
Sharing With Care
Multidisciplinary Teams and Secure Access to Electronic Health Records
Mohamed Abomhara
1
, Berglind Smaradottir
2
, Geir M. Køien
1
and Martin Gerdes
2
1
Department of Information and Communication Technology, University of Agder, Norway
2
Centre for eHealth, University of Agder, Norway
Keywords:
Multidisciplinary Team, Collaborative Healthcare, Electronic Health Record, Access Control, Security,
Privacy.
Abstract:
Ensuring patient privacy and improving patient care quality are two of the most significant challenges faced
by healthcare systems around the world. This paper describes the importance and challenges of effective mul-
tidisciplinary team treatment and the sharing of patient healthcare records in healthcare delivery. At present,
electronic health records are used to create, manage and share patient healthcare information efficiently and
effectively. The security and privacy concerns with sharing and the proper use of protected health information
need to be highlighted. Additionally, an access control solution is presented, which is suitable for collabora-
tive healthcare systems to address concerns with information sharing and information access. In this access
control model, the multidisciplinary team is classified based on Belbin’s team role theory to ensure that access
rights are adapted dynamically to the actual needs of healthcare professionals and to guarantee confidentiality
as well as protect the privacy of sensitive patient information.
1 INTRODUCTION
Electronic health records (EHRs) and multidisci-
plinary teams (MDTs) have become a vital part of
modern healthcare delivery (Smaradottir et al., 2016b;
O’Daniel and Rosenstein, 2008; Firth-Cozens, 2001).
Daily clinical care necessitates the collaborative sup-
port of MDTs including healthcare professionals
(physicians, specialists, and nurses) and healthcare
organizations (clinics and hospitals) (Abomhara and
Køien, 2016). Such MDT treatment within or among
healthcare organizations has been shown to have im-
mediate and positive impact on patient care (Jnr,
2011; Kim et al., 2010). Moreover, EHRs are widely
adopted by healthcare providers and patients to cre-
ate, manage and share patient healthcare informa-
tion efficiently and effectively (Chao, 2016). The
barrier that currently overshadows the effective use
of EHRs is the lack of security control over infor-
mation flow, whereby protected health information
is shared among a group of people within or across
healthcare organizations (Abomhara and Yang, 2016;
Fern
´
andez-Alem
´
an et al., 2013). A major concern is
to avoid unauthorized disclosure and improper access
to patient healthcare records. Patient records contain
sensitive information, which calls for the enhance-
ment and development of existing security mecha-
nisms (particularly access control) to ensure secure
sharing of health information (Vodicka et al., 2013;
Alhaqbani and Fidge, 2008).
In this study, an investigation is conducted on the
collaboration requirements, patient data confidential-
ity and the need for flexible access of the MDTs cor-
responding to the requirements to fulfill their duties
(section 2), followed by an overview of the existing
access control models (section 3). Section 4 demon-
strates how the proposed work-based access control
model (WBAC) (described earlier by (Abomhara and
Køien, 2016; Abomhara and Yang, 2016; Abomhara
and Nergaard, 2016; Abomhara et al., 2017)) is suit-
able for supporting MDT treatment of information
sharing and information security. Discussion and crit-
ical observations are presented in section 5. Section 6
concludes the study.
2 BACKGROUND
This section provides a background of MDTs care,
EHRs and healthcare record security.
Abomhara, M., Smaradottir, B., Køien, G. and Gerdes, M.
Sharing With Care - Multidisciplinary Teams and Secure Access to Electronic Health Records.
DOI: 10.5220/0006562403790386
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 5: HEALTHINF, pages 379-386
ISBN: 978-989-758-281-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
379
Resource
1
Resource
2
Resource
3
Alex
Dean
Cara
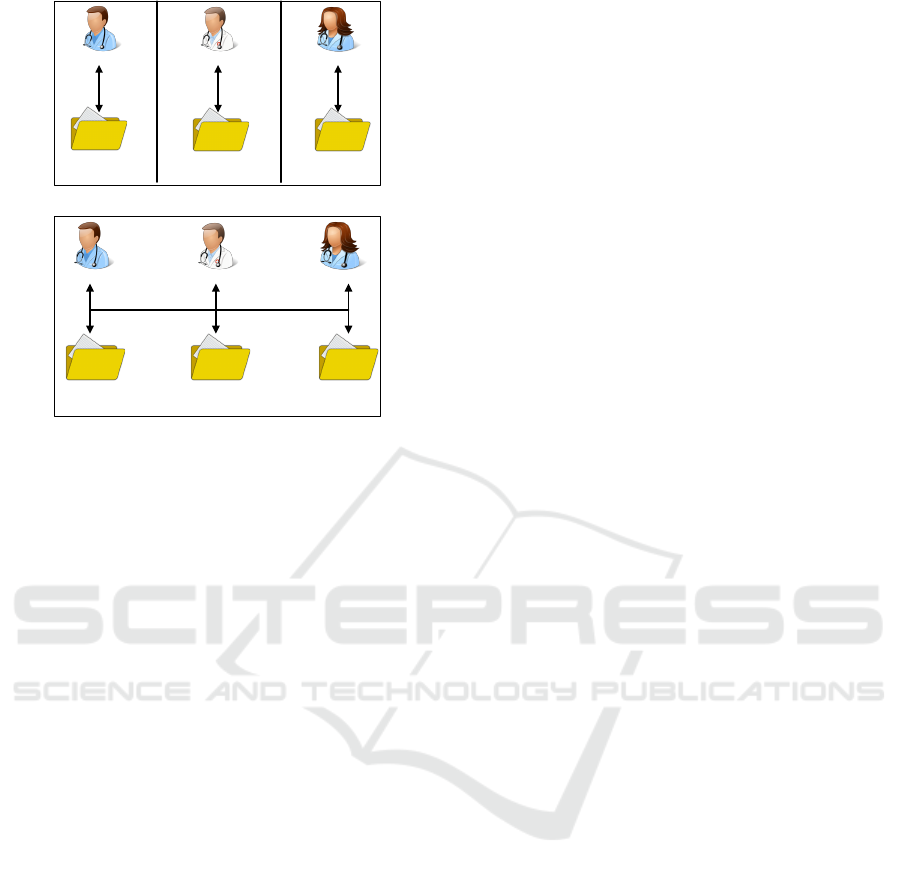
(a) Resource in isolation
Resource
1
Resource
2
Resource
3
Alex
Dean
Cara
(b) Resource sharing in collaborative environ-
ment
Figure 1: Resource in isolation and resource sharing
(Abomhara and Yang, 2016).
2.1 Multidisciplinary Team Care
A MDT is defined as a group of healthcare profession-
als from different disciplines, who ideally possess a
variety of skills necessary to provide specific patient
services with the aim of delivering effective patient
care (Jnr, 2011; Firth-Cozens, 2001) and improving
the outcomes of patients with complex chronic dis-
eases (Monteleone et al., 2016; Kim et al., 2010).
The importance and the effectiveness of MDT have
been particularly highlighted in many studies (Jnr,
2011; Kim et al., 2010). A typical example of patient
care involving MDT is a pregnant woman (Amy) with
diabetes who develops a pulmonary embolism (PE)
(Monteleone et al., 2016). Her medical care team
could include (but is not limited to) an obstetrician, an
endocrinologist, a respiratory physician, nurses and
others.
One of the key aspects of an MDT is resource
sharing (Fabian et al., 2015). To cooperate, each team
member must be prepared to gather and share their
findings with the other team members. In order to an-
alyze, decide and solve a certain patient case collabo-
ratively, the team members must have similar knowl-
edge of the actual situation. According to Figure 1,
each healthcare professional initially accesses their
own resource in isolation (Fig. 1(a)). However, upon
establishing the MDT treatment, the process of shar-
ing progresses (Figure 1(b)).
Although MDT treatment generally improves pa-
tient outcome, there are a number of challenges and
barriers to the success of the MDT. These chal-
lenges can be insufficient organization and resource
management, poor coordination and communication
(O’Daniel and Rosenstein, 2008; Firth-Cozens, 2001)
as well as health records security and privacy vi-
olation (Fern
´
andez-Alem
´
an et al., 2013; Coorevits
et al., 2013). If the effort in an MDT is not prop-
erly managed and organized, productivity may suf-
fer. Good coordination and communication skills are
at the core of patient safety and effective teamwork.
When healthcare providers engage in an MDT activ-
ity, they are required to switch between varying tasks
and roles of distinct nature. It implies that the MDT
environment must include a systems such as EHRs
that assist with task switching accordingly, allows
good resource communication between the MDT and
the patient, as well as ensures the availability, con-
fidentiality, and integrity of resources by providing
them only to those with proper authorization.
2.2 Electronic Health Records
EHRs are compilations of the various types of health
records of patients and are stored in electronic format.
EHR integration in healthcare organizations (clinics
and hospitals) offers potential benefits in terms of im-
proved care quality (Chao, 2016), simplified manage-
ment and enabling efficient in- and out-patient record
exchange. Thus, costs associated with patient care
and administrative overhead are reduced (Bain, 2015;
Alhaqbani and Fidge, 2008). A significant component
of EHRs is the key role in various aspects of facilitat-
ing the MDT to fulfil the information requirements
of daily clinical care (Chao, 2016). Both healthcare
providers (healthcare professionals and/or organiza-
tions) and patients can benefit from the EHR feature
of health record management and sharing. Patient
records can be created by one healthcare professional
and digitally shared and reviewed by other profession-
als instantly.
EHRs can overcome the traditional barriers to
MDTs by enabling communication between partici-
pants and providing rapid access to healthcare records
when distance separates the participants (Vawdrey
et al., 2011). It improves how the MDTs work and
enables more fluid cooperation and information ex-
change between healthcare professionals within and
among healthcare organizations. To cite an example,
within the EU project United4Health (United4Health,
2017), a collaborative telemedicine system for remote
monitoring of chronic obstructive pulmonary disease
(COPD) was developed to support MDT work across
the organization of health care services. Both hospi-
tals and municipal healthcare services have access to
HEALTHINF 2018 - 11th International Conference on Health Informatics
380
patient information (Smaradottir et al., 2016a). In a
related study, a similar system was developed to sup-
port collaborative MDT work in dementia healthcare
(Smaradottir et al., 2016b; Smaradottir et al., 2015).
Although EHR systems may improve healthcare
quality, the digitalization of health records, the col-
lection, evaluation and provisioning of patient data,
and the transmission of health data over public net-
works (the Internet) pose new privacy and security
threats (Abomhara et al., 2015; Rostad et al., 2007).
Such threats include, among others, (1) improper dis-
closure of sensitive healthcare information by privi-
leged healthcare professionals, (2) unauthorized ac-
cess to healthcare information by persons taking ad-
vantage of the MDT environment and (3) cyber crim-
inals gaining access to valuable data such as protected
health information (PHI) (Abomhara et al., 2015).
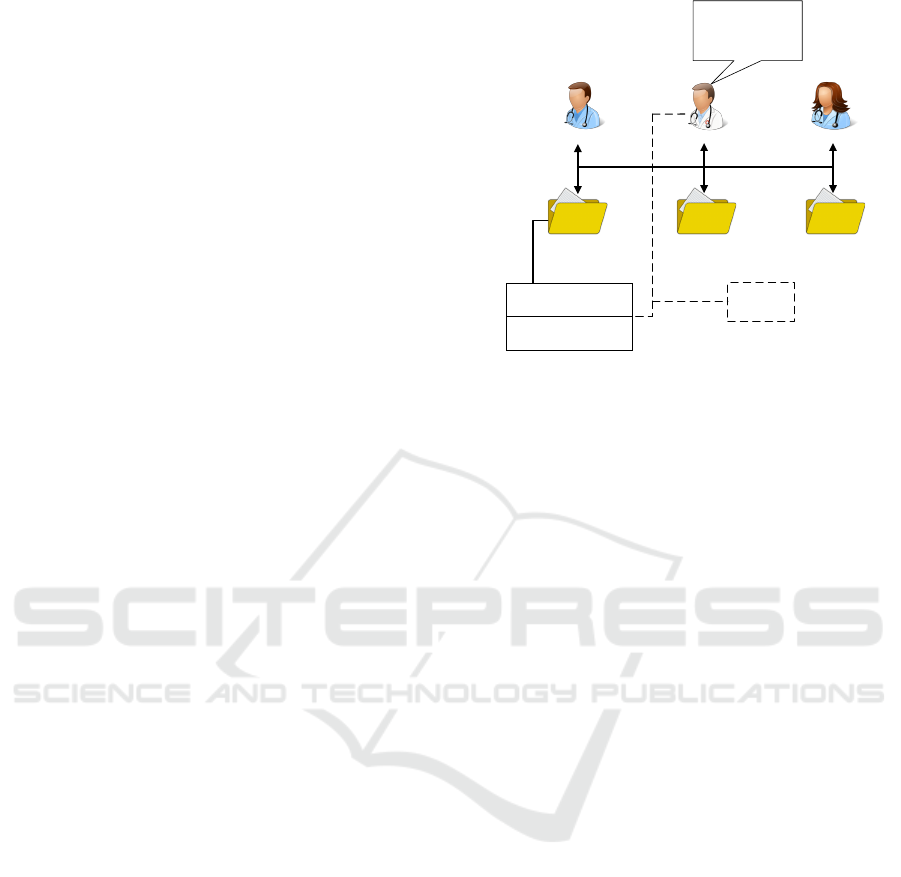
Improper disclosure or unauthorized access may
occur when someone within the MDT accesses shared
resources for unethical reasons (insider threat (Probst
et al., 2010)), for instance accessing a patient’s private
information for personal gain. One of the main causes
of an improper disclosure is information leakage,
which emerges when a supporting party is granted ac-
cess beyond what is actually required. In Figure 2, it
is assumed that three physicians are working collab-
oratively on a pregnant woman example (section 2.1)
at the hospital. They are discussing the possible treat-
ment for a patient. To do so, they must analyze her
medical file but not her personal information. How-
ever, the 2
nd
physician (Alex) is curious about the pa-
tient. He exploits the collaborative environment to ob-
tain more personal information without permission.
2.3 Security and Privacy of EHRs
Security and privacy have been a major con-
cern for patient and healthcare providers world-
wide (Fern
´
andez-Alem
´
an et al., 2013; Liu et al.,
2011). These concerns have limited the international
adoption of EHRs and their uptake by healthcare
providers. Vodicka et al. (2013) carried out a sur-
vey on considering online access to patient records
and found that approximately one-third of partici-
pants had concerns about the security and privacy
of their health records. Moreover, according to “the
2017 cost of a data breach study: global overview”
report (survey done by IBM and Ponemon Institute
(Snell, 2017)), a report on “improving cybersecurity
in the healthcare industry” (US Department of Health
and Human Services et al., 2017), and a report entitled
“hacking healthcare IT in 2016 lessons the healthcare
industry can learn from the opm breach” (Institute
for critical infrastructure technology, 2016), health-
Resource
1
Resource
2
Resource
3
Amy personal
information
Contact number,
Address, Marital status
Amy personal
information
Contact number,
Address, Marital status
Amy is attractive!
I can get more
information about
her easily.
Unethical
access
Alex
Dean
Cara
Figure 2: Insider threat.
care data breach costs are the second highest category
in comparison. Breaches include stealing protected
health information for later use to launch numerous
fraud attacks on related medical parties. Thus, the
findings of these studies demonstrate that the security
and privacy concerns regarding EHRs need to be ad-
dressed before EHRs can be fully accepted by patients
and health providers.
The “Health Insurance Portability and Account-
ability Act” (HIPAA) (Nosowsky and Giordano,
2006) and “code of conduct for information secu-
rity” (Norwegian Directorate of eHealth, 2017) are
examples for legislation to protect the privacy of pa-
tients’ medical records as well as ensure the way
health information is used, disclosed and maintained
by healthcare organizations and healthcare profes-
sionals. They provided a list of security and privacy
suggestions and legal requirements to address the
need to protect healthcare information. As a means
of overcoming authorization and improper access is-
sues associated with EHRs, access control models
such as role-based access control (RBAC) (Ferraiolo
et al., 2001), attribute-based access control (ABAC)
(Hu et al., 2014) and others (Tolone et al., 2005) may
prove to be the answers.
3 ACCESS CONTROL MODELS
Access control is the most popular approach for de-
veloping an active form of mitigating authorization
threats (Rubio-Medrano et al., 2013; Tolone et al.,
2005). The most challenging concern with deploy-
ing access control in a collaborative healthcare en-
vironment is deciding on the extent and limit of in-
formation sharing. For instance, if the main physi-
Sharing With Care - Multidisciplinary Teams and Secure Access to Electronic Health Records
381
cian is treating a patient with sensitive data, the ques-
tion is which data should be disclosed to an assist-
ing practitioner so that collaboration can be effective,
and which should be hidden to safeguard the patient’s
privacy (Fern
´
andez-Alem
´
an et al., 2013). According
to our survey and others’ (Fern
´
andez-Alem
´
an et al.,
2013), it appears that, RBAC is a popular model for
access control and it widely employed in medical in-
dustry (Rostad et al., 2007). RBAC provides security
by utilizing the role of a person in a particular organi-
zation. However, it is quite difficult to define access
when considering other relevant aspects beyond the
one specified by role (e.g., time and location). This
was one of the motivations for developing ABAC (Hu
et al., 2014). The result of using RBAC is not quite
satisfactory. The main reason is that, among others,
RBAC are not well-suited with EHRs to handling un-
planned and dynamic events (e.g., when healthcare
provider asked for second opinions from other health-
care provider) (Fern
´
andez-Alem
´
an et al., 2013; Ros-
tad et al., 2007).
It can be concluded that current access control
models in most previous studies do not support poli-
cies for collaborative MDT environments. This lim-
its these methods to single access to the resources
in centralized environments. Thus, extended fine-
grained components need to be developed for collabo-
rative healthcare MDT environments (Abomhara and
Køien, 2016).
4 SECURE SHARING OF EHRs
To combine the strengths of both RBAC and ABAC
approaches without being hindered by their limita-
tions, work-based access control (WBAC) has been
proposed by introducing the team role (section 4.1)
concept and modifying the team user-role assignment
model from RBAC and ABAC (Abomhara et al.,
2017; Abomhara and Køien, 2016; Abomhara and
Yang, 2016). WBAC enforces a three-layer access
control that applies RBAC, a secondary RBAC and
ABAC. The secondary RBAC layer, with extra roles
extracted from the MDT work requirements, is added
to manage the complexity of cooperative engage-
ments in the healthcare domain. Policies related to
collaboration and MDT’s work are encapsulated in
this coordination layer to ensure that the RBAC layer
and ABAC layer are not overly burdened. The WBAC
model is defined in terms of individuals being as-
signed to roles or teams, team members being as-
signed to team roles, work being assigned to teams
and permissions being associated with roles and team
roles. Role and team role are used in conjunction with
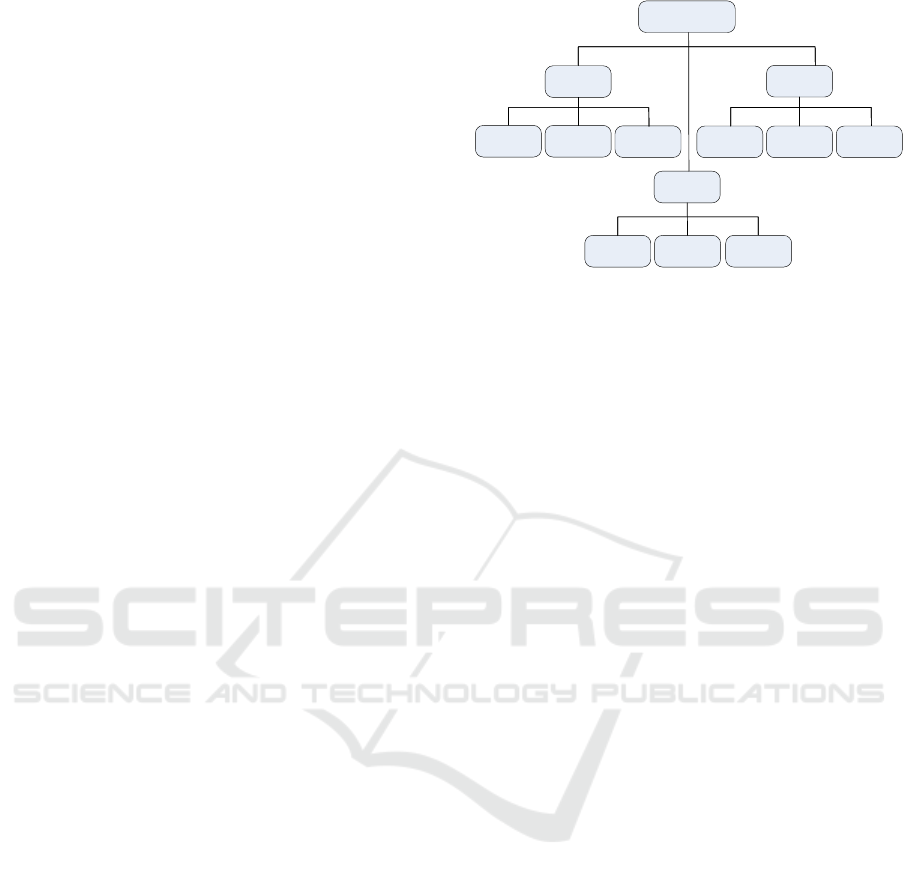
Role
Management
Action
Thought
Coordinator
Networker
Doer Motivator
Thinker Evaluator
Mediator
Mentor
Checker
Figure 3: Taxonomy of team role (Abomhara and Køien,
2016).
dealing with access control in dynamic collaborative
environments.
4.1 Team Role Classification
Hospital personnel roles are often simplistically split
into medical practitioners, nurses and administrators,
to name a few. However, their roles in an MDT can
be further categorized using the team role theory (so-
called also Belbin’s team roles) (Belbin, 2012; Bel-
bin, 2010).
The effectiveness of MDTs is limited unless they
have a clear role and position in organizational struc-
ture of the service. Belbin’s team role theory is
very useful for higher level team building processes,
as it helps an experienced facilitator identify pat-
terns that exist within any team and thus underpin
their strengths and weaknesses. In previous works
(Abomhara et al., 2017; Abomhara and Køien, 2016;
Abomhara and Yang, 2016), the MDT was segregated
into thought, action and management (Figure 3)
based on contributions to the MDT work.
• Thought denotes a role that is dominated mostly
in thinking, analyzing problems and/or providing
technical expertise. To be a successful thought
collaborator, the person may need to understand
the medical predicament in detail without neces-
sarily knowing the patient. A worker in this role
could be involved in devising strategies to con-
front particular medical enigmas. Thus, a cardi-
ology specialist may offer his expertise regarding
the best practices of performing a heart transplant
on a child without being involved in the actual op-
eration.
• The action role pertains to team leaders (e.g., pri-
mary doctor) and members who are involved in
the direct care of the patient, such as meeting
the patient for a medical checkup. These team
members like physicians and nurses are generally
HEALTHINF 2018 - 11th International Conference on Health Informatics
382

based where the patient receives treatment. Hav-
ing an action role usually implies close interaction
with the patient. Nevertheless, discretion is still
feasible with care.
• The management category comprises personnel
who are mostly involved in managing others (e.g.,
guide, listen, delegate, and solve conflicts). These
types of collaborators are adept at coordinating
teamwork. For example, in conflict management,
they may have to resolve series of opposing di-
agnoses made by medical practitioners that may
otherwise escalate into serious altercations. In
this regard, such personnel’s need for information
is inwardly oriented. They have a greater need
to know personal information about other team
members rather than about patients.
4.2 Resource Classification
Medical record classification requires a great deal of
effort and skills to accomplish. This is due to prob-
lems like, for one, medical records containing a wide
range of information (Thomas, 2009), not all of which
may be shareable (Asif et al., 2007). It may include
personal names, phone numbers, addresses, appoint-
ment schedules, to do lists, as well as medical history
and surgical history records, to name a few. Some
elements of this information may be confidential and
sensitive, while others may be open for access. In
an environment that supports resource sharing (Fig-
ure 1(b)), unwanted parties could retrieve confiden-
tial information (Figure 2), thus causing information
leakage and leading to the violation of patient privacy.
Second, healthcare providers cannot decide on what
appropriate information is really necessary in a pa-
tient’s treatment case.
In general, information sharing is required for
treatment; therefore, healthcare providers may use
and disclose patient records on the patient’s treatment
without that patient’s authorization. This may occur
during consultation between healthcare providers re-
garding a patient or patient referral by one provider
to another. However, in most cases when health-
care providers are dealing with sensitive informa-
tion regarding the patient, patient authorization is re-
quired for disclosure, for instance, the disclosure of
psychotherapy notes. According to HIPAA Privacy
Rule (US Department of Health and Human Services
et al., 2014), psychotherapy notes are treated differ-
ently from other mental health information. This is
because they contain particularly sensitive informa-
tion and they are the therapist’s personal notes, which
are not typically required or useful for treatment or
healthcare operation purposes, other than by the men-
tal health professional who created the notes.
It can be said that the amount of information
healthcare providers need to complete their tasks may
vary greatly. The number of medical records a health-
care provider needs to access over a certain period of
time depends on many factors, including the number
of patients they serve, the case they are working on,
and so on. Moreover, such factors vary among health-
care providers and may change from time to time. It
is thus very hard to determine how much risk should
be tolerated for a healthcare provider, if the healthcare
provider believes that knowing more information that
is relevant to their patients conditions enables them to
make better decisions (Rostad et al., 2007).
A realistic way of handling collaboration risks
is to minimize the discrepancy between granted and
required access based on the “minimum necessary”
standard to use and disclose records for treatment
(Agris, 2014). Thus, resources within WBAC are
mainly divided into two types: protected and pri-
vate resources. Protected resources can be shared
within an MDTs work. This depends on whether
the collaborative work needs access to the protected
resources. Contrary to the former type, private re-
sources are highly classified pieces of information in
medical records that would be shared during the MDT
work only if needed. As such, the spreading of ac-
cess control on the basis of collaboration will not af-
fect private resources. It is meant to safeguard cer-
tain confidential information from being leaked out
accidentally through collaborative means. Consider
the example of patient Amy given in section 2.1, in
WBAC model, it was assumed that personal informa-
tion (e.g. name, phone number, address, and/or ID,
etc) and any medical records unrelated to the current
medical case are private resources. In this case, only
the main practitioner (e.g., primary doctor) should be
aware of the patient’s personal information. The other
medical practitioners with supporting roles are given
only information essential for diagnosis (protected re-
source) based on their contributing roles.
4.3 Flow Model of WBAC
The WBAC model utilizes role, team role and WBAC
policies to perform an access control evaluation pro-
cess. First, it checks the access request to verify
whether the requesting user (healthcare provider) pos-
sesses a valid role specified in the system (first RBAC
layer). If the requesting user holds the right role,
WBAC will check the permission associated with
the role and then inspect the rule(s) within the main
WBAC policies for additional constraints (ABAC
layer) on access. In other models such as RBAC, fail-
Sharing With Care - Multidisciplinary Teams and Secure Access to Electronic Health Records
383

ure in this stage results in the complete termination of
the decision process. WBAC, however, treats this dif-
ferently. If the requesting user does not hold a valid
role (in most cases, the requesting user might be an
outsider who is invited to collaborative work and does
not hold a role in the organization), WBAC investi-
gates further to determine whether the requesting user
is part of the collaborative work (a secondary RBAC
layer). If so, the respective user’s team role is ex-
tracted and examined for whether the requesting user
possesses a valid team role over the resource. WBAC
also checks the permission associated with the team
role and checks the rule(s) within WBAC collabora-
tive policies for additional constraints (ABAC layer)
on access.
According to the security and performance analy-
sis of the proposed model (Abomhara et al., 2017),
WBAC is suitable for collaborative healthcare sys-
tems in addressing information sharing and informa-
tion security matters. It caters to the requirements of
access control in collaborative environments and pro-
vides a flexible access control model without compro-
mising the granularity of access rights. Moreover, this
model is secure and easy to manage for supporting co-
operative engagements that are best accomplished by
organized, dynamic teams of healthcare practitioners
within or among healthcare organizations whose ob-
jective is to achieve a specific work (patient treatment
case).
5 DISCUSSION AND
OBSERVATIONS
MDTs are likely to benefit everyone, but for such
teams to keep working well, skills and sufficient coor-
dination as well as resource management are needed.
EHRs can improve the work within MDTs, through
which medical providers share healthcare informa-
tion more easily and work together as a team to solve
particular medical cases. However, the EHRs might
also leave patients more susceptible to privacy viola-
tion where confidential information is improperly ac-
cessed and exploited by MDT members. It is chal-
lenging to predefine all access needs for MDTs based
on the subject-object model. One example of such
a situation is explained in our example (section 2.1),
which may not be predictable and it would be hard
to express the condition of who should join the MDT.
Moreover, in deciding on the extent and limit of re-
source sharing, for instance, in the case of Amy’s treat-
ment (section 2.1), which sensitive data should be dis-
closed to an assisting practitioner so collaboration can
be effective, and which should be hidden to safeguard
the patient’s privacy?
There are certain observations that we have
learned from the previous studies that should be con-
sidered before we could decide on the security model.
Observations as follows:
1. What do patients and healthcare providers
want from EHRs? From the patient perspec-
tive, patients found EHRs are useful and accept-
able. The majority were concerned about security
and confidentiality, including access and disclo-
sure of their records. It’s clear that, on the one
hand, patients want EHR systems to make health
data accessible, available and easy for healthcare
provider to find and use. However, on the other
hand, they also want to be informed regarding
access, disclosure and use of their data. From
the perspective of healthcare providers, they want
EHRs to make their practice work better, easy to
manage and be able to coordinate patient care eas-
ily by communicating with one another, deciding
who will be doing what interventions and then
sharing the information across all of them in a way
that EHRs really facilitate (O’Daniel and Rosen-
stein, 2008).
2. What is good for security is not necessary use-
ful for MDT practice? Bridging the gap between
security requirements and MDT practice is a crit-
ical focus for security researchers. This is a chal-
lenge because what is good for security is not al-
ways what healthcare providers want. On the one
hand, healthcare provider (members of MDTs)
need tools such as EHRs to provide, among oth-
ers, an easy sharing of health information, real-
time access to health records and should be easy
to use. On the other hand, security seeks to en-
sure the healthcare records’ availability, confiden-
tiality, and integrity while providing them only
to those with proper access rights. Security re-
searchers, specifically in access control and au-
thorization, have made the best effort to propose
an access control model that balances between se-
curity and MDT requirements. Yet, these models
do not always meet the needs of MDTs due to the
inconsistencies that exist within the MDT work-
flow and these models’ approaches.
3. How do MDTs form and develop? In general,
many studies (Monteleone et al., 2016; Jnr, 2011;
Firth-Cozens, 2001) have discussed the need and
the effectiveness of MDTs in healthcare delivery.
Yet, however, few address the development of the
MDTs in healthcare organization. It would be
worthwhile if studies could also be conducted on
the forming, storming, norming and performing
HEALTHINF 2018 - 11th International Conference on Health Informatics
384

of MDTs similar to other industries (Arrow et al.,
2000).
4. EHRs require better ways to securely exchange
information: EHRs are promising to be an ideal
solution for addressing the information exchange
challenges that today’s MDTs are facing. It pro-
vides an automated and fast information exchange
to healthcare providers within or among health-
care organizations. However, security and privacy
mechanisms to ensure secure interoperable EHR
applications are slowly beginning to emerge. For
access (uses and disclosures) of patient health in-
formation, access control policies and procedures
must be in place to identify and authorize a health-
care provider or MDT member who needs access
to the health information to carry out their job du-
ties, the type of information needed, and condi-
tions appropriate to such access. For example, ac-
cess control policies should permit only doctors,
or other involved in treatment, to have access to
patient medical records, as needed.
5. Legislation and regulation of electronic ex-
change of health information: According to
HIPPA (Nosowsky and Giordano, 2006) and the
code of conduct for information security (Nor-
wegian Directorate of eHealth, 2017), healthcare
providers should inform and obtain a patient’s
permission (e.g., consent or authorization) on how
the patient’s records are used or disclosed. Un-
der the terms of HIPAA (Agris, 2014), a valid au-
thorization to use or disclosure health information
must contain “a description of the information to
be used or disclosed”; “the name of the person or
entity authorized to make the use or disclosure”;
“the name of the person or entity to whom the dis-
closure may be made”; “a description of each pur-
pose of the requested use or disclosure”; “an expi-
ration date or expiration event” and “the signature
of the individual and date”.
As a result of this, it could be concluded that, if
we don’t coordinate the MDT and shared information,
we cannot coordinate the patient care, and if we don’t
coordinate the patient care, we will have inefficiency
and poor healthcare quality.
6 CONCLUSIONS
It is evident that EHRs have a great potential to sup-
port MDTs work, including but certainly not limited
to create, manage and share patient healthcare infor-
mation as well as facilitate an easy coordination and
communication between healthcare providers, thus
improving patient satisfaction and engagement. How-
ever, unauthorized disclosure and improper access
to patient healthcare records are a major concern of
this study, where sensitive healthcare data is shared
among a group of healthcare professionals within or
across organizations.
WBAC was proposed to address these concerns
and support the security and MDT requirements on
access control. The major contributions of the WBAC
model include ensuring that access rights are dy-
namically adapted to the actual needs of health-
care providers, and providing fine-grained control
of access rights with the least privilege principle,
whereby healthcare providers are granted minimal ac-
cess rights to carry out their duties.
REFERENCES
Abomhara, M., Gerdes, M., and Køien, G. M. (2015).
A stride-based threat model for telehealth systems.
Norsk informasjonssikkerhetskonferanse (NISK),
8(1):82–96.
Abomhara, M. and Køien, G. M. (2016). Towards an access
control model for collaborative healthcare systems.
In HEALTHINF’16, 9th International Conference on
Health Informatics, volume 5, pages 213–222.
Abomhara, M. and Nergaard, H. (2016). Modeling of work-
based access control for cooperative healthcare sys-
tems with xacml. In Proceedings of the Fifth in-
ternational conference on global health challenges
(GLOBAL HEALTH 2016), pages 14–21.
Abomhara, M. and Yang, H. (2016). Collaborative and
secure sharing of healthcare records using attribute-
based authenticated access. International Journal on
Advances in Security Volume 9, Number 3 & 4, 2016.
Abomhara, M., Yang, H., Køien, G. M., and Lazreg, M. B.
(2017). Work-based access control model for coop-
erative healthcare environments: Formal specification
and verification. Journal of Healthcare Informatics
Research, pages 1–33.
Agris, J. L. (2014). Extending the minimum necessary
standard to uses and disclosures for treatment: Cur-
rents in contemporary bioethics. The Journal of Law,
Medicine & Ethics, 42(2):263–267.
Alhaqbani, B. and Fidge, C. (2008). Access control re-
quirements for processing electronic health records.
In Business Process Management Workshops, pages
371–382. Springer.
Arrow, H., McGrath, J. E., and Berdahl, J. L. (2000). Small
groups as complex systems: Formation, coordination,
development, and adaptation. Sage Publications.
Asif, K., Ahamed, S. I., and Talukder, N. (2007). Avoiding
privacy violation for resource sharing in ad hoc net-
works of pervasive computing environment. In Com-
puter Software and Applications Conference, 2007.
COMPSAC 2007. 31st Annual International, vol-
ume 2, pages 269–274. IEEE.
Sharing With Care - Multidisciplinary Teams and Secure Access to Electronic Health Records
385

Bain, C. (2015). The implementation of the electronic med-
ical records system in health care facilities. volume 3,
pages 4629–4634. Elsevier.
Belbin, R. M. (2010). Management teams: Why they suc-
ceed or fail. Human Resource Management Interna-
tional Digest, 19(3).
Belbin, R. M. (2012). Team roles at work. Routledge.
Chao, C.-A. (2016). The impact of electronic health records
on collaborative work routines: A narrative network
analysis. International journal of medical informatics,
94:100–111.
Coorevits, P., Sundgren, M., Klein, G. O., Bahr, A., Claer-
hout, B., Daniel, C., Dugas, M., Dupont, D., Schmidt,
A., Singleton, P., et al. (2013). Electronic health
records: new opportunities for clinical research. Jour-
nal of internal medicine, 274(6):547–560.
Fabian, B., Ermakova, T., and Junghanns, P. (2015). Collab-
orative and secure sharing of healthcare data in multi-
clouds. Information Systems, 48:132–150.
Fern
´
andez-Alem
´
an, J. L., Se
˜
nor, I. C., Lozoya, P.
´
A. O., and
Toval, A. (2013). Security and privacy in electronic
health records: A systematic literature review. Journal
of biomedical informatics, 46(3):541–562.
Ferraiolo, D. F., Sandhu, R., Gavrila, S., Kuhn, D. R., and
Chandramouli, R. (2001). Proposed nist standard for
role-based access control. ACM Transactions on In-
formation and System Security (TISSEC), 4(3):224–
274.
Firth-Cozens, J. (2001). Multidisciplinary teamwork: the
good, bad, and everything in between.
Hu, V. C., Ferraiolo, D., Kuhn, R., Schnitzer, A., Sandlin,
K., Miller, R., and Scarfone, K. (2014). Guide to at-
tribute based access control (abac) definition and con-
siderations. NIST Special Publication, 800:162.
Institute for critical infrastructure technology (2016). Hack-
ing healthcare it in 2016 lessons the healthcare indus-
try can learn from the opm breach. Institute for critical
infrastructure technology.
Jnr, G. O. A. (2011). The effect of multidisciplinary team
care on cancer management. Pan African Medical
Journal, 9(1).
Kim, M. M., Barnato, A. E., Angus, D. C., Fleisher, L. F.,
and Kahn, J. M. (2010). The effect of multidisci-
plinary care teams on intensive care unit mortality.
Archives of internal medicine, 170(4):369–376.
Liu, L. S., Shih, P. C., and Hayes, G. R. (2011). Barriers
to the adoption and use of personal health record sys-
tems. In Proceedings of the 2011 iConference, pages
363–370. ACM.
Monteleone, P. P., Rosenfield, K., and Rosovsky, R. P.
(2016). Multidisciplinary pulmonary embolism re-
sponse teams and systems. volume 6, page 662. AME
Publications.
Norwegian Directorate of eHealth (2017). Code of conduct
for information security the healthcare and care ser-
vices sector.
Nosowsky, R. and Giordano, T. J. (2006). The health insur-
ance portability and accountability act of 1996 (hipaa)
privacy rule: implications for clinical research. Annu.
Rev. Med., 57:575–590.
O’Daniel, M. and Rosenstein, A. H. (2008). Professional
communication and team collaboration.
Probst, C. W., Hunker, J., Gollmann, D., and Bishop, M.
(2010). Insider Threats in Cyber Security, volume 49.
Springer Science & Business Media.
Rostad, L., Nytro, O., Tondel, I., and Meland, P. H. (2007).
Access control and integration of health care systems:
An experience report and future challenges. In Avail-
ability, Reliability and Security, 2007. ARES 2007.
The Second International Conference on, pages 871–
878. IEEE.
Rubio-Medrano, C. E., D’Souza, C., and Ahn, G.-J. (2013).
Supporting secure collaborations with attribute-based
access control. In Collaborative Computing: Net-
working, Applications and Worksharing (Collaborate-
com), 2013 9th International Conference Conference
on, pages 525–530. IEEE.
Smaradottir, B., Gerdes, M., Martinez, S., and Fensli, R.
(2016a). The eu-project united4health: User-centred
design of an information system for a norwegian
telemedicine service. Journal of telemedicine and
telecare, 22(7):422–429.
Smaradottir, B., Martinez, S., Holen-Rabbersvik, E.,
Vatnøy, T. K., and Fensli, R. W. (2016b). Usabil-
ity evaluation of a collaborative health information
system. lessons from a user-centred design process.
In HEALTHINF’16, 9th International Conference on
Health Informatics, volume 5, pages 306–313.
Smaradottir, B. F., Martinez, S., Holen-Rabbersvik, E., and
Fensli, R. (2015). ehealth-extended care coordina-
tion: Development of a collaborative system for inter-
municipal dementia teams: A research project with a
user-centered design approach. In International Con-
ference on Computational Science and Computational
Intelligence (CSCI2015), pages 749–753. IEEE.
Snell, E. (2017). Healthcare data breach costs highest for
7th straight year. HealthITSecurity.com.
Thomas, J. (2009). Medical records and issues in negli-
gence. Indian journal of urology: IJU: journal of the
Urological Society of India, 25(3):384.
Tolone, W., Ahn, G.-J., Pai, T., and Hong, S.-P. (2005). Ac-
cess control in collaborative systems. ACM Comput-
ing Surveys (CSUR), 37(1):29–41.
United4Health (2017). European commission competitive-
ness innovation programme.
US Department of Health and Human Services et al. (2014).
Hipaa privacy rule and sharing information related to
mental health.
US Department of Health and Human Services et al. (2017).
Health care industry cybersecurity task force.
Vawdrey, D. K., Wilcox, L. G., Collins, S., Feiner, S.,
Mamykina, O., Stein, D. M., Bakken, S., Fred, M. R.,
Stetson, P. D., et al. (2011). Awareness of the care
team in electronic health records. Appl Clin Inform,
2(4):395–405.
Vodicka, E., Mejilla, R., Leveille, S. G., Ralston, J. D.,
Darer, J. D., Delbanco, T., Walker, J., and Elmore,
J. G. (2013). Online access to doctors’ notes: patient
concerns about privacy. Journal of medical Internet
research, 15(9).
HEALTHINF 2018 - 11th International Conference on Health Informatics
386
