
Towards a Fully Automated Bracelet for Health Emergency Solution
Igor Matias
1,2
, Nuno Pombo
1,2,3
and Nuno Garcia
1,2,3
1
Computer Science Department, Universidade da Beira Interior,
R. Marquês de Ávila e Bolama, 6201-001, Covilhã, Portugal
2
Instituto de Telecomunicações, Av. Rovisco Pais, 1, 1049-001, Lisboa, Portugal
3
Universidade Lusófona de Humanidades e Tecnologias, Campo Grande, 376, 1749-024, Lisboa, Portugal
Keywords: Bio Signal Monitoring Device, Arduino, Sensors, RF Communications, Emergency Scenarios Detection.
Abstract: Activity and health monitoring bracelets are currently a popular consumer electronic wearable, and several
different manufacturers market several different versions, integrating a wide and diverse range of sensors.
The several different types of bracelets often require the user to interact with the bracelet itself or with the
help line attendant. However, this interaction is not suitable in many emergency scenarios. Thus, this paper
presents a novel system to monitor, detect and communicate health critical situations, in a full automated
manner. The system encompasses a bracelet capable for health abnormalities detection based on both vital
signs, and accelerometer data collection from the user. This paper also describes the design and prototyping
process of the bracelet, providing insight and solutions to observed problems. In spite of the early stage of
this system, the observed results are promising and offer room for improvements on either complementary
studies or different clinical emergence scenarios.
1 INTRODUCTION
According to (United Nations, 2015), by the year of
2015, Europe, Oceania and North America, had
about 20 percent of elderly people (60 or more years
old). By 2050, these numbers are expected to
become higher than 30 percent. Authors of
(Administration on Aging; Administration for
Community Living; U.S. Department of Health and
Human Services, 2012) indicate that, only in the
United States of America, by 2011, the number of
persons aged 65 years old or more was representing
41.4% of the total country’s population, number
expected to increase to about 56% in 2020. The
authors also indicate that “about 28% (11.8 millions)
of noninstitutionalized older persons live alone (8.4
million women, 3.5 million men)”, where “almost
half of older women (46%) age 75+ live alone”.
As studied in (“Saúde Pública - Fatores
associados a quedas em uma coorte de idosos
residentes na comunidade Fatores associados a
quedas em uma coorte de idosos residentes na
comunidade,” n.d.), the fact that an elderly is living
alone contributes to the increase of the chance of
occurring a fall, representing 28,5 percent in 1667
studied Brazilian elderly people, during two years.
Living alone, described as “loneliness” in (Barg et
al., 2006), is even “highly associated with depressive
symptoms, anxiety, and hopelessness”.
Depression being so present among people with
more than 60 years old and taking into account that
“high levels of depressive symptomatology are
associated with increased risks of myocardial
infarction (MI) and mortality” ((Barefoot and
Schroll, 1996)), elderly living alone is a current and
an expected future scenario for many families,
which raises pertinent challenges due to the fact that
accidents may occur with elderly and frail people,
which may result in morbidity or eventually in
death.
Only in the United States of America (USA), as
presented in (Lloyd-Jones et al., 2010), from the
total amount of deaths caused by Cardiovascular
Disease (CVD) in all ages during 2006, the origin
for 51 percent of the cases was Coronary Heart
Disease (CHD) and Stroke for 17 percent. These
same data show that approximately 677 thousand
deaths were recorded due to CVD in people aged 65
years or older, and were also noted approximately 33
thousand deaths caused by Heart Failure (HF) in
people 60 years of age or older, in the same year as
the previous.
Matias, I., Pombo, N. and Garcia, N.
Towards a Fully Automated Bracelet for Health Emergency Solution.
DOI: 10.5220/0006800803070314
In Proceedings of the 3rd International Conference on Internet of Things, Big Data and Security (IoTBDS 2018), pages 307-314
ISBN: 978-989-758-296-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
307

Notwithstanding every emergency solution is
intended to be the fastest and easiest possible, the
current solutions are merely based on emergency
calls, wrist bracelets, or pendant devices with an
emergency button. Therefore, its application in real
life is limited to cases when the user is conscious
and at the same time is susceptible to limitations due
to the “human factor”, in either the call duration or
the difficult to press the button.
Although every created solution tried to decrease
the time until the receipt for therapeutic strategies,
delays such as “human factor”, manual emergency
buttons, people avoiding ambulance services when
they really need it and others, “prevent the early
application of life-saving procedures and contribute
substantially to a diminished effectiveness of
treatment” ((Luepker RV et al., 2000)).
Thus, this paper describes the design and the
implementation of a fully automated device capable
of recognizing several types of health conditions, as
well as contacting the emergency services when
needed, using the vital signals collected from the
users’ wrist.
The proposed system also provides a personal
database of collected vital signals, which will then
be used by a doctor to detect any abnormalities in an
early stage, also as providing other ways to decrease
the emergency response time.
In summary, the main contribution of this study
is to define a fully automated system architecture to
measure vital signals, in order to detect movement
abnormalities or hearth related diseases and,
therefore, to alert physicians and/or informal health
care providers on alarm episodes, while using
mostly open access electronics. The ultimate goal is
to provide an intelligent and autonomous solution to
help persons living alone or being monitored due to
a chronical disease.
2 BACKGROUND
As presented in Table 1, there are already on the
market several solutions for the simple “emergency
button” option, such as (Bay Alarm Medical, n.d.;
Rescue Alert, n.d.; LifeStation Inc., n.d.; Alert1,
n.d.; Philips N.V., n.d.; ADT LLC, n.d.; Life Fone,
n.d.; Medical Guardian LLC, n.d.; Solodev, n.d.;
Samsung, n.d.; FitBit, n.d.; Mi, n.d.), some having
an extra feature like Global Position System tracking
or fall-detection and others being able to collect
some important health data used in this new
approach, such as heart rate and body temperature
(smart bands and smart watches).
However, none offers a way to interlink the
collected data to detect health conditions and/or
immediate emergency situations, this is, some of the
current solutions already have some of the same
sensors this new approach uses, but they are not
using its data to recognize health
conditions/emergencies.
For example, by using a pulse monitor (capable
of reading heart rate variability and others), it is
possible to detect arrhythmia ((Patel et al., 2012;
Tsipouras and Fotiadis, 2004)), CVD ((“HEART
RATE AS A PROGNOSTIC FACTOR FOR
CORONARY HEART DISEASE AND
MORTALITY: FINDINGS IN THREE CHICAGO
EPIDEMIOLOGIC STUDIES | American Journal of
Epidemiology | Oxford Academic,” n.d.)), Coronary
Artery Disease (CAD) ((Kligfield et al., 1989)), HF
((Nolan et al., 1998)) or even a stroke ((Glotzer et
al., 2003; Ritter et al., 2011)). Using a body
temperature sensor, it is still possible to establish a
relation between hypothermia/hyperthermia and
longevity after a stroke happen ((Kammersgaard et
al., 2002)). Finally, by using an accelerometer to
monitor the user’s sleep, it’s possible to detect
certain episodes and/or disorders, described in
(Hjorth et al., 2012).
Thus, to decrease the lack of assistance in
emergency situations, it is necessary to create a
device capable of, using mainly already existing
sensors, detect and automatically react to health
abnormalities, being anyway portable and easy to
use.
Table 1: List of Features of Each Device.
Features
Name of solution
Fall detection/accelerometer
GPS locator
Heart rate monitor
Body temperature
Skin detection
Health record
Emergency button/contact
Bay Alarm
Medical ((Bay
Alarm Medical,
n.d.))
X
X
Rescue Alert
((Rescue Alert,
n.d.))
X
IoTBDS 2018 - 3rd International Conference on Internet of Things, Big Data and Security
308
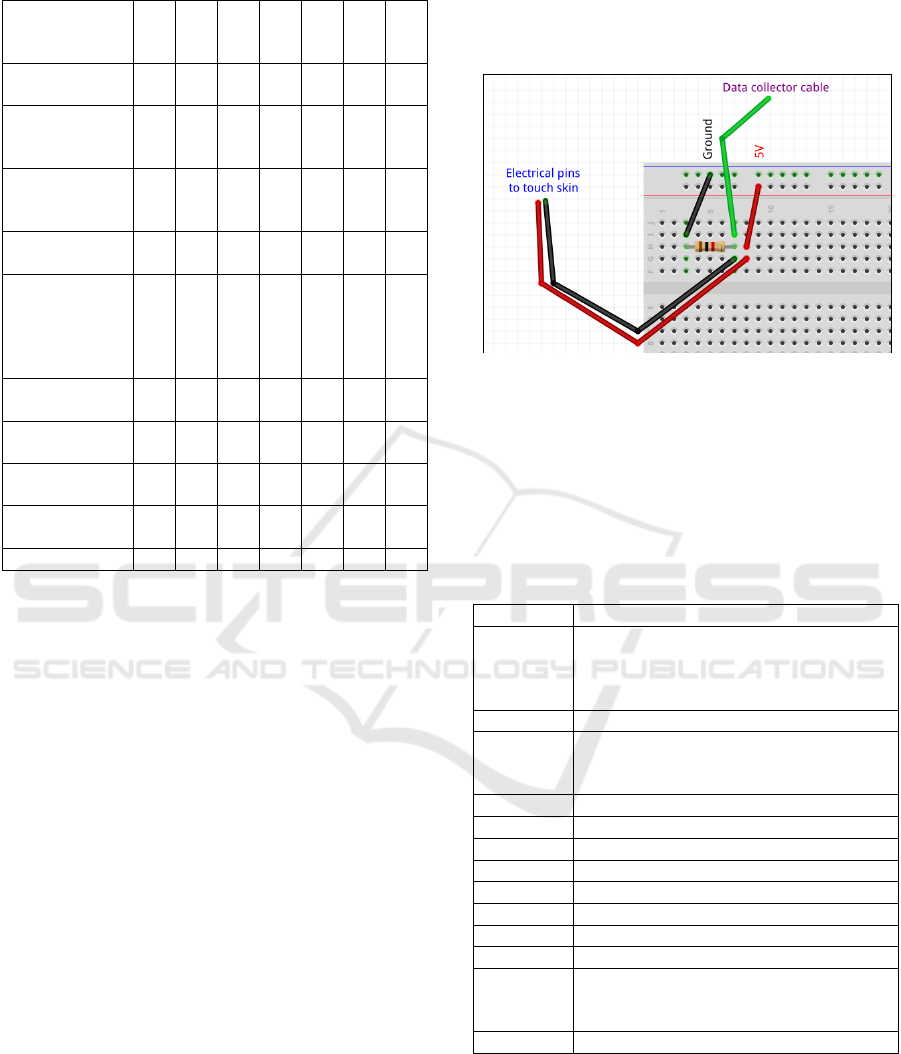
Table 1: List of Features of Each Device. (cont.)
LifeStation
((LifeStation Inc.,
n.d.))
X
X
Alert1 ((Alert1,
n.d., p. 1))
X
X
X
Philips LifeLine
((Philips N.V.,
n.d.))
X
X
X
ADT Medical
Alert ((ADT LLC,
n.d.))
X
X
X
LifeFone ((Life
Fone, n.d.))
X
X
X
Medical
Guardian
((Medical
Guardian LLC,
n.d.))
X
X
MobileHelp
((Solodev, n.d.))
X
X
X
Samsung Gear S3
((Samsung, n.d.))
X
X
X
FitBit alta HR
((FitBit, n.d.))
X
X
Mi Band 2 ((Mi,
n.d.))
X
X
Proposed system
X
X
X
X
X
X
X
3 METHODS
This section describes the proposed system,
including its components, and decision workflow. In
this study, a prototyping platform, known as
Arduino, was used. In fact, two units were used, one
to collect data from the sensors and other to collect
data sent from the first, which is stored and
interpreted, combined with the following sensors:
3-axis accelerometer ((Analog Devices Inc.,
2009));
GPS antenna ((Sparkfun Eletronics, n.d.));
Pulse sensor ((Sparkfun Electronics, n.d.));
Body temperature sensor ((Sparkfun
Electronics, n.d.));
Skin contact detection sensor;
Waterproof speaker ((VISATON GmbH & Co.
KG, n.d.));
434 MHz radio frequency transmitter and
receiver ((Sparkfun Electronics, n.d.));
All these sensors, excluding the skin contact
detection, are off-the-shelf components, and
available on the market, not from medical grade.
The skin contact detector was designed and built for
this specific study. It is composed by two electrical
pins (wires) and one 1 kilo ohm resistor (similar to
the human skin resistance, as studied and concluded
in (Ho et al., 2012)), as illustrated in Fig. 1, referring
the output power of the Arduino board.
Figure 1: Skin contact detection sensor scheme.
The data collector cable was connected to an
analogue input port, which receives 10 bits’ data,
and the electrical pins are designed to touch the skin
of the user (placed on his/her arm).
All the boards’ ports used to connect all the
sensors are listed in Table 2.
Table 2: Ports and Sensors.
Input/output
Sensor(s) connected
GND
Accelerometer, GPS antenna, Pulse
sensor, Body temperature sensor, RF
transmitter, RF receiver, Speaker, Skin
contact detection sensor
3.3V
Accelerometer
5V
GPS antenna, Pulse sensor, Body
temperature sensor, RF transmitter, RF
receiver, Skin contact detection sensor
A5
Accelerometer
A4
Accelerometer
A3
Accelerometer
A1
Skin contact detection sensor
A0
Pulse sensor
8
GPS antenna
9
GPS antenna
10
Body temperature sensor
3
RF transmitter (part of the device for the
user to wear), RF receiver (part of the device
to collect data to store)
11
Speaker
This project is composed by two distinct parts,
assembled in two Arduino boards.
On the collector and transmitter board we
assembled all the sensors to collect data, the speaker
and the RF transmitter. This part was responsible to
be on the users’ wrist, powered by a 7.0 volts’
Towards a Fully Automated Bracelet for Health Emergency Solution
309

battery, to read all the sensors and send the
information collected, each 10 seconds, to the other
board.
On the other hand, the receiver and interpreter
board was connected to a computer and, by reading
the data received from the RF receiver, checked if
any emergency scenario (described below) were
detected and, if necessary, sounded an alarm,
contacting the emergency services automatically,
also sending the recorded vital signals data of the
last 24 hours.
By combining these two concepts and running
the scenarios described below, the device can
produce alarms, that can be deactivated in case of a
false alarm, establish the automated contact with the
emergency services, send sensors data from the
moment and the last hours to that crew and guide
them to the victim, using sound.
Some of the already designed scenarios need to
be improved and tested in real cases, being then
interpreted by an Artificial Intelligence.
Besides very basic yet, they are the following:
Detect if the device is placed on the user’s
wrist:
o If the data collected from the skin contact
detection sensor is higher than “200”
(skin detected), proceed to the next
scenarios. Else, repeat this scenario.
Pulse abnormalities detection:
o If the pulse is below 30 beats per minute
(BPM) or higher than 140 BPM, check
temperature;
o If the body temperature is under 38ºC and
higher than 36ºC, check the pulse during
the next 20 seconds;
o If, during the next 20 seconds, the pulse
average is lower than 35 BPM or higher
than 135 BPM, start “emergency
procedure”;
o (the BPM and body temperature values
will be adapted to each user of the
prototype, regarding his/her previous
recorded data and known health
condition);
Body temperature abnormalities detection:
o If the body temperature is lower than
36ºC or higher than 39ºC, repeat this
scenario during the next 30 seconds;
o If in the next 30 seconds the temperature
average is lower than 34ºC or higher than
40ºC, start “emergency procedure”.
Movement abnormalities detection (falls or
abrupt movements originated by some type of
injury):
o If there are “G-force” readings higher
than 3.55 G (fall peaks studied in (Bourke
et al., 2007)), check data from the
accelerometer during the next 10 seconds;
o If, in the next seconds, another positive of
the first point is detected or the “G-force”
average is lower than 1.2 G, start
“emergency procedure” (it was detected a
fall and the user isn’t moving anymore);
o (the movement values will be studied
more closely in the next phase of this
research).
Emergency procedure:
o The alarm is sounded by the speaker on
the collector and transmitter device;
o If, during the next 30 seconds, a “false
alarm” button in the collector device is
not pressed (to implement on the next
phase of this research), start the
automated call to the emergency services,
sending the location of the person
(detected by the GPS antenna) and the
data collected 30 seconds before the
scenario was detected;
o When it’s confirmed that an emergency
crew is on the way to the user’s location
to help, start sending the data collected
every 30 seconds, preceded by the
sending of the records of the last 24
hours.
Moreover, all the collected data are stored during 24
hours on the collector and then sent to a remote
database, which can be accessed and used by a
physician to detect some health issue not causing an
emergency.
4 RESULTS
By assembling the two concept parts, it was possible
to collect and interpret the “normal” vital signals
data from a person on a non-controlled environment
or state.
Making an automated device capable of
detecting health issues means it needs to have
sensors capable of measuring certain vital signals. In
line with this, the presented project is designed to be
able to recognize patient’s behavioural abnormality,
based on heartbeat, body temperature and body
movements.
IoTBDS 2018 - 3rd International Conference on Internet of Things, Big Data and Security
310
Related to the heart, this type of device would
have to be capable of detecting, for example, a
stroke. According to (Ritter et al., 2011), a stroke
can be diagnosed and evaluated using the pulse
BPM collected data and, as studied in (Glotzer et al.,
2003), it can also be detected thru Atrial High Rate.
Other important heart disease is arrhythmia which,
as tested in (Patel et al., 2012), is possible to detect
through the “R-R interval” (also known as “Inter
Beat Interval”). With Heart Rate Variability, it is
even possible to detect a Heart Failure case ((Nolan
et al., 1998)) and, as concluded in (Kligfield et al.,
1989), a Coronary Artery Disease can also be
assumed using data collected from heart rate.
Finally, it is also possible to establish a connection
between the heart rate and the probability of having
Cardiovascular Diseases, thus being an important
way of diagnose. To solve and be able to detect
these five studied types of heart diseases we used a
pulse sensor (Sparkfun Electronics, n.d.), measuring
BPM, ST segment and IBI of the patient.
About body temperature, it is needed to measure
the users’ one, allowing the device to detect any
abnormalities as described in (Lu and Dai, 2009)
(more specific to people above 65 years old) and
recognize patterns for diagnose after a stroke has
occur, as concluded in (Kammersgaard et al., 2002).
For that, the solution was using a body temperature
sensor found in (Sparkfun Electronics, n.d.).
Finally, using a 3-axis accelerometer ((Analog
Devices Inc., 2009)) the device can detect falls,
false-alarms and sleep monitoring the user, as
detailed in (Hjorth et al., 2012).
The only scenario coded so far was a small part
of the movement abnormalities detection one.
Because there were only tested the average signals,
it is not possible to present any significant results of
this at this stage of the project.
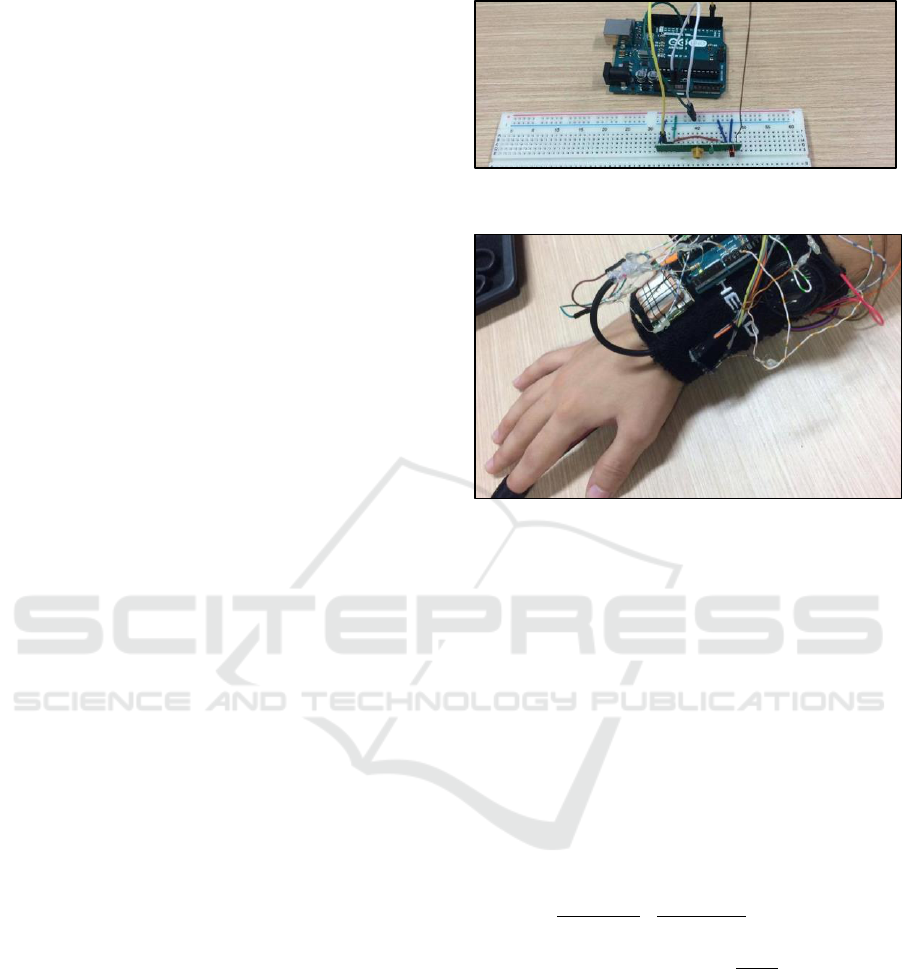
The Fig. 4 shows the current prototype of the
receiver and interpreter board, as well as the current
prototype of the collector and transmitter
(“Intelligent Health Monitoring Bracelet” – adapted
to a real-life bracelet – Fig.5). The current prototype
of the collector is yet in a large scale, which will be
reduced to a simple and discrete bracelet, replacing
the Arduino board with a smaller version for
wearable prototypes, also removing the extra amount
of wires and replacing some sensors with other
smaller and equivalent versions of them.
Figure 2: Current prototype of the receiver and interpreter.
Figure 3: Current prototype of the collector and
transmitter.
After assembling these two parts of the device,
we found some issues on working with all the
sensors together:
Receiver and interpreter:
o The length of the antenna had to be
calculated depending on the frequency of
the transmissions (0,17 metres as
calculated in (1)), the same that was
applied to the collector and transmitter. If
lower or higher than 17 centimetres, the
communication efficiency was lower in
distance (the average was around 15
metres).
=
≈ 0,691244
(1)
¼ of antenna wavelength =
≈ 0,17 metres
Collector and transmitter:
o The GPS antenna had to be tested
separately to the remaining sensors,
because when all were plugged to the
“5V” port, the GPS antenna didn’t receive
the minimal amount of current and
wouldn’t start seeking a satellite signal;
o The accelerometer sometimes presented
some values over 7 G-forces, due to bad
connections of the sensors’ pins;
Towards a Fully Automated Bracelet for Health Emergency Solution
311

The skin contact detection sensor works best in non-
fully dry skin, i.e. with some humidity in the human
tissue (because the resistance is lower – more similar
to the resistor used). To solve this, we forced the
sensor against the user skin, working as expected.
5 DISCUSSION AND
CONCLUSIONS
By crossing data from three sensors, namely, GPS,
accelerometer, pulse sensor, body temperature and
skin contact detection sensor, on the presented
scenarios and implementing the two devices
communication system, it is now possible to create a
new e-health and intelligent emergency solution,
with new features, complementing the ones
described in the Introduction section. The proposed
solution may solve several limitations observed on
the literature:
By removing the “human factor” during a routine
or an emergency call this is a quicker solution;
By sending the collected data from the 30
seconds before an emergency scenario detection
and every 30 seconds after, it allows the medical
crew to have real-time vital signals from the
user, decreasing the “first medical exam”
duration, done when arriving to the patients’
home, also decreasing the helping time,
increasing the chances of a good recovery of the
person;
By having an intelligent and advanced
emergency scenarios software detector, it is
avoided having an “emergency button” present
on the current devices, this way reducing the
chance of a “false alarm” or a false press of the
button;
With the data being stored and sent to a database,
it allows a doctor to constantly remotely monitor
the health of the user, being possible to detect
several health issues in an early stage.
The skin contact detection sensor had to be
implemented due to the non-exact values readied
from the pulse sensor (when not placed on the user’s
finger the values derivate from below 20 BPM and
higher than 200 BPM often) – this sensor has to be
on the users’ finger because it was designed for that
and when tested on the arm the values were not
correct (average of 20 BPM of difference to the real
ones). This same sensor was built by us, because we
didn’t find any identical on the market.
After testing the reading process of the sensors
data, we realize the storage capability of the Arduino
board was not enough and preferred to send them to
the receiver and interpreter device, being then stored
in a computer. The same was applied to the
scenarios recognition, offering a decrease of power
consume of the battery.
Regarding the frequency on which the data must
be collected, it is needed to study more deeply the
ideal of collections in one minute (the minimum that
won’t affect the emergency solution efficiency), due
to the high power consumption of the current one,
which is constantly reading new values.
For the communicators antenna length, it will be
sought a better antenna architecture, being then
possible to implement it more easily on a real life
wrist bracelet.
The list of the three sensors used were chosen
due to the data collected and described in the Results
section.
Related to the radio frequency communicators,
they were chosen instead of “Wi-Fi” or “Bluetooth”
due to the lower power consumption.
6 FUTURE WORK
Because this is an early stage of this project, it’s
only possible to us to present the work done so far.
On its next stage, there will be presented:
The results of the tests, involving the
scenarios detection (improve of the
current ones and addition of new ones);
The result of implementing an Artificial
Intelligence algorithm for analysing the
health data;
The power consumption of each sensor
used;
The battery power management
efficiency (turning on and off the
sensors to economize it);
Detailed success rates for the current
communication process and its
efficiency affected by distance, amount
of data and environment;
Possible communications alternatives,
to prevent data loss when in rooms with
many objects;
A new and more easy to use version of
the bracelet, using smaller and more
efficient sensors;
The results of the tests of the overall
system (synchronization, success rate of
IoTBDS 2018 - 3rd International Conference on Internet of Things, Big Data and Security
312

the communications and alarm
generation and success rate for the
health issue recognition).
ACKNOWLEDGEMENTS
Contributing to this research, the authors affiliated
with the Instituto de Telecomunicações also
acknowledge the funding for the research by means
of the program FCT project UID/EEA/50008/2013.
The authors would also like to acknowledge the
contribution of the COST Action IC1303 –
AAPELE – Architectures, Algorithms and Protocols
for Enhanced Living Environments.
REFERENCES
Administration on Aging; Administration for Community
Living; U.S. Department of Health and Human
Services, 2012. A Profile of Older Americans: 2012.
ADT LLC, n.d. Medical Alert System & Fall Detection
Monitoring from ADT [WWW Document]. URL
https://www.adt.com/health (accessed 9.29.16).
Alert1, n.d. Alert1 Medical Alert Services for Seniors
[WWW Document]. URL https://www.alert-1.com
(accessed 9.29.16).
Analog Devices Inc., 2009. ADXL335 3-Axis
Accelerometer Module [WWW Document]. URL
http://www.robotshop.com/en/3-axis-accelerometer-
module.html (accessed 2.26.17).
Barefoot, J.C., Schroll, M., 1996. Symptoms of
Depression, Acute Myocardial Infarction, and Total
Mortality in a Community Sample. Circulation 93,
1976. https://doi.org/10.1161/01.CIR.93.11.1976
Barg, F.K., Huss-Ashmore, R., Wittink, M.N., Murray,
G.F., Bogner, H.R., Gallo, J.J., 2006. A Mixed-
Methods Approach to Understanding Loneliness and
Depression in Older Adults. J. Gerontol. Ser. B 61,
S329–S339. https://doi.org/10.1093/geronb/61.6.S329
Bay Alarm Medical, n.d. Bay Alarm Medical: Medical
Alert Systems for Seniors [WWW Document]. URL
http://www.bayalarmmedical.com (accessed 9.29.16).
Bourke, A.K., O’Brien, J.V., Lyons, G.M., 2007.
Evaluation of a threshold-based tri-axial accelerometer
fall detection algorithm. Gait Posture 26, 194–199.
https://doi.org/10.1016/j.gaitpost.2006.09.012
FitBit, n.d. FitBit alta HR [WWW Document]. URL
https://www.fitbit.com/altahr (accessed 4.20.17).
Glotzer, T.V., Hellkamp, A.S., Zimmerman, J., Sweeney,
M.O., Yee, R., Marinchak, R., Cook, J., Paraschos, A.,
Love, J., Radoslovich, G., Lee, K.L., Lamas, G.A.,
2003. Atrial High Rate Episodes Detected by
Pacemaker Diagnostics Predict Death and Stroke.
Circulation 107, 1614. https://doi.org/10.1161/01.
CIR.0000057981.70380.45
HEART RATE AS A PROGNOSTIC FACTOR FOR
CORONARY HEART DISEASE AND
MORTALITY: FINDINGS IN THREE CHICAGO
EPIDEMIOLOGIC STUDIES | American Journal of
Epidemiology | Oxford Academic [WWW Document],
n.d. URL https://academic.oup.com/aje/article-
abstract/112/6/736/133827 (accessed 1.26.18).
Hjorth, M.F., Chaput, J.-P., Damsgaard, C.T., Dalskov, S.-
M., Michaelsen, K.F., Tetens, I., Sjödin, A., 2012.
Measure of sleep and physical activity by a single
accelerometer: Can a waist-worn Actigraph adequately
measure sleep in children? Sleep Biol. Rhythms 10,
328–335. https://doi.org/10.1111/j.1479-8425.2012.
00578.x
Ho, J.D., Dawes, D.M., Kroll, M.W., 2012. Atlas of
Conducted Electrical Weapon Wounds and Forensic
Analysis, 1st ed. Springer-Verlag New York, New
York.
Kammersgaard, L.P., Jørgensen, H.S., Rungby, J.A.,
Reith, J., Nakayama, H., Weber, U.J., Houth, J.,
Olsen, T.S., 2002. Admission Body Temperature
Predicts Long-Term Mortality After Acute Stroke.
Stroke 33, 1759. https://doi.org/10.1161/01.STR.
0000019910.90280.F1
Kligfield, P., Ameisen, O., Okin, P.M., 1989. Heart rate
adjustment of ST segment depression for improved
detection of coronary artery disease. Circulation 79,
245. https://doi.org/10.1161/01.CIR.79.2.245
Life Fone, n.d. Medical Alert System & Medical Alarm |
LifeFone [WWW Document]. URL
https://www.lifefone.com (accessed 9.29.16).
LifeStation Inc., n.d. Medical Alert System & Medical
Alarms | LifeStation [WWW Document]. URL
https://www1.lifestation.com/ (accessed 9.29.16).
Lloyd-Jones, D., Adams, R.J., Brown, T.M., Carnethon,
M., Dai, S., De Simone, G., Ferguson, T.B., Ford, E.,
Furie, K., Gillespie, C., Go, A., Greenlund, K., Haase,
N., Hailpern, S., Ho, P.M., Howard, V., Kissela, B.,
Kittner, S., Lackland, D., Lisabeth, L., Marelli, A.,
McDermott, M.M., Meigs, J., Mozaffarian, D.,
Mussolino, M., Nichol, G., Roger, V.L., Rosamond,
W., Sacco, R., Sorlie, P., Stafford, R., Thom, T.,
Wasserthiel-Smoller, S., Wong, N.D., Wylie-Rosett,
J., 2010. Heart Disease and Stroke Statistics—2010
Update. Circulation 121, e46. https://doi.org/
10.1161/CIRCULATIONAHA.109.192667
Luepker RV, Raczynski JM, Osganian S, et al, 2000.
Effect of a community intervention on patient delay
and emergency medical service use in acute coronary
heart disease: The rapid early action for coronary
treatment (react) trial. JAMA 284, 60–67.
https://doi.org/10.1001/jama.284.1.60
Lu, S.-H., Dai, Y.-T., 2009. Normal body temperature and
the effects of age, sex, ambient temperature and body
mass index on normal oral temperature: A prospective,
comparative study. Int. J. Nurs. Stud. 46, 661–668.
https://doi.org/10.1016/j.ijnurstu.2008.11.006
Medical Guardian LLC, n.d. Medical Alert Systems,
Devices & Alarms for Seniors in Emergencies |
Towards a Fully Automated Bracelet for Health Emergency Solution
313

Medical Guardian [WWW Document]. URL
https://www.medicalguardian.com (accessed 9.29.16).
Mi, n.d. Mi Band 2 [WWW Document]. URL
http://www.mi.com/en/miband2/ (accessed 4.20.17).
Nolan, J., Batin, P.D., Andrews, R., Lindsay, S.J.,
Brooksby, P., Mullen, M., Baig, W., Flapan, A.D.,
Cowley, A., Prescott, R.J., Neilson, J.M.M., Fox,
K.A.A., 1998. Prospective Study of Heart Rate
Variability and Mortality in Chronic Heart Failure.
Circulation 98, 1510. https://doi.org/10.1161/01.CIR.
98.15.1510
Patel, A.M., Gakare, P.K., Cheeran, A.N., 2012. Real
Time ECG Feature Extraction and Arrhythmia
Detection on a Mobile Platform.
Philips N.V., n.d. How We Help [WWW Document].
URL https://www.lifeline.philips.com (accessed
9.29.16).
Rescue Alert, n.d. Medical Alert Systems | Rescue Alert
[WWW Document]. URL https://www.rescuealert.
com (accessed 2.28.17).
Ritter, M.A., Rohde, A., Heuschmann, P.U., Dziewas, R.,
Stypmann, J., Nabavi, D.G., Ringelstein, B.E., 2011.
Heart rate monitoring on the stroke unit. What does
heart beat tell about prognosis? An observational
study. BMC Neurol. 11, 47. https://doi.org/10.1186/
1471-2377-11-47
Samsung, n.d. Samsung Gear S3 [WWW Document].
URL http://www.samsung.com/us/explore/gear-s3/
#specs (accessed 4.20.17).
Saúde Pública - Fatores associados a quedas em uma
coorte de idosos residentes na comunidade Fatores
associados a quedas em uma coorte de idosos
residentes na comunidade [WWW Document], n.d.
URL https://scielosp.org/scielo.php?pid=S0034-
89102002000700008&script=sci_arttext#ModalArticl
es (accessed 1.27.18).
Solodev, n.d. Medical Alert Systems from MobileHelp
[WWW Document]. URL http://www.mobilehelp.com
(accessed 9.29.16).
Sparkfun Electronics, n.d. Pulse Sensor - SEN-11574 -
SparkFun Electronics [WWW Document]. URL
https://www.sparkfun.com/products/11574 (accessed
9.29.16a).
Sparkfun Electronics, n.d. Temperature Sensor -
Waterproof (DS18B20) - SEN-11050 - SparkFun
Electronics [WWW Document]. URL
https://www.sparkfun.com/products/11050
Sparkfun Electronics, n.d. RF Link Transmitter - 434MHz
- WRL-10534 - SparkFun Electronics [WWW
Document]. URL https://www.sparkfun.com/
products/10534 (accessed 9.29.16c).
Sparkfun Eletronics, n.d. GPS Receiver - EM-506 (48
Channel) - GPS-12751 - SparkFun Electronics.
[WWW Document]. URL https://www.sparkfun.com/
products/12751 (accessed 9.29.16).
Tsipouras, M.G., Fotiadis, D.I., 2004. Automatic
arrhythmia detection based on time and time–
frequency analysis of heart rate variability. Comput.
Methods Programs Biomed. 74, 95–108.
https://doi.org/10.1016/S0169-2607(03)00079-8
United Nations, 2015. World Population Ageing [WWW
Document]. URL http://www.un.org/en/development/
desa/population/publications/pdf/ageing/WPA2015_R
eport.pdf (accessed 2.27.17).
VISATON GmbH & Co. KG, n.d. K 36 WP - 8 Ohm
[WWW Document]. URL http://www.visaton.de/en/
industrie/klein/k36wp_8.html (accessed 9.29.16).
IoTBDS 2018 - 3rd International Conference on Internet of Things, Big Data and Security
314
