offset
90 offset
135 offset
average
0 50 100 150 200 25 0
-0.5
0
0.5
1
Offset
Correlation
0 offset
45 offset
90 offset
135 offset
average
0 50 100 150 200 25 0
0
0.1
0.2
0.3
0.4
0.5
0.6
0.7
Offset
Contrast
0 offset
45 offset
90 offset
135 offset
average
Computer-Aided Diagnosis for Endotracheal Intubation Confirmation using Video-image Classification
537
out tests are used to make the classification decision.
4 RESULTS
4.1 Classification of Cow Intubation
Video Images
In order to perform a preliminary evaluation of the
proposed system, we recorded two datasets. The first
dataset includes a total of 10 intubation videos that
were recorded from animal (cow) models, out of
which 1600 images were extracted, visually inspected
by a medical expert and classified into one of the
following categories: upper-trachea (490 images),
carina (550 images) and esophagus (560 images).
The second dataset includes 358 images, extracted
from intubations performed on 8 human subjects that
were downloaded from various web sites
1
. These
images were also categorized into the three categories
mentioned above.
Evaluation of the proposed approach was
performed using a leave-one-subject-out validation
method: in each iteration, the images extracted from
all videos (for a particular dataset) but one were used
to train the models, i.e. estimate the network
parameters, and the images from the remaining video
were used to test system performance. This process
was repeated such that each image participated once
in the testing phase.
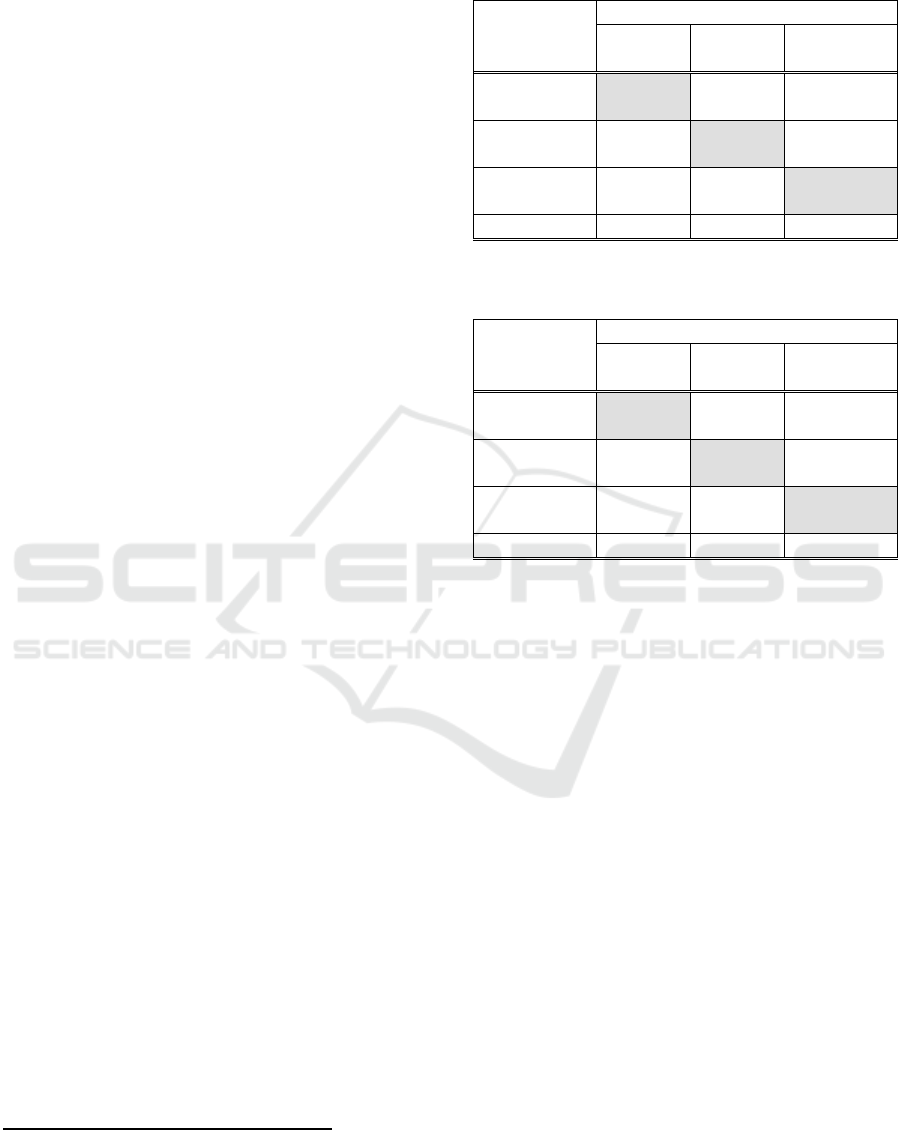
The classification results are summarized in
Tables 1 and 2, for the two datasets, respectively,
where the rows represent the predicted (recognized)
classes and the columns represent the actual classes.
The system achieved an overall classification rate of
97.9% (1567 out of 1600 images) for the cow
intubation database, and 97.5% (349 out of 358
images) for the human intubation database.
Specifically, most of the errors are due to
incorrect classification of carina images as upper-
trachea (e.g., 12 cases (2.2%), in the cow dataset and
2 cases (2%) in the human dataset), and incorrect
classification of upper-trachea images as carina and
esophagus (8 cases (1.7%), and 9 cases (1.8%),
respectively, for the cow dataset; 2 cases (1.05%), and
2 cases (1.05%), respectively, for the human dataset).
For both datasets, in two cases, an esophagus image
was mistakenly classified as either upper-tracheal or
carina.
1
University of Florida:
http://vam.anest.ufl.edu/airwaydevice/videolibrary/index.html
and http://www.youtube.com
Table 1: Summary of classification results for the cow
intubations dataset.
Recognized
Actual
Upper-
trachea
Carina Esophagus
Upper-
trachea
473
(96.5%)
12
(2.2%)
1 (0.2%)
Carina 8 (1.7%) 536
(97.5%)
1 (0.2%)
Esophagus 9 (1.8%) 2 (0.3%) 558
(99.6%)
Total 490 550 560
Table 2: Summary of classification results for the human
intubations dataset.
Recognized
Actual
Upper-
trachea
Carina Esophagus
Upper-
trachea
185
(97.9%)
2 (2%) 1 (1.5%)
Carina 2
(1.05%)
98
(97.0%)
1 (1.5%)
Esophagus 2
(1.05%)
1 (1.0%) 66 (97.0%)
Total 189 101 68
4.2 Discussion
A novel approach for automatic endotracheal
intubation confirmation was introduced. According to
the approach, direct physical determination of the
tube position with respect to the relevant anatomical
structures is performed based on image classification.
Images are represented using textural features which
are utilized by the ANN classifier. The proposed
scheme is simple and computationally efficient.
The proposed confirmation method was evaluated
using cow and human intubations videos, out of
which images were extracted and classified by a
medical expert into one of three categories: upper
tracheal, carina and esophagus. The method achieved
a high precision of 97.9% (1567 out of 1600 images)
using the cow intubations dataset, and 97.5% (349 out
of the 358 images) using the human intubation
dataset.
The method has a number of advantages over
existing endotracheal intubation confirmation
devices, including reliability in any medical
condition, suitability for both esophageal intubation
detection and one-lung intubation detection (although
not tested in this preliminary study), and the fact that
it is fully automatic and may be used, with a
designated endotracheal tube, for continuous and
ICPRAM 2017 - 6th International Conference on Pattern Recognition Applications and Methods
538

long-distance screening of tube misplacement and
dislodgment. The method can be easily integrated in
all patient monitoring systems. Moreover, the system
can be used to improve medical professionals
training.
The proposed method is computationally
efficient. Specifically, all of the algorithms used in
this work were implemented in Matlab R2016a 64bit.
Using a conventional PC equipped with Dual Intel
Xeon 3.4 GHz with a 16 GBytes of RAM, feature
extraction requires less than 1 second for each image.
Future improvements are the inclusion of other
anatomical landmarks, such as vocal cords, and the
development of a video-analysis algorithm, which are
expected to improve confirmation performances.
The results are encouraging, but clearly much
work is needed to further validate the proposed
approach. The available database consists of only 10
cow intubation videos and 8 human intubation videos.
A much larger database is required in order to reliably
validate system performance. Various factors might
challenge the system performance, especially fog and
secretions, which could result in poor image quality.
In addition, the effect of possible physiological
variability between patients on system performance is
yet to be evaluated.
Our ultimate goal is to develop a reliable, cost-
effective, easy to use and fully automatic device for
confirmation of correct tube positioning. For this
purpose, we plan to develop an advanced prototype,
which will be thoroughly evaluated in pre-clinical
trials and, upon receiving the appropriate regulatory
approvals, on humans. Based on this preliminary
study, we believe that implementation of the
proposed method into a real-time confirmation
system will lead to a major improvement in the ability
to detect intubation incidents as they occur, while the
patient is still well oxygenated and stable.
5 CONCLUSIONS
The ANN-based classification system achieved a
high precision of 97.9% and 97.5% for the cow and
human datasets, respectively. The results are
encouraging but as mentioned above, more research
is needed in order to reliably validate system
performance. With these challenges in mind,
successful implementation of the proposed method
into a real-time confirmation system can serve as a
major contribution to patient safety.
REFERENCES
Bhende, S. M., and Thompson, A. E., 1995. Evaluation of
an end-tidal CO2 detector during pediatric
cardiopulmonary resuscitation. Pediat., 95(3), 395-399.
Brunel, W., Coleman, D. L., and Schwartz, D. E., 1989.
Assessment of routine chest reoentgenograms and the
physical examination to confirm endotracheal tube
position. Chest, 96, 1043-1045.
Gravenstein, J. S., Jaffe, M. B., and Paulus, D. A., 2004.
Capnograhpy clinical aspects: Cambridge University
Press.
Haralick, R. M., Shanmugam, M., and Dinstein, I., 1973.
Textural features for image classification. IEEE Trans.
on Systems, Man, and Cybernatics, SMC-3(6), 610-621.
Howells, T. H., 1985. Oesophageal misplacement of a
tracheal tube. Anaesthesia, 40, 398-389.
Jacobs, L. M., Berrizbeitia, L. D., Bernnett, B., and
Madigan, C., 1983. Endotracheal intubation in the
prehospital phase of emergency medical care. JAMA,
250(2175-2177).
Jemmet, M. E., Kendal, K. M., and Fourre, M. W., 2003.
Unrecognized misplacement of endotracheal tubes in a
mixed urban to rural emergency medical services
setting. Acad. Emerg. Med., 10, 961-965.
Jones, J. H., Murphy, M. P., and Dickson, R. L., 2004.
Emergency physician-verified out-of-hospital
intubation: miss rates by paramedics. Acad. Emerg.
Med., 11, 707-709.
Katz, S. H., and Falk, J. L., 2001. Misplaced endotracheal
tubes by paramedics in an urban emergency medical
services system. Ann. Emerg. Med., 37, 32-37.
Klepper, I. D., Webb, R. K., Walt, J. V. D., Ludbrooks, G.
L., and Cockings, J., 1993. The sthethoscope:
Application and limintation- an analysis of 2000
incidents reports. Anaesth. Intens. Care, 21(5), 575-578.
Lederman, D., 2006. An energy ratio test for one lung
intubation detection. Paper presented at the 18th
Biennial International EURASIP conference, Brno,
Czech Republic.
Lederman, D., 2011. Endotracheal intubation confirmation
based on video image classification using a parallel
GMMs framework- a preliminary evaluation. Annals of
Biomed. Eng., 39(1), 508-513.
Li, J., 2001. Capnography alone is imperfect for
endotracheal tube placement confirmation during
emergency intubation. J. Emerg. Med., 20(3), 223-229.
Linko, K., Paloheimo, M., and Tammisto, T., 1983.
Capnograhphy for detection of accidental oesophageal
intubation. Acta Anaesthesiol. Scand., 27, 199-202.
Nolan, J. P., Deakin, C. D., and Soar, J., 2005. European
resuscitation council guidelines for resuscitation.
Resuscitation, 67(1), S39-S86.
O'connor, C. J., Mansy, H., Balk, R. A., Tuman, K. J., and
Sandler, R. H., 2005. Identification of endotracheal
tube malpopsitions using computerized analysis of
breath sounds via electronic stethoscopes. Anesth.
Analg., 101(3), 735-739.
Owen, R. L., and Cheney, F. W., 1987.
Endobronchial Intubation: a Preventable Complication.
Computer-Aided Diagnosis for Endotracheal Intubation Confirmation using Video-image Classification
539

Anesthesiology, 67, 255-257.
Peterson, A. W., and Jacker, L. M., 1973. Death following
inadvertent esophageal intubation: a case report.
Anesth. Analg., 52, 398-401.
Pointer, J. E., 1988. Clinical characteristics of paramedics'
performance of endotracheal intubation. J. Emerg.
Med., 6(505-509).
Silvestri, S., Ralls, G. A., and Krauss, B., 2005. The
effectiveness of out-of-hospital use of continuous end-
tidal carbon dioxide monitoring on the rate of
unrecognized misplaced intubation within a regional
emergency medical services system. Ann. Emerg. Med.,
45, 497-503.
Steward, R. D., Paris, P. M., and Winter, P. M., 1984. Field
endotracheal intubation by paramedical personnel:
success rates and complications. Chest, 85(341-345).
Tejman-Yarden, S., Lederman, D., Weksler, N., and
Gurman, G., 2006. Acoustic monitoring of double
lumen ventilated lungs for the detection of selective
unilateral lung ventilation. Anesth. Analg., 103, 1489-
1492.
Tejman-Yarden, S., Zlotnik, A., Weizman, L., Tabrikian, J.,
Cohen, A., Weksler, N., and Gurman, G. M., 2007.
Acoustic monitoring of lung sounds for the detection of
one-lung intubation. Anesth. Analg., 105(2), 397-404.
Timmermann, A., Russo, S. G., Eich, C., Roessler, M.,
Braun, U., Rosenblatt, W. H., and Quintel, M., 2007.
The out-of-hospital esophageal and endobronchial
intubations performed by emergency physicians. Crit.
Care and Trauma, 104(3), 619-623.
Vergese, S. T., Hannallah, R. S., Slack, M. C., Cross, R. R.,
and Patel, K. M., 2004. Auscultation of bilateral breath
sounds does not rule out endobronchial intubation in
children. Anesth. Analg., 56-58.
Wang, H. E., Cook, L. J., Chang, C. H., Yealy, D. M., and
Lave, J. R., 2009. Outcomes after out-of-hospital
endotracheal intubation errors. Resuscitation, 80(1),
50-55.
Wang, H. E., Lave, J. R., Sirion, C. A., and Yealy, M., 2006.
Paramedic intubation errors: isolated events or
symptoms of larger problems? Health Affairs, 25(2),
501-509.
Webb, R. K., Walt, J. H. V. D., Runciman, W. B.,
Williamson, J. A., Cockings, J., Russel, W. J., and
Helps, S., 1993. Which monitor? an analysis of 2000
indicent reports. Anaesth. Intens. Care, 21(5), 529-542.
Weizman, L., Tabrikian, J., and Cohen, A., 2008. Detection
of one-lung intubation incidents. Annals of Biomed.
Eng., 36(11), 1844-1855.
Wodicka, G. R., DeFrain, P. D., and Kraman, S. S., 1994.
Bilateral asymmetry of respiratory acoustic
transmission. Med. Biol. Eng. Comp., 32(5), 489-494.
Yap, S. J., Morris, R. W., and Pybus, D. A., 1994.
Alterations in endotracheal tube position during general
Anesthesia. Anaesth. Crit. Care, 586-588.
Zwillich, C. W., Pierson, D. J., and Creagh, C. E., 1974.
Complications of assisted ventilation, a prospective
study of 354 consecutive episodes. Am. J. Med., 57,
161-170.
ICPRAM 2017 - 6th International Conference on Pattern Recognition Applications and Methods
540
