
Factors Affecting Lower Back Pain (LBP) among Undergraduate
Nursing Students
Rifa Rindayani Syafitri, Ira Suarilah and Makhfudli
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
Keywords: Lower Back Pain, Nursing Students, Biological Factors, Psychological Factors, Social Factors.
Abstract: Introduction: The earlier young people experience lower back pain (LBP), the more potential there is to
acquire chronic back pain in the future. Nursing is a high-risk job regarding LBP. Knowing the factors that
affect the occurrence of LBP in nursing students is important to prevent LBP when working as a nurse later.
Methods: This study analyzed the factors that influence the occurrence of LBP in nursing students at the
Faculty of Nursing, Universitas Airlangga. A stratified random sampling method was used. This study was a
cross-sectional study with questionnaires as the method for data collection, and a logistic regression test for
data analysis. The sample comprised of 120 undergraduate nursing students. The independent variables
were factors influencing the occurrence of LBP: biological, psychological, and social factors. The
dependent variable was the occurrence of LBP during the last 12 months. Results: As many as 60% of
students experienced LBP in the last 12 months and significant factors affecting LBP were: history of spinal
trauma (p = 0.023), stress level (p = 0.000), sports habits (p = 0.044), and motor vehicle usage (p = 0.033).
Conclusions: Biological, psychological, and social factors influence the occurrence of LBP in nursing
students. Avoiding factors affecting LBP may reduce the prevalence and impact of LBP in the nursing
profession.
1 BACKGROUND
Symptoms of lower back pain (LBP) or perceived
pain in the lower back region (Wulandari, 2014) is
major causes of disability, absenteeism, and poor
performance at work (Novitasari et al., 2016). Most
of the research on LBP is performed in adults
engaged in certain types of work, so there is little
understanding of the onset of early LBP among
adolescents and young adults (Heuscher et al.,
2007). The incidence of LBP in the early stages of
life increases the chronic, recurrent risk of LBP,
which potentially reduces the efficiency of the
young population (Study et al., 2017).
Anderson (1999) estimates the prevalence of
LBP in the world at30% (Study et al., 2017).
Research in Perth (Australia), shows that more than
30% of nursing students in clinical education have
experienced LBP in the past 12 months (Mitchell et
al., 2009). In Indonesia, the number of LBP patients
is not known, but it is estimated to be between 7.6%
to 37% (Lailani, 2013). The prevalence of LBP in
nurses in Jakarta is around 61.1% (Kurniawidjaja et
al., 2013). The researchers conducted a preliminary
study in September 2017 with 16 undergraduate
nursing students at Universitas Airlangga (Unair)
who had not undergone professional education, aged
17–35 years. It was determined that 12 students had
suffered with LBP during the last 12 months, but the
factors affecting LBP are still inexplicable.
The risk factor for LBP is a multifactorial
biopsychosocial problem (Mitchell et al., 2009).
Biological factors that can affect the occurrence of
LBP are biomechanics, the central nervous system,
and personal factors. A psychological factor that can
cause LBP is stress. Social factors, such as smoking,
backpack use, driving, sports habits, and
environmental factors, including mattress used, can
also cause LBP (Farrokhi et al., 2017).
According to a preliminary study, all Unair
nursing students complained about the severity of
academic demands. Purwati (2012) states that the
demands of academic work cause students to
experience stress that can have a negative impact
such as starting smoking. time demand lectures and
tasks increase the duration of sitting so there is a
decrease in physical activity. The results of a study
by Idyan (2005) regarding extension students at the
138
Syafitri, R., Suarilah, I. and Makhfudli, .
Factors Affecting Lower Back Pain (LBP) among Undergraduate Nursing Students.
DOI: 10.5220/0008321701380145
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 138-145
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
Faculty of Nursing Universitas Indonesia, of 35
respondents who sat in every lecture for 1–3 hours,
51.4% experienced severe pain (Saputra, 2009). The
majority of Unair nursing students say the demands
of the tasks cause them to stay up late, so they
consume coffee to relieve drowsiness. Unair nursing
students often carry heavy bags containing a laptop,
medical books, and lecture notes. The majority of
Unair students live in the boarding houses and most
of them complain about their uncomfortable
mattresses. The characteristics of Surabaya as a big
city causes congestion on the road. Congestion
results in an increase in travel time and increased
psychological stress (Tondok, 2009). All Unair
nursing students usually use private vehicle
transportation (cars and motorcycles), because they
feel more safe and comfortable.
In Indonesia, there are still limited studies on risk
factors for LBP. This is important to discuss because
work and lifestyles in Indonesia are not the same as
in places abroad (Kurniawidjaja et al., 2013).
Discussion about risk factors of LBP among nursing
students who have not undergone clinical education
is important based on the high incidence of LBP in
previous research. Therefore, before starting work as
a nurse, attempts to prevent LBP should be carried
out. Based on the description above, the researcher
is interested in analyzing the factors that affect the
occurrence of LPB in students at the Faculty of
Nursing, Universitas Airlangga.
2 METHODS
This research was carried out using a cross-sectional
design, using binary logistic regression statistic test
to measure the influence of the independent variable
on the dependent variable with the degree of
significance p <0.05. The population of this research
were bachelor students from the Faculty of Nursing
at Universitas Airlangga (Unair), who were active
students, aged 1-35 years, with experience of LBP or
not in the last 12 months, and not currently
undergoing clinical education. The total sample was
120 respondents selected by simple stratified
random sampling. This research already has ethical
approval by the Ethical Committee for Health
Research at Universitas Airlangga, No: 582-KEPK.
The independent variables of this study were
factors that influence the occurrence of LBP with
biological factors (age, BMI, history of spinal
trauma, and family disease history associated with
LBP), psychological factors (stress level), social
factors (sitting habits, exercise habits, smoking,
coffee consumption, use of bags, use of mattresses,
and use of motor vehicles). The dependent variable
was the incidence of LBP over the past 12 months.
The research instrument was modified from the
Nordic Low Back Pain questionnaire (Kuorinka et
al., 1987) to measure the incidence of LBP in the
last 12 months and the risk level of disability,
depression anxiety stress scale (DASS) 42
(Psychology Foundation of Australia, 2014) to
measure social factors, and the modified
questionnaire from previous studies by Korovessis
(2010) and Widiasih (2015) to measure biological
and social factors.
3 RESULTS
The population sample represents 16.67% of the
study. Table 1 illustrates the demographic
characteristics of the population. There are 20
respondents per class and most are female (81.7%).
Most respondents had experienced LBP during the
last 12 months (60%).
Table 2 shows the results of the distribution of
data measured regarding the biological,
psychological, and social factors of the respondents.
In relation to biological factors, most respondents, in
the final adolescent age range (90%), had a normal
BMI (65.8%), had never had a spinal trauma
(91.7%), and had no family disease history
associated with LBP (95.8%). In relation to
psychological factors, most respondents experienced
a normal stress level (40%). For social factors, most
respondents sat for 6–9 hours per day (66.7%), took
part in sports <2 hours per week (31.7%), did not
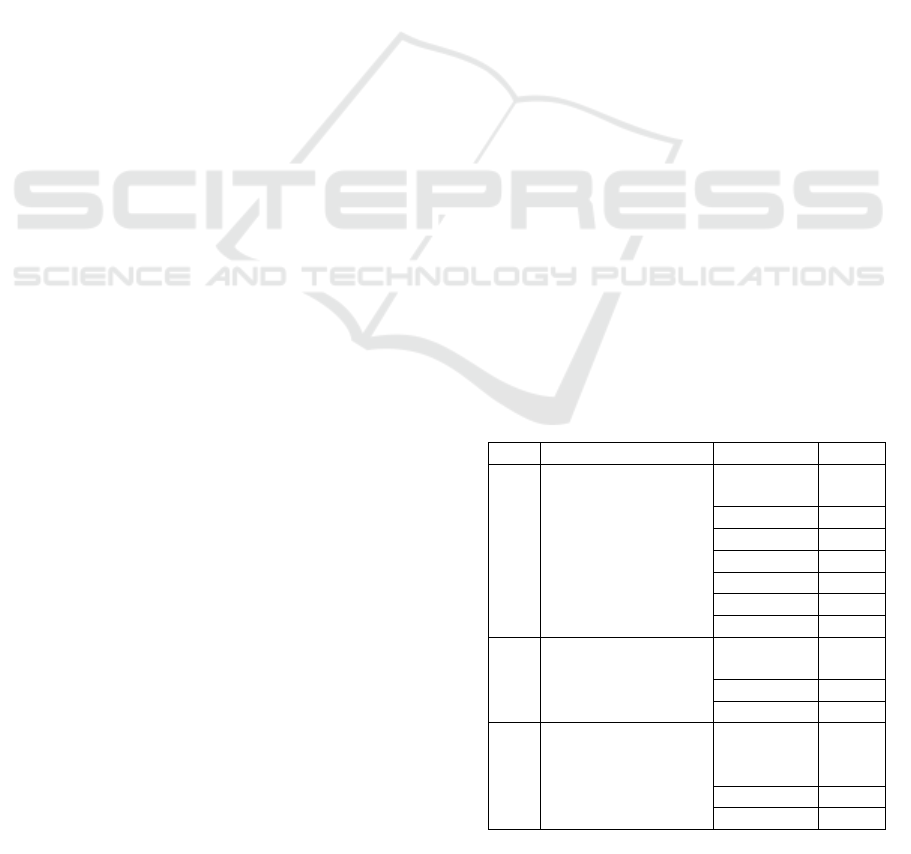
Table 1: Demographic data of respondents
No Characteristics Frequency %
1. Class year
4
th
year
3
rd
year
2
nd
year
1
st
year
2
nd
year (extension)
1
st
year (extension)
Total
20
16.7
20 16.7
20 16.7
20 16.7
20 16.7
20 16.7
120 100
2. Age
Male
Female
Total
22
18.3
98 81.7
120 100
3. The LBP incident in
the last 12 months
Never experienced
Ever experienced
Total
48
40.0
72 60.0
120 100
Factors Affecting Lower Back Pain (LBP) among Undergraduate Nursing Students
139
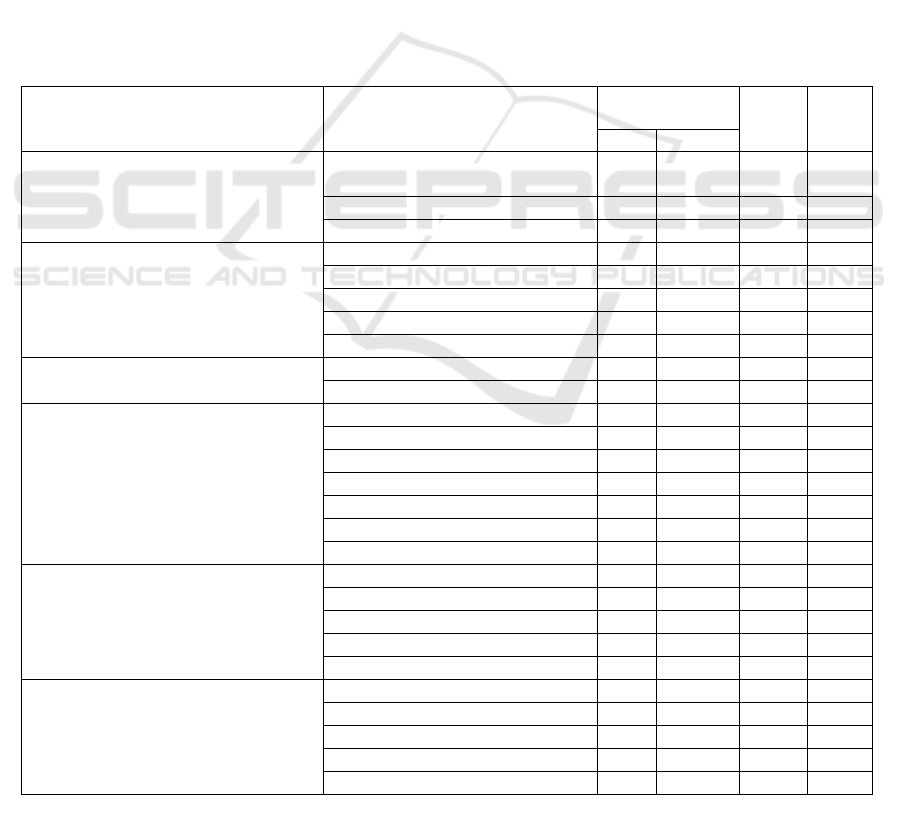
smoke (96.7%), did not consume coffee (62.5%),
used bags with two shoulders straps (85.8%),
described the bag as having a normal weight (55%),
carried bags for 10–20 minutes (30.8%), described
their mattresses with medium description (60%), and
used motor vehicles for around 20–40 minutes per
day (29.2%).
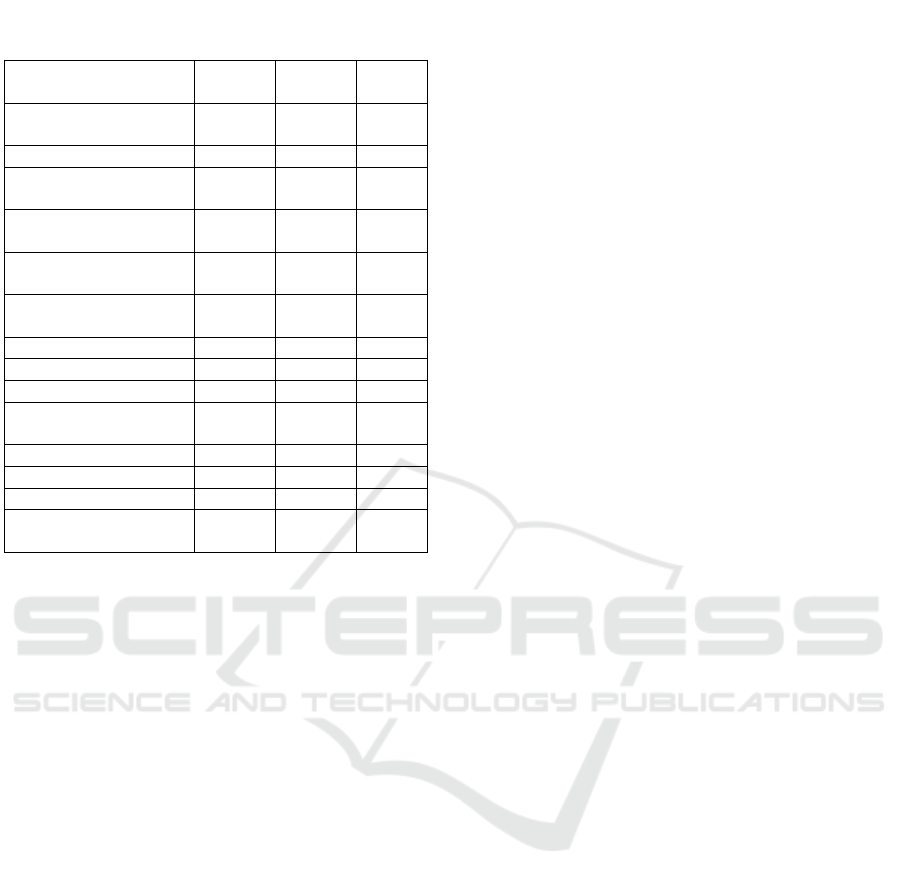
Table 3 shows the results of the logistic
regression test; the factors that significantly
influence the occurrence of LBP are the history of
spinal trauma (biological factor), stress level
(psychological factor), sports habits and the use of
motor vehicles (social factors). The magnitude of
influence can be shown by the value of the Odds
Ratio (OR). The result of data analysis indicates that
the greater history of spinal trauma, the higher
chance of LBP, the higher the stress level, the higher
chance of LBP, the longer time exercising time in
one week, the lower chance of LBP, the longer the
driving time, the higher likelihood of LBP. From the
logistic regression analysis, it is clear that the history
of spinal trauma is the most dominant factor
affecting the incidence of LBP.
4 DISCUSSION
4.1 Analysis of the Influence of
Biological Factors on the
Occurrence of LBP
Analysis on the biological effects of age, BMI,
history of spinal trauma, and family history of LBP
is discussed in this section.
Table 2: The Measurements of Variable Data Distribution in the Biological, Psychological, and Social Factors of
Respondents.
Measured Variables Category
LBP the last 12
months
f %
No Yes
Biological Factors
Age
Early adolescents (12–16 years
old)
0 0 0 0
Teenagers (17–25 years old)
45 63 108 90.0
Early Adult (26–35 years old)
3 9 12 10.0
BMI
Very thin (BMI <17)
1 3 4 3.3
Thin (BMI 17–18,4)
7 10 17 14.2
Normal (BMI 18.5–25)
35 44 79 65.8
Fat (BMI 25,1–27)
4 3 7 5.8
Very Fat (BMI> 27)
1 12 13 10.8
History of Spinal Trauma
Never experienced
48 62 110 91.7
Ever experienced
0 10 10 8.3
Medical diagnosis of respondents who
have experienced spinal trauma
Minor injury
- - 3 2.5
Dislocation
- - 2 1.7
Fracture of the sacrum
- - 1 0.8
LBP
- - 1 0.8
Spondylolisthesis
- - 1 0.8
Lumbar muscle spasms
- - 1 0.8
Coccydynia
- - 1 0.8
Family Disease History Associated
with LBP
Chronic LBP
0 1 1 0.8
Osteoarthritis <50 years of age
1 2 3 2.5
Disk hernia
0 0 0 0
Spinal form disorders
1 0 1 0.8
None
46 69 115 95.8
Psychological Factor
Stress Level
Awful
0 8 8 6.7
Severe
0 19 19 15.8
Medium
5 22 27 22.5
Light
8 10 18 15.0
Normal
35 13 48 40.0
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
140
4.1.1 The Influence of Age
Age did not have a significant effect on the
occurrence of LBP, which is not in accordance with
the assertion that the older a person becomes, the
greater the risk of LBP due to bone degeneration. At
the age of 30 years, degeneration occurs in the form
of tissue damage (Andini, 2015). The onset of bone
degeneration cannot be prevented, but LBP can be
prevented by strengthening bone and muscle
structure. Exercise and nutritional balance can
maintain the strength of the musculoskeletal system
(Gabr & Al-eisa, 2017). Differences in previous
research could be caused by the definition of early
adulthood beginning at the age of 26 in this study, so
it can be concluded that respondents aged less than
30 years have not risked the occurrence of bone
degeneration that can cause bias in the early adult
age range. Age factors still need to be considered to
prevent early bone degeneration in college students.
4.1.2 The Influence of BMI
Results showed that BMI did not affect the
occurrence of LBP. This was relevant to a previous
study by Koley et al. (2010) in India and Mangwani
et al. (2010) in the UK showed no significant
difference between BMI and LBP (Lailani, 2013).
The result study by Yasin et al. (2010) in RSDS
Surabaya indicates that BMI influences the
occurrence of LBP. Increased BMI can weaken
abdominal muscles, so that the center of gravity is
pushed to the front of the body causing an increase
in lumbar lordosis and fatigue in the paravertebral
muscle. The mismatch of the research results to the
theory may be influenced by the respondents’
increased time spent sitting; the burden of the
abdomen is sustained by the thigh, so it will not
burden the spine.
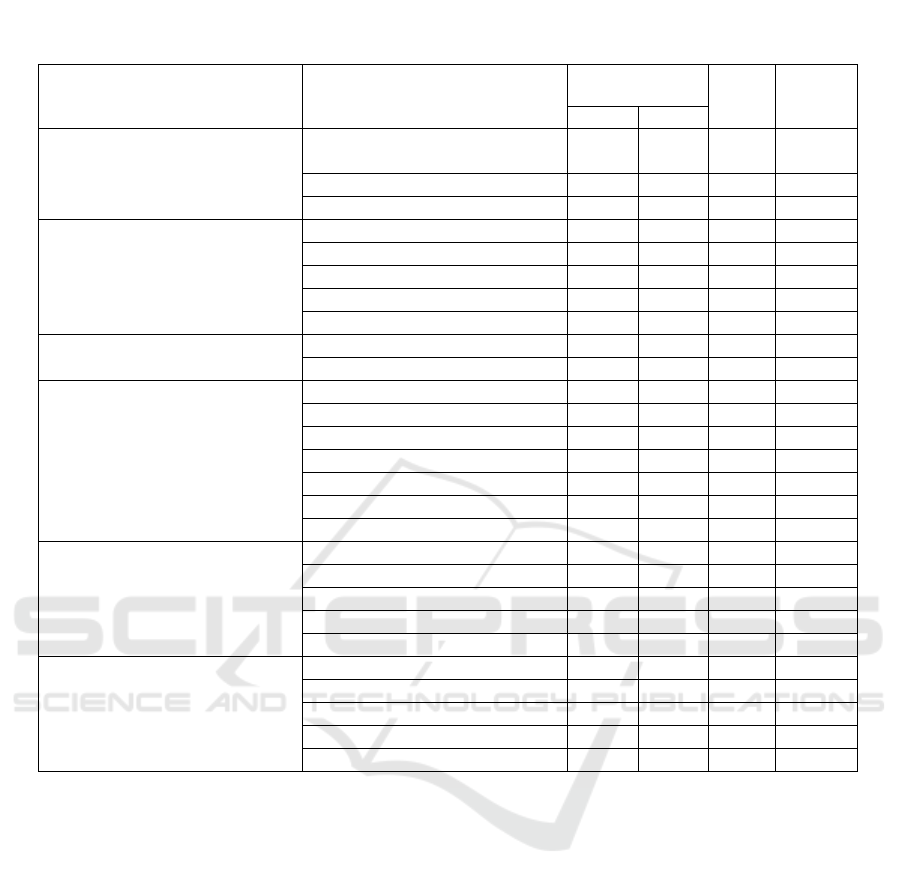
Table 2: The Measurements of Variable Data Distribution in ... (continued)
Measured Variables Category
LBP the last 12
months
f %
No Yes
Biological Factors
Age
Early adolescents (12–16 years
old)
0 0 0 0
Teenagers (17–25 years old)
45 63 108 90.0
Early Adult (26–35 years old)
3 9 12 10.0
BMI
Very thin (BMI <17)
1 3 4 3.3
Thin (BMI 17–18.4)
7 10 17 14.2
Normal (BMI 18.5–25)
35 44 79 65.8
Fat (BMI 25,1–27)
4 3 7 5.8
Very Fat (BMI> 27)
1 12 13 10.8
History of Spinal Trauma
Never experienced
48 62 110 91.7
Ever experienced
0 10 10 8.3
Medical diagnose on
respondents who had
experienced spinal trauma
Minor injury
- - 3 2.5
Dislocation
- - 2 1.7
Fracture of the sacrum
- - 1 0.8
LBP
- - 1 0.8
Spondylolisthesis
- - 1 0.8
Lumbar muscle spasms
- - 1 0.8
Coccydynia
- - 1 0.8
Family Disease History
Associated with LBP
Chronic LBP
0 1 1 0.8
Osteoarthritis <50 years of age
1 2 3 2.5
Disk hernia
0 0 0 0
Spinal form disorders
1 0 1 0.8
None
46 69 115 95.8
Psychological Factor
Stress Level
Awful
0 8 8 6.7
Severe
0 19 19 15.8
Medium
5 22 27 22.5
Light
8 10 18 15.0
Normal
35 13 48 40.0
Factors Affecting Lower Back Pain (LBP) among Undergraduate Nursing Students
141
4.1.3 Influence of History of Spinal Trauma
The results indicated that the history of spinal
trauma influenced the occurrence of LBP; the more
history of spinal trauma, the higher chance of LBP
occurrence. Hendri (2014) also states that a history
of back injury has a risk of LBP 1.95 times greater
than with no history. The spine has an extremely
sturdy and stable structure (Standring, 2016). The
intervertebral discs form a strong joint that allows
the spine to move and support a heavy burden
(Widiasih, 2015). Spinal trauma may alter the
structure of the spine, but the recovery system of the
spinal structure may support its regeneration (Munir,
2012). Most respondents are late adolescents so the
backbone should still be able to regenerate
optimally. The backbone is a solid unit, but in the
results of bone trauma studies can cause LBP. This
may be because the respondents’ history of spinal
trauma is so severe that it causes damage to the
backbone structure, causing LBP to occur.
4.1.4 Influence of Family Disease History
The results showed that family history did not affect
the occurrence of LBP. The results did not match the
assertion that some elements of genetic factors that
can affect the occurrence of LBP, include the
receptor elements of vitamin D, VDR, COL1,
COL9, and Aggrecan. Matsui et al. (1997) suggest
that family history of disc herniation has a
significant relationship to the occurrence of Discus
Degenerative Disease with vitamin D receptors as
one of the disposition genes. VDR plays a role in
normal bone mineralization and remodeling.
Osteoarthritis is associated with the VDR gene.
COL1 and COL9 play a role in facilitating the stress
of the intervertebral discs. Aggrecan acts as a fluid
binder that keeps nucleus pulposus well hydrated
(Hemanta et al., 2016). Genetic factors also
contribute to sensitivity to pain, such as the disorder
of the spine (scoliosis), and degeneration of the
discus (Wong et al., 2017). The differences with the
theory may be caused by only a minority of
respondents who have a family history of disease
associated with LBP. Most respondents never
experienced spinal cord injury, so the spinal
structure should not be disturbed. Also, most
respondents were in the late adolescent age range.
However, it is necessary to be more vigilant if you
have parents who have a family history of illness
that can affect the occurrence of LBP.
4.2 Analysis of the Influence of
Psychological Factors on the
Occurrence of LBP
Most respondents experienced stress. Stress levels
stress affect the occurrence of LBP; the higher the
level of stress, the higher the chance of LBP
occurrence. Research by Purwati (2012) in FIK UI
shows that nursing students have high stress levels.
Stress is a psychological factor that can cause LBP
(Farrokhi et al., 2017). Stress can cause pain through
increased spinal mechanical load due to increased
muscle tension (Mitchell et al., 2009). This study did
not measure the causes of stress, but based on
preliminary studies, stress was caused by heavy
academic demands. Stress on Unair nursing students
needs to be anticipated. Stress can directly affect the
onset of symptoms of disease, e.g. LBP, but stress
can also cause various behaviors that can trigger the
occurrence of LBP, such as smoking.
4.3 Analysis of the Influence of Social
Factors on the Occurrence of LBP
Analysis on the social influences of length of time
sitting, exercise habits, smoking, coffee
consumption, the use of bags, mattress description,
and the length of time using motor vehicles
compared with the occurrence of LBP are discussed
in this section.
Table 3: Bivariate Test Results Between Independent
and Dependent Variables.
B
P
value
OR
Biological Factors
BMI -0.221 0.592 0.801
Age -1.275 0.228 0.280
History of Spinal
Trauma 3.275 0.023 26.4
Family Disease
Histor
y
-0.441 0.414 0.643
Psychological Factors
Stress Level 1.550 0.000 0.212
Social Factors Sitting
habits -1.051 0.145 0.349
Physical Exercise -0.852 0.044 0.427
Smokin
g
-2.020 0.188 0.133
Drinkin
g
coffee -0.120 0.833 0.887
Carrying Bag
Carrying style -1.779 0.087 0.169
Wei
g
ht -0.800 0.144 0.449
Duration -0.230 0.373 0.794
Matrass 0.271 0.659 1.31
Transportation from
and to cam
p
us -0.620 0.033 0.538
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
142

4.3.1 The Influence of Time Spent Sitting
The results showed that Unair nursing students
regularly sat for 6–9 hours but the habit of sitting did
not significantly affect LBP occurrence. The results
do not match previous studies. Matthews et al.
(2012) states that sitting for 6–9 hours a day
increases the risk of LBP and sitting more than 9
hours a day is classified as too long sitting (Van der
Ploeg et al., 2012). Sitting for a long time can reduce
lubrication in the joints, causing stiffness (Widiasih,
2015). Continuous seated work causes muscle
contraction to become static and causes repetitive
muscle loading, which blocks blood flow, so that the
oxygen supply is insufficient for aerobic
metabolism. This condition causes accumulation of
lactic acid accumulation and body heat, ultimately
causing skeletal muscle fatigue in a form of muscle
satisfaction.
The mismatch of the study and the theory may be
because respondents who sit for shorter lengths of
time are likely to have other LBP risk factors that
may cause bias on the results. This study also did not
measure how the length of time sitting, posture, and
ergonomic modelled seating commonly used by
students. Anatomically, sitting in a non-upright
position and frequently changing the sitting posture
reduces the load between bone segments, and
provides a discus of time to enter water and nutrients
to keep the disc moist and regenerate in the form of
collagen tissue therein. Students’ sitting habits
require special attention, considering most sit for 6–
9 hours daily. It is advisable not to sit for more than
six hours a day, and if there is no choice, it is
important to stretch and change position as often as
possible during sitting.
4.3.2 The Influence of Exercise Habits
Most respondents only exercise <2 hours per week,
and exercise has a significant effect on the
occurrence of LBP. The results of data analysis
showed that the longer exercise time in one week,
the lower the chance of LBP occurrence. The results
are consistent with the assertion that exercise can
increase the strength and flexibility of the spinal
support muscles, so regular exercise can reduce the
risk of LBP (Kurniawidjaja et al., 2013). Korovessis
et al. (2010) also state that more frequent exercise (>
6 hours per week) showed a lower incidence of LBP
than for those not exercising. Regular exercise can
improve the quality of life, prevent osteoporosis and
various diseases of the skeleton and other diseases
(Andini, 2015). Respondents who exercised for
longer did not experience LBP, i.e. with frequent
sports such as jogging, dancing, and gymnastics.
This type of exercise not only increases muscle and
bone strength, but can also train and maximize
flexibility between joints, so that the structure of the
spine is stronger and the spine's ability to hold the
load can increase.
4.3.3 The Influence of Smoking
According to the results, smoking does not affect the
occurrence of LBP, which is not supported by some
previous studies. Hemanta et al. (2016) suggest that
smoking can lead to reduced blood flow to the
vertebral body, and lower bone mineral content,
which promotes intervertebral disc degeneration.
Nicotine also induces irreversible disc degeneration.
The mismatch with previous studies could be
because almost all respondents were not smokers.
There is an absence of measurements as to how long
the respondent had smoked, nor is there any
literature that states whether the length of time
smoking can affect LBP; the rare frequency of
smoking could also cause bias on the results.
4.3.4 The Influence of Coffee Consumption
Results showed that coffee consumption had no
significant effect on the occurrence of LBP, which
differ from the opinion of Hallstrom (2010) who
states that coffee consumption can accelerate bone
degeneration. Coffee consumption more than three
times per week had a higher risk (88%) of LBP
(Huang et al., 2014). Caffeine helps in overcoming
fatigue and drowsiness and reduces pain, but Currie
(1995) states the importance of reducing coffee
intake, because caffeine contributes to the
modulation of pain perception in various acute pain
states. Caffeine also increases urinary calcium and
may have long-term adverse effects on bones
(Alshagga et al., 2013). Until now there is still no
literature that states how much coffee should be
consumed to cause the risk of LBP. The Dietary
Guidelines Advisory Committee recommends no
more than 400 mg/day of coffee (equivalent to 3–5
cups). The maximum coffee drinking limit has
different effects on individuals, such as heart
palpitations, nausea, and vomiting (Sass, 2015).
Coffee has beneficial effects but also has long-
term effects that are very harmful, so the coffee-
drinking habits of nursing students should be
anticipated. This must be individualised as everyone
has different toleration of coffee. The mismatch with
previous research could be because this study does
not measure the concentration level of coffee
consumed per cup and how long the students
Factors Affecting Lower Back Pain (LBP) among Undergraduate Nursing Students
143

consume coffee for, so further research on the level
of coffee concentration and duration of coffee
consumption should be conducted to determine how
that may affect LBP occurrence.
4.3.5 Effect of Bag Usage
The results of carrying a bag, the bag’s weight and
the length of time carrying the bag have no
significant effect on LBP occurrence. This was a
different opinion to that of Korovessis et al. (2010)
who state in their study that backpacks with one or
both shoulders cause LBP. Aggarwal (2017) states
that an increase in bag load can explain the increase
in LBP. Korovessis et al. (2010) state that high
school students in Greece show that the use of bags
with heavy descriptions has the highest significance
value compared with the description of normal or
very heavy bags. The use of backpacks for 40–60
minutes has a higher significance value compared to
<40 minutes.
The mismatch with previous studies could be
because most respondents only carry their bags for
10–20 minutes. Respondents often use vehicles to
travel to the campus and usually put their bags on
chairs or on the floor when they arrive at the
campus, reducing the duration of time carrying bags.
The data also determines that Unair nursing students
who carry bags >1 hour per day do not experience
LBP, which is different to the theory. This could be
because students carrying bags for longer may only
be carrying lighter loads.
4.3.6 Effect of Mattress Description
The results showed that the types of mattress used
did not have a significant effect on the occurrence of
LBP. This is different to the opinion of Korovessis
et al. (2010) who states that a hard mattress has a
significant effect on the incidence of LBP in school
students. A hard bed will cause static and recurrent
muscle loading causing blocked blood flow,
resulting in insufficient oxygen supply for aerobic
metabolism. This condition causes the accumulation
of lactic acid accumulation and body heat, ultimately
causing skeletal muscle fatigue (Widiasih, 2015).
The use of appropriate mattresses in most
respondents caused the mismatch with previous
research, which states that a hard mattress
significantly affects the occurrence of LBP. Based
on raw data of respondents who perceived a hard
mattress experienced LBPThis is in sharp contrast to
previous theories that suggest that a soft mattress
will reduce muscle tension. Based on this, it can be
attributed as a cause of LBP; multifactorial and
biopsychosocial approaches can also explain the
occurrence of LBP, i.e. biological, psychological,
and social factors are interrelated.
4.3.7 Influence of the Use of Motor Vehicles
The results showed that the duration of using motor
vehicles in a day can affect the occurrence of LBP:
the longer the driving time, the higher the chance of
LBP occurrence. This is consistent with claims that
driving with a vibrating vehicle (car or motorcycle)
has the potential to generate LBP. Vibration may
cause increased muscle contractions resulting in
poor blood circulation, accumulation of lactic acid,
and pain (Andini, 2015). Complaints of LBP will be
felt after six months, if motorcyclists routinely drive
every day for at least 2.5 hours (Saputra, 2009).
Based on preliminary studies, most respondents
travel on motorcycles and carry heavy bags, which
will further increase the burden and pressure on the
lower back and increase the risk of LBP. This
research does not link motorcyclists and motorists to
LBP, but almost all students travel to work on
motorcycles, so it can be generalized that the
duration of driving on motorbikes might influence
the occurrence of LBP. This study did not measure
how long the students had been driving a motor
vehicle: it could be that nursing students had used
motor vehicle since high school, or since becoming a
student, junior high school or even elementary
school, so this needs further consideration to achieve
more accurate results.
5 CONCLUSIONS
The results reinforce the previous theory that LBP is
a biopsychosocial problem. Factors influencing the
occurrence of LBP in nursing students of Universitas
Airlangga can be based on biological factors, such as
the history of spinal trauma, psychological factors
such as stress levels, on social factors, such as sport
habits and motor vehicle usage. The most dominant
factor of LBP is the history of spinal trauma. It is
suggested that nursing students prevent factors
affecting LBP, and further research related to LBP is
also recommended.
ACKNOWLEDGEMENTS
The author is very grateful to the participants, the
undergraduate nursing students of the Faculty of
Nursing, Universitas Airlangga.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
144

REFERENCES
Alshagga, M. A., Nimer, A. R., Yan, L. P., Abdel, I.,
Ibrahim, A., & Al-ghamdi, S. S. (2013). Prevalence
and factors associated with neck , shoulder and low
back pains among medical students in a Malaysian
Medical College.
Andini, F. (2015). Risk factors of low back pain in
workers, 4, 12–19.
Farrokhi, S., Mazzone, B., Schneider, M., Gombatto, S.,
Highsmith, M. J., & Hendershot, B. D. (2017).
Biopsychosocial Risk Factors Associated with Chronic
Low Back Pain after Lower Limb Amputation.
Medical Hypotheses.
https://doi.org/10.1016/j.mehy.2017.07.030
Gabr, S. A., & Al-eisa, E. S. (2017). Mechanical factors
and vitamin D deficiency in schoolchildren with low
back pain : biochemical and cross-sectional survey
analysis, 855–865.
Hemanta, D., Jiang, X., & Feng, Z. (2016). Etiology for
Degenerative Disc Disease. Chinese Medical Sciences
Journal, 31(3), 185–191.
https://doi.org/10.1016/S1001-9294(16)30049-9
Heuscher, Z., Gilkey, D. P., Peel, J. L., & Kennedy, C. A.
(2007). The Association of Self-Reported Backpack
Use and Backpack Weight With Low Back Pain
Among College Students. Journal of Manipulative and
Physiological Therapeutics, 33(6), 432–437.
https://doi.org/10.1016/j.jmpt.2010.06.003
Huang, H., Chang, H., Lin, K., & Chiu, H. (2014). A
Closer Examination of the Interaction Among Risk
Factors for Low Back Pain, 28(6), 372–379.
https://doi.org/10.4278/ajhp.120329-QUAN-171
Kuorinka, I., Jonsson, B., Kilbom, A., & Vinterberg, H.
(1987). Standardised Nordic questionnaires for the
analysis of musculoskeletal symptoms, 233–237.
Kurniawidjaja, L. M., Purnomo, E., Maretti, N., Pujiriani,
I., Kajian, P., Kerja, K., … Keselamatan, M. (2013).
Pengendalian Risiko Ergonomi Kasus Low Back Pain
pada Perawat di Rumah Sakit Ergonomic Risk Control
on Low Back Pain among Hospitals â€
TM
Nurses,
46(4), 225–233.
Lailani, T. M. (2013). Hubungan antara Peningkatan
Indeks Massa Tubuh dengan Kejadian Nyeri
Punggung pada Pasien Rawat Jalan di Poliklinik Saraf
RSUD Dokter Soedarso Pontianak. Retrieved from
http://uad.portalgaruda.org/index.php?page=19&ipp=1
0&ref=browse&mod=viewjournal&journal=2307
Mitchell, T., Sullivan, P. B. O., Smith, A., Burnett, A. F.,
Straker, L., Thornton, J., & Rudd, C. J. (2009).
International Journal of Nursing Studies
Biopsychosocial factors are associated with low back
pain in female nursing students : A cross-sectional
study, 46, 678–688.
https://doi.org/10.1016/j.ijnurstu.2008.11.004
Munir, S. (2012). Analisis Nyeri Punggung Bawah pada
Pekerja Bagian Final Packing dan Part Supply di PT.
X Tahun 2012. Universitas Indonesia.
Novitasari, D. D., Sadeli, H. A., Soenggono, A., Sofiatin,
Y., Sukandar, H., & Roesli, R. M. A. (2016).
Prevalence and Characteristics of Low Back Pain
among Productive Age Population in Jatinangor, 469–
476.
Psychology Foundation of Australia. (2014). Depression
Anxiety Stress Scale (DASS). Retrieved September
11, 2017, from http://www2.psy.unsw.edu.au/dass/
Purwati, S. (2012). Tingkat Stres Akademik pada
Mahasiswa Reguler Angkatan 2010 Fakultas Ilmu
Keperawatan Universitas Indonesia Tingkat Stres
Akademik Pada Mahasiswa Reguler Angkatan 2010.
Universitas Indonesia.
Saputra, R. H. (2009). Hubungan Lama Berkendara
dengan pada Pengendara Sepeda Motor. Universitas
Muhammadiyah Surakarta.
Sass, C. (2015). How Much Coffee Should You Really Be
Drinking? Retrieved December 5, 2017, from
http://www.health.com/nutrition/how-much-coffee-is-
healthy
Standring, S. (2016). Grey’s Anatomy: The Anatomy Bases
of Clinical Practice (41st ed.). London: Elsevier.
Study, Y. A. A. C., Ganesan, S., Acharya, A. S., Chauhan,
R., & Acharya, S. (2017). Prevalence and Risk Factors
for Low Back Pain in 1,355 Young Adults: A Cross-
Sectional Study. Asian Spine Journal, 610–617.
https://doi.org/10.4184/asj.2017.11.4.610
Tondok, M. S. (2009). Stress Kemacetan Lalu-Lintas :
Bagaimana Mengatasinya ?, 2–5.
Widiasih, G. (2015). Hubungan Posisi Belajar dan Lama
Duduk. UIN Syarif Hidayatullah Jakarta.
Wong, A. Y. L., Karppinen, J., & Samartzis, D. (2017).
Low back pain in older adults : risk factors ,
management options and future directions, 1–23.
https://doi.org/10.1186/s13013-017-0121-3
Wulandari, R. A. (2014). Gambaran Faktor yang
Mempengaruhi Nyeri Punggung Bawah pada Buruh
Kapal, 1–8.
Factors Affecting Lower Back Pain (LBP) among Undergraduate Nursing Students
145
