
Threatening Factor Exposure Triggers Recurrence of Asthma in
Children
Sandi Alfa Wiga Arsa
1
, Tintin Sukartini
1
and Sri Utami
2
1
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
2
Politeknik Kesehatan Kementrian Kesehatan,Surabaya, Indonesia
Keywords: Childhood Asthma, Relapse, Trigger Factor.
Abstract: Asthma is an important health problem because of the high recurrence rate in children, if not handled
properly, asthma can reduce the quality of life of children, interfere with growth, limit daily activities,
interfere with sleep, increase school attendance, and lead to academic achievement in school decreased. The
threat of trigger factors for recurrence is overwhelming and varies in every child. Usually, there are one or
more factors of some dominant factors, so that efforts to educate health better focus on the factors that
threaten the recurrence. This study aims to identify the factors of the threat of exposure to asthma triggers in
children. The design of this research is analytical descriptive with the cross-sectional design. The number of
respondents was 53 children with asthma. Bivariate analysis showed that the trigger factors associated with
the occurrence of recurrence of asthma were allergen exposure (p = 0.177), physical activity (p = 0.69),
foods (0.036) and weather (0.192). The result of the multivariate analysis showed the strength of the
strongest relationship until weakest relapse of asthma in children was the activity (OR = 0,241) and allergen
(OR = 0,05). It is expected that management of asthma through education in children or parents can be more
focused on avoiding the threat factors of exposure trigger recurrence.
1 BACKGROUND
Asthma in children continues to be one of the most
common chronic diseases in childhood. This is a
common disease in children). Most asthma-related
deaths occur in low- and middle-income countries
(WHO, 2017). Although not occupying the top spot
as a cause of morbidity or mortality in children, if
not handled properly, asthma can reduce the quality
of life of children, interfere with growth, limit daily
activities, interfere with sleep, increase school
attendance, and lead to academic achievement in
school decreased (National Heart Lung and Blood
Institute, 2007). The results of the survey using the
International Study on Asthma and Allergy in
Childhood (ISAAC, 2013) have been conducted in
155 centers of asthma in 56 countries, one of which
is Indonesia aimed at the age group of 6-7 years and
13-14 shows the results varies in some countries
with asthma prevalence between 2.1 - 32.2% (IDAI,
2016). Asthma is an important health problem
because of the high recurrence rate in children, in
2013, 3.4 million (school-aged children) SAC
experienced asthma exacerbations, SAC with asthma
and exacerbations had 18.9 times more visits to
emergency departments (Sullivan et al., 2017). The
threats to the occurrence of recurrence are exercise,
exposure to allergens or irritants, weather changes,
or viral respiratory infections (Page et al., 2017).
The exact mechanisms for the cause of asthma are
not known exactly but there are several factors that
trigger an asthma attack. The term trigger factor or
current precipitating factor is more commonly used
which includes allergens, exercise, air pollution,
occupational factors, respiratory infections, nasal
and sinus problems, sensitive to drugs and food,
gastroesophageal reflux disease (Gastroesophageal
Reflux Disease / GERD) and psychological factors
(emotional stress) (Lewis, Bucher, Heitkemper, &
Dirksen, 2013). Asthma control in children is very
difficult to achieve because children are still
dependent on their parents or caregivers to make
decisions about their health (Conn, Halterman,
Lynch, & Cabana, 2007). Recurrence of asthma in
children often occurs due to the threat of trigger
recurrence has not been identified by nurses, health
workers or parents. Parents are aware of the
symptoms of asthma that worsen, they are not
302
Arsa, S., Sukartini, T. and Utami, S.
Threatening Factor Exposure Triggers Recurrence of Asthma in Children.
DOI: 10.5220/0008324303020308
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 302-308
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

always clear what triggers relapse (Searle, Jago,
Henderson, & Turner, 2017). The threat of trigger
factors for recurrence is overwhelming and varies in
every child, usually, there are one or more factors of
some dominant factors, so that efforts to educate
health better focus on the factors that threaten the
recurrence. It is, therefore, the purpose of this study
to explore the threat factors of the trigger for
childhood asthma relapse.
2 METHODS
2.1 Participants
Children aged 6 - 11 with diagnoses of asthma by
doctors at Pediatric Department in Mardi Waluyo
Hospital Blitar, Indonesia. Children who come to a
child health center, with parents between January
and February 2018 to complete the contents of the
questionnaire provided by the researcher. Questions
in the questionnaire involve parents and children in
filling in. The inclusion criteria in this study were 1)
parents with asthma children aged 6-11 years 2)
parents who can communicate orally and written
well 3) parents with children with asthma without
any other illness that aggravate the condition of
children such as tuberculosis, sepsis, typhoid fever,
bronchitis, and pneumonia. The exclusion criteria in
this study were 1) the child suffered the severe
attack and the threat of stop breathing 2) the elderly
with hearing, psychiatric disorder. Determination of
sample size in this study using software G Power
(Buchner, 2010) with the statistical test: Logistic
regression. Using 1% error rate and 95% power.
Determination of the value with the lowest and
highest value p value refers to the previous research
(Brigham, Goldenberg, Stolfi, Mueller, & Forbis,
2016) p the lowest value of 0.675 and the highest of
0.001 to obtain the number of samples of 53
participants. Sampling in this research is done by
probability sampling method through simple random
sampling.
2.2 Measurement
Measurement of recurrence of asthma using
questions addressed to parents in the questionnaire
Childhood Asthma Control Test for children 4 to 11
years (asthma.com, 2017) and open-ended questions
about specific symptoms of childhood asthma
relapse in the last 2 weeks such as: cough especially
at night or early morning, shortness of breath,
difficulty of sputum, breath sounds (wheeze) that
sounds if the child exhales, the weight on the chest
(National Heart Lung and Blood Institute, 2007).
Through the assessment found that asthma children
in the last 2 weeks relapse or not relapse.
Measurements for the threat factor variables of
asthma relapse were adapted from (Lewis et al.,
2013) compiled into questionnaires used by (Putu,
2012), which were then modified according to the
needs of this study. The threat factors for relapse are
as follows: 1) allergens 2) physical activity 3) air
and environmental pollution 4) respiratory infections
5) drug and food sensitivity 6) psychological
condition 7) emotional stress condition 8) air
condition/weather, with each -the threat factor of the
relapse trigger is categorized by x > median
(exposed), x < median (not exposed).
2.3 Statistical Analysis
2.3.1 Univariate
Univariate analysis was conducted to describe the
characteristics of each of the variables studied.
Univariate analyzes for categorical data such as
recurrence, child sex, long-suffering from asthma,
and trigger threat factors are presented in the form of
frequency distribution using percentages or
proportions. In numerical data such as the child's age
is described as the mean, median, maximum-
maximum and standard deviations. All data were
analyzed at the 95% significance level (α = 0,05).
2.3.2 Bivariate
Bivariate analysis to analyze the relationship of the
categoric variable with categoric variable was done
by using chi-square statistic test. The chi-square
statistical test aims to examine the difference in
proportion. If the bivariate test results have p <0.25
then the variable can be entered in the multivariate
model. However, if p value> 0.25 then still put into
multivariate if the variable is substantially important.
2.3.3 Multivariate
Multivariate analysis in this study to perform
multivariate analysis, used multiple logistic
regression analysis because it has the categorical
dependent variable. The important variables
included in the multivariate model are those with p-
value <0.05. The variables affect the dependent
variable is known from the value of each p-value.
The relationship strength sequence of the variables
affects the dependent variable. In the logistic
Threatening Factor Exposure Triggers Recurrence of Asthma in Children
303
regression, the order of strength of the relationship is
known from the value of the Odd Ratio (OR).
3 RESULTS
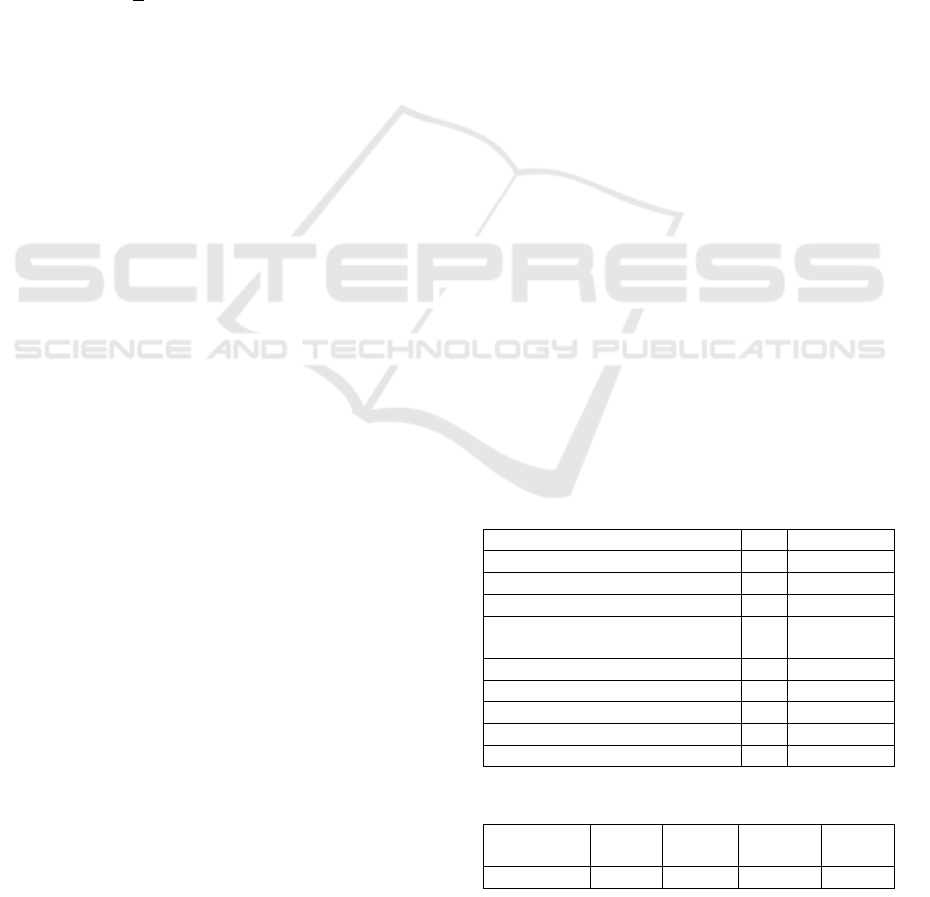
Table 1 shows the number of respondents obtained
is 53 children with diagnosis of asthma, the majority
of them, male gender as much as 31 respondents
(58.5%), as many of 35 respondents (66%) have
suffered from asthma for more than 2 years and the
majority of children experienced a recurrence in the
last 2 weeks by 34 respondents (64.2%)
Table 2 Discussion of the respondents in this
study was 8.25 + 1.592 years with the age range of
6-11 years.
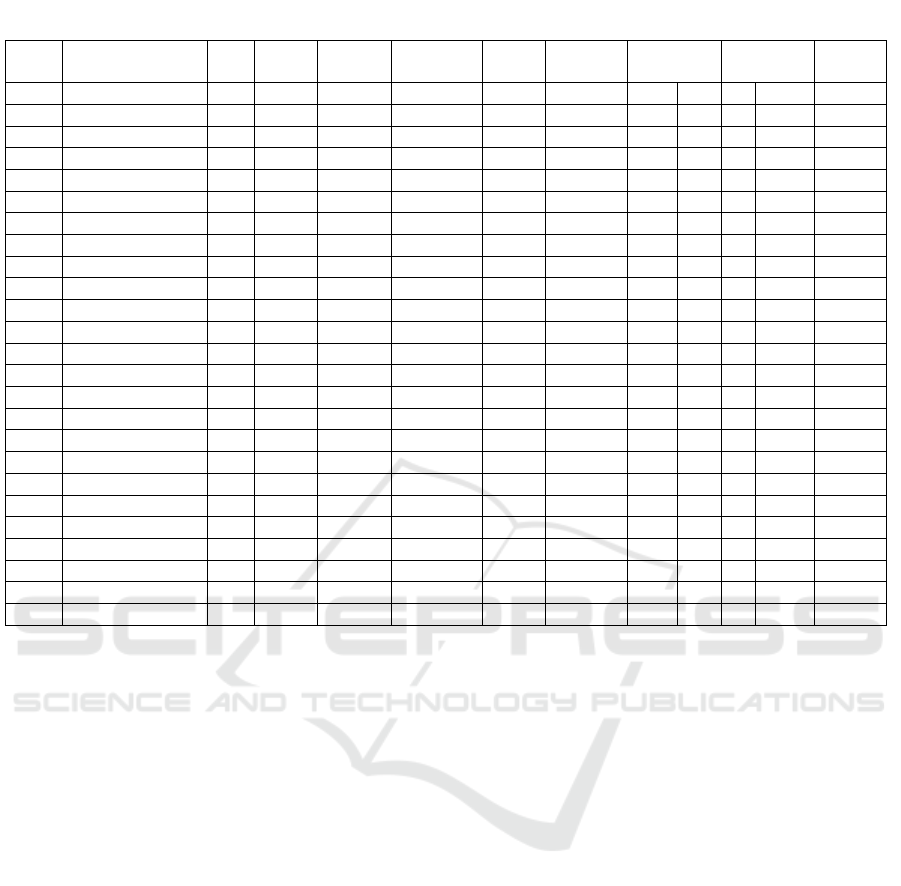
Table 3 presents the distribution of respondents
based on the exposure of the threatening factors of
relapse, of all the factors of the majority of
respondents exposed to these threat factors, allergen
38 respondents (71.7%), severe physical activity 27
respondents (50.9%), air pollution around the
environment 32 respondents (60.4 %), respiratory
infection 27 respondents (50.9%), food 31
respondents (58.5%), psychological 48 respondents
(90.6%), emotional stress 30 respondents (56.6%),
weather 30 respondents (56.6%). This table also
shows of bivariate selection, not all variables show
p-value <0.25 as a requirement to enter into
multivariate test. Variables that will be included into
the logistic regression analysis is a variable that in
bivariate analysis has a value of p <0.25. The
variables were allergen (p = 0.177), activity (p =
0.069), foods (p = 0.036), and weather (p = 0.192).
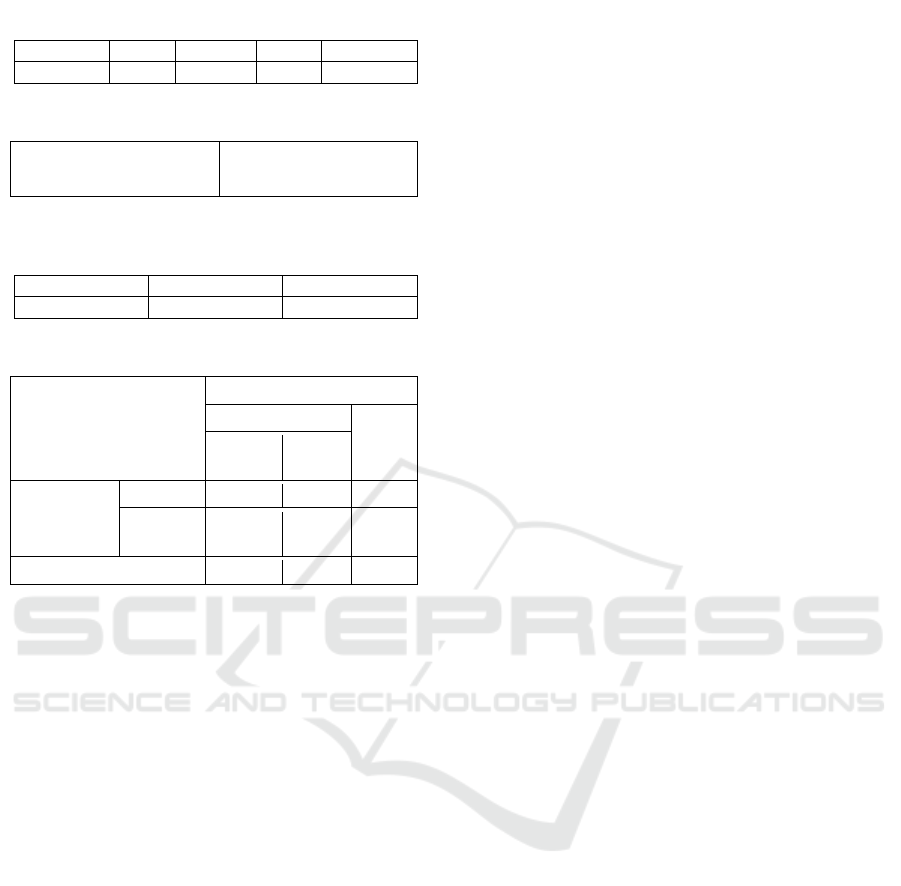
Table 4 above gives value Nagelkerke R square of
0.474 which means that contribution of four variable
that is allergens, activities, eating, and weatherable
explain accuracy by 47% and 34% others explained
by other factors.
Table 5 shows the chi-square test of Hosmer and
Lemeshow test with p-value of significance of 0.775
(p > 0.05), then H0 is accepted that the model has
sufficient to explain the data (goodness of fit)
Table 6 shows that accuracy prediction in this
reasearch is 77.4 %
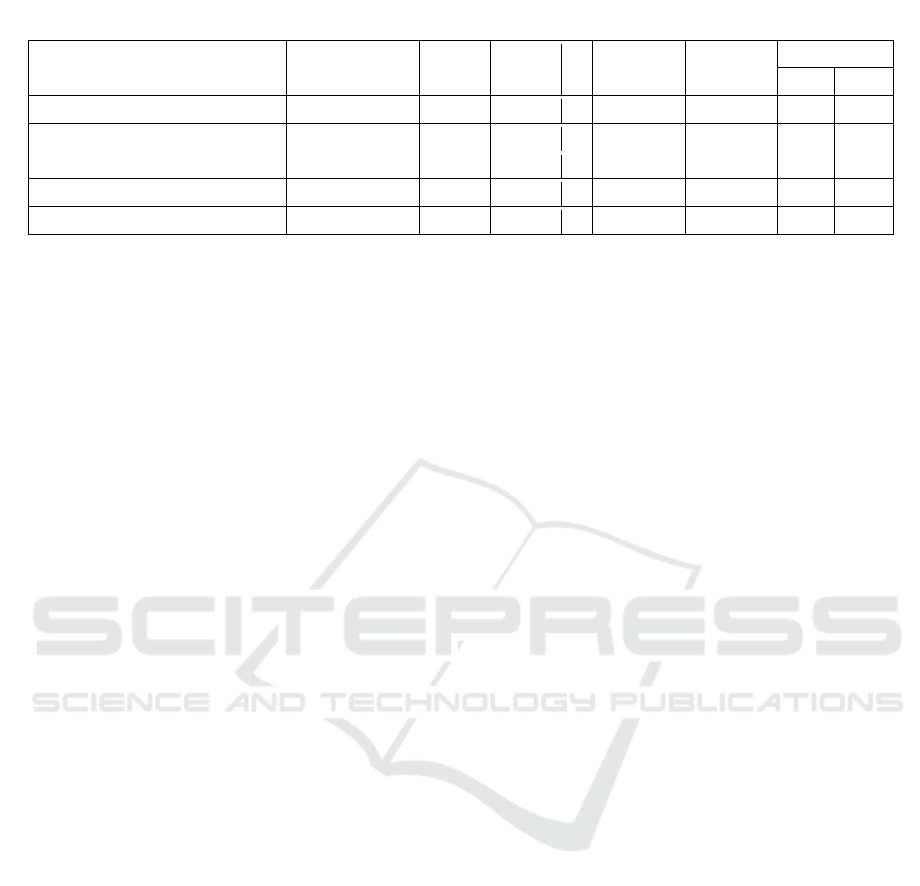
Table 8 shows the results of variables that affect
the recurrence of asthma in children are allergens,
physical activity, food and weather. The strength of
the relationship can be seen from the value of OR
(EXP (B)). The strength of the largest and smallest
relation is activity (OR = 0,241) and allergen (OR =
0,057). Testing on alone evidently allergen (p =
0.018), food (p = 0.008), weather (p = 0.026) has a
significance value <0.05 while activity (p = 0.056)
has sig value > 0,05 me aning on alone allergens,
food, and weather have a significant influence
to relaps, and activities have no effect on recurrence
but in a manner at the same time all four variables
have an effect on recurrence with a value of p =
0.007. Thus, it can be we conclude that the equation
obtained is : g(x) = (constant = 6.130) + (-2.856
(allergen)) + (-1.421 (activity)) + (-2.006 (food)) + (-
2.914 (weather)). Value of free variable: 1 if
exposed and 0 if not exposed
4 DISCUSSION
This study shows that the majority of children with
58.5% of asthma have an average age of 6-11, an
average score of 8.25 years, 66% of children have
had asthma for more than 2 years, and 64% of them
have relapsed in the last 2 weeks. From the results of
the survey conducted (Zahran, Bailey, Damon,
Garbe, & Breysse, 2018) in the United States, the
number of boys is 51% more than women with 5-11
age range of 39%, this indicates that at this age
group is a condition where children are more
frequently exposed to the risk factors for recurrence.
There were 8 recurrence threat factors which were
assessed in this study. The majority of respondents
received the exposure, namely: allergen (71%),
physical activity (50.9%), pollution (60%),
respiratory infections (50.9%), food (58%) ,
psychological (90%), emotion (56%), and weather
(56.6%). Only 4 factors had a requirement to pass a
multivariate assay suspected to be associated with
recurrence experienced by a child with asthma (see
Table 4). This shows that asthma is a unique chronic
respiratory disease, not all children have the same
Table 1: Respondent demographic.
Variables
N
%
Gender
Man
31
58.5
Women
22
41.5
Long-time suffering from
asthma
> 2 years
35
66
<2 years
18
34
Recurrence in the last 2 weeks
Relapse
34
64.2
No relapse
19
35.8
Table 2: Distribution of respondents by age.
Variables
Mean
Median
SD
Min-
Max
Age
8.25
8
1.592
6-11
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
304
triggering factor of recurrence, asthma in children
becomes a very interesting material to do research to
get the best formulation for each place in providing
preventive measures in lowering the number
recurrence in children. It is explained in Table 5 that
the four variables are able to explain the accuracy of
47% and the other 34% explained by other factors.
Table 7 shows that the prediction accuracy in this
study is 77.4%. the strength of the relationship of
each variable can be seen through indigo Odd Ratio
(OR), which sequentially from the strongest
relationship to the weakest is the activity (OR =
0241), allergen (OR = 0.057), food (OR = 0.050),
weather (OR- 0.004) Here's a discussion on 4 factors
that are suspected to have an effect on recurrence in
this study.
4.1 The Association of Allergen with
Recurrence of Asthma in Children
The result of univariate analysis showed that the
average of allergen exposure was 7.34 with a
minimum value of 4-10. Exposure to allergens in
this study includes exposure to allergens indoors or
outdoors consisting of mites, room dust, outdoor
dust, foul odour and animal dander. The result of
bivariate analysis showed that allergen variable was
eligible for multivariate test with p = 0.177 (p
<0.25). In multivariate test alone allergen variables
have significant effect on recurrence with value p =
0.018 where p <0.05. The results of this study are in
line with several research results that have been
done with different environmental conditions. It has
been 50 years since dust mites were first appreciated
to be the main source of allergens in house dust, and
by extension into the main trigger of respiratory
illness due to allergies. Dust mites are a major
contributor to asthma in many parts of the world and
well-defined first-line allergens that cannot be
visually identified (Wilson & Platts-Mills, 2018).
The most predictive triggers of asthma exacerbations
are dust allergens predicted as a trigger for asthma
relapse in children (OR, 1.65, 95% CI, 1.13-2.43, P
= 0.01) (Chipps et al., 2018). This proves that
allergens should be avoided in order not to recur
asthma in children. Efforts to avoid allergens by
modifying the home environment are important in
the effort to reduce the rate of childhood asthma
relapse, some avoiding dust mites can be explained
in the review done by commonly also described in
(IDAI, 2016).
Table 3: Distribution of respondents based on exposure to threatening triggering factors of recurrence.
No.
Variables
N
%
Mean
Median
SD
Min-
Max
Relapse
No relapse
p-value
N
%
n
%
1.
Allergens
7.34
7
1.4
4-10
0.177 *)
Exposed
38
71.7
27
71.1
11
28.9
Not exposed
15
28.3
7
46.7
19
53.3
2.
Activity
6.72
7
1.53
4-10
0.069*)
Exposed
27
50.9
21
77.8
6
22.2
Not exposed
26
49.1
13
50
13
50
3.
Pollution
7.11
7
1.20
5-9
0.987
Exposed
32
60.4
20
62.5
12
37.5
Not exposed
21
39.6
14
66.7
7
33.3
4.
Infection
9.55
10
2.53
3-13
0.918
Exposed
27
50.9
18
66.7
9
33.3
Not exposed
26
49.1
16
61.5
10
38.5
5.
Food
14.47
15
2.75
8-19
0.036*)
Exposed
31
58.5
24
77.4
7
22.6
Not exposed
22
41.5
10
45
12
54.5
6.
Psychological
2.47
2
0.85
1-4
0.774
Exposed
48
90.6
30
62.5
18
37.5
Not exposed
5
9.4
4
80
1
20
7.
Stress
4.74
5
1.13
3-7
0.468
Exposed
30
56.6
21
70
9
30
Not exposed
23
43.4
13
56.5
10
43.5
8.
Weather
2.19
2
0.83
1-4
0.192*)
Exposed
30
56.6
31
68.9
14
31.1
Not exposed
23
43.4
3
37.5
5
62.5
Threatening Factor Exposure Triggers Recurrence of Asthma in Children
305
4.2 The Association of Food and Drug
with Recurrence of Asthma in
Children
The result of the univariate analysis shows that the
average of exposure is 14.47 with minimum-
maximum value 8-19. The food in this study was
food exposure containing preservatives, dyes and
flavoring, consumption of animal protein, vegetable,
while medicines were the consumption of febrifuge,
antibiotics, prescription drugs, and drugs that may
have been consumed in the last 2 weeks. The result
of the bivariate analysis showed that the variable of
food was eligible for the multivariate test with p =
0.036 (p <0.25). In multivariate test alone food
variables have a significant effect on recurrence with
value p = 0.008 where p <0.05. Study of the results
of the III Phase III Asthma and Allergies in
Childhood (ISAAC) questionnaire, with more
specifically collected data on the association of risk
of asthma incidence with the diet consumed.
Vegetable intake is negatively associated with the
risk of symptoms in children 6-7, but this association
is attenuated in the 13-14 age group. Fastfood /
burger intake is positively associated with all three
results in older children. Higher intake of fruits and
vegetables is associated with a lower prevalence of
allergy symptoms in Latin American children. In
contrast, fast-food intake was positively associated
with the prevalence of wheeze in adolescent age
(Cepeda et al., 2017). Research conducted by
(Singh, Jindal, & Goyal, 2017) for children with
asthma showed that family history of asthma,
passive smoking, and food allergies were
significantly associated with asthma, food allergies
had a value of p <0.001 OR 3.03 (95% CI: 2.25-4.0).
In this study, the factors of consumption of drugs
and foods became the trigger factor for recurrence,
but most of the children cannot keep the diet
continuously, because in the age group 6-11 years is
the age of school where food and snacks in school
become a factor making them unable to adhere to the
diet. Food factors need to be wary of factors causing
recurrence in children with asthma. The choice of
schools that tighten food consumption contains
preservatives, dyes, and flavoring as an option for
the avoidance of this factor.
4.3 The Association of Weather with
Recurrence of Asthma in Children
The univariate analysis result shows that the average
of exposure is 2.19 with minimum-maximum value
1- 4. The weather in this study is exposure to high
and hot weather conditions experienced by children
during the last 2 weeks. The result of bivariate
analysis showed that the weather variable was
eligible for multivariate test with p = 0,192 (p
<0.25). In the multivariate test by itself the weather
variable had a significant effect on recurrence with
the value p = 0.026 where p <0.05. Generally asthma
attacks are caused by cold air (59.2%)
(Dharmayanti, Hapsari, & Azhar, 2013). Studies
conducted by (Hyrkäs, Ikäheimo, Jaakkola, &
Jaakkola, 2016) found that patients with less
controlled asthma were more susceptible to cold-
breathing respiratory symptoms and even worsened
asthma control increased the prevalence of
symptoms. In this study recurrence often occurs in
cold air conditions, this study was conducted in
Blitar City, East Java Indonesia, at the time of the
study, the weather in the study location was in cold
and rain conditions during January to February, the
majority of respondents complained of shortness of
breath when approaching night until late afternoon.
This is in accordance with the theory that the
assumption that asthma is defined as a condition
when there is a disturbance in the respiratory system
that causes patients experiencing wheezing,
shortness of breath, coughing, and tightness in the
chest, especially during the night or early morning
Table 4: Distribution of respondents by age.
Variables
Mean
Median
SD
Min-Max
Age
8.25
8
1.592
6-11
Table 5: Negelkerke R square value.
Cox & Snell R Square
Nagelkerke R Square
0.345
0.474
Table 6: The chi-square value of the Hosmer
and Lemeshow Test.
Chi-square
Df
Sig.
3.261
6
0.775
Table 7: The predicted accuracy of the study.
Observed
Predicted
Recurrence
%
Correct
Relapse
No
Relapse
Recurrence
Relapse
27
7
79.4
No Relaps
e
5
14
73.7
Overall Percentage
77.4
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
306
(National Heart Lung and Blood Institute, 2007).
Efforts that can be done is to adjust the self-
protection against weather changes such as the use
of hats, masks, jackets or scarves when needed.
4.4 The Association of Activity with
Recurrence of Asthma in Children
The result of the univariate analysis shows that the
average of exposure is 6.72 with a minimum value
of 4-10. Activities in this study consist of cycling,
swimming, running, climbing stairs, walking fast.
The result of the bivariate analysis showed that the
activity variable was eligible for the multivariate test
with p = 0.069 (p <0.25). In the multivariate test
alone the activity variable had no significant effect
on recurrence with p-value = 0.056 where p> 0.05.
In previous studies found no association between
physical activity, asthma control levels, spirometric
measurements and quality of life (Lim, Ko, Benton,
Berge, & Mak, 2017). But in fact, there are several
studies that mention that physical activity causes the
occurrence of recurrence of asthma in children.
Exercise can trigger acute exacerbations in almost
all individuals with asthma. Heat loss, water loss,
postexertional rewarming, and the role of some
mediators have been proposed as a possible
mechanism responsible for airway obstruction
caused by exercise (Hughes, 2014). Physical training
should be part of the overall management plan for
people with asthma. In this study, physical activity
of swimming, sport, cycling, and running was most
commonly found in asthmatic children, but only a
few children had a recurrence after physical activity.
Recurrence after an activity is suspected to have 3
other factors that also affect in this study, possibly
when doing activities outside the room also exposed
to large, eat or even weather. The goal of asthma
treatment alone is to get a controlled condition, with
a minimum of recurrence rates during physical
activity. When treated correctly, individuals with
asthma should be able to participate in sports
gradually.
5 CONCLUSIONS
The threat factors of trigger recurrence of asthma in
children vary with each other, in this study obtained
4 threat factors that trigger the recurrence of children
with asthma in the Pediatric Department, Mardi
Waluyo Hospital. Sequentially from the strength of
the relationship are activity, allergen, food, weather.
From this research can be known the recurrence
characteristics of children with asthma triggered by
these 4 factors. Avoidance of these trigger factors
will have many benefits. Activity can be controlled,
quality of sleep gradually improving, children can
attend school and can achieve. Benefits that parents
get, is not the amount of time consumed to manage
the recurrence of asthma in children, the costs
incurred for treatment becomes more effective.
Therefore, nursing intervention in the form of
education, home visit, in children or parents can be
focused on these 4 factors. The hope of further
research at the same place is to provide education
formulated from this study. Will be more effective
and efficient in providing education.
REFERENCES
Asthma.com. (2017). Childhood Asthma Control Test for
children 4 to 11 years, (January), 816205. Retrieved
from
http://www.asthma.com/content/dam/NA_Pharma/Co
untry/US/Unbranded/Consumer/Common/Images/MP
Y/documents/816205R0_childhoodasthmacontrolcest_
printable.pdf
Brigham, E. L., Goldenberg, L., Stolfi, A., Mueller, G. A.,
& Forbis, S. G. (2016). Associations between Parental
Health Literacy, Use of Asthma Management Plans,
and Child’s Asthma Control. Clinical Pediatrics,
55(2), 111–117.
https://doi.org/10.1177/0009922815587089
Buchner, P. D. A. (2010). Universität Düsseldorf:
G*Power. Retrieved December 14, 2017, from
http://www.gpower.hhu.de/en.html
Cepeda, A. M., Thawer, S., Boyle, R. J., Villalba, S.,
Table 8: Variables associated with recurrence of asthma in children.
Variables
Coefficient
SE
Wald
df
P-value
OR
95% IK
Min
Max
Exposed to allergen
-2.856
1.208
5.586
1
.018
.057
.005
.614
Exposure to activity
-1.421
.744
3.651
1
.056
.241
.056
1,037
Exposed food
-3.006
1.127
7.119
1
.008
.050
.005
.450
Exposure to the weather
-2.914
1.305
4.984
1
.026
.054
.004
.701
Constant
6.130
2.282
7.219
1
.007
459446
Threatening Factor Exposure Triggers Recurrence of Asthma in Children
307

Jaller, R., Tapias, E., … Garcia-Larsen, V. (2017).
Diet and Respiratory Health in Children from 11 Latin
American Countries: Evidence from ISAAC Phase III.
Lung, 195(6), 683–692.
https://doi.org/10.1007/s00408-017-0044-z
Chipps, B. E., Haselkorn, T., Rosén, K., Mink, D. R.,
Trzaskoma, B. L., & Luskin, A. T. (2018). Asthma
Exacerbations and Triggers in Children in TENOR:
Impact on Quality of Life. Journal of Allergy and
Clinical Immunology: In Practice, 6(1), 169–176.e2.
https://doi.org/10.1016/j.jaip.2017.05.027
Conn, K. M., Halterman, J. S., Lynch, K., & Cabana, M.
D. (2007). The Impact of Parents’ Medication Beliefs
on Asthma Management. Pediatrics, 120(3), e521–
e526. https://doi.org/10.1542/peds.2006-3023
Dharmayanti, I., Hapsari, D., & Azhar, K. (2013). Asma
pada anak di Indonesia : penyebab dan pencetus
Asthma among children in Indonesia :causes and
triggers. Jurnal Kesehatan Masyarakat Nasional,
Volume 9(29), 320–326.
Hughes, D. (2014). Childhood asthma and exercise.
Paediatrics and Child Health (Canada).
https://doi.org/10.1093/pch/19.9.467
Hyrkäs, H., Ikäheimo, T. M., Jaakkola, J. J. K., &
Jaakkola, M. S. (2016). Asthma control and cold
weather-related respiratory symptoms. Respiratory
Medicine, 113, 1–7.
https://doi.org/10.1016/j.rmed.2016.02.005
IDAI. (2016). Asma Anak. Pedoman Nasional Asma
Anak, 2.
ISAAC. (2013). ISAAC Tools. Retrieved February 25,
2018, from
http://isaac.auckland.ac.nz/resources/tools.php?menu=
tools1
Lewis, S., Bucher, L., Heitkemper, M., & Dirksen, S.
(2013). Medical-Surgical Nursing - 9th Edition (9th
ed.). Mosby Elsevier. Retrieved from
https://www.elsevier.com/books/medical-surgical-
nursing/lewis/978-0-323-08678-3
Lim, T. K., Ko, F. W. S., Benton, M. J., Berge, M. Van
den, & Mak, J. (2017). Year in review 2016: Chronic
obstructive pulmonary disease and asthma.
Respirology, 22(4), 820–828.
https://doi.org/10.1111/resp.13037
National Heart Lung and Blood Institute. (2007). Expert
Panel Report 3 (EPR-3): Guidelines for the Diagnosis
and Management of Asthma-Summary Report 2007. J
Allergy Clin Immunol, 120(5 Suppl), S94-138.
https://doi.org/10.1016/j.jaci.2007.09.043
Page, P. M., Broek, J. L., Bousquet, J., Baena-Cagnani, C.
E., Bonini, S., Canonica, G. W., … Schünemann, H. J.
(2017). Global Strategy For Asthma Management and
Prevention. Global Initiative for Asthma (Vol. 126).
https://doi.org/10.1183/09031936.00138707
Putu, N. L. E. (2012). Analisis Faktor-faktor Pemicu
Dominan Terjadinya Serangan Asma Pada Pasien
Asma. Universitas Indonesia.
Searle, A., Jago, R., Henderson, J., & Turner, K. M.
(2017). Children’s, parents’ and health professionals’
views on the management of childhood asthma: A
qualitative study. Npj Primary Care Respiratory
Medicine, 27(1), 1–6. https://doi.org/10.1038/s41533-
017-0053-7
Singh, S., Jindal, S., & Goyal, J. P. (2017). Risk Factors
for Bronchial Asthma in School Going Children.
Indian Journal of Pediatrics, 84(11).
https://doi.org/10.1007/s12098-017-2400-7
Sullivan, P. W., Ghushchyan, V., Navaratnam, P.,
Friedman, H. S., Kavati, A., Ortiz, B., & Lanier, B.
(2017). National Prevalence of Poor Asthma Control
and Associated Outcomes among School-Aged
Children in the United States. The Journal of Allergy
and Clinical Immunology: In Practice, 1–10.
https://doi.org/10.1016/j.jaip.2017.06.039
WHO. (2017). WHO | Asthma. WHO. Retrieved from
http://www.who.int/entity/mediacentre/factsheets/fs30
7/en/
Wilson, J. M., & Platts-Mills, T. A. E. (2018). Home
Environmental Interventions for House Dust Mite.
Journal of Allergy and Clinical Immunology: In
Practice, 6(1), 95–98.e3.
https://doi.org/10.1016/j.jaip.2017.10.003
Zahran, H. S., Bailey, C. M., Damon, S. A., Garbe, P. L.,
& Breysse, P. N. (2018). Vital Signs : Asthma in
Children — United States, 2001–2016. MMWR.
Morbidity and Mortality Weekly Report, 67(5), 149–
155. https://doi.org/10.15585/mmwr.mm6705e1
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
308
