
FHIR FLI: An Open Source Platform for Storing, Sharing and Analysing
Lifestyle Data
Kiran Gopinathan
1
, Nikolaos Alexandros Kaloumenos
1
, Kinnari Ajmera
1
, Alexandru Matei
1
,
Ian Williams
2
and Andrew Davis
2
1
University College London, United Kingdom
2
Nuffield Health, United Kingdom
Keywords:
Personal Health Record, Lifestyle Data, FHIR.
Abstract:
Consumers and healthcare organisations alike are increasingly interested in using digital health solutions to
reduce the risk of chronic conditions or to help manage these conditions outside hospitals. Equally, there is
a strong public health benefit in helping individuals adopt and improve healthy lifestyle behaviours. The first
step in this direction is the ability to record and analyse lifestyle data. Currently, lifestyle logging platforms
use proprietary data formats. Data is segregated among different platforms, impacting consumers, service
providers, research institutes and public health bodies. Our aim is to facilitate the transfer of information
between individuals and organisations that hold or require their lifestyle data. We demonstrate that an open
source platform based on a clinically recognised interoperability standard - Fast Healthcare Interoperability
Resources (FHIR) - can meet both consumers and industry needs. We use as an example the case of people
managing arthritis. Our contributions are: (i) an extension of the FHIR standard for lifestyle data, (ii) a
reference architecture for a Personal Lifestyle Record, (iii) integration with voice-enabled digital assistants
for lifestyle data capture and (iv) an open source implementation of this architecture that retrieves, saves and
analyses lifestyle data from wearable devices.
1 INTRODUCTION
The UK population is living longer, but at the same
time people spend more years in ill-health, managing
chronic conditions (Public Health England, 2015).
To cope with the increasing burden of disease,
more and more resources are dedicated to preven-
tion and management of chronic conditions within the
community. For example, a recent study in the UK
has shown a remission in Type 2 diabetes for par-
ticipants following a low-calorie, diet-based, weight
management programme. Throughout the process,
the trial participants had interaction with their GP and
could access a dietician (Lean et al., 2017)
As fitness, well-being and lifestyle data becomes
more relevant in the provision of care, consumers
and healthcare professionals need the ability to aggre-
gate disparate information about one’s lifestyle into a
consolidated view spanning across the years, across
providers, and covering many data sources. Improved
access to lifestyle data can lead to better quality of
care, better health outcomes and improved customer
satisfaction.
We consider lifestyle data any measurement re-
lated to:
• lifestyle risk factors (e.g. physical activity)
• mental health (e.g quality of sleep, stress levels)
• monitoring of chronic conditions (e.g blood glu-
cose)
• maintaining or improving ability (e.g physiother-
apy, rehabilitation, mental resilience, elite sports).
The current landscape in the industry is very frag-
mented - each organisation that generates lifestyle
data uses proprietary formats. The challenge we aim
to address in this paper is the lack of a true platform
approach, in the well-being and lifestyle domain.
In a platform approach, the analysis of data (for
day-to-day monitoring, service personalisation or be-
haviour change) is separated from data collection. For
this to happen, there is a need for an encompassing
and open standard to describe lifestyle data in a con-
sistent manner, agnostic of the source systems gen-
erating the data. This will open the way for services
specifically designed to deliver value by interpreting
Gopinathan, K., Kaloumenos, N., Ajmera, K., Matei, A., Williams, I. and Davis, A.
FHIR FLI: An Open Source Platform for Storing, Sharing and Analysing Lifestyle Data.
DOI: 10.5220/0006791302270233
In Proceedings of the 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2018), pages 227-233
ISBN: 978-989-758-299-8
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
227

the data in new, useful ways. This is the path fol-
lowed in the medical community, where much effort
has been put into defining interoperability standards
to describe clinical data.
In this paper, we propose an architecture for a Per-
sonal Lifestyle Record that offers capabilities to re-
trieve, store and analyse lifestyle data in a provider-
agnostic environment, illustrating the potential of a
platform approach. To inform our proposal, we use as
an illustrative case study the management of arthritis.
The paper is organised as follows. Section 2
presents the current technology landscape for man-
aging and using lifestyle data. Section 3 discusses
an illustrative customer journey, in arthritis manage-
ment. Section 4 proposes a method for standardis-
ation of lifestyle data and offers two specific exam-
ples. Section 5 presents a reference architecture that
decouples data generation from data analysis. Sec-
tion 6 discusses emerging user interaction channels,
such as voice-enabled digital assistants for capturing
lifestyle data. Section 7 describes the implementation
work done to date and Section 8 summarises our con-
tributions and discusses future work.
2 BACKGROUND
Smart-phones have become a leading consumer
choice for managing lifestyle data. They are a nat-
ural hub to bring together data coming from built-in
sensors on the phone, data coming from wearable de-
vices that synchronise with the phone and data com-
ing from mobile apps installed on the phone. There
are a number of limitations when using a smart-phone
based lifestyle record:
• it is not an inclusive approach: Apple Healthkit
data can only be accessed from an iPhone.
• it does not cover the needs of service providers,
who need to access and aggregate data from a
population of clients
Solutions created by wearable companies have the
advantage of being accessible across platforms, mo-
bile and web. They focus on analysing and providing
insight on data collected through the wearable. They
have two main limitations:
• the data model of each platforms is controlled
by the vendor and it only contains items relevant
within the context of use for each wearable - third
parties cannot extend the data model.
• the data is still locked, as Fitbit users can only
compare themselves against other Fitbit users for
example.
Cloud-based platforms like Open MHealth or Mi-
crosoft Health Vault have cross-platform accessibility
and allow developers to extend the data model. Infor-
mation can be shared with service providers. How-
ever, these platforms also have some limitations.
• at the moment, they still use proprietary data for-
mats
• third-party developers cannot develop custom vi-
sualisations or predictive models
There are two conclusions we can draw from re-
viewing the current landscape. First, there is a clear
direction towards enabling data movement. Many
wearable companies allow customers to download
their own data for example. Conversely, other compa-
nies position themselves as data repositories, offering
the necessary integrations for consumers to bring data
into their platforms.
Second, there is no open, standard information
model for lifestyle data, with clear governance sup-
porting it, which is not tied to a specific commercial
organisation.
We argue that such an information model could
well be developed following an open and inclusive
approach, as opposed to being developed internally
by any one company. There is a large body of work
which could inform these efforts, stemming from the
clinical community pursuit to standardise the way
medical data is represented.
FHIR (Bender and Sartipi, 2013) is such a stan-
dard, supported by HL7 and adopted by a grow-
ing number of healthcare organisations, including the
NHS (Kavanagh, 2017).
The FHIR specification defines a set of core re-
sources (Person, Observation, Diagnostic etc). and
an infrastructure for handling resources. FHIR Ob-
servations are already used to describe:
• Vital signs: e.g. temperature
• Laboratory Data: e.g. blood glucose
• Devices Measurements: e.g. pulse oximetry
• Clinical assessments: e.g. Glasgow Coma Score
• Personal characteristics: e.g. eye colour
The FHIR standard can be extended to suit par-
ticular contexts of use - including management of
lifestyle data. Extending FHIR to suit particular sce-
narios of use is achieved by creating FHIR Profiles. A
profile extends or restricts core FHIR resources, based
on the domain-specific needs.
A FHIR extension for lifestyle data is being devel-
oped as part of the Finnish national Personal Health
Record infrastructure (Kanta, 2017). However, their
approach is to create a limited number of FHIR ob-
servations, describing fitness information aggregated
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
228

over a period of time - for example ’Distance reached
in 24h’. We favour an approach where any data point
created at the source system is mapped to a FHIR ob-
servation. In our approach, three distinct walking /
running episodes in a 24 hour window would be rep-
resented as three FHIR observations, not a single one.
3 ILLUSTRATIVE CASE STUDY
Lifestyle data can be used to improve the health and
well-being of people of all ages.
To discuss our proposal for managing lifestyle
data, we consider the case of arthritis, a group of
chronic conditions that affect the joints in the body.
As of 2017, 400,000 adults in the UK have rheuma-
toid arthritis, and prevalence increases with age. Fur-
ther, 8.75 million people in the UK have sought
treatment for osteoarthritis, where prevalence also in-
creases with age (Arthritis Research UK, 2017).
For the management of rheumatoid arthritis, the
National Institute for Health and Care Excellence
(NICE) in the UK recommends access to physiother-
apy services, to improve fitness and encourage reg-
ular exercise (Deighton et al., 2009). Similarly, for
the management of osteoarthritis NICE recommends
physical exercise for local muscle strengthening and
general aerobic fitness (Conaghan et al., 2008).
In term of assessing pain intensity - a key mea-
surement for arthritis management - there are differ-
ent scales available, with good degree of correlation
among them (Downie et al., 1978). Once could use a
descriptive scale (nil, mild, moderate, severe, very se-
vere), a numeric scale (0 - no pain, 10 - worst possible
pain) (Farrar et al., 2001) or a visual analogue scale
(100 mm in length anchored by the two extremes)
(Hawker et al., 2011).
Based on the clinical context, there is a demon-
strable need for data related to physical activity and
pain levels to be shared between users, GPs and phys-
iotherapists. The hypothetical customer journey we
use as a source of requirements is then: a patient di-
agnosed with arthritis has been referred by his GP to
a physiotherapist. The physiotherapist recommends a
regime of moderate physical activity, which includes
outside running sessions and pilates classes at a local
gym. The user would like to share a full record of his
physical activity with the physiotherapist, as well as
be able to track how his symptoms (i.e. pain levels)
change over time, as a result of his efforts. In turn,
the physiotherapist would like to share summary data
with the patients GP.
To support this journey, we need to enable three
types of information flows.
The first scenario we aim to support is a person
centric view: allowing one individual to aggregate
data about himself which is held by different plat-
forms and providers. For example, somebody manag-
ing osteoarthritis could attend physiotherapy sessions,
he could run in the park during the weekend and at-
tend a T’ai chi class in the gym once a week. He
should have access, combine and own all of this data
- information generated by a specialist, by a wearable,
by a fitness service provider, or self reported.
The second scenario we aim to support is an or-
ganisation centric view: allowing service providers to
receive data shared with them by their clients. For ex-
ample, a physiotherapist should be able to access data
about physical activity levels and self reported pain
levels from each individual under treatment. Equally,
a research institution may want to accumulate large
datasets of lifestyle data for clinical research, from
patients willing to share their data.
Third, we are looking to support organisations that
hold lifestyle data about their clients and want to of-
fer access to this data to the individuals themselves.
For example, a gym chain looking to share individual
attendance data with the gym members, so that they
can further share this data with a physiotherapist.
4 FHIR PROFILES FOR
LIFESTYLE DATA
Our first contribution is a demonstration of how the
FHIR standard may be used to describe lifestyle data
in a provider agnostic fashion. There are many poten-
tial data sources for lifestyle data:
• self-recorded observations
• observations captured by providers of a certain
service: health assessments, personal coach
• smartphones, wearables and body sensors
• smart home devices: smart meters, environment
sensors, smart speakers with voice-enabled digital
assistants
In order to capture this variety of data we needed
to identify a set of profiles capable of representing
it. Following FHIR best practices (Furore, 2017), we
chose to extend the Observation profile, prioritizing
removing fields irrelevant for our context of use, and
only introducing new fields when no existing fields
could possibly represent the data. The constructed ob-
servation profile is shown in Figure 1. This could be
used for example to create a recording of self reported
pain intensity, in reference to our arthritis case study.
FHIR FLI: An Open Source Platform for Storing, Sharing and Analysing Lifestyle Data
229
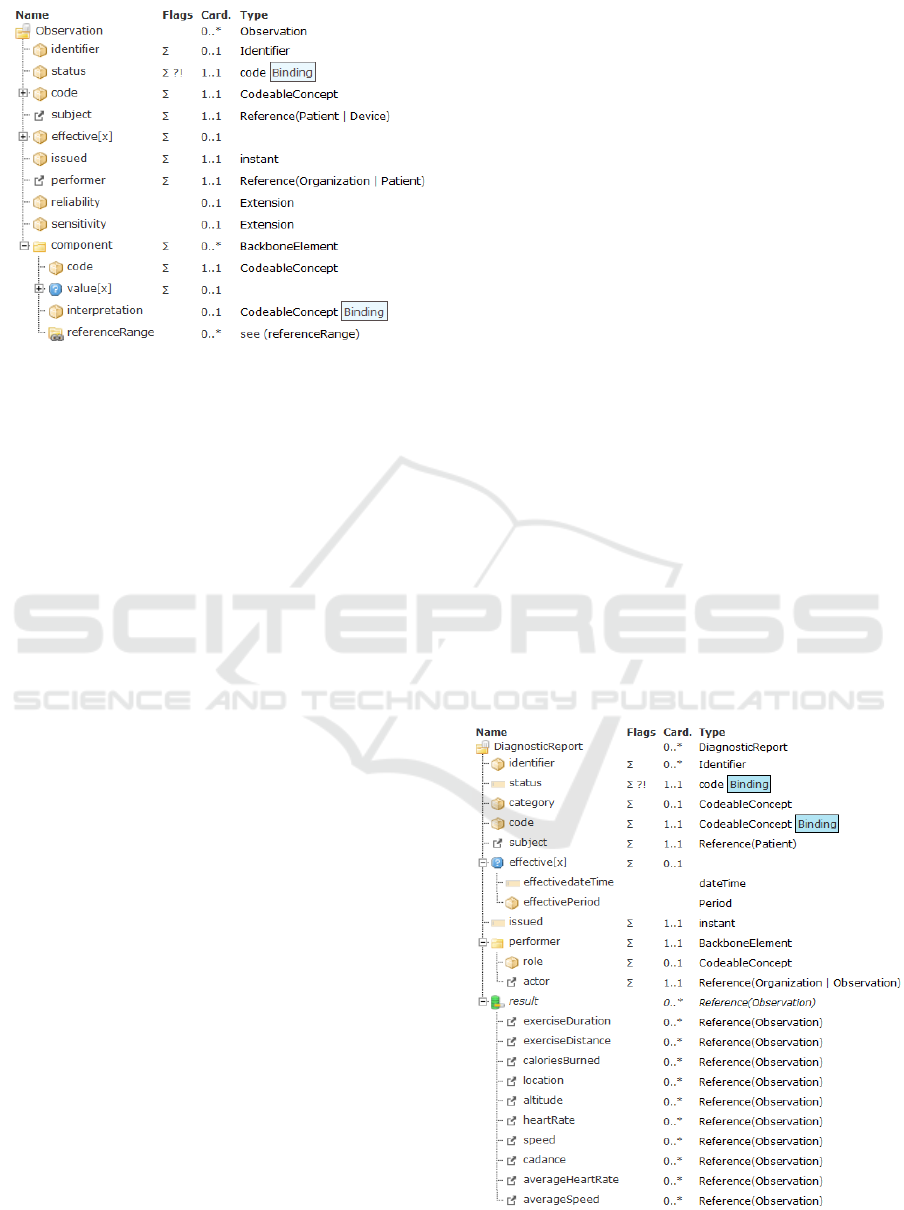
Figure 1: FHIR Observation Profile.
The code field is used to specify the type of obser-
vation (in our case, a pain intensity recording). The
subject field is a reference to the person the observa-
tion concerns. The performer field is a reference to
the source system (e.g. device, organisation or per-
son). To record the measurement result, we use a set
of related fields, grouped under Component. These
include the actual value, but also the admissible range
and the method of measurement. Finally, we record
both the time period described by this observation -
the effective time (in our case, when did the pain oc-
cur) and also the date the FHIR observation has been
created - the issued date.
The fields discussed so far are applicable to any
type of observation. There are some additional con-
siderations that are specific to the lifestyle domain.
First, we need to account for the varying degree
of reliability for the data sources: looking at a simple
measure such as weight measured in kilograms - this
could be self-reported, retrieved from a smart scale,
or measured during a health assessment. To capture
this ’trustworthiness’ of the data, we introduce a field
for reliability, that takes numerical values. Each or-
ganisation using these FHIR profile may specify rules
that assign reliability scores to source systems. Every
FHIR observation created based on data coming from
a given source would then carry the same reliability
value as that assigned to the source system.
Second, the same event (measurement) may be
captured in more than one system. The same physical
workout (e.g. a pilates class) could be captured by a
consumer wearable device and by the class booking
system of the gym. However, the event would be de-
scribed differently in the two platforms. Our design
approach is to avoid any reconciliation or aggrega-
tion at this stage. We recommend creating two dis-
tinct FHIR observations. The relation between these
observations (duplicate data, contradictory data, com-
plementary data) shall be established if and when nec-
essary to answer a specific query.
Third, depending on the source system, data may
be more or less sensitive, so different access rules
would apply to data. To enable differentiated access
rules for different types of observation, we add to the
profile a field to record how sensitive the data is.
In reference to our arthritis case study, the other
type of lifestyle information that should be saved re-
lates to physical workout sessions. To document an
exercise session, we propose using a Diagnostic Re-
port profile, shown in Figure 2. This is another type
of FHIR resource that groups observations related to
the same episode. First, our profile on Diagnostic Re-
port specifies the same fields we have discussed for
individual observations: a code, subject, performer,
time. Second, the result field contains reference to
additional observations. The list we provide is not ex-
haustive. Depending on what information is available
from the source system, implementers may add addi-
tional references to observations, so that all available
information is captured.
Many lifestyle devices also make the distinction
between aggregate and trace data - running watches
are able to record a user’s heart rate every few sec-
onds during a session (trace), and also calculate an
average heart rate at the end (aggregate). To reflect
this, where applicable, fields for both types of data
have been added to the profile - heartRate and aver-
ageHeartRate.
Figure 2: FHIR FLI Profile - Workout Session.
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
230

5 REFERENCE ARCHITECTURE
A range of EHR platforms already use the FHIR
standard as a data exchange mechanism. However,
FHIR messages are mapped to an internal clinical
model (for example, OpenEHR) and then saved in
a structured database. Data can be interrogated ei-
ther through structured query languages on the inter-
nal clinical model.
For example, SMART ON FHIR (Mandel et al.,
2016) is an EHR platform built to support importing
and exporting healthcare data through FHIR compli-
ant messages - however, all data is stored internally as
a set of key value pairs in a relational database.
In comparison, we aim to investigate whether an
infrastructure based solely on FHIR messages can be
used for reporting and analytics. By designing and
implementing such a platform, we aim to evaluate the
role of the FHIR standard when it comes to storing
data, as opposed to transmitting data (as it has been
traditionally seen).
In this section, we discuss the components of a
reference architecture built around the FHIR profiles
for lifestyle data.
First, the platform should have a Connector com-
ponent to allow consumers to retrieve lifestyle data
from different sources. The connector is required be-
cause lifestyle data is usually spread across a multi-
tude of systems and platforms, each offering an in-
complete view of the individual. We aim to offer con-
sumers an easy way to retrieve their own data from
these various platforms. The connector comes with
built-in integrations to the main consumer-oriented
lifestyle tracking platforms. The connector can also
be extended by each organisation implementing the
reference architecture so that it also retrieves data
from company-specific internal databases or systems.
The connector is also responsible to retrieve and send
data in the FHIR format. This ensures interoperability
between different organisations that have committed
to exposing data in FHIR format.
Second, the architecture requires a Converter
component, which maps data from proprietary for-
mats onto FHIR profiles for lifestyle data. The con-
verter is also responsible to record the source of the
information for each FHIR observation created. It
also enacts the business rules, assigning values to the
reliability and sensitivity fields of the FHIR profiles.
The converter component relies on a library of se-
lected FHIR profiles suitable to capture common data
items in the lifestyle domain. Organisations imple-
menting the infrastructure for internal use could de-
velop additional FHIR profiles for data they hold in-
ternally. We propose a development process whereby
whenever a new FHIR profile for lifestyle data is cre-
ated by organisations implementing this architecture,
the converter component is updated accordingly.
Third, the reference architecture requires a docu-
ment database, to store each FHIR observation in its
native format - a JSON message.
Fourth, the reference architecture includes a data
visualisation component, which comes with built-in
visualisations for common lifestyle data. We pro-
pose a process whereby whenever a new FHIR pro-
file is created, the data visualisation component is ex-
tended so that it can graphically represent the new
type of data. Organisations implementing the archi-
tecture may develop custom data visualisations to suit
their specific needs. One clear benefit of building vi-
sualisations on top of a standard data model such as
FHIR is that visualisation over the data will continue
to function as expected, even if the systems generat-
ing the data change.
Fifth, the reference architecture allows for an ad-
vanced analytics component. This enables machine
learning experts to build predictive models against a
standard representation of data. These models can be
evaluated and used independently of the underlying
data source. The type of models particularly suitable
to lifestyle data is based on time series analysis of
behavioural traces, in order to predict trends in be-
haviours of interest or occurrence of specific events.
6 USER EXPERIENCE
In this section, we discuss new ways for customers
and organisations to interact with lifestyle records.
Whereas health records are accessed by clinicians in
controlled environments (a GP clinic, a hospital etc),
interaction with lifestyle records are more diverse, in
terms of users, context and purpose.
One such interaction model is that of voice-
enabled services, which, aside from increasing con-
venience, could remove a host of accessibility barriers
from users.
A personal lifestyle record could allow consumers
to create self-reported observations (for example, re-
lated to pain levels) using voice-enabled digital as-
sistants. Through this, elderly people facing accessi-
bility problems when a using a smartphone can more
easily manage a chronic condition using voice to track
their symptoms. Conversely, when developing these
interfaces, it is important to ensure that they respond
logically as otherwise could lead to frustration.
Similarly, lifestyle records can also by queried by
voice, asking for example for the next physiotherapy
session booked at the gym.
FHIR FLI: An Open Source Platform for Storing, Sharing and Analysing Lifestyle Data
231

Due to the nature of the interfaces provided by
voice enabled services, the types of data that can be
recorded must be predefined. For example, the Ama-
zon Alexa interface does not allow users to submit
voice recordings as inputs, hence it would not be
possible to record qualitative data. However most
lifestyle data can be recorded quantitatively. For those
that can’t, quantitative mappings can be defined (a nu-
merical scale in the case of pain) mitigating this issue.
7 FHIR FLI - OPEN SOURCE
IMPLEMENTATION
Based on the reference architecture, we have started
development of an open-source implementation -
FHIR FLI. This acts as a starting point for organisa-
tions wishing to deploy a software solution that con-
forms to the proposed reference architecture.
FHIR FLI contains a number of FHIR profiles
specifically developed for the lifestyle domain. For
example, a profile to standardise sleep information,
or for describing a workout session. The full list is
available at https://simplifier.net/FhirFli/ resources
FHIR FLI offers out of the box connectors that
allow consumers to authenticate and pull lifestyle data
from Fitbit, Google Fit and Apple Healthkit. Data is
then converted into the new FHIR profiles and saved
into a document database.
Finally, FHIR FLI contains a data visualisation
component and an Amazon Alexa skill under current
development.
The FHIR FLI data visualization component pro-
vides an interface for both corporate and individual
users to view and analyse FHIR data. Using the
dashboard, individual users can view their own per-
sonal data, whereas corporate users can view aggre-
gate anonymised data for all users registered with
their companies. The dashboard draws its data from a
document database, but also reroutes requests through
an Apache Drill connector to allow for larger scale
queries (in the case of corporate users).
The FHIR FLI Amazon Alexa skill provides
users a fluid interface for making specific prede-
fined queries on FHIR data stored within a docu-
ment database - queries such as ”What was my aver-
age heart rate yesterday?” will retrieve and return any
matching data through the Amazon Alexa device. The
skill also allows users to record data into a document
database through an Amazon Alexa, and once a user
has submitted the data, it is converted into the new
FHIR profiles and stored into the document database.
The source code is available at https://github.com/
fhirfli
8 CONCLUSIONS
FHIR FLI is an open source Personal Lifestyle
Record that helps both consumers and organisations
to combine and analyse lifestyle data, independently
of the source systems.
Using FHIR ensures interoperability, allowing
consumers to share data with service providers or
research institutes and empowering organisations to
share more data with customers.
The next step we are pursuing is assessing the fea-
sibility and performance of a FHIR based data reposi-
tory compared with data repositories based on clinical
models such as OpenEHR.
Future work should also concentrate on the imple-
mentation of access control policies and development
of the machine learning module. This would demon-
strate how large data sets of lifestyle data can be
assembled from individuals willing to anonymously
share their data with research institutes, to build new
predictive models linking lifestyle behaviours to clin-
ical risks and outcomes.
ACKNOWLEDGEMENTS
We are indebted to Dr. Dean Mohamedally, our
project supervisor, for guiding our research.
REFERENCES
Arthritis Research UK (2017). State of musculoskeletal
health 2017. https://www.arthritisresearchuk.org/
arthritis-information/data-and-statistics/state-of-
musculoskeletal-health.aspx.
Bender, D. and Sartipi, K. (2013). Hl7 fhir: An agile and
restful approach to healthcare information exchange.
In Computer-Based Medical Systems (CBMS), 2013
IEEE 26th International Symposium on, pages 326–
331. IEEE.
Conaghan, P. G., Dickson, J., and Grant, R. L. (2008). Care
and management of osteoarthritis in adults: summary
of nice guidance. Bmj, 336(7642):502–503.
Deighton, C., OMahony, R., Tosh, J., Turner, C., Rudolf,
M., Group, G. D., et al. (2009). Management of
rheumatoid arthritis: summary of nice guidance. BMJ,
338(mar16
1):b702–b702.
Downie, W., Leatham, P., Rhind, V., Wright, V., Branco,
J., and Anderson, J. (1978). Studies with pain rating
scales. Annals of the rheumatic diseases, 37(4):378–
381.
Farrar, J. T., Young, J. P., LaMoreaux, L., Werth, J. L., and
Poole, R. M. (2001). Clinical importance of changes
in chronic pain intensity measured on an 11-point nu-
merical pain rating scale. Pain, 94(2):149–158.
ICT4AWE 2018 - 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health
232

Furore (2017). Fhir best practices. https://simplifier.net/
guide/ProfilingAcademy/Best-practices.
Hawker, G. A., Mian, S., Kendzerska, T., and French,
M. (2011). Measures of adult pain: Visual analog
scale for pain (vas pain), numeric rating scale for pain
(nrs pain), mcgill pain questionnaire (mpq), short-
form mcgill pain questionnaire (sf-mpq), chronic pain
grade scale (cpgs), short form-36 bodily pain scale (sf-
36 bps), and measure of intermittent and constant os-
teoarthritis pain (icoap). Arthritis care & research,
63(S11).
Kanta (2017). Phr for developers. https://www.hl7.org/
documentcenter/public temp B8B93A79-1C23-BA
17-0CD130736D1F56A7/wg/mobile/Kanta%20PHR
%20for%20Developers.pdf.
Kavanagh, R. (2017). How is nhs digital using fhir.
http://www.hl7.org.uk/doc store/FHIR/NHSDigital
FHIR.pdf.
Lean, M. E., Leslie, W. S., Barnes, A. C., Brosnahan, N.,
Thom, G., McCombie, L., Peters, C., Zhyzhneuskaya,
S., Al-Mrabeh, A., Hollingsworth, K. G., Rodrigues,
A. M., Rehackova, L., Adamson, A. J., Sniehotta,
F. F., Mathers, J. C., Ross, H. M., McIlvenna, Y., Ste-
fanetti, R., Trenell, M., Welsh, P., Kean, S., Ford, I.,
McConnachie, A., Sattar, N., and Taylor, R. (2017).
Primary care-led weight management for remission
of type 2 diabetes (direct): an open-label, cluster-
randomised trial. The Lancet.
Mandel, J. C., Kreda, D. A., Mandl, K. D., Kohane,
I. S., and Ramoni, R. B. (2016). Smart on fhir: a
standards-based, interoperable apps platform for elec-
tronic health records. Journal of the American Medi-
cal Informatics Association, 23(5):899–908.
Public Health England (2015). England has the potential
to have the lowest disease burden in the world.
https://www.gov.uk/government/news/england-has-
the-potential-to-have-the-lowest-disease-burden-in-
the-world.
FHIR FLI: An Open Source Platform for Storing, Sharing and Analysing Lifestyle Data
233
