
Interoperability in Pervasive Health: Is It Tackled as a Priority?
Ana Dias
1
, Ana Isabel Martins
2
, Alexandra Queirós
3
and Nelson Pacheco Rocha
2
1
GOVCOPP, Department of Economics, Management, Industrial Engineering and Tourism, University of Aveiro,
Campo Universitário de Santiago, 3810-193 Aveiro, Portugal
2
IEETA, Department of Medical Sciences, University of Aveiro,
Campo Universitário de Santiago, 3810-193 Aveiro, Portugal
3
IEETA, Health Sciences School, University of Aveiro, Campo Universitário de Santiago, 3810-193 Aveiro, Portugal
Keywords: eHealth, Pervasive Health, Interoperability, Home Monitoring.
Abstract: For the electronic health record (EHR) to be considered a true clinical decision support system, it must be
possible to access and integrate the patients’ clinical information collected throughout their lives, guaranteeing
up-to-date, safe and congruent information, immediately accessible at the place of care. Moreover, there is a
considerable capacity to develop and manufacture personal health devices (PHD) highly integrated and
miniaturized, which facilitate the home monitoring of patients with chronic diseases. Since the information
collected by PHD should be integrated in existing EHR, interoperability is an essential requirement of eHealth
to allow the integration of care into a diversity of settings and care providers. The purpose of this systematic
review was to identify and analyse references related to the topic of home monitoring that reveal an explicit
concern with interoperability requirements. Regarding the results and considering the initial 2778 references,
only 2% (61 references) explicitly mentioned interoperability issues and, within these 61 references, only
eight reported end-to-end solutions that can be integrated and usable in care service provision. Therefore, the
issue of interoperability of PHD, both semantic and technological, a priority for the establishment of a remote
patient monitoring solution market, is discussed in this review.
1 BACKGROUNG
Progresses attained in the last decades in health
information technology (HIT) are undeniable;
however, some goals apparently have not yet been
achieved. Efforts to link and aggregate patients’
clinical information collected throughout the care
process have been hampered by factors such as
technological "heritage", proprietary technology,
obsolete regulation, incomplete specification of end-
to-end standards and financial concerns (Perlin,
2016). The design and implementation of HIT has not
yet reached its potential in terms of impact it can have
on health care provision and interoperability is
assumed as being an essential requirement to
integrate health care into a diversity of settings and
care providers (Kuziemsky et al., 2016).
In health care delivery, there is significant amount
of information available, so the problem is less the
volume and more the value that is created with the
available information. Major difficulties are related to
the aggregation of information from different sources,
with different formats and meanings, as well as the
lack of tools to recognise, within all the available
information, which is relevant for each particular
situation and to make it useful rather than just being
visible (Halevy, 2011).
Due to the growing importance of the eHealth
paradigm (Eysenbach, 2001) and related concepts
(e.g. connected health (Kvedar et al., 2014), holistic
health (Rossi et al., 2013) or pervasive health
(Connelly et al., 2017)), contexts regarding health
care delivery have evolved. Particularly, health care
delivery has evolved from hospital to home, and
home monitoring of patients’ clinical information
together with context information resulting from their
environment might be incorporated in the
characterization of their health conditions. In this
pervasive context, different groups of technologies
assume an important role, namely telecare, mobile
health (mHealth) and ambient assisted living (AAL):
telecare include solutions such as monitoring devices
or medical alert devices to support patients in their
environments (Emery et al., 2002) or rehabilitation
activities (Cruz et al., 2013; Teixeira et al., 2013);
Dias, A., Martins, A., Queirós, A. and Rocha, N.
Interoperability in Pervasive Health: Is It Tackled as a Priority?.
DOI: 10.5220/0006545400570065
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 5: HEALTHINF, pages 57-65
ISBN: 978-989-758-281-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All r ights reserved
57

mHealth is related to the use of mobile
communication devices for the health care provision
(WHO, 2011); and AAL intends to respond to the
specific needs and major diseases of older adults in
their domestic spaces, increasing their autonomy,
confidence and participation ability (Queirós et al.,
2015).
The information is no longer stored and
exclusively managed by the electronic health records
(EHR) of the health care institutions. Although EHR
are adequate for the presentation of information from
patients, collected and aggregated in local HIT, the
reality is that the provision of health care is not
restricted to an institution or even to a single care
provision system (Queirós et al., 2013). All
caregivers need comprehensive, up-to-date, safe and
congruent information from the patient, immediately
accessible at the place of care, to ensure the highest
levels of clinical quality. For instance, when
considering the home monitoring of a patient with a
chronic disease (e.g. diabetes, heart failure or chronic
obstructive pulmonary disease), the resulting
monitoring information should be distributed within
an information network ranging from clinicians,
social care network, and family members to the
patients themselves. These requirements promote the
emergence of new technological approaches such as
personal health record (PHR) (Krukowski et al.,
2015) that aimed at electronic management of
information between the patients and their formal and
informal health care providers, and that might
contribute to the availability of the patients’ clinical
information that is collected throughout their lives
(Halevy, 2011).
However, the implementation of this vision is
bounded by a set of problems: for instance, clinical
information is blocked in HIT silos, generated and
stored in different systems that either do not
communicate with one another or are unable to
synthesize information to make it meaningful and
usable. Therefore, interoperability must be ensured,
in terms of communications protocols and semantic
normalization, between a wide range of information
sources and eHealth applications. Hence, initiatives
efforts carried out by international institutions such as
the Continua Health Alliance, the Health Care
Information and Management Systems Society
(HIMSS), the National Institute of Standards and
Technology (NIST), and the Integrating the
Healthcare Enterprise (IHE) are crucial to overcome
interoperability difficulties and to promote a
homogeneous eHealth ecosystem (Aragüés et al,
2011).
Given this background, the main purpose of the
systematic review reported in the present article was
to explore if interoperability is a real concern when
developing concrete pervasive solutions (e.g.
telehealth, mHealth or AAL applications) to gather
patients’ information, both clinical and contextual
information.
2 METHODS
The purpose of this systematic review was to identify
and analyse in more detail references related to home
monitoring, which reveal an explicit concern with
interoperability requirements. The general goals of
this systematic review were to identify, within the
selected references, how interoperability is addressed
in the solutions being proposed, how they are
validated and if there is effective technological and
semantic interoperability. The ultimate goal of this
analysis was to assess if, in addition to allowing
information sharing, the solutions proposed are able
to produce meaningful and contextualized
information that can be integrated into EHR, that is,
if the information they collect is qualified to be
integrated and usable in the care service provision.
Moreover, if this is the case, it is important to identify
standards that are most commonly used.
2.1 Study Design
Considered the aforementioned purposes, the
systematic review of the present study was informed
by the following research question: is there an explicit
concern related to interoperability during the
development of new eHealth applications to gather
patients’ information in their home environments?
Within references selected as expressing an
effective concern related to interoperability, some
sub-questions were raised:
▪ What are the problems being addressed?
▪ Which types of interoperability computational
support were provided?
▪ How the proposed solutions addressed
interoperability?
▪ Which technical implementation has been
used?
▪ Which methods were used to validate the
proposed interoperability implementations?
▪ Is the resulting information ready to be
integrated into the health care service
provision? If yes, which standards are being
used?
HEALTHINF 2018 - 11th International Conference on Health Informatics
58

To achieve these goals, initially, a systematic
review of literature published between 2011 and 2016
was performed.
Exclusively the references that had the keywords
“interoperability” or “interoperable” in title or
abstract were considered for further assessment and
classification, being excluded the first group of
references.
Subsequently, the references included for analysis
were assessed and some more were excluded
reflecting specified criteria, which is described
below. The remaining references were then
categorized according to the degree of significance to
answer the questions posed within this research, that
is to say the option was to analyse in greater detail the
references that proposed solutions in which it was
considered relevant that the information produced
could be integrated into the health care service
provision.
The methods used to conduct this systematic
review of literature as well as the subsequent
categorization of search results is described in the
following subsections.
2.2 Data Sources and Searches
The research was carried out using the Scopus, Web
of Science and IEEE Xplore Digital Library
databases, in the publications titles, abstracts and
keywords.
The keywords used in the search, simultaneously,
were: “monitoring” and “pervasive health”, since
these are the topics around which it is important to
evaluate the centrality of the interoperability issue.
Pervasive health is seen as a contribution to a more
personalized model of care allowing individuals to be
more actively involved in their care process. A classic
pervasive health care application is home monitoring
of health conditions, particularly patients with
chronic diseases. However, it is important to note that
pervasive health is more than monitoring applications
as it can also include preventive applications (e.g.
elderly people to live independently) (Queirós et al.,
2015).
The remaining keywords were: “mobile health”,
“mhealth” and “ambient assisted living”. These
keywords were combined so that at least one of them
corresponded to the subject of the search.
2.3 Inclusion and Exclusion Criteria
References with no author, no abstract, not written in
English, duplicates and editorials were excluded.
References selected for review were all written in
English and all who had a date of publication between
2011 and 2016. Then, all the references that did not
explicitly mention the “interoperability” or
“interoperable” keywords in tittle and/or in abstract
were also rejected.
Subsequently, within the references’ full texts
revised, those that corresponded to items out of ambit
of this systematic review were also excluded. Then,
in the group of references within the scope of this
systematic review, were also identified and excluded
those references that corresponded to categories to be
rejected in view of the objectives of this analysis,
specifically: overviews, political perspectives,
position papers, reviews and systematic reviews.
Then, the remaining references were clustered in
ascending order of importance for this study:
connection between devices; intermediate
components between devices and client applications
for handling the storage and sharing of the
information being gathered (e.g. architectures,
gateways, middleware or data hubs); intermediate
components but incorporating medical devices
specificities; and end-to-end solutions.
2.4 Study Selection
After the first screening, one author assessed all titles
for relevance. Those clearly not meeting the inclusion
criteria were removed.
Afterwards, the abstracts of the retrieved articles
were assessed against the inclusion and exclusion
criteria, by two authors. Any disagreements were
discussed with a third reviewer and resolved by
consensus. Abstracts were then subject to a first
classification and grouping.
Finally, the references that were selected by the
superior interest for this study were gathered and
analysed in more detail. Two authors, according to
the outlines criteria, then assessed again these full
texts thought to be of relevance, and any divergences
were also discussed with a third reviewer and agreed
by consensus.
3 RESULTS AND DISCUSSION
This systematic review followed the guidelines of the
Preferred Reporting Items for Systematic Reviews
and Meta-Analyses (PRISMA) (Moher et al., 2009)
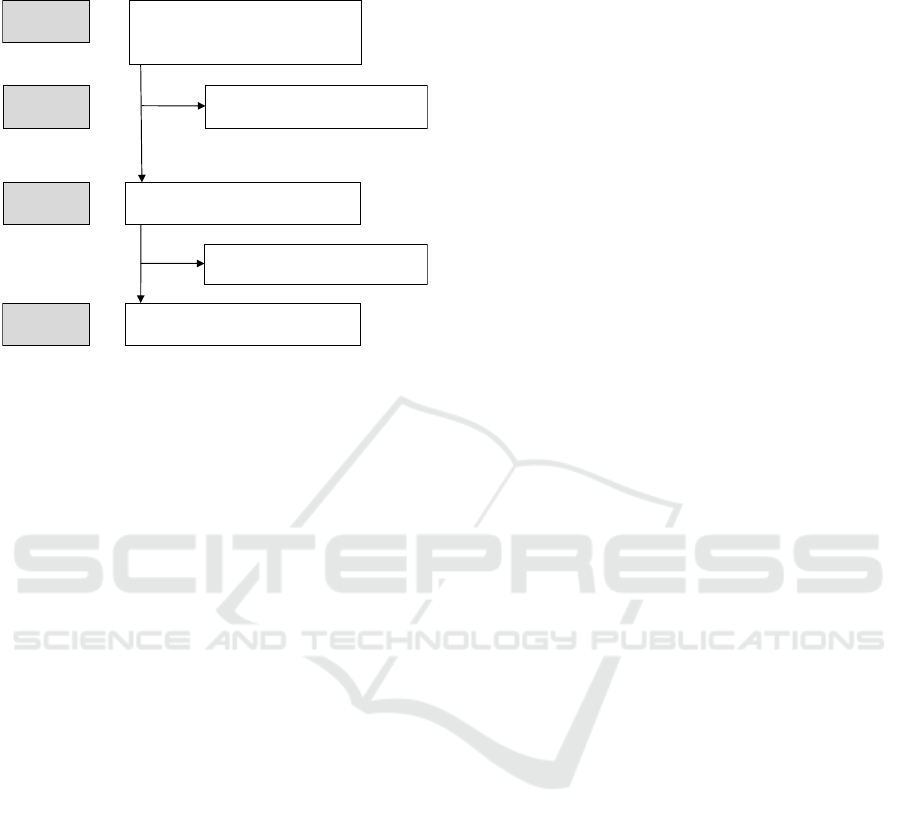
as described in Figure 1.
A total of 2778 references were retrieved from the
initial search of the selected databases. Then, 2717 of
these references were rejected because they did not
Interoperability in Pervasive Health: Is It Tackled as a Priority?
59
explicitly mention “interoperability” or
“interoperable” in the tittle and/or in the abstract.
Figure 1: PRISMA flowchart.
Afterwards, by reviewing these 61 references’
full-texts, 31 were excluded: the first 17 references
grouped and classified are articles assumed as out of
the scope of this study; other cluster (n=14) are
references that, although within the ambit of the
present analysis, were also excluded because they
correspond to position papers (n=5), systematic
reviews (n=3), reviews (n=1), overviews (n=2) and
political standpoints (n=3).
The remaining 30 references were first clustered
in ascending order of importance for this study: five
references deal with the connection between devices;
14 references are related to the intermediate
components between different types of sensors and
the client applications for handling the storage and
sharing of the devices’ information; three references
are similar to the previous, but incorporating medical
devices specificities; and the latter cluster (eight
references) comprises the references that propose
end-to-end solutions.
The group of references related to the connection
between devices (n=5) include those that describe
solutions providing communication protocols to
network sensors. The remaining three categories have
an ascendant interest to answer the questions raised in
this systematic review, going from ways to guarantee
connection between sensors to end-to-end solutions.
The group of 14 references contains articles that
report solutions with different designations (e.g.
architectures, gateways, middleware or data hubs) but
with the same purpose, which is to aggregate data
from various sources to provide it in an integrated
way to client applications. These references, although
being related to health care applications, they do not
allude to interoperability standards used in health care
applications. As for the three references incorporated
in the other cluster, they describe the same type of
solutions proposed in the last group, but explicitly
referring the use of health care standards.
Finally, the references that were selected by the
superior interest for this study (n=8), because
referring to end-to-end applications, allowing
connections to EHR and based on standards such as
Health Level Seven (HL7), were analysed in more
detail in the study reported by the present article.
3.1 Characteristics of the Studies
Within the 30 references selected and categorized
according to the degree of relevance for this
systematic review, there are several aspects to be
highlighted and analysed in this section.
Five references (Elsaadi et al, 2016; Escobar et al.,
2015; Fong, 2011; Grossi et al, 2012, Palma et al.,
2016) describe solutions providing communication
protocols to connect a large number of sensors.
Fourteen references report solutions to aggregate
data from various sources to provide it in an
integrated way to client applications (Carr et al.,
2013; Costa et al., 2014; Denkovski et al, 2015; Ding
et al. 2016; Ferreira et al., 2012; Kilintzis, et al., 2013;
Norgall et al., 2013; Pradilla et al, 2015; Rossi et al.,
2014; Ruiz-Zafra et al., 2013; Smirek, et al., 2016; Su
et al., 2011; Xiao et al., 2016; Woznowski et al.,
2015). These articles, though being related to health
care applications, they do not allude to
interoperability standards used in health care,
inhibiting the information that is produced from being
integrated into the health care service provision.
However, what is described in the type of solutions
proposed in three references (Damas et al., 2013;
Norgall et al., 2012; Pereira et al., 2014), explicitly
refer the use of health care standards, considering the
specificity of medical devices (e.g. the already
established ISO/IEEE 11073 standards-based
Continua personal health ecosystem - X73 protocol
(Damas et al., 2013)).
The main problem being addressed here is the lack
of interoperability among different levels of available
technologies which restricts a wider deployment
among intermediate and end-users (Pereira et al.,
2014), therefore the demand for interoperability
among devices is emphasized as most commercially
available devices include their own software and
communication protocols, which cause serious
problems and hinder the application of a standard
(Damas et al., 2013). Therefore, the shortfalls of
Included
Eligibility
Screening
Identification
Articles found in Scopus, Web of Science and
IEEE Xplore Digital Library (n=2778):
Articles underwentfullreview (n=61).
Excluded based on the full review (n=31).
Total number of articles (n=30).
Articles excluded based on the review of
their titles and abstracts (n=2717).
HEALTHINF 2018 - 11th International Conference on Health Informatics
60

dominating insulated available products are
highlighted (Norgall et al., 2012).
To address interoperability, the references
reported different communication protocols,
including Bluetooth Health Device Profile (HDP)
(Pereira et al., 2014) and Open Services Gateway
initiative (OSGi), a framework for modular systems
that simplifies building, deploying, and managing
complex applications. OSGi is complemented with
the X73 standard data model, which allowed, for
instance, the modelling of the information being
gathered (Damas et al., 2013) so that the information
resulting from different AAL systems might be
integrated (Norgall et al., 2012).
Concerning the type of interoperability
computational support, different solutions’
designations are reported although they pursue the
same objective, which is the aggregation of data from
multiple sources to provide them in an integrated way
to client applications, namely: architectures (Costa et
al., 2014, Ding et al., 2016, Norgall et al., 2013, Ruiz-
Zafra et al., 2013; Xiao et al., 2016; Woznowski et al.,
2015), gateways (Costa et al., 2014, Denkovski et al,
2015, Ding et al., 2016, Smirek, et al., 2016),
middleware (Carr et al., 2013, Kilintzis, et al., 2013)
or data hub (Woznowski et al., 2015).
Regarding the validation of the proposed
interoperability solution, the following methods are
reported: prototype (Ruiz-Zafra et al., 2013; Xiao et
al., 2016), case study (Kilintzis, et al., 2013; Pradilla
et al, 2015), proof of concept (Costa et al., 2014) and
scenarios implementation (Su et al., 2011).
3.2 Interoperability
The results presented and discussed in this section
relate to the eight articles (within the 61 references
assessed for inclusion) that have been highlighted by
this systematic review. These eight articles
correspond to end-to-end solutions and they report an
effective concern related to the interoperability issue,
proposing concrete solutions to ensure that the
information produced could be integrated into the
health care provision, as summarized in Tables 1, 2
and 3.
Concerning Table 1, it gives a global perspective
on how the subject of interoperability is addressed in
the references analysed herein, namely the problems
to be solved, the interoperability computational
support and the proposed technical solutions. In
particular, and with regard to the problems addressed
in literature, one of them are the difficulties
experienced in the sharing of information between
personal health devices (PHD) and care providers.
This reinforces the need to provide data in proven
standard form (Mihaylov et al., 2015), as well as the
requirement to ensure the interoperability of various
PHD and EHR for continuous self-management of
chronic disease patients. However, reliability,
interoperability, and scalability between different
PHD imply additional costs during the healthcare
applications development (Park et al., 2016). Another
difficulties that were tackled in literature was the need
to integrate data from different eHealth applications,
for instance to maximize the access to better therapies
and advanced medical devices (Torres Zenteno et al.,
2016) as well as the demand for the information
sharing between the PHR and the EHR, namely to
allow patients to alert health care professionals
automatically in real time when necessary (Galligioni
et al., 2015).
Considering the references which were subject to
a depth analysis (Alberts et al., 2014; Galligioni et al.,
2015; Gietzelt et al., 2014; Jung et al., 2014; Lee et
al., 2013; Mihaylov et al., 2015; Park et al., 2016;
Torres Zenteno et al., 2016), in all the solutions
reported the focus is on guaranteeing integration of
information, being reported in every case that the
resulting information is ready to be integrated in the
health care service provision. However, concerning
this issue, in some cases this is more explicit and
detailed (Lee et al., 2013; Mihaylov et al., 2015; Park
et al., 2016; Torres Zenteno et al., 2016) than others
(Alberts et al., 2014; Galligioni et al., 2015; Gietzelt
et al., 2014; Jung et al., 2014).The integration of
information from existing eHealth applications to
provide integrated data analysis is a central concern
(Alberts et al., 2014).
In particular the demand to ensure interoperability
of various PHD and EHR for continuous monitoring
and self-management of patients with chronic
diseases (Galligioni et al., 2015; Gietzelt et al., 2014;
Jung et al., 2014; Lee et al., 2013; Mihaylov et al.,
2015; Park et al., 2016; Torres Zenteno et al.,
2016).The need to provide sensor data in proven
standard form is denoted, as the existing coding
systems do not appear to be sufficient to encode the
data resulting from a variety of sensors (Gietzelt et
al., 2014). Thus, current solutions are considered to
lack interoperability and obstruct the establishment of
a remote patient monitoring solution market
(Mihaylov et al., 2015).
Interoperability in Pervasive Health: Is It Tackled as a Priority?
61

Table 1: Problem addressed, solution and computational support.
ID
Problem addressed
Interoperability
computational support
Proposed solutions
Lee et al., 2013
Sharing of information from
PHD to care providers.
Middleware
A multi-agent platform that transmits patient clinical
data for services based on interoperability standards.
Alberts et al., 2014
Information sharing between
eHealth applications.
Middleware
An Integrated eHealth platform that consists of two
sub-platforms: the health integration and analysis sub-
platform and the communications sub-platform.
Jung et al., 2014
Information sharing between
PHR and EHR.
Application
A mHealth application that interfaces with hospital
EHR
Gietzelt et al., 2014
Information sharing between
eHealth applications.
Architecture
Centralized registration of placeholder-documents
together with a decentralized data storage at peoples’
home.
Galligioni et al., 2015
Information sharing between
PHR and EHR.
Architecture
Web-based, multi-tier architecture with the following
components: electronic oncological patient record
(eOPR), RFID bar code reader, bar-coded drug labels,
disposable RFID bracelets for patients, RFID tags for
nurses and a mobile device.
Mihaylov et al., 2015
Sharing of information from
PHD.
Application
Design and implementation of an interoperable,
intelligent caring home system offering personalized
context-aware applications.
Torres Zenteno et al., 2016
Information sharing between
eHealth applications.
Platform
A technological platform that supports the predefined
process following an interoperability model based on
standards and implemented by a service-oriented
architecture.
Park et al., 2016
Sharing of information from
PHD.
Application
The application for continuous self-management of
chronic disease patients that communicates with PHD.
Table 2: Standards being reported.
ID
Standards used for integration
Alberts et al., 2014; Jung et al., 2014; Galligioni et al., 2015
Not reported
Gietzelt et al., 2014
HL7 CDA; HL7 Arden syntax; SNOCAP-HET; MQTT
protocol
Lee et al., 2013
HL7 V2.5 Messages
Mihaylov et al., 2015
HL7 V3 CDA; X73
Park et al., 2016
HL7 V2.6; CCR; CCD; X73; HDP
Torres Zenteno et al., 2016
CEN/ISO 13606; IHE
Table 3: Validation.
ID
Validation
Alberts et al., 2014; Jung et al., 2014
Not reported
Galligioni et al., 2015
Laboratory tests
Gietzelt et al., 2014
Future work
Lee et al., 2013
Meaningful use
Mihaylov et al., 2015
Proof of concept
Park et al., 2016
Clinical trial
Torres Zenteno et al., 2016
Simulation
HEALTHINF 2018 - 11th International Conference on Health Informatics
62

Three references are particularly focused on the
need to find more advanced solutions to guarantee
interconnection with the EHR as well as to improve,
optimize and reduce the time in care in particular
pathologies, specifically diabetes (Jung et al., 2014),
cancer (Galligioni et al., 2015) and stroke (Torres
Zenteno et al., 2016).
In order to address interoperability, the reported
solutions include, for instance: an application, the
Self-Management mobile PHR that communicates
with PHD (e.g. blood pressure monitor or pulse
oximeter) that have implemented standard protocols
so that stored vital signs are converted to HL7 and are
transmitted to PHR (Park et al., 2016); a PHR service,
interconnected with mHealth applications that use
clinical information from the EHR system of a
tertiary hospital to provide services to support
patients with chronic diseases, such as diabetes
patients (Jung et al., 2014); an architectural approach
to integrate Home-Centred Health-Enabling
Technology into Regional Health Information
Systems, a centralized registration of placeholder-
documents with a decentralized data storage at
patients’ home, using the Systematic Nomenclature
for Contexts, Analysis methods and Problems in
Health Enabling Technologies (SNOCAP-HET),
which is a nomenclature to describe the context of
sensor-based measurements in health-enabling
technologies (Gietzelt et al., 2014).
Regarding the standards applied in the proposed
solutions (Table 2), the choice of HL7 was made in
most of the solutions in which standardized solutions
are reported (Gietzelt et al., 2014; Lee et al., 2013;
Mihaylov et al., 2015; Park et al., 2016): X73 with
HL7 V2.6 was used in two cases (Mihaylov et al.,
2015; Park et al., 2016), being stated others such as
Continuity of Care Document (CCD) and Continuity
of Care Record (CCR) (Park et al., 2016), Message
Queue Telemetry Transport protocol (MQTT)
(Gietzelt et al., 2014) and the CEN/ISO 13606, which
has been designed to support the semantic
interoperability of the communications between EHR
(Torres Zenteno et al., 2016). The standards applied
were not reported in three cases (Alberts et al., 2014;
Galligioni et al., 2015; Jung et al., 2014).
Finally, concerning the methods used to validate
the proposed interoperability solutions (Table 3): in
one of the cases, the evaluation was carried out by
meaningful use (Lee et al., 2013); in another case,
after laboratory tested, it was adopted as a routine in
two hospitals, having also been investigated its
usability and acceptance within professionals using
the system (Galligioni et al., 2015); and in other cases
the options were the proof of concept (Mihaylov et
al., 2015), simulation (Torres Zenteno et al., 2016)
and clinical trial (Park et al., 2016). In the remaining
three cases (Alberts et al., 2014; Gietzelt et al., 2014;
Jung et al., 2014) the validation methods were not
reported.
As an example, a clinical trial was carried out to
evaluate the transmission error rate for the measured
vital signs transmitted from PHD to a mHealth
application and from this to PHR Systems (Park et al.,
2016). Another case was the technological platform
that was tested with clinician staff, researchers,
electronic support staff and actors playing patients
role, having been defined several scenarios to test the
technological structure, being stated that, after this
phase, the platform would be tested with patients
suffering from clinical suspicion of stroke (Torres
Zenteno et al., 2016).
4 CONCLUSIONS
The first relevant conclusion concerning the retrieved
references is that in all the solutions reported the
focus is on guaranteeing integration of information,
being stated in every case that the resulting
information is ready to be integrated in the health care
service provision, although in only half of the cases
the details concerning this issue, are given more
objectively. The integration of information from
existing eHealth applications to provide integrated
data analysis is a central concern and current
solutions are considered to lack interoperability and
obstruct the establishment of a remote patient
monitoring solution market.
The design and implementation of eHealth
applications has not yet reached its potential in terms
of impact it can have on health care provision, and
interoperability is assumed as being an essential
requirement of HIT for the need to integrate patient
care into a diversity of settings and care providers.
Therefore, EHR systems should not only provide
access to patients’ clinical information, but also as a
true clinical decision support method, have the ability
to access and integrate patients’ clinical information
that is collected throughout their lives.
This is particularly important when dealing with
home monitoring of clinical and non-clinical
parameters recorded in daily life using various PHD.
So that the provision of remote medical services is
possible, the PHD should be connected in conjunction
with the institutional EHR systems as the occasion
demands.
This envisaged scenario is constrained by the lack
of implementations based on standardized
Interoperability in Pervasive Health: Is It Tackled as a Priority?
63

information models that have same information
content and transmission purposes.
The results of the systematic review presented in
this article show that interoperability is not the major
concern of a significant number of current
technological developments. Indeed, it should be
emphasized that of the 2778 initial references only
2% (61 references) explicitly mentioned the issue of
interoperability. Moreover, within these 61
references assessed for inclusion, only eight
corresponded to end-to-end solutions, since the
information produced could be integrated into the
health care service provision, where interoperability
was considered an effective concern. Furthermore,
within these eight references only one refers
standards specifically related to semantic
interoperability, used in a system whose validation is
not yet reported.
So, and despite the developments that have been
made in this area, there seems to be a lack of
integration in the care chain, which may indicate the
need to give greater priority to the issue of
interoperability of PHD, both semantic and
technological.
ACKNOWLEDGEMENTS
This work was partially supported by COMPETE
2020 - Programa Operacional Competitividade e
Internacionalização, Sistema de Incentivos à
Investigação e Desenvolvimento Tecnológico (SI
I&DT), under the project Social Cooperation for
Integrated Assisted Living (SOCIAL).
REFERENCES
Alberts, R., Fogwill, T., Botra, A., Cretty, M., 2014. An
integrative ICT platform for eHealth. In 2014 IST-
Africa Conference and Exhibition, IST-Africa 2014.
Aragüés, A., Escayola, J., Martínez, I., Del Valle, P.,
Muñoz, P., Trigo, J. D., García, J., 2011. Trends and
challenges of the emerging technologies toward
interoperability and standardization in e-health
communications. IEEE Communications Magazine,
49(11), 182-188.
Connelly, K., et al., 2017. The Future of Pervasive Health.
IEEE Pervasive Computing, 16.1: 16-20.
Carr, D., O'Grady, M. J., O'Hare, G. M. P., Collier, R.,
2013. SIXTH: A middleware for supporting ubiquitous
sensing in personal health monitoring. International
Conference on Wireless Mobile Communication and
Healthcare. Springer, Berlin, Heidelberg, 2012.
Costa, A., Novais, P., Simoes, R., 2014. An AAL
collaborative system: The AAL4ALL and a mobile
assistant case study. Working Conference on Virtual
Enterprises (pp. 699-709). Springer, Berlin,
Heidelberg.
Cruz, V.T. et al., 2013. A rehabilitation tool designed for
intensive web-based cognitive training: Description and
usability study. Journal of Medical Internet Research,
15 (12), pp. e59.
Damas, M., Pomares, H., Gonzalez, S., Olivares, A., Rojas,
I., 2013. Ambient assisted living devices
interoperability based on OSGi and the X73 standard.
Telemedicine and e-Health, 19(1).
Denkovski, D., Atanasovski, V., Gavrilovska, L., 2015.
Device gateway design for ambient assisted living.
Future Access Enablers of Ubiquitous and Intelligent
Infrastructures (pp. 100-107). Springer International
Publishing.
Ding, F., Song, A., Tong, E., Li, J., 2016. A smart gateway
architecture for improving efficiency of home network
applications. Journal of Sensors, 2016.
Elsaadi, R., Shafik, M., 2016. Deployment of assisted living
technology using intelligent body sensors platform for
elderly people health monitoring. Advances in
Transdisciplinary Engineering, 3, 219-224.
Emery D., Heyes B.J., Cowan A.M., 2002. Telecare
delivery of health and social care information. Health
Informatics Journal, 8(1):29-33.
Escobar, R., Akopian, D., Boppana, R., 2015. A sensor data
format incorporating battery charge information for
smartphone-based mHealth applications. In
Proceedings of SPIE - the International Society for
Optical Engineering.
Eysenbach G., 2001. What is e-health? J Med Internet Res.,
3(2): e20.
Ferreira, L., Ambrósio, P., 2012. Towards an interoperable
health-assistive environment: The eHealthCom
platform. In Proceedings - IEEE-EMBS International
Conference on Biomedical and Health Informatics, BHI
2012, 930-932.
Fong, S., 2011. Integration RFID in Internet Applications.
In Özcan, A., Zizka, J. and Nagamalai, D. (Eds.):
WiMo/CoNeCo 2011, CCIS 162, pp. 207–216, 2011.
Heidelberg: Springer.
Galligioni, E., et al., 2015. Integrating mHealth in
oncology: Experience in the province of Trento.
Journal of Medical Internet Research, 17(5).
Gietzelt, M., et al., 2014. Home-centered health-enabling
technologies and regional health information systems
an integration approach based on international
standards. Methods of Information in Medicine, 53(3),
160-166.
Grossi, F., Bianchi, V., Losardo, A., Matrella, G., De
Munari, I., Ciampolini, P., 2012. A flexible framework
for ambient assisted living applications. In Proceedings
of the IASTED International Conference on Assistive
Technologies, AT 2012, 817-824.
Halevy, A., 2011. Game-changing interoperability for
healthcare: Bringing semantically harmonized clinical
information into provider workflows from disparate
HEALTHINF 2018 - 11th International Conference on Health Informatics
64

health information technologies. In 8th International
Conference and Expo on Emerging Technologies for a
Smarter World, CEWIT 2011.
Jung, E. -., Kim, J., Chung, K. -., Park, D. K., 2014. Mobile
healthcare application with EMR interoperability for
diabetes patients. Cluster Computing, 17(3), 871-880.
Kilintzis, V., Moulos, I., Koutkias, V., Maglaveras, N.,
2013. Exploiting the universAAL platform for the
design and development of a physical activity
monitoring application. In Proceedings of the 6th
International Conference on PErvasive Technologies
Related to Assistive Environments. ACM.
Krukowski, A., et al., 2015. Personal Health Record.
Cyberphysical Systems for Epilepsy and Related Brain
Disorders. Springer International Publishing (205-
238).
Kuziemsky, C. E., Peyton, L., 2016. A framework for
understanding process interoperability and health
information technology. Health Policy and Technology,
5(2), 196-203.
Kvedar J., Coye, M.J., Everett, W., 2014. Connected health:
a review of technologies and strategies to improve
patient care with telemedicine and telehealth. Health
Aff (Millwood), 33(2):194-199.
Lee, D. -., Bae, S., Song, J. H., Yi, B. -., Kim, I. K., 2013.
Improving chronic disease management with mobile
health platform. In Proceedings of the Annual
International Conference of the IEEE Engineering in
Medicine and Biology Society, EMBS, 2275-2278.
Mihaylov, M., Mihovska, A., Kyriazakos, S., Prasad, R.,
2015. Interoperable eHealth platform for personalized
smart services. In 2015 IEEE International Conference
on Communication Workshop, ICCW 2015, 240-245.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G., Group,
P., 2009. Preferred reporting items for systematic
reviews and meta-analyses: The PRISMA statement.
PLoS Med., 6, e1000097.
Norgall, T., Wichert, R., 2012. Towards interoperability
and integration of personal health and AAL
ecosystems. In Studies in Health Technology and
Informatics, 177, 272-282.
Norgall, T., Wichert, R., 2013. Personalized use of ICT-
from telemonitoring to ambient assisted living. In
Studies in Health Technology and Informatics, 187
145-151.
Palma, L., Pernini, L., Belli, A., Valenti, S., Maurizi, L.,
Pierleoni, P., 2016. IPv6 WSN solution for integration
and interoperation between smart home and AAL
systems. In Proceedings of SAS 2016 - Sensors
Applications Symposium, 171-175.
Park, H. S., Cho, H., Kim, H. S., 2016. Development of a
multi-agent M-health application based on various
protocols for chronic disease self-management. Journal
of Medical Systems, 40(1).
Pereira, R., Barros, C., Pereira, S., Mendes, P. M., Silva, C.
A., 2014. A middleware for intelligent environments in
ambient assisted living. In Annual International
Conference of the IEEE Engineering in Medicine and
Biology Society, 2014.
Perlin, J. B., 2016. Health information technology
interoperability and use for better care and evidence.
JAMA - Journal of the American Medical Association,
316(16), 1667-1668.
Pradilla, J., Palau, C., Esteve, M., 2015. SOSLITE:
Lightweight Sensor Observation Service (SOS) for the
Internet of Things (IOT), In 2015 ITU Kaleidoscope:
Trust in the Information Society (K-2015), Barcelona,
2015, pp. 1-7.
Queirós, A., Carvalho, S., Pavão, J., Rocha, N.P. 2013.
AAL information based services and care integration.
In HEALTHINF 2013 - Proceedings of the
International Conference on Health Informatics, pp.
403-406.
Queirós, A., Silva, A., Caravau, H., Ferreira, A., Cerqueira,
M., Alvarelhão, J., Santos, M., Rocha, N.P. 2015.
Pervasive health and regulatory frameworks. In
Proceedings of the International Conference on Health
Informatics - Volume 1: HEALTHINF, 494-501, 2015,
Lisbon, Portugal.
Rossi, L., et al., 2014. Interoperability issues among smart
home technological frameworks. In MESA 2014 - 10th
IEEE/ASME International Conference on Mechatronic
and Embedded Systems and Applications.
Rossi M. A., Mazzeo M., Mercurio G., Verbicaro R., 2013.
Holistic health: predicting our data future (from inter-
operability among systems to co-operability among
people). Int J Med Inform, 82(4): e14-e28.
Ruiz-Zafra, Á., Benghazi, K., Noguera, M., Garrido, J. L.,
2013. Zappa: An open mobile platform to build cloud-
based m-health systems. Ambient Intelligence-Software
and Applications (pp. 87-94). Springer, Heidelberg.
Smirek, L., Zimmermann, G., Beigl, M., 2016. Just a smart
home or your smart home - A framework for
personalized user interfaces based on eclipse smart
home and universal remote console. Procedia
Computer Science, 58, 107-116.
Su, C. -., Wu, C. -, 2011. JADE implemented mobile multi-
agent based, distributed information platform for
pervasive health care monitoring. Applied Soft
Computing Journal, 11(1), 315-325.
Teixeira, A. et al., 2013. New telerehabilitation services for
the elderly. In Handbook of Research on ICTs and
Management Systems for Improving Efficiency in
Healthcare and Social Care, pp. 109-132. IGI Global.
Torres Zenteno, A. H., et al., 2016. Mobile platform for
treatment of stroke: A case study of tele-assistance.
Health Informatics Journal, 22(3), 676-690.
Xiao, B., Kanter, T., Rahmani, R., 2016. Logical
interactions for heterogeneous IoT entities via virtual
world mirrors in support of ambient assisted living.
Journal of Ambient Intelligence and Smart
Environments, 8(5), 565-580.
WHO, 2011. mHealth: New horizons for health through
mobile technologies. Global Observatory for eHealth
series - Vol. 3. World Health Organization.
Woznowski, P., et al., 2015. A multi-modal sensor
infrastructure for healthcare in a residential
environment. In 2015 IEEE International Conference
on Communication Workshop, ICCW 2015, 271-277.
Interoperability in Pervasive Health: Is It Tackled as a Priority?
65
