
A Remote Home Monitoring System to Support Informal Caregivers
of People with Dementia
Stefan Lentelink
1
, Monique Tabak
1,2
, Boris van Schooten
1
, Dennis Hofs
1
,
Harm op den Akker
1
and Hermie Hermens
1,2
1
Telemedicine Group, Roessingh Research and Development, Enschede, The Netherlands
2
Telemedicine Group, University of Twente, Enschede, The Netherlands
Keywords: Dementia, Informal Caregiver, Aging in Place, eHealth, Health Informatics, Ambient Assisted Living,
Remote Home Monitoring.
Abstract: Informal caregivers of people with dementia have a high risk of becoming overburdened. Health informatics
for aging in place can provide them support by deploying unobtrusive remote home monitoring systems to
assess real-time events and monitor changes in the behavior of the person with dementia (PwD). In this paper,
we describe the concept, development, and evaluation of an intelligent remote Home Monitoring System
(HMS) that provides support to informal caregivers by giving key information related to the health and
independent living of the PwD. The HMS consists of a Sensor System that monitors low-level behaviors of
the PwD, a Decision Support System that translates this into high-level behaviors, and a connected
Smartphone Application that allows the caregiver to receive notifications, review behavioral information at a
glance, and facilitates the collaborative care process between informal caregivers. The final HMS prototype
was evaluated and scored high in terms of usability and quality of the Smartphone Application. The Sensor
System showed no significant flaws during testing, and the Decision Support System is considered a viable
proof of concept. The next step is to evaluate the HMS in a real-life setting in terms of offering peace of mind
and reducing the burden of care.
1 INTRODUCTION
The world population is aging, resulting in an
increasing number of people suffering from dementia.
In the Netherlands, 1 in 5 people develop dementia
(VUmc Alzheimercentrum et al. 2012). In its early
stages, people are able to remain at home with the
support of informal caregivers who provide the
majority of care, and who have a key role in
determining the person’s wellbeing (Ministry of
Health Welfare and Sport et al. 2009). The
dependency on informal caregivers in society is
increasing, many of whom face difficulties in their
caregiving tasks and are (at high risk of becoming)
overburdened (Ministry of Health Welfare and Sport
et al. 2009; VUmc Alzheimercentrum et al. 2012).
Providing them with sufficient support is therefore of
great importance, but also to ensure that those with
dementia can continue to live at home longer.
Technological innovations that promote aging in
place, such as Ambient Assisted Living (AAL), could
provide a solution by implementing unobtrusive
remote home monitoring systems that employ a
network of sensors to assess real-time events and
monitor changes in the behavior of a person. AAL has
the potential to promote the quality of life and safety
for people with dementia, give peace of mind to the
informal caregivers, and promote independence and
autonomy for both target groups (Alzheimer’s
Society 2017). This fits well with informal
caregivers’ need for reassurance in terms of
(Instrumental) Activities of Daily Living ((I)ADL)
and safety in the home of the person with dementia
(Kirsi et al. 2004; Pollitt et al. 1991; Bank et al. 2006;
Nolan et al. 2002).
However, the majority of AAL and related
systems found in systematic reviews do not report on
informal caregivers as end-users (Ienca et al. 2017;
Liu et al. 2016; Carswell et al. 2009). This is also
reflected in studies on caregiver burden (Peeters,
Werkman and A Francke 2014; Peeters, Werkman
and AL Francke 2014; Zwaanswijk et al. 2013;
Miranda-Castillo et al. 2013; Peeters et al. 2010),
94
Lentelink, S., Tabak, M., Schooten, B., Hofs, D., Akker, H. and Hermens, H.
A Remote Home Monitoring System to Support Informal Caregivers of People with Dementia.
DOI: 10.5220/0006565300940102
In Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2018) - Volume 5: HEALTHINF, pages 94-102
ISBN: 978-989-758-281-3
Copyright © 2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
where informal caregivers are rarely surveyed
about using AAL to support them in care tasks.
Clearly, we can observe that support for informal
caregivers of people with dementia is needed.
As part of the H2020 project IN LIFE
(http://www.inlife-project.eu), we developed and
implemented a Health Monitoring Application, called
HELMA. This monitoring tool aims to inform
informal caregivers about the health and wellbeing of
the person with dementia over the long-term by
means of short frequent online questionnaires. To
improve the support for informal caregivers, and to
make the system more discreet and time-efficient, we
aim to improve HELMA with objective monitoring.
Motion and door sensors are proven to be useful
to quantify (changes in) ADL (Yang and Hsu 2012)
(Urwyler et al. 2017), are readily accepted in society
(Pol et al. 2016), appear to be almost unnoticed by
residents after installation in their homes (Nijhof et al.
2013), and are relatively simple and not too expensive
(Peetoom et al. 2015). In addition, simple estimation
methods can be used to quantify daily rhythms (Yang
& Hsu 2012), and measuring baselines are useful to
find changes in behavior (Glascock and Kutzik 2000).
As such, we have developed a Health Monitoring
System (HMS): a remote home monitoring system to
support informal caregivers of people with dementia
in their caregiving tasks. In this paper, we describe
the concept, development, and evaluation of this
remote home monitoring system.
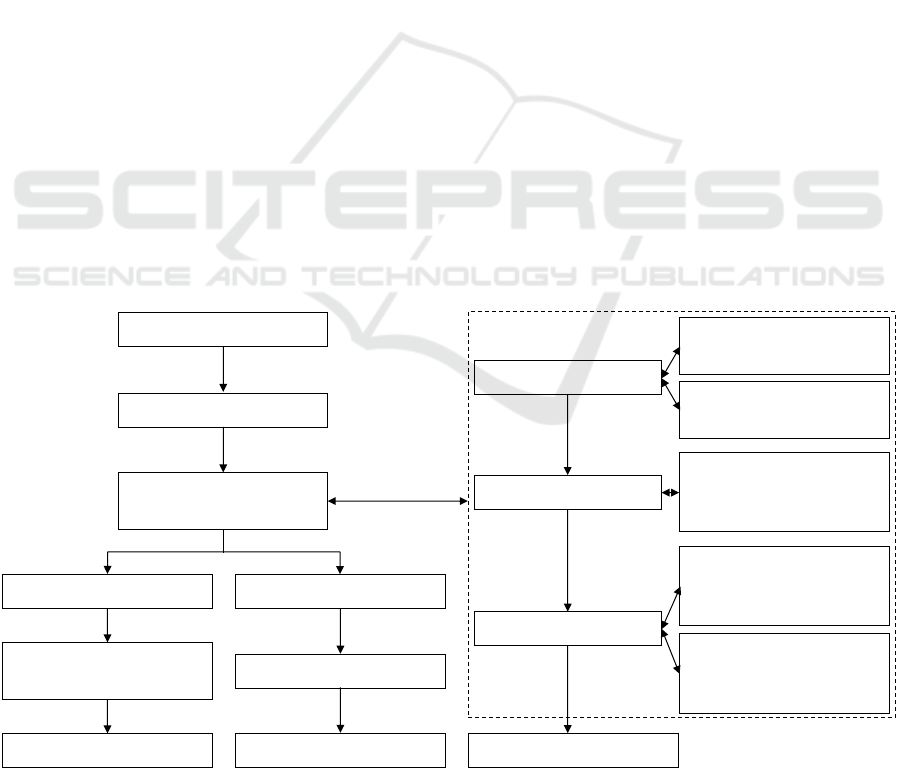
2 METHODS
The work described in this paper is based on an
iterative, user-centered design approach as shown in
Figure 1. By involving potential end-users in the
design process, we aim to increase the usability and
usefulness of the developed system. The HMS
consists of three main components: (1) Smartphone
Application; (2) Sensor System; and (3) Server.
First, we performed a state-of-the-art study by
searching in among others scientific databases
(e.g., Scopus, PubMed, and ScienceDirect) on the
topics of dementia, informal caregivers, remote home
monitoring, user interface design, and state-of-the-art
of remote home monitoring systems. Based on our
findings we developed a scenario following the
approaches of PACT (People; Activities; Context;
and Technology) (Huis in ‘t Veld et al. 2010) and
FICS (Function and events; Interactions and usability
issues; Content and structure; and Style and
aesthetics) (Benyon and Macaulay 2002). Starting
from the scenario, potential end-users were involved
to collect, elaborate, and refine the HMS
requirements. The end-users were contacted via local
healthcare organizations, and consisted of small
groups based on the assumption that the best results
in terms of usability testing come from no more than
5 end-users and performing as many small tests as
possible (Nielsen and Landauer 1993). During the
evaluations, which were divided into three phases, the
Smartphone Application was central.
Figure 1: General iterative design process of the HMS.
Evaluation Smartphone Application
Phase 3
Literature
Scenario (PACT & FICS)
Functional & technical
requirements
Available systems
Decision Support System
Integration
controller & sensors
Technical evaluation
Sensor System
Server
Phase 1
Semi-structured interview:
(in)formal caregivers (n=3)
Low-fidelity prototype
Semi-structured interview:
(in)formal caregivers (n=3)
Pase 2
Semi-structured interview,
tasks, and SUS:
(in)formal caregivers (n=6)
High-fidelity prototype
Semi-structured interview,
tasks, SUS, and uMARS:
non-caregivers (n=5)
Final prototype
Smartphone Application
Semi-structured interview,
tasks, SUS, and uMARS:
(in)formal caregivers (n=5)
A Remote Home Monitoring System to Support Informal Caregivers of People with Dementia
95

Smartphone Application: In phase 1, we drafted
the first requirements of the HMS and created a low-
fidelity prototype of the application based on the
scenario. The prototype was evaluated in two
successive sessions using semi-structured interviews
on demographics, HMS functionalities, and the
designed prototype. Each session included two
informal caregivers of people with dementia and one
dementia case manager (total n=6).
In phase 2, a high-fidelity prototype was created
for Android-based smartphones. The prototype was
evaluated using a mixed-methods approach,
including a semi-structured demographics interview,
task-based think-aloud protocol, controlled
observation, System Usability Score (SUS) (Brooke
1996), and a semi-structured interview in terms of
usefulness. The evaluation included the four informal
caregivers and two case managers from phase 1.
In phase 3, a final prototype was created
corresponding to the approach in phase 2. In addition,
the evaluation included two successive sessions and
the User Version of the Mobile Application Rating
Scale (uMARS) (Stoyanov et al. 2016) (using
multiple-forward translation). The first session
included five non-caregivers, and the second session
included three informal caregivers of people with
dementia and two dementia case managers.
The resulting functional requirements of the HMS
were prioritized by the first author (SL).
Sensor System: Based on the requirements, we
searched for a suitable Sensor System based on
current systems in literature and commercially
available systems. The Sensor System should have a
suitable controller with open API, bi-directional
communication, support for motion and door sensors,
and should be commercially available in the
Netherlands. The necessary motion and door sensors
should be simple, small, compatible with the chosen
controller, and commercially available in the
Netherlands.
Server: The Server consists of the Decision
Support System (DSS), which interprets the data
collected by the Sensor System, and the Database
Server. For the DSS, the requirements were used as a
guiding principle to determine how and what should
be monitored.
The technical evaluation of the DSS, and indirect
of the Sensor System, was conducted in a 5-day in-
home test where the first author (SL) annotated all in-
home activities (see Section 7), while being
monitored by the Sensor System (see Figure 5). The
outcome of the annotations was compared to the data
of the DSS to explore the reliability of the system.
Table 1: Functional requirements of the HMS; showing five
high-priority examples.
#
Functional requirement – HMS
The HMS should:
F1
… support multiple users
F2
… show information about events and behavioral
changes
F3
… differentiate between normal, abnormal, and
alarming situations
F4
… include a shared calendar
F5
… include a chat function
3 HMS CONCEPT
The HMS concept can be described as follows:
The Health Monitoring System includes multiple
wireless sensors that can be easily placed in the home
of the person with dementia (i.e., the resident). All
these sensors together unobtrusively monitor the
activities and behavioral changes of this person.
The informal caregivers will be remotely informed
via a smartphone application about the home
situation, and receive notifications upon meaningful
events and behavioral changes regarding the person
they care for.
Table 1 shows a selection of five high-priority
functional requirements of the HMS (as determined
by the first author (SL), based on functionality,
desirability, and feasibility). The original functional
requirements varied in terms of specificity, ranging
from for example “should support multiple users” to
“should only display the latest event or notification in
the home screen”. The functional requirements with
respect to the parameters to be monitored by the HMS
were divided into Detections (basic activities and
actions) and Patterns (slow changes and unusual
behavior). The Detections are shown in Table 2. The
Patterns are defined as deviations on the Detections,
based on the person’s standard behavior. An example
is: “The HMS should monitor deviations in the time
of going to bed”.
The Smartphone Application should primarily
provide key information (i.e., on location, activity,
sleeping, and eating) related to the health and
independent living of the person with dementia. It is
also important to support and improve communi-
cation between informal caregivers, for example by
including a shared calendar and chat function.
The Sensor System should include multiple
wireless sensors that can be easily placed in the home
of the person with dementia. All these sensors
together should unobtrusively monitor the activities
HEALTHINF 2018 - 11th International Conference on Health Informatics
96
and behavioral changes of this person. The sensors
should be simple, small, and largely respect privacy.
Finally, the Server should be a secure
environment for the collected data. In addition, the
DSS should be reliable and complete in terms of the
activities and behaviors to be measured.
Table 2: Functional requirements of the HMS Detections.
#
Functional requirement – HMS Detection
The HMS should inform about location by monitoring:
D1
… leaving the house
D2
… outdoor location
The HMS should inform about sleeping by monitoring:
D3
… time of going to bed
D4
… time of getting out of bed
D5
… sleep duration
D6
… number of times and time out of bed
D7
… restlessness
The HMS should inform about activity by monitoring:
D8
… wandering
D9
… toilet usage
D10
… physical activity
D11
… social activity
The HMS should inform about eating by monitoring:
D12
… meals (breakfast, lunch, and dinner)
D13
… drinking
The HMS should inform about … by monitoring:
D14
… medication intake
D15
… personal hygiene
D16
… body weight
D17
… falling
D18
… appliances
D19
… fire alarm
D20
… in-home temperature
D21
… (unwanted) visitors
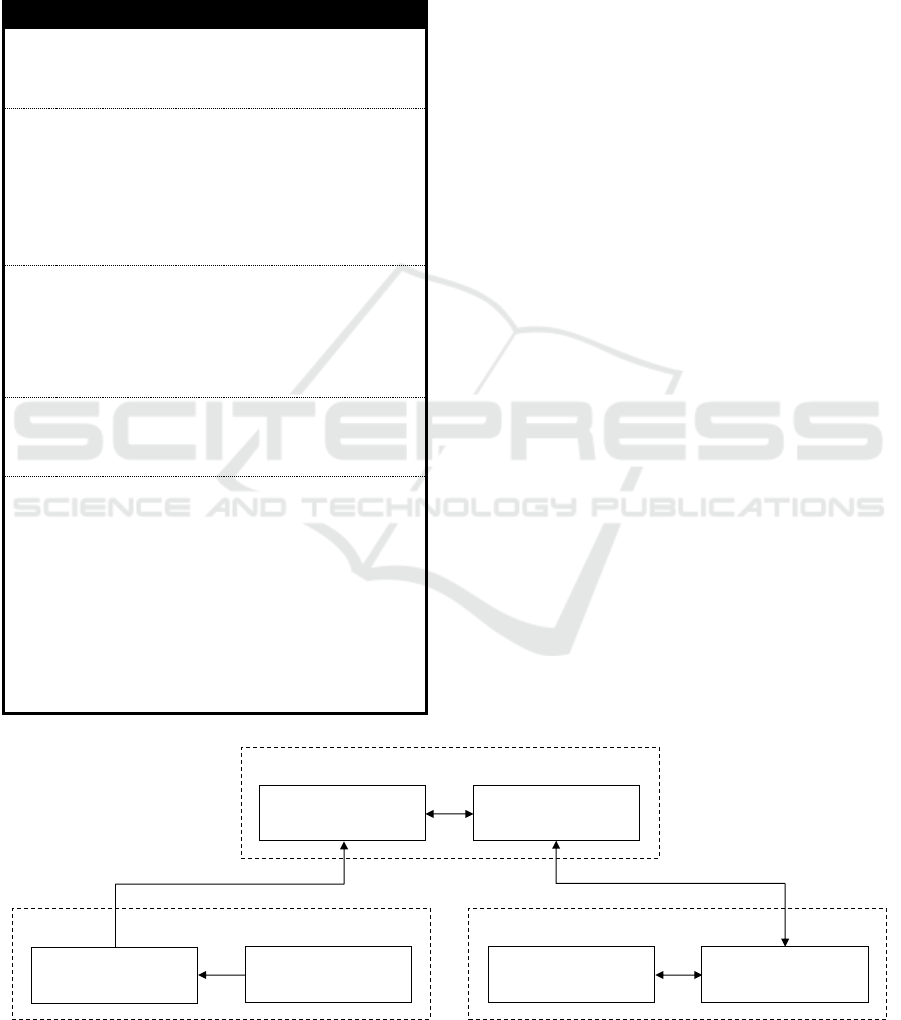
4 ARCHITECTURE
The architecture of the HMS consists of: (1) Sensor
System; (2) Server; and (3) Smartphone Application
(see Figure 2).
The Sensor System consists of a controller and
several door/motion sensors. It monitors the home of
the person with dementia (i.e., the resident) and sends
all sensor detections to the DSS.
The DSS receives and stores the sensor detections
received from the Sensor System. Algorithms then
analyze and process the data, and generate events.
The DSS can generate events on multiple levels (see
Section 7), which are written to the Database Server.
The Database Server consists of a MySQL back-
end and secure API that both communicate with the
DSS and the Smartphone Application. It contains the
data of all residents, and informal caregivers, based
on the DSS and Smartphone Application. The DSS
generates sensor events, whereas the Smartphone
Application generates chat messages and shared
calendar items. Every data record is linked to a
resident ID that determines the access control.
Informal caregivers can only access data from their
own resident.
The Smartphone Application consists of the Local
Database, which is automatically synchronized with
the Database Server, and the User Interface,
consisting of all the necessary components for the
user interface interaction. The Local Database is a
replication of part of the Database Server and only
contains relevant data for its user. The Local Database
allows the user to use the Smartphone Application
offline and improves the user experience.
Figure 2: Architecture of the HMS.
Server
Smartphone Application
Sensor System
Decision Support
System
Database Server
Controller
Sensors
User Interface
Local Database
A Remote Home Monitoring System to Support Informal Caregivers of People with Dementia
97

5 SMARTPHONE APPLICATION
The Smartphone Application consists of three main
components: (1) Home; (2) Calendar; and (3) Chat
(see Figure 3).
The Home screen displays clear information
regarding the person with dementia (i.e., the resident).
There are three states for displaying information:
(1) normal; (2) abnormal; and (3) alarming (see
Figure 4). In the normal state, general information is
displayed about the resident (e.g., “The resident went
to bed.”). In the abnormal state, information is
displayed which does not require immediate
attention, but must be kept an eye on (e.g.,
“The resident was 2 hours out of bed last night.”).
And in the alarming state, immediate action is
required (e.g., “The resident left the house at night!”).
An overview of all notifications is shown in Table 3.
The Home screen is also the gateway to many
other features of the application. Starting at the top,
there are four buttons. In order from left to right, the
Phone button allows the informal caregiver to call the
resident directly, but also to temporarily block the
calls from the resident. This measure is implemented
because some residents call their informal caregivers
extremely often, leading to frustration of the informal
caregiver. When the calls are blocked, the caller (i.e.,
the resident) will be redirected to the voicemail.
Informal caregivers are therefore advised to set a
reassuring voicemail beforehand. The Mute button
allows the informal caregiver to set all HMS
notifications to sound and vibrate, vibrate, or mute.
This does not affect other phone notifications. The
Connection button allows the informal caregiver to
check the connection with the HMS. And the Settings
button allows the informal caregiver to view and
adjust various system settings, such as Account,
Notifications, Calls, Events, and Installation. The
Home screen also contains a Menu button, allowing
the user to view current and historical notifications
about each of the Location, Activity, Sleeping, and
Eating domains (see Figure 4). The user can view all
aforementioned domains in a single view in
Overview. Each domain also gives the user the
opportunity to view data graphically per week,
month, quarter, or half year, with a view to inform
about behavioral changes. The Calendar gives
informal caregivers the opportunity to schedule
mutual appointments. And the Chat gives informal
caregivers the option to send each other messages.
The Smartphone Application follows the general
design principles to clearly show its users at a glance
all the necessary information.
The phase 3 evaluation with the final prototype
showed a median (range) SUS score of 87.50 (15.00),
and a uMARS score of 4.27 (0.73) with the
following subdomains: Engagement 4.00 (1.60);
Functionality 4.25 (0.75); Aesthetics 4.33 (1.00); and
Information 4.50 (1.00).
In addition, the interviews highlighted improve-
ments such as:
• The application should include the option to
assign caregivers to calendar items.
• The application should include the option to
add notes, photos, and contact information to
calendar items.
• The application should geographically
prioritize caregivers in case of alarming
situations, so that geographically close
caregivers are warned first. They should
however be able to forward the alarm.
Figure 3: Smartphone Application; showing the Calendar on the left, the Home screen in the center, and the Chat on the right.
HEALTHINF 2018 - 11th International Conference on Health Informatics
98
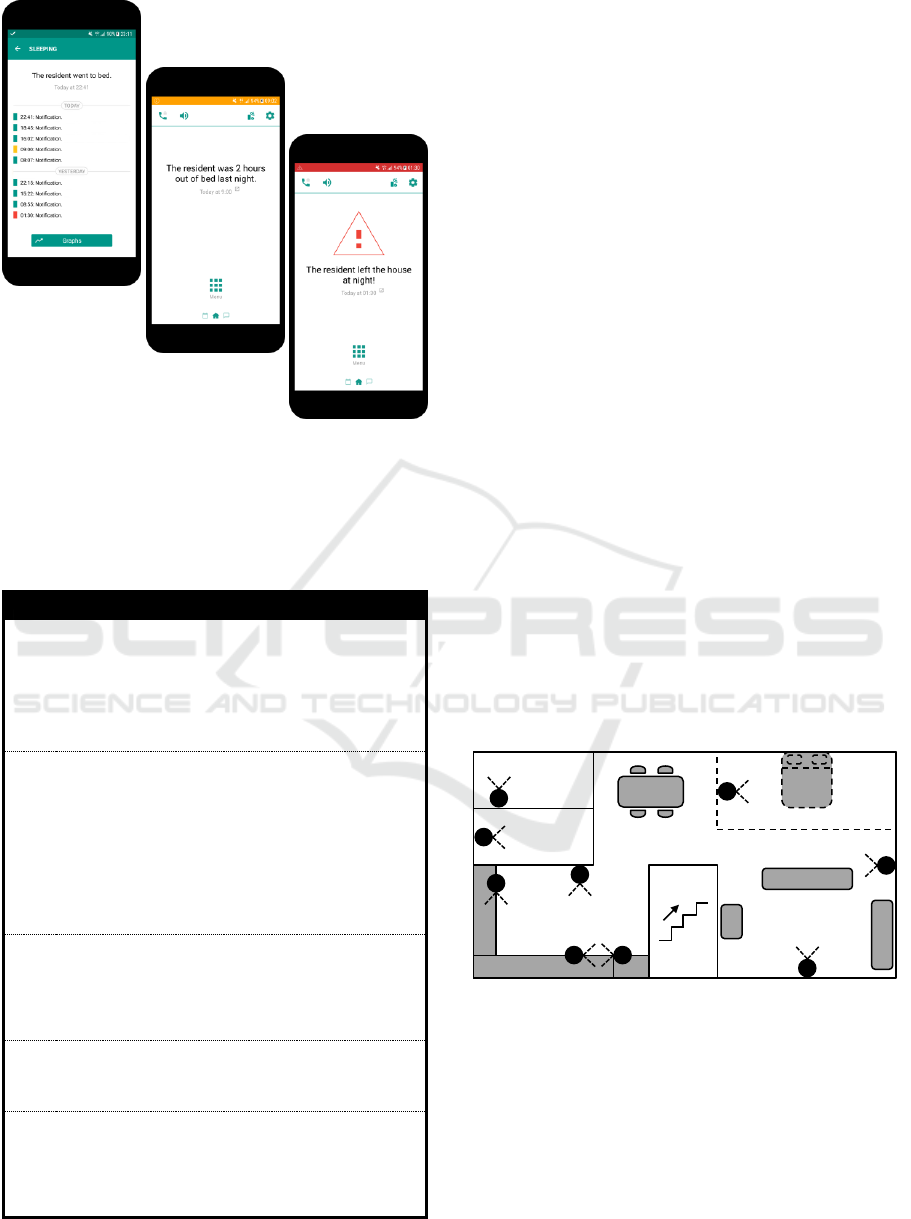
Figure 4: Smartphone Application; showing the Sleeping
overview on the left, the Home screen during an abnormal
event in the center, and the Home screen during an alarming
event on the right.
Table 3: Overview of the notifications implemented in the
Smartphone Application.
#
Smartphone Application notification
Location notification about:
N1
… coming / leaving home during the day
N2
… coming / leaving home at night
N3
… leaving home for a long period of time
N4
… not coming home at night
Sleeping notification about:
N5
… going to bed
N6
… getting out of bed
N7
… not going to bed
N8
… not getting out of bed
N9
… sleep duration
N10
… number of times and time out of bed
Activity notification about:
N11
… physical in- or overactivity
N12
… social inactivity
N13
… remarkable toilet usage
Eating notification about:
N14
… forgetting / preparing too many meals
(breakfast; lunch; and dinner)
Other notification about:
N15
… in-home temperature
N16
… new calendar item
N17
… new chat message
6 SENSOR SYSTEM
In our search for a controller, thirty products were
found varying from complete systems to standalone
controllers. Of these, the following five products
fitted the requirements: (1) Insteon; (2) Fibaro; (3)
Raspberry Pi + RaZberry + Domoticz; (4) Eedomus;
and (5) Vera. Other systems, such as Samsung
SmartThings, BeNext, Zipato, D-Link, Devolo,
Wink, and others, were unsuitable due to not being
available for the Netherlands, not having an open
API, or other reasons. The final choice was the Vera
Plus. In the search for suitable sensors, the
compatibility with this controller, and the in Section
3 mentioned requirements, were taken into account.
As a result, the Philiotech PST02-1A sensor was
chosen, based on its compatibility and suitability;
small, and combining both motion and door sensor.
In our test environment (see Figure 5), the
controller was placed in a location where all sensors
were still in range. The sensors were placed in each
room of interest, if possible at 1.60 m height, and
focused on the area were movement was most likely.
The sensors all monitored motion and/or
opening/closing of doors (see Section 7), and were
placed inside the appointed room for a more reliable
outcome (e.g., the toilet sensor measures motion
inside the toilet room).
Figure 5: Sensor System; showing the sensor locations.
7 DECISION SUPPORT SYSTEM
The DSS of the Server interprets the sensor data
collected from the Sensor System. Following the
various abstraction levels of the monitoring
requirements, the DSS subdivides information into
four levels: (1) raw sensor data; (2) location/action;
(3) events/alerts/statistics; and (4) trends. Information
Sensors
1. Front door
2. Toilet
3. Kitchen
4. Cutlery drawer
5. Kitchen cabinet
6. Fridge
7. Bedroom
8. Living room
9. Back door
Kitchen
Living room
1
7
5
2
8
3
6
9
4
Toilet
Hallway
Bedroom (upstairs)
A Remote Home Monitoring System to Support Informal Caregivers of People with Dementia
99

from each level is used to generate information for the
subsequent level.
At the location/action level, location refers to a
room in the house. Location cannot be tracked outside
the house, but the system can reliably detect when a
person leaves or enters the house. Actions defined at
this level are particularly cooking and sleeping.
Locations and actions are directly determined
from the door/motion sensors. We decided that the
DSS should consider the motion sensing as primary
data, as it reliably detects the presence of a person
(i.e., none of the errors were related to the motion
sensor). The door sensing is used as supplemental
data. A door opening and closing could mean a person
is either entering or leaving a room, and sometimes
doors remain open. A simple algorithm where a door
opening is assumed to mean a person leaves the room,
unless the room’s location sensor is triggered, is used.
Cooking can be determined by the fridge and on
operating either the cutlery drawer or kitchen cabinet.
We tested the location/action algorithm using the
annotated 5-day in-home test data. This test consisted
of the following annotations: leaving the house (via
front or back door); entering the house (via front or
back door); bedroom (entering or leaving); sleeping
(going to bed or going out of bed); cooking (start or
end); and toilet (entering or leaving).
For each location, we determined: minutes seen
(how many minutes being in the location were
correctly detected); minutes unseen (how many
minutes being in the location were not detected),
times seen (how many times being in the location
were correctly detected); times unseen (how many
times being in the location were never detected for the
duration the resident was there); and times false (how
many times being in the location were falsely
detected). The results are shown in Table 4.
Overall accuracy is quite high, 92%. Standing out
is the relatively high unseen minutes of the toilet. Our
findings are that the motion sensor picks up motion
slowly with respect to the typical duration of the toilet
visits (about 1-2 minutes). The number of visits is
however the most relevant for toilet use, which scores
well (only 12% total error rate). The same applies for
cooking, where times are far more relevant than
minutes (which is why minutes for cooking were not
calculated). The opposite applies to Bedroom/Sleep-
ing, Indoors (other), and Outdoors, where number of
times seen are not relevant for the alerts we generate.
For these, the number of false positives seem quite
high. This can be explained by the system registering
opening a door as leaving that room. When residents
do not actually leave the room, it takes only about 30
seconds before the motion sensor corrects that, but it
does clock up the number of false positives. This is a
trade-off between measuring minutes (necessary for
Bedroom/Sleeping, Indoors (other), and Outdoors)
and times (necessary for Toilet and Cooking).
Table 4: DSS location detection results;
Minutes seen is defined as the number of correctly detected
minutes in the location. Minutes unseen is defined as the
number of undetected minutes in the location. Times seen
is defined as the number of correctly detected times in the
location. Times unseen is defined as the number of
undetected times in the location. And times false is defined
as the number of falsely detected times in the location.
TOTAL is the sum of all above described parameters. The
corresponding percentage is calculated as follows: minutes
seen and minutes unseen are the result of dividing each by
the sum of minutes seen and minutes unseen; times seen,
times unseen, and times false are the result of dividing each
by the sum of times seen, times unseen, and times false.
Location/
action
Minutes
seen
Minutes
unseen
Times
seen
Times
unseen
Times
false
Toilet
12
26
38
3
2
Bedroom/
Sleeping
2637/
2271
354
23
2
20
Indoors
(other)
3123
140
118
5
42
Outdoors
2021
149
42
1
27
Cooking
-
-
14
1
5
TOTAL
7793
(0.92)
669
(0.08)
235
(0.69)
12
(0.03)
96
(0.28)
For the events/alerts/statistics level, the DSS
relies on the location to generate events. Most events
could be specified with the help of two types of
triggers: a time interval trigger (the resident visits a
specific location in a specific time interval); and a
timeout trigger (the resident remains in, or never
reaches, a specific location for a given duration). For
example, the resident leaving the house at night is
specified as a time trigger between 11.00 pm and 6.00
am, and the resident staying away for a long period is
specified as a timeout trigger on staying outdoors for
5 hours. In addition, the system must reliably model
the sleep/wake cycle in order to generate statistics
like sleep duration. The sleep/wake cycle progresses
when the resident goes to sleep or gets out of bed for
at least 45 minutes on particular times of the day.
Finally, the trends level uses the non-parametric
Mann-Kendall test (Kendall 1975), which enables
any trends to be detected in time-series data. The
Mann-Kendall test detects statistical significance and
direction of a trend. The test is conducted periodically
on statistics data, so the alpha value was lowered each
time using Bonferroni correction (Dunn 1961). We
did not have data to test the effectiveness of the
HEALTHINF 2018 - 11th International Conference on Health Informatics
100

algorithm, but we created simulated data to assess it.
We generated noisy data with a linear trend, with
daily values over a year, and we looked at the point at
which the algorithm could detect the trend in spite of
the noise. We used either normal or Poisson
distribution, depending on the statistics. For example,
wake-up time is normally distributed, and number of
toilet visits per day is a Poisson distribution. We
found that the algorithm could detect small trends at
low alpha levels even in cases where the trend was
not visually apparent. For example, a 30-minute shift
in wake-up time over a year with a standard deviation
of 1 hour was detected with α < 0.001. As such, we
consider the algorithm a viable proof of concept.
8 DISCUSSION & CONCLUSION
In our effort to improve HELMA with objective
monitoring, we conceptualized, developed, and
evaluated the Health Monitoring System (HMS). The
majority of identified requirements have been
implemented, and the HMS scored high in terms of
usability and quality of the Smartphone Application.
The Sensor System showed no significant flaws
during our tests, and the DSS is considered a viable
proof of concept.
The user-centered design resulted in a set of
requirements with emphasis on the provision of
relevant information in terms of the health and
independent living of the person with dementia by
monitoring their activities and behavioral changes,
and on the communication between informal
caregivers. In this way, the concept of the HMS
distinguishes itself from other systems (e.g., systems
found in systematic reviews (Ienca et al. 2017; Liu et
al. 2016; Carswell et al. 2009)) by focusing on
informal caregivers of people with dementia as
primary end-user. Moreover, the HMS aims to be a
versatile, unobtrusive, and privacy-friendly system.
The current HMS implements most of the
identified requirements. The requirements that have
not yet been addressed in this work are: outdoor
location; restlessness at night; wandering; drinking;
medication intake; personal hygiene; body weight;
falling; appliances; fire alarm; and (unwanted)
visitors. These requirements should be incrementally
added to the system to enrich the information
provision on health and independent living, and to
add the element of safety (indoors and outdoors).
Priority should be given to: outdoor location (e.g., by
using a GPS wristband); medication intake (e.g., by
using a medicine dispenser); falling (e.g., by using a
wristband or unobtrusive fall detection sensor);
appliances (e.g., by using a sensor on the stove); fire
alarm (e.g., by using a smoke detector); and
(unwanted) visitors (e.g., by registering the presence
of the visitor’s smartphone). The discussed
recommendations from participants should be
incrementally added to the Smartphone Application
to improve its functionalities and user-friendliness.
This provides particularly more overview on who
takes care of which task or alarming situation.
The Smartphone Application shows with a
median (range) SUS score of 87.50 (15.00) and
uMARS score of 4.27 (0.73) excellent usability and
good quality, suggesting that the application is most
likely well implementable in practice. The high
outcome is most likely due to our chosen design
process; involving potential end-users throughout the
design. The current drawback is the lack of testing in
a real-life setting, which could have determined
whether the provided information is sufficient, the
Calendar and Chat come to their full right, and
functionalities such as blocking calls are being used.
The Sensor System seems to work well, and the
DSS shows a high accuracy score of 92%. This is
most likely due to using relatively simple sensors and
algorithms. On the downside, the technical evaluation
was short and in a controlled environment. Future
evaluations should pursue carrying out longer (real-
life) trials, allowing to find unnoticed problems, and
to test the Sensor System on properties such as
durability and battery life. In addition, the DSS
should be brought to a higher level, using for example
machine learning to map behavior of the resident to
better identify activities and behavior, making the
system more reliable and thus more user-friendly.
The next step for the HMS would be to evaluate
the system in a real-life setting, and to search for
possibilities to merge the HMS with HELMA. We do
expect that, over time, much of the HELMA data can
be replaced with more accurate objective
measurements, making the HELMA questionnaires
more time-efficient and more focused on purely
subjective information.
In conclusion: the HMS seems to be a promising
proof of concept in providing effective support to
informal caregivers of people with dementia. The
system gives key information related to the health and
independent living of the person with dementia, and
aims therewith to promote the quality of life of the
informal caregivers by offering peace of mind and
reducing the burden of care.
A Remote Home Monitoring System to Support Informal Caregivers of People with Dementia
101

ACKNOWLEDGEMENTS
The authors would like to thank all participants,
TriviumMeulenbeltZorg, and Liberein, for their
valuable time and support. The HMS is developed by
Roessingh Research and Development, Telemedicine
Group. This work was partly funded by the H2020
program (PHC-20-2014) within the IN LIFE project
(grant no. 643442).
REFERENCES
Alzheimer’s Society, 2017. How assistive technology can
benefit people with dementia and their carers. Available
at: https://www.alzheimers.org.uk/info/20091/what_
we_think/85/assistive_technology/2.
Bank, A. et al., 2006. The value of telephone support groups
among ethnically diverse caregivers of persons with
dementia. The Gerontologist, 46(1), pp.134–138.
Benyon, D. & Macaulay, C., 2002. Scenarios and the HCI-
SE design problem. Interacting with Computers, 14(4),
pp.397–405.
Brooke, J., 1996. SUS - A quick and dirty usability scale.
In P. Jordan et al., eds. Usability Evaluation in Industry.
Taylor & Francis, pp. 189–194.
Carswell, W. et al., 2009. A review of the role of assistive
technology for people with dementia in the hours of
darkness. Technology and Health Care, 17(4), pp.281–
304.
Dunn, O., 1961. Multiple Comparisons Among Means.
Journal of the American Statistical Association,
56(293), pp.52–64.
Glascock, A. & Kutzik, D., 2000. Behavioral Telemedicine:
A New Approach to the Continuous Nonintrusive
Monitoring of Activities of Daily Living. Telemedicine
Journal, 6(1), pp.33–44.
Huis in ‘t Veld, M. et al., 2010. A scenario guideline for
designing new teletreatments: a multidisciplinary
approach. Journal of Telemedicine and Telecare, 16,
pp.302–307.
Ienca, M. et al., 2017. Intelligent Assistive Technology for
Alzheimer’s Disease and Other Dementias: A
Systematic Review. Journal of Alzheimer’s Disease,
56(4), pp.1301–1340.
Kendall, M., 1975. Rank Correlation Methods (4th ed.),
Griffin.
Kirsi, T., Hervonen, A. & Jylhä, M., 2004. Always one step
behind: husbands’ narratives about taking care of their
demented wives. Health (London), 8(2), pp.159–181.
Available at: http://www.ncbi.nlm.nih.gov/pubmed/
15068635.
Liu, L. et al., 2016. Smart homes and home health
monitoring technologies for older adults: A systematic
review. International Journal of Medical Informatics,
91(1), pp.44–59.
Ministry of Health Welfare and Sport et al., 2009. Guideline
for Integrated Dementia Care [excerpt],
Miranda-Castillo, C., Woods, B. & Orrell, M., 2013. The
needs of people with dementia living at home from user,
caregiver and professional perspectives: a cross-
sectional survey. BMC Health Services Research,
13(1), p.43.
Nielsen, J. & Landauer, T., 1993. A mathematical model of
the finding of usability problems. In Proceedings of the
INTERACT ’93 and CHI ’93 Conference on Human
Factors in Computing Systems. pp. 206–213.
Nijhof, N. et al., 2013. An evaluation of preventive sensor
technology for dementia care. Journal of Telemedicine
and Telecare, 19(2), pp.95–100.
Nolan, M., Ingram, P. & Watson, R., 2002. Working with
Family Carers of People with Dementia. SAGE, 1(1),
pp.75–93.
Peeters, J., Werkman, W. & Francke, A., 2014. Kwaliteit
van dementiezorg door de ogen van mantelzorgers.
Dementiemonitor Mantelzorg 2013: deelrapportage 1,
Peeters, J., Werkman, W. & Francke, A., 2014.
Mantelzorgers over ondersteuning bij dementie door
het sociale netwerk en de gemeente. Dementiemonitor
Mantelzorg 2013: deelrapportage 2,
Peeters, J.M. et al., 2010. Informal caregivers of persons
with dementia, their use of and needs for specific
professional support: a survey of the National Dementia
Programme. BMC Nursing, 9(1), p.9.
Peetoom, K. et al., 2015. Literature review on monitoring
technologies and their outcomes in independently
living elderly people. Disability and Rehabilitation:
Assistive Technology, 10(4), pp.271–294.
Pol, M. et al., 2016. Older People’s Perspectives Regarding
the Use of Sensor Monitoring in Their Home.
Gerontologist, 56(3), pp.485–493.
Pollitt, P., Andersont, I. & O’Connor, D., 1991. For Better
or for Worse: The Experience of Caring for an Elderly
Dementing Spouse. Ageing and Society, 11(4), pp.443–
469.
Stoyanov, S. et al., 2016. Development and Validation of
the User Version of the Mobile Application Rating
Scale (uMARS). JMIR mHealth and uHealth, 4(2),
p.e72.
Urwyler, P. et al., 2017. Cognitive impairment categorized
in community-dwelling older adults with and without
dementia using in-home sensors that recognise
activities of daily living. Scientific Reports, 7.
Available at: http://www.nature.com/articles/srep42084.
VUmc Alzheimercentrum et al., 2012. Deltaplan Dementie,
Available at: http://www.rijksoverheid.nl/documenten-
en-publicaties/rapporten/2013/04/04/rapport-deltaplan-
dementie.html.
Yang, C. & Hsu, Y., 2012. Remote monitoring and
assessment of daily activities in the home environment.
Journal of Clinical Gerontology and Geriatrics, 3(3),
pp.97–104.
Zwaanswijk, M. et al., 2013. Informal Caregivers of People
with Dementia: Problems, Needs and Support in the
Initial Stage and in Subsequent Stages of Dementia: A
Questionnaire Survey. The Open Nursing Journal, 7,
pp.6–13.
HEALTHINF 2018 - 11th International Conference on Health Informatics
102
