
The Effect of Walking Exercise and Pursed Lips Breathing on Signs
and Symptoms of COPD Patients: A Systematic Review
Arum Dwi Ningsih, Muhammad Amin and Abu Bakar
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
Keywords: Walking Exercise, Pursed Lips Breathing, COPD.
Abstract: World Health Organization (WHO) at Global Status of Non-communicable diseases in 2015 explained that
COPD is the 4th largest non-communicable disease in the world. Dyspnea, increased respiratory rate,
decreased oxygen saturation and activity intolerance are typical symptoms in COPD patients. These
symptoms correlate to pulmonary function abnormalities such as impairment of FEV1 and FEV1/FVC. The
condition of the patients will become worse if they don’t get therapy and rehabilitation. The purpose of this
systematic review was to identify research about the effect of walking exercise and pursed lips breathing to
clinical symptoms, lung function, and exercise tolerance of COPD patients. Search articles through
database: Pro quest, Scopus, Science Direct, and EBSCO published between 2007 -2017. There are sixteen
research journals. Based on the search results, found 43 journals. After being selected according to the
inclusion criteria, 16 journals have been reviewed. Eleven journals used pursed lips breathing intervention,
while 5 journals on walking exercise intervention in COPD patients. The application of walking exercise
and pursed lips breathing improved symptoms, lung function, and exercise tolerance in COPD patients. We
suggest to do further research with larger sample quantities, increase exercise frequency and the need for
further monitoring.
1 INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a
pulmonary disease that can lead to exacerbations and
progressive life-threatening (GOLD, 2017). Chronic
Obstructive Pulmonary Disease (COPD) is a chronic
lung disease that causes the limitation of air flow in
the lung causing interference with the lung function.
Decreased lung function occurs due to chronic
inflammatory changes in the proximal, peripheral
and pulmonary vascular channels. This condition
results in decreased ventilation function in the lung,
and the patient will experience an increase in
breathing frequency with expiratory length(Black
and Hawks, 2014).
World Health Organization (WHO) in Global
Status of Non-communicable Diseases 2015
explains that COPD is the fourth major non-
communicable disease in the world that has high
mortality after ischemic heart disease, stroke and
lung cancer. Globally, an estimated 3 million deaths
are caused by this disease in 2015 ie, 5% of all
deaths worldwide in that year. More than 90% of
COPD deaths occur in developing countries with a
weak economic level(WHO, 2017).
Shortness of breath and activity intolerance are
major complaints in COPD patients. The shortness
of breath in COPD patients is progressive,
irreversible, and lowers tolerance in activity. The
presence of inflammation, fibrosis, and luminal
exudate in the respiratory tract associated with
decreased FEV1 and FEV1/FVC ratios. Decreased
FEV1 is a characteristic symptom of COPD,
peripheral respiratory tract obstruction causes air
trapped and leads to hyperinflation. Hyperinflation
reduces the inspiratory capacity of functional
residual capacity, especially during exercise
(dynamic hyperinflation), seen as dyspnea and
limited exercise capacity. Hyperinflation that
develops early in the disease is the main mechanism
of the onset of dyspnea (GOLD, 2017).
Pulmonary function in patients with COPD will
get worse if the therapy and rehabilitation are not
well done. COPD patients will experience an
exacerbation and result in respiratory failure.
Patients will also experience complications of heart
function abnormalities. Therefore, it requires the
Ningsih, A., Amin, M. and Bakar, A.
The Effect of Walking Exercise and Pursed Lips Breathing on Signs and Symptoms of COPD Patients: A Systematic Review.
DOI: 10.5220/0008324002870291
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 287-291
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
287
management of therapy and treatment of complex
rehabilitation in order to improve the lung function
of COPD patients. Rehabilitation therapy for COPD
patients that can be applied to improve lung function
is to control breathing Pursed Lips Breathing (PLB).
Pursed Lips Breathing (PLB) is a ventilation
maneuver technique by pursing lips during
expiration (Spahija et al., 2010). Breathing exercises
are performed to get better breathing arrangements
from quicker and shallower breathing to slower and
deeper breathing. The purpose of this exercise is to
reduce and control shortness of breath.
Another therapy that can be done for the
rehabilitation of COPD patients is by doing light
exercise. Mild exercise gradually in COPD patients
can improve exercise tolerance, as well as decrease
dyspnea and fatigue. One form of mild exercise
recommended for activity therapy is walking
exercise. The purpose of this study was to conduct a
systematic review of walking exercise and pursed
lips breathing on clinical symptoms, lung function,
and exercise tolerance of COPD patients.
2 METHODS
In this study, the authors identified the journal
publication of research results on the use of walking
exercise and Pursed Lips Breathing in patients with
COPD. The results of this systematic review is
expected to be applied to health services, especially
nursing. This systematic review is presented in the
form of article consisting of; abstract, introduction,
method, result and discussion, conclusion, and
bibliography.
Search articles using PICOT framework
(Population: COPD patient in criteria of GOLD I, II,
III, and IV with stable condition, Intervention:
Pursed Lips Breathing and walking exercise,
Control: -, Outcome: Clinical symptoms, Pulmonary
function, and Exercise Tolerance, Time: 2007 -
2017, based on the keywords determination of
walking exercise, pursed lips breathing, and COPD.
No other restrictions were used to maximize
literature search. Database search results; Ebscho,
Science Direct, Elsevier, Sage Journals, Scopus,
ProQuest, Pub Med, limited range of 10 years 2007
to 2017 got 43 journals and after further reading, 16
International Journals were chosen to be reviewed.
The literature inclusion criteria was quantitative
research on the use of walking exercise and pursed
lips breathing on clinical symptoms, lung function,
and exercise tolerance of COPD patients with a 10
year limitation (2007-2017). Quantitative research
should meet the criteria of PICOT.The population
used was the COPD patients with the criteria of
GOLD I, II, III, and IV. The patients were stable and
were not undergoing an acute exacerbation.
Intervention used in the form of walking exercise or
pursed lips breathing. Comparison in this study
consisted of at least 1 group of intervention groups
or groups of placebo and intervention, outcomes
produced were clinical symptoms, pulmonary
function, and exercise tolerance. All studies used
English. From all journals, there were 43 journals
and after further election 16 International Journals
were chosen to be reviewed.
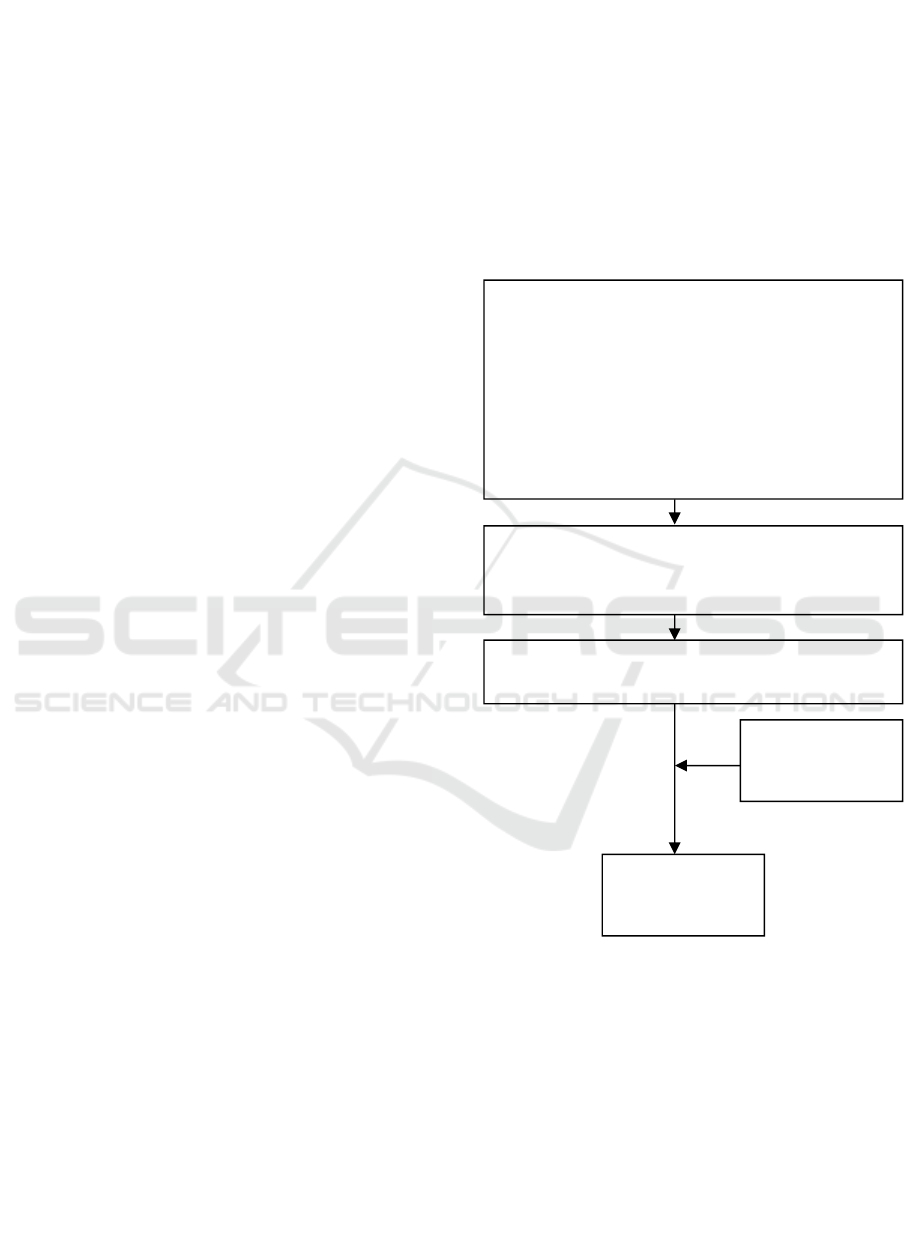
Figure 1: Searching Strategy
3 RESULTS
Based on the results review of 16 journals, the data
were collected from United Nation of America for 2
journals, Canada for 2 journals, North Korea for 1
journal, Italia for 1 journal, Brazil for 3 journals,
India for 1 journal, Netherlands for 3 journals,
Germany for 1 journal, and Sweden for 1 journal.
Total of all respondents in the literature were 539
respondents. The research design consisted of 5
Searching articles using PICOT framework
Population : COPD patients with the criteria of
GOLD I, II, III, and IV
Intervention: Walking Exercise and Pursed Lips
Breathing.
Control: -
Outcomes : Clinical symptoms, Pulmonary
function, and Exercise Tolerance
Time : 2007-2017
Search the journal through Boolean Logic in
database; Ebscho, Science direct, Elseiver, Sage
Journals, Scopus, ProQuest , Pub Med
Number of the journals found
(n = 43)
Journals that
do not fit the
criteria
Appropriate
Journal Criteria
(n = 16)
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
288

journals with Randomized control trial, 9 journals
Randomized cross over study and 2 journals cross
sectional study.
Based on 16 journals reviewed, there were 5
journals using walking exercise and 11 journals
using pursed lips breathing in patients with COPD.
Pursed Lips breathing is a breathing technique for
breathing for 2 seconds through the nose with the
mouth closed, then slowly releasing air for 4-6
seconds with a conical mouth (Bhatt et al., 2013).
Respiratory technique is done by various methods.
There were 6 journals that apply pursed lips
breathing during exercise. 6 journals applied the
PLB when the patient is rested and relaxes with
duration of 10 minutes. 1 journal applied PLB at the
time of recovery after light exercise. 1 journal
applied PLB with a combination of mouth taping,
and 1 journal applied PLB in 3 different positions
i.e. PLB applied with neutral sitting position, arm
support position, or arm and head support position.
From the results of those journals’ review,
walking exercise was applied with several methods.
Research conducted by Gagnon, P., et al, applied
walking exercises by performing a warm-up phase
for 90 seconds, followed by a casual walking
exercise in open areas and flat floors. The walk was
10 meters (Gagnon et al., 2012).
Research conducted by Roos, P., et al. applied
exercise training and home base walking program
for 10 weeks. Exercise training was carried out by
applying treadmill and cycling program for 10
minutes and the patient was educated to apply home
based walking exercise at least 30 minutes per
session, at least once a week, and exercise time was
added 5 minutes per week(de Roos et al., 2017).
Research conducted by Dreher, M., et al.,
applied 6 MWT and Stair-climbing in the hospital
area (Dreher et al., 2008). This is similar to a study
conducted by Vaes, Anouk., Et al., which
implemented 6 MWT by comparing walking with a
collator and modern drainage(Vaes et al., 2012).
Research conducted by Leung, Regina W. M. et al.,
applied walking exercise at the hospital for 8 weeks.
The exercise performed 3 times per week with
exercise duration of 30 to 45 minutes per session
(Leung et al., 2010).
The clinical symptoms analyzed by this
systematic review consisted of dyspnea, respiratory
rate (RR), and oxygen saturation (SaO2). RR
measurements were done manually, whereas to
assess oxygen saturation using pulse ox-meter.
Measurement of dyspnea was by using instrument in
the form of questionnaire. There were 2 journals that
assessed dyspnea with Visual Analog Scale (VAS),
3 journals with mMRC Dyspnea Scale, 6 Journals
with Borg Scale dyspnea, 1 journal with BDI Scale,
and 1 journal with Chronic Respiratory Disease
Questionnaire Dyspne Scale. Pulmonary function in
the results of the study was measured using a
spirometer.
There were several measurements to measure the
exercise tolerance of COPD patients i.e. 2 journals
using 6 MWD test, 2 journals with Endurance
Shuttle Walking Test, 1 journal with 6 MWT test, 1
journal with walking test treadmill, 1 journal with
physical function scale, 1 journal with ISWT , 1
journal with ESWT and 1 journal with Personal
Activity Monitor (PAM).
The results of the journal analysis showed that
walking exercise and pursed lips breathing provide a
positive impact on the improvement of clinical
symptoms, lung function and exercise tolerance.
There were 6 journals for the improvement on
shortness of breath symptom, 6 journals decreased
RR, and 5 journals for increased oxygen saturation.
In addition, the improvement of lung function was
looked significant.
There were 2 journals of FEV1 grade upgrades, 2
FVC value improvement journals, 2 PEFR score
improvement journals, 1 FEV1 / FVC grade
improvement journal and 2 TV value refining
journals. Interval walking exercise and pursed lips
breathing significantly had a positive impact on
exercise tolerance; as many as 9 journals have
improved exercise tolerance in the respondents.
4 DISCUSSION
This systematic review identified one of breathing
techniques that was pursed lips breathing (PLB) and
light exercise that was walking exercise applied to
COPD patients. Identification was aimed at
reviewing the benefits of applying pursed lips
breathing and walking exercise to clinical
symptoms, lung function and exercise tolerance.
Based on the study of 16 journals, it was known that
there were 12 journals which reviewed the benefits
of pursed lips breathing and walking exercise on the
change of clinical signs and symptoms of COPD
patients. There were improvements in oxygen
saturation, respiratory rate and dyspnea scale of
COPD patients.
Study conducted by Bhatt, et al., found that after
applying Pursed Lips breathing, patients would
experience increased exercise capacity. Patients
revealed decreased dyspnea, and RR frequency.
Respiratory control during the pursed lips breathing
period caused decreased vicious cycle interrupts in
air trapping. This occurred because of lower central
nervous transmission, and leaded to a lower
dissociation between actual ventilator signals and
The Effect of Walking Exercise and Pursed Lips Breathing on Signs and Symptoms of COPD Patients: A Systematic Review
289

perceived effort, resulting in lower perceived
dyspnea perception (Bhatt et al., 2013).
Based on research conducted by Leung et al., it
was known that the grand walk training could reduce
dyspnea and Respiration Rate (RR). In addition, this
exercise could reduce the production of carbon
dioxide, and increased minute ventilation when
compared to basic data. Reduction of carbon dioxide
and minute ventilation could increase the oxidative
capacity of trained muscles with walking exercise,
thereby reducing dyspnea (Leung et al., 2010).
Based on the results of 16 journals review, it was
known that there were 4 journals of research which
proved that pursed lips breathing and walking
exercise gave advantage towards lung function
improvements, namely FEV1 (%), FVC, PEFR and
FEV1 / FVC. This breathing technique used a
second pursing strategy lips together during exhale.
Thus, the airways became exposed, with respiratory
pressure back and air emptying process when
expiration became better (Maind et al., 2015).
In a study conducted by Bhatt, et al, found that
the breath-control technique with pursed lips
breathing increased 20% FEV1 and FVC, and
reduced water trapping. Reduction of hyperinflation
was due to an increase in expiratory volume
resulting in an increase in tidal volume. Decreased
respiratory frequency also occurred due to
adjustment of time perfusion and ventilation (VA /
Q). In addition, by doing Walking exercise, it could
improve the efficiency and capacity of the oxygen
transport system, increased VO2 max, improved
aerobic and anaerobic work capacity, increased
cardiac output and stroke volume, increased blood
distribution efficiency and shortened recovery time
(Bhatt et al., 2013).
Based on the results of 16 journals review, it was
known that there were 9 journals of research which
proved that pursed lips breathing and walking
exercise gave advantage against improvement of
exercise tolerance in COPD patients. Physical
exercise in people with COPD resulted in increased
exercise tolerance due to increased maximum work
capacity with low oxygen consumption. Improved
exercise tolerance was an indication of the efficient
use of oxygen in the tissues and tolerance of lactic
acid. Based on research conducted by de Roos, et al,
it was known that the combination of exercise
training and home based walking program could
improve Physical activity (PA). Patients who had an
increased level of exercise tolerance, then the use of
peripheral oxygen could be efficient (de Roos et al.,
2017).
Walking exercise and pursed lips breathing
performed regularly can improve clinical signs and
symptoms, lung function and physical activity of
COPD patients. This is because by doing this
exercise, the patient is able to increase expiratory
strength characterized by increased FEV1, as well as
tidal volume improvement. So that the perfusion of
ventilation to the maximum and the activity
tolerance for the better.
5 CONCLUSIONS
Systematic review on Evaluation for the Effect of
Walking Exercise and Pursed Lips Breathing on
Clinical Symptoms, Lung Function and Exercise
Tolerance of COPD Patients found that the
application of pursed lips breathing and walking
exercise techniques could provide positive
improvement in COPD patients. This was certainly
very effective if applied to COPD patients, since
lung damage was not completely reversible, so it
was important to keep patients in stable condition
and prevent exacerbations.
The nursing implication of this systematic review
was improving the health of COPD patients.
Walking exercise and Pursed lips breathing could be
applied in nursing care in patients with COPD. This
could be included in the nursing care plan by
conducting health education to the patient, that was
about how to do walking exercise and pursed lips
breathing and its benefits to COPD patients. Nurses
could evaluate the successful implementation of
walking exercise and pursed lips breathing and its
clinical effects.
The lack of this systematic review is on the
criteria of research journals, ie not having uniformity
in terms of research methods. The journal in this
study revealed that the research method did not
always use the control group as a comparison.
REFERENCES
Bhatt, S. P. et al. (2013) ‘Volitional pursed lips breathing
in patients with stable chronic obstructive pulmonary
disease improves exercise capacity’, Chronic
Respiratory Disease, 10(1), pp. 5–10. doi:
10.1177/1479972312464244.
Bianchi, R. et al. (2007) ‘Patterns of chest wall kinematics
during volitional pursed-lip breathing in COPD at
rest’, Respiratory Medicine, 101(7), pp. 1412–1418.
doi: 10.1016/j.rmed.2007.01.021.
Black, J. M. and Hawks, J. H. (2014) Keperawatan
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
290

Medikal Bedah: Manajemen klinis untuk hasil yang
diharapkan. Edisi 8. jakarta: PT Salemba Emban
Patria.
Cabral, F. et al. (2015) ‘IN C ER IG E ® A’, 51(1), pp.
79–88.
Dreher, M. et al. (2008) ‘Exercise in severe COPD: Is
walking different from stair-climbing?’, Respiratory
Medicine, 102(6), pp. 912–918. doi:
10.1016/j.rmed.2008.01.002.
Gagnon, P. et al. (2012) ‘Walking exercise response to
bronchodilation in mild COPD: A randomized trial’,
Respiratory Medicine, 106(12), pp. 1695–1705. doi:
10.1016/j.rmed.2012.08.021.
GOLD (2017) Global Initiative for Chronic Obstructive
Lung Disease. Available at: goldcopd.org (Accessed:
1 January 2017).
Institutet, K. et al. (2008) ‘Influence of spontaneous
pursed lips breathing on walking endurance and
oxygen saturation in patients with moderate to severe
chronic obstructive pulmonary disease’, pp. 675–683.
Kim, K. et al. (2012) ‘Effects of breathing maneuver and
sitting posture on muscle activity in inspiratory
accessory muscles in patients with chronic obstructive
pulmonary disease’, pp. 1–6.
Leung, R. W. M. et al. (2010) ‘Ground walk training
improves functional exercise capacity more than cycle
training in people with chronic obstructive pulmonary
disease (COPD): A randomised trial’, Journal of
Physiotherapy. Elsevier, 56(2), pp. 105–112. doi:
10.1016/S1836-9553(10)70040-0
Maind, G. et al. (2015) ‘Comparison Between Effect Of
Pursed Lip Breathing And Mouth Taping On
Dyspnoea: A Cross Sectional Study’, Int J Cur Res
Rev, 7(16), pp. 17–21.
Margare et al. (2007) ‘Efficacy Of Pursed-Lips Breathing
A Breathing Pattern Retraining Strategy For Dyspnea
Reduction’, Journal of Cardiopulmonary
Rehabilitation and Prevention, 27, pp. 237–244.
Pereira De Araujo, C. L. et al. (2015) ‘Pursed-lips
breathing reduces dynamic hyperinflation induced by
activities of daily living test in patients with chronic
obstructive pulmonary disease: A randomized
crossover study’, Journal of Rehabilitation Medicine,
47(10), pp. 957–962. doi: 10.2340/16501977-2008.
Ramos, E. M. C. et al. (2009) ‘Influence of pursed-lip
breathing on heart rate variability and
cardiorespiratory parameters in subjects with chronic
obstructive pulmonary disease (COPD)’, Revista
Brasileira de Fisioterapia, 13(4), pp. 288–293. doi:
10.1590/S1413-35552009005000035.
de Roos, P. et al. (2017) ‘Effectiveness of a combined
exercise training and home-based walking programme
on physical activity compared with standard medical
care in moderate COPD: A randomised controlled
trial’, Physiotherapy (United Kingdom). The Chartered
Society of Physiotherapy, pp. 6–11. doi:
10.1016/j.physio.2016.08.005.
Spahija, J. et al.
(2010) ‘Factors discriminating
spontaneous pursed-lips breathing use in patients with
COPD.’, Copd, 7(4), pp. 254–261. doi:
10.3109/15412555.2010.496820.
Vaes, A. W. et al. (2012) ‘The effects of a “new” walking
aid on exercise performance in patients with COPD: A
randomized crossover trial’, Chest. The American
College of Chest Physicians, 141(5), pp. 1224–1232.
doi: 10.1378/chest.11-1076.
Visser, F. J. et al. (2011) ‘Pursed-lips breathing improves
inspiratory capacity in chronic obstructive pulmonary
disease’, Respiration, 81(5), pp. 372–378. doi:
10.1159/000319036.
WHO (2017) Chronic obstructive pulmonary disease
(COPD), WHO. Available at: http://www.who.int
(Accessed: 3 September 2017).
The Effect of Walking Exercise and Pursed Lips Breathing on Signs and Symptoms of COPD Patients: A Systematic Review
291
