
Effect of Cutaneous Stimulation and Virgin Coconut Oil on Skin
Moisture in Patients with Chronic Renal Failure
Putu Intan Daryaswanti
1
, Elyana Asnar
2
and Ilya Krisnana
1
1
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
2
Department of Physiology, Airlangga University, Surabaya, Indonesia
Keywords: Cutaneus Stimulation, Virgin Coconut Oil, VCO, Hemodialysis.
Abstract: Skin problem in patients with Chronic Kidney Failure that often appear that dry skin and most often appear
on the forearm and lower extremities. Dry skin that appears in patients undergoing hemodialysis is usually
due to atrophy of the sebaceous glands, impaired function of external secretions, and stratum corneum
hydration disturbance. The aim of this study was to explain of the combination of cutaneus stimulation and
VCO on skin moisture. Cutaneous stimulation and virgin coconut oil (VCO) was performed as a non-
pharmacological treatment option to improve skin moisture. This study used quasy experiment pre-post test
control group design, conducted between January – March 2018. A total of 52 patients undergoing
hemodialysis divided randomly into two groups. The treatment group was given cutaneous stimulation and
VCO for 4 weeks and the control group was not given cutaneous stimulation and VCO. The skin moisture
assessment was performed five times, ie pre-test at week0, week1, week2, week3 and post-test at week4
using skin moisture analyzer. Giving cutaneous stimulation and VCO effective in improving skin moisture
in patients undergoing dialysis seen from Wilcoxon test with p<0.05. Based on Friedman nonparametric test
results, there were significant differences in skin moisture value at five measurement times (pre-test, week1,
week2, week3, and post-test) p=0.000. Giving cutaneous stimulation and VCO can be used as an option to
improve skin moisture in patients undergoing hemodialysis.
1 BACKGROUND
Patients with Chronic Renal Failure (CRF) have at
least one change in their skin of 50-100% (Min et
al., 2016). One of the skin changes that occur is
pruritus where the mechanism that causes pruritus is
dry skin. Dry skin is described in most patients with
CRF and is thought to be a significant pathogenic
factor in pruritus and may increase the intensity of
itching in patients with CRF. In the study (Kolla et
al., 2012) found that 52% of patients who undergo
HD experience dry skin. Knowing early and
performing management of rapid dermatology
manifestations can reduce morbidity and improve
the quality of life of patients. Dry skin that appears
in patients with CRF who undergo hemodialysis is
usually caused due to atrophy of the sebaceous
glands, impaired function of external secretions, and
stratum corneum hydration disturbance. Dry skin in
patients with pruritic hemodialysis has lower
hydration than hemodialysis patients without
pruritus complaints (Roswati, 2013). Xerosis is a
common symptom of patients with dialysis which
occurs between 50-100%. It most often appears in
the lower extremities and forearms. It has been
reported that CRF-related pruritus is more common
and more severe in patients with xerosis. However,
patients with xerosis do not always suffer from
itching if they rehydrate and moisturize their skin
well. Thus the possibility of xerosis increases the
intensity of itch if associated with CKD-aP (Chronic
Kidney Disease-associated Pruritus) (Mettang,
2016). Skin moisture is state of moisture content of
the stratum corneum and a balance between the
evaporation of water and the ability of the skin to
retain water. Moisturizing skin can cause cracks,
allowing germs that can cause infection to enter the
body (Perry.A. Griffin., Potter, Patricia.A.,
Ostendorf, 2014). Based on the results interviews
with patients, all this time that is used to reduce dry
skin by using baby oil, olive oil, body lotion and
traditional oil sold in pharmacies. Results obtained,
moist skin only after use, a few hours later, the skin
will dry again.
338
Daryaswanti, P., Asnar, E. and Krisnana, I.
Effect of Cutaneous Stimulation and Virgin Coconut Oil on Skin Moisture in Patients with Chronic Renal Failure.
DOI: 10.5220/0008324903380344
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 338-344
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reser ved

Kidney failure can cause changes in the sweat
glands and oil glands that cause the skin to lose its
natural ability to moisturize. This condition can also
be caused by changes in metabolism in chronic renal
failure, which are related to the volume of fluid from
patients undergoing dialysis.
Cutaneous stimulation is a stimulation of the skin
and underlying tissue that aims to reduce unwanted
signs and symptoms such as pain, muscle spasms,
inflammation, nausea and so on (Bullechek, Gloria;
Butcher Howard; Dechteerman, joanne; wagner,
2013). Cutaneous stimulation may include massage,
hot bath, ice packs and TENS (Transcutaneous
Electrical Nerve Stimulation). In this study using
cutaneous stimulation type of massage with stroking
technique. Massage stroking technique is the
provision of massage from proximal to distal along
the tissue at depth and speed corresponding to the
desired effect (Hollis, 1998). This technique is
chosen because it is easy to do independently by the
patient. Massage applied to dry skin certainly causes
friction and pain on the skin surface. And the
combination when given a massage that is by giving
the VCO. VCO is a pure coconut oil has antiseptic
effect and is used as an efficient skin moisturizer
(DebMandal & Mandal, 2011). VCO is a processed
product that contains fatty acids (especially uric acid
and oleic) which has the properties of softening the
skin. In addition VCO effective and used as a
moisturizer on skin so that can increase skin
hydration and accelerate skin healing and can
eliminate itching (Sukartin, 2005). The aim of this
study was to explain of the combination of cutaneus
stimulation and VCO on skin moisture.
2 METHODS
2.1 Study Design and Sample
This was a quasy experimental research with pre-
post test control group design. This research was
conducted for 4 weeks from 22 January 2018 – 21
February 2018 at Hemodialysis Room Regional
Hospital Public Buleleng, Singaraja Bali.
Calculation of sample size using Lemeshow
formula, where level of significant 5% = 1.96, power
the test 80% = 0.84 and got 24 subjects in each
group. Considering the probable loss in the sample,
the number of subjects in each group was increased
to 26. This study involved 52 patients: 26 patients
comprised the experimental group, whereas 26
patients comprised the control group.
The population in this study were patients who
underwent hemodialysis. Sampling technique in this
study was done by random sampling with inclusion
criteria: respondents did regular HD twice a week,
experienced dry skin measured using skin moisture
tool, while the exclusion criteria were patients who
did HD cito, decreased consciousness, women who
have menopause, patients with HD travelling,
patients with Hbs Ag (+) and patients with injury or
secondary infection of the skin. Random selection of
samples was perfomed. We believed that patients
undergoing dialysis in the same session could affect
each other, so we chose the control and study groups
according to their session times. Patients who met
the criteria were grouped according to the time of
their sessions. The drawing method was used to
determine which group would start the study. After
drawing, HD patients in the morning sessions were
considered the study group, whereas those in the
afternoon session were regarded as the control
group. Group study: giving cutaneous stimulation
for 30 minutes and VCO 5 ml, before patients
undergoing standard HD treatment on the skin of a
hand that is not attached to the AV Shunt. Group
control: group that did not giving stimulation
cutaneous and VCO.
2.2 Data Collection
2.2.1 Patient Information Form
The patients information form was developed by the
researchers by screening the literature. This form
consisted of 7 questions that included
sosiodemographic characteristic and duration of
hemodialysis.
2.2.2 Skin Moisture Analyzer
Skin moisture analyzer using SK-IV Digital
Moisture Monitor for Skin as especially designed
precision instrument, this product utilizes the lastest
Bioelectric Impedance Analysis (BIA) technology.
With a non-destructive measuring approach. In the
skin analyzer, has an LCD screen that serves to
display data measurements of skin moisture. This
tool has a small design and shape and portable so it
can be taken anywhere. Measurement of skin
moisture is done in a very short time is within 6
seconds and appears in the form of percentage
figures. Standard values of skin moisture in the arm
are: 0-35% meant very dry skin, 36-45% meant
normal skin and 46-100% meant moist skin.
Effect of Cutaneous Stimulation and Virgin Coconut Oil on Skin Moisture in Patients with Chronic Renal Failure
339

2.3 Process
2.3.1 Study Group
In the study group, the first patient information form
and measure the skin’s moisture level before patients
undergoing HD treatment. In practice, giving
cutaneous stimulation in this case massage is given
for 30 minutes with stroking technique, and when
giving massage followed by giving VCO as much as
5 ml. 10 ml bottle given 5 ml VCO given each
intervention. Intervention is given twice a day, ie
morning before HD treatment and night before going
to bed. Patients taking part in the study were patients
with regular HD twice a week. At the first session of
the first week, the patient was provided with 5
bottles (25 ml) of VCO to the house until the second
HD session of the first week, the patient was again
provided with 7 bottles (35 ml) for the house. Then
when the first HD session in the second week is
given back and forth for four weeks. At the
beginning of administration, perform allergic tests
on the back of the hand for 10 minutes, by applying
a small amount of VCO, if the patient feels itchy or
sore, there is a possibility that the patient is allergic,
and the patient is not included as a research sample.
VCO should not be given on the hands of the AV
shunt and on the hands that are having an open
wound.
Patients in the study group performed skin
moisture measurements every week. Measurements
were made five times, ie pre-test in the zero week,
first week, second week, third week, and post-test in
the fourth week.
2.3.2 Control Group
In the control group, the first patient information
form and measure the skin’s moisture level patients
undergoing HD treatment. Education about the
research procedure was provided to the patients.
Provide VCO and cutaneous stimulation guides at
the end after doing post-test. Skin moisture
measurements were made twice in the first sessions
of HD in the fifth week. Then the patient is given
one bottle of VCO as much as 300 ml.
2.4 Virgin Coconut Oil (VCO) Practice
VCO provided by students majoring in Traditional
Medicine, Airlangga University. VCO is made from
selected coconut is old coconut. Oil is made without
heating. VCO is packed in clear 10 ml plastic bottles
(for study group) and 300 ml (for control group),
tightly sealed so that it does not spill easily. Clear
colored oil, not rancid and smells typical of coconut
oil.
2.5 Data Analysis
The statistical analyses were performed with SPSS.
Average and percentage were used for analysis of
descriptive features. Normal distribution of the data
was tested by Shapiro-Wilk test. The two groups
were compared via Wilcoxon test and Independent t-
test. To evaluate more than two variance, the
Friedman test is used.
2.6 Ethical Considerations
This study has gained approval of ethical eligibility
from Ethical Commision of Health Research at
Nursing Faculty of Universitas Airlangga number
609-KEPK on 4
th
January 2018. Written consent was
obtained from all centers. The aim of the study was
explained to the participants, and informed consent
forms the participants were collected.
3 RESULTS
Fithty four selected for eligibility with simple
random sampling, 2 patients were dropped out
because passing away before post test, leaving a
final study sample of 52 patients, who were assigned
to intervention group (n=26) and control group
(n=26).
Based on table 1 shows the characteristics of
respondent by age, gender, education, occupation,
and duration of hemodyalisis. Most respondents
were 30-45 years old (38.5%), male sex (69.2%),
had level of education in high school (42.3%), did
not work (19.2%), and undergoing HD less than five
years (75%). Based on homogeneity test, it was
found that the characteristic of age, education and
occupation showed homogeneous (p>0.05).
Dry skin occurred in both group, all of
respondents both the intervention group and control
group obtained dry skin. After given intervention
has increased the skin moisture level to normal as
much 11 (42.3%) and 9 (34.6%) skin becomes
moist. However, there are 6 patients (23%) are still
at very dry skin level, but skin’s moisture value has
increased slightly.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
340
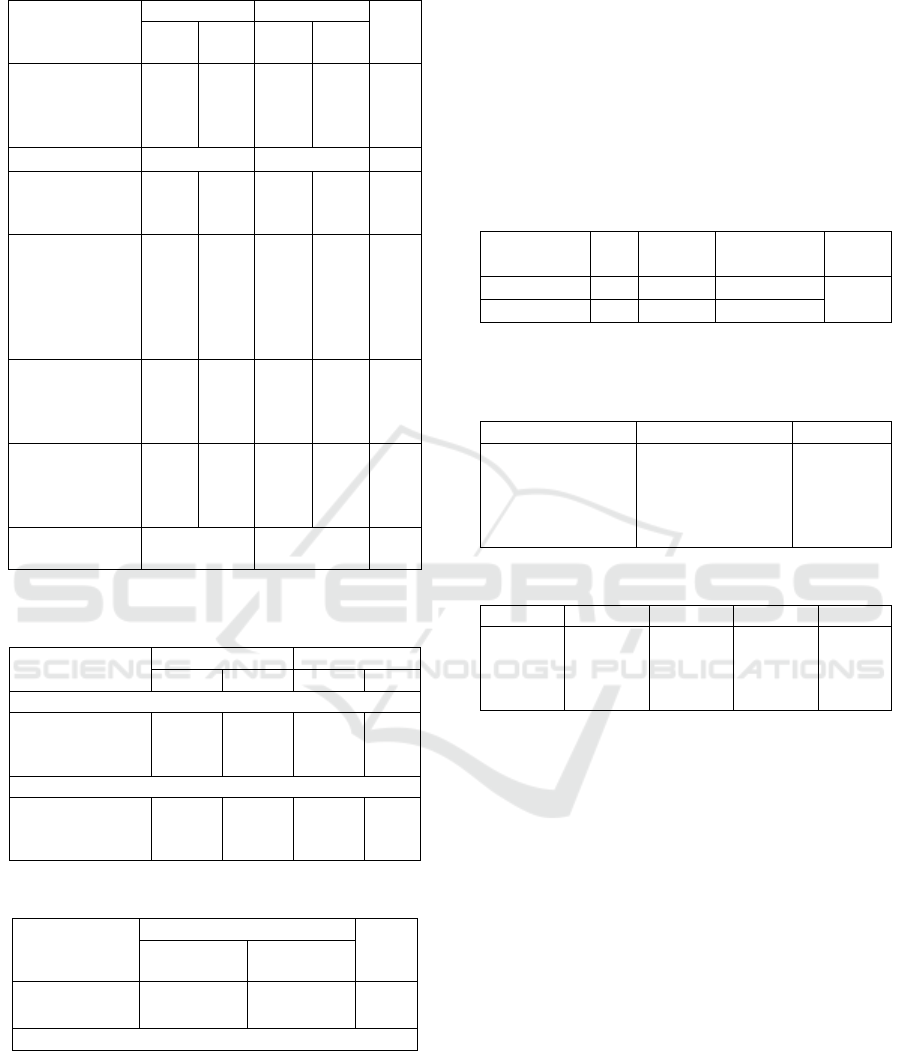
Table 1: Characteristics and demographic.
Characteristic
Intervention
Control
p
val
ue
N
%
n
%
Age (years)
30-45
46-55
56-65
14
6
6
53.8
23.1
23.1
6
11
9
23.1
42.3
34.6
0.1
02
Mean Age
47.73±7.68
50.85±7.58
Gender
Male
Female
14
12
53.8
46.2
22
4
84.6
15.4
0.0
16
Education
Not schooling
Primary
Secondary
High School
Collage
1
6
5
11
3
3.8
23.1
19.2
42.3
11.5
-
5
5
11
5
-
19.2
19.2
42.3
19.2
0.3
92
Occupation
Not Working
Working
10
16
38.4
61.6
5
21
19.2
80.8
0.1
20
HD Duration
0 – 5 years
6-10 years
>10 years
16
8
2
61.5
30.8
7.7
23
3
-
88.5
11.5
-
0.0
23
Mean HD
Duration
4.76±3.13
2.40±1.76
Table 2: Incidence of skin moisture in intervention and
control group (pre test-post test).
Stage of skin
moisture
Intervention
Control
n
%
n
%
Skin moisture before intervention (pre test)
Dry skin
Normal
Moisture
26
0
0
100
0
0
26
0
0
100
0
0
Skin moisture after intervention (post test)
Dry skin
Normal
Moisture
6
11
9
23
42.3
34.6
26
0
0
100
0
0
Table 3: Result Wilcoxon and Independent t test.
Group
Skin Moisture
p
value
Pre test
Post test
Intervention
Control
20.31±4.84
21.96±5.89
41.08±5.95
21.12±4.44
0.000
0.557
Independent t test p: 0.000
Table 3 shows, that effectivity of cutaneous
stimulation and vco on skin moisture, each group
was tested by Wilcoxon statistic analysis, because
the result of Shapiro Wilk data not normally test, the
normal data distribution (p<0.05). Based on the
results of the test showed that the results obtained
significant in the treatment group (p<0.05), whereas
in the control group showed no significant result
(p>0.05).
After testing on each group, the next test is to
know the difference of effectivity of cutaneous
stimulation and VCO in the intervention and control
group. The used Independent t-test because the
distribution of the difference data between pre and
post both treatments is normally distributed
(p>0.05).
Table 4: Result Independent t-test.
Groups
N
Mean
Standar
Deviasi
p
value
Intervention
26
20.77
6.641
0.000
Control
26
-0.85
4.722
Table 5: Distribution of mean and standar deviasi of skin
moisture scores of the participants in treatment group
according to measurement time (Friedman Test).
Measurement time
Study griup (n=26)
p value
week 0
week 1
week 2
week 3
week 4
20.69 ± 5.98
24.88 ± 6.21
27.92 ± 5.78
32.35 ± 5.67
41.46 ± 6.51
0.000
Table 6: Result post hoct test of Friedman test.
Weeks
Week1
Week2
Week3
Week4
0
1
2
3
0.000
-
0.000
0.000
-
0.000
0.000
0.000
-
0.000
0.000
0.000
0.000
The results in table 4 show that there is a
significant difference (p<0.05) in the treatment
group compared with the control group.
Giving cutaneous stimulation and VCO is given
for four weeks. And the skin moisture measurement
is done 5 times, that is pre test in the first week,
second week, third week, fourth week and post test
in the fifth week. To test the result of skin moisture
measurements on a weekly basis the measurements
in the group given cutaneous stimulation
intervention and VCO using Anova Repeated
Measure test. However, since the residual value of
the data distribution group is not normally
distributed, it uses the Friedman test. Table 5 shows
a significant relationship between the differences in
mean skin moisture score in the first week and the
fifth week in the treatment group.
The groups that differed significantly on the
friedman test, using the post hoc test by performing
the Wilcoxon Signed Rank Test. there was a
significant difference in skin moisture value between
Effect of Cutaneous Stimulation and Virgin Coconut Oil on Skin Moisture in Patients with Chronic Renal Failure
341

week 0 value with first week (0.000), second week
(0.000), third week (0.000) and fourth week (0.000).
4 DISCUSSION
The results of this study showed that all patients had
dry skin (100%). Ankudowicz et al, in patients
treated with hemodialysis because of CRF, various
skin lesions were detected, the most common
symptomps were skin dryness and pruritus
(observed in 63% of patients) (A. Ankudowicz,
Król, & Dębska-Ślizień, 2016). Giving cutaneous
stimulation and VCO can improve skin moisture in
patients with CRF who undergo hemodialysis tend
to have dry skin. Dry skin that appears in patients
dialysis is usually due to retention of vitamin A
which causes decreased function of the kidneys to
secrete some body substances. This vitamin A
accumulates in the subcutaneous tissue of the skin.
This excessive vitamin causes the atrophy of
sebaceous glands and sweat glands that make skin
dry and itchy (Melastuti, Erna., Setyaningrum,
2016). Xerosis is a skin disorder number two after
pruritus. Skin xerosis is a frequent complication in
hemodialysis patients. It can be seen in CRF before
HD, but a significant rise in its frequency is found
after the start of dialysis (Masmoudi, Darouiche,
Salah, Hmida, & Turki, 2014). Dry skin conditions,
triggering the itching of the skin. If this condition
persists there will be pruritus. Before pruritus
occurs, making the skin moist is very important. In
addition to improving patient comfort can also
improve the quality of life patients. The results
showed that the combination of cutaneous
stimulation and VCO significantly gave good
results. Patients say more moist and less itchy skin,
making patients more comfortable.
Cutaneous stimulation in the form of massage, in
addition to providing a sense of relaxation in the
skin, also helps the VCO more quickly absorbed into
the skin. The massage is given in the type of
stroking, which provides massage from the proximal
to distal direction along the tissue at depth and speed
corresponding to the required effect, but the
direction of stroking may vary to provide greater
comfort (Hollis, 1998). Massage is oriented to the
superficial region, so it can stimulate the receptors
that exist on the skin. One of the physiological
effects of massage is its ability to increase local
blood and lymphatic flow, improve nutritional
status, facilitate removal of toxins released by
wounded tissue and speed healing (Hollis, 1998).
Increase blood flow and lymph nodes may occur as a
result of direct mechanical displacement, as well as
the neural reflex response of blood and lymph
channels. In addition, vasodilator release, such as
histamine from mast cells, is associated with
increased local blood flow. Massage that is done can
provide relaxation to the muscles so that the blood
vessels dilate. Under these conditions, can lower
levels of cortisol, epineprin and norepineprin (Unal
& Balci Akpinar, 2016). Other physiological effects,
massage can increase the secretions of sweat glands
and sebaceous glands. Massage mechanically has the
ability to change the texture and consistency of the
skin if doing repeatedly and prolonged, the skin will
be more elastic (Hollis, 1998).
Most of patients had increased skin moisture
(94%) after giving VCO, 6% did not increase
significantly, but showed slight improvement. A
total of 17 people after being given intervention
have not been at the skin level to be moist. As many
as 11 people who were previously at the dry skin
level became normal skin, there was an increase of
approximately 20 points. While as many as 6 people
remain in dry skin condition although there is an
increase in value in quantity. This is because the
skin moisture value at pre test is at very low value
(<21%), so to achieve the normal value required a
considerable increase of points. The increase in the
value of six people is approximately 15 points. The
skin condition of each patient is certainly not always
the same, some factors that cause the patient to
remain in dry skin condition after four weeks of
intervention due to atrophy of the sebaceous glands
associated with decreased lipid surfaces that cause
dehydration of the stratum corneum (Masmoudi et
al., 2014). In addition to the duration of patients
undergoing HD also may affect skin moisture due to
the decline in the glans with abnormal functions
associated with hypervitaminosis A when patients
undergoing dialysis (Anna Ankudowicz, Król,
Dębska Ślizień, & Czernych, 2018); (Robles-
Mendez, Vazquez-Martinez, & Ocampo-Candiani,
2015). Therese et al, observed in atopic dermatitis
patients, the results are an increase in stauts, whereas
formerly atopic patients of severe dermatitis after
being given VCO intervention, became atopic of
moderate dermatitis (Evangelista, Casintahan, &
Villafuerte, 2014). Noor et al study showed 24.8%
increase in skin moisture for lotions with VCO-SLPs
compared with 12.7% increase in skin moisture in
regular lotion use for duration of use twice daily for
28 days. The use of lotions with VCO-SLPs has
igher moisture retention and this could be due to the
high occlusion factor of smaller particles.
Moisturizing lotion containing VCO with 0.608 μm
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
342

show a better way of working that is by extending
the effects of moisture on the skin. This effect can be
caused by a smaller particle size that allows the
particles to be maintained in the stratum corneum
layer. The most important criterion for moisturizers
is to prevent water loss from the skin and keep the
moisture of stratum corneum skin about 20-35% or
more. In addition to increasing skin hydration, VCO
can also improve skin elasticity. There was an
increase in skin elasticity by 2.60% from day 0 and
day 28 compared to using moisturizers could be an
increase of 0.76% after 28 days. This may be due to
higher skin hydration and decreased transpidermal
water loss (Noor, Norhayati Mohamed., Aziz, Azila
Abd., Sarmidi, Mohamad Roji., Aziz, 2013).
When the VCO is applied to the skin, the VCO
not only coats the skin, but also penetrates the skin.
VCO has saturated fat and contains 62% Medium
Chain Fatty Acids (MCFAs). When applied to the
skin, MCFAs react with the lipase of the skin flora
and convert it into free fatty acids, which penetrate
the dermis. In addition, VCO has been shown to
destroy free radicals, compounds that can cause skin
disorders. The antioxidant capacity of VCO can be
caused by phenolic compounds such as ferulic acids
and p-coumaric acids (Evangelista et al., 2014).
VCO is applied to the skin, in addition to coating the
skin, cover and protect by slowing transpidermal
water loss and increase hydration in the stratum
corneum and upper layer of dermis, this makes the
skin moist (Verallo-Rowell, Dillague, & Syah-
Tjundawan, 2008).
The use of traditional coconut oil as a lotion has
been done in many parts of the world. Coconut oil is
shown to have an antiseptic effect and is used as a
safe skin moisturizer (DebMandal & Mandal, 2011).
In addition to cheap, coconut oil is also easy to
obtain and easy to make.
4.1 Limitations
This study has some limitation. Limitations of this
study are that researcher can not control well during
the implementation of home interventions.
Respondents only provided an observation sheet and
reminded via SMS or telp. Researcher rely on the
results of an observation sheet that has been filled
with the patient or patient’s family.
5 CONCLUSIONS
Based on the test results of the treatment, obtained
significant results on the treatment of cutaneous
stimulation and VCO. That the provision of
cutaneous stimulaton and VCO can effectively
improve skin moisture and can be used as a non-
pharmacological therapy option to improve skin
moisture. In addition VCO is easy to obtain, cheap
and easy to make.
REFERENCES
Ankudowicz, A., Król, E., & Dębska-Ślizień, A. (2016).
Do Patients With End-Stage Chronic Renal Failure
Treated With the Use of Hemodialysis Have Healthy
Skin? Evaluation of Skin Lesions and Basic Education
About Risk Factors for Skin Cancer in This Patient
Population. Transplantation Proceedings, 48(5),
1435–1438.
https://doi.org/10.1016/j.transproceed.2016.03.004
Ankudowicz, A., Król, E., Dębska Ślizień, A., &
Czernych, R. (2018). The risk of skin diseases in
maintenance hemodialysis. Transplantation
Proceedings.
https://doi.org/10.1016/J.TRANSPROCEED.2018.02.
133
Bullechek, Gloria; Butcher Howard; Dechteerman, joanne;
wagner, C. (2013). Nursing Intervention Classification
(NIC).
DebMandal, M., & Mandal, S. (2011). Coconut (Cocos
nucifera L.: Arecaceae): In health promotion and
disease prevention. Asian Pacific Journal of Tropical
Medicine, 4(3), 241–247.
https://doi.org/10.1016/S1995-7645(11)60078-3
Evangelista, M., Casintahan, F., & Villafuerte, L. (2014).
The effect of topical virgin coconut oil on scorad,
transepidermal water loss and skin capacitance in mild
to moderate pediatric atopic dermatitis: A randomized,
double-blind clinical trial. International Journal of
Dermatology, 53(4), 100–108.
https://doi.org/10.1111/ijd.12339
Hollis, M. (1998). Margaret Hollis, Elisabeth Jones-
Massage for Therapists (1998)(1).pdf (Second Edi).
Oxford: Blackwell Science.
Kolla, P. K., Desai, M., Pathapati, R. M., Mastan Valli, B.,
Pentyala, S., Madhusudhan Reddy, G., & Vijaya
Mohan Rao, A. (2012). Cutaneous Manifestations in
Patients with Chronic Kidney Disease on Maintenance
Hemodialysis. ISRN Dermatology, 2012, 1–4.
https://doi.org/10.5402/2012/679619
Masmoudi, A., Darouiche, M. H., Salah, H. Ben, Hmida,
M. Ben, & Turki, H. (2014). Cutaneous Abnormalities
in Patients with End Stage Renal Failure on Chronic
Hemodialysis. A Study Of 458 Patients. J Dermatol,
86–94.
Melastuti, Erna., Setyaningrum, D. . (2016). Effectiveness
of providing Virgin Coconut Oil (VCO) towards
pruritus reduction: Study on patients with chronic
kidney disease undergoing hemodialysis. In Global
Nursing Challenges in The Free Trade Era (pp. 281–
285). Surabaya.
Effect of Cutaneous Stimulation and Virgin Coconut Oil on Skin Moisture in Patients with Chronic Renal Failure
343

Mettang. (2016). Pruritus. London: Springer.
Min, J. W., Kim, S. H., Kim, Y. O., Jin, D. C., Song, H.
C., Choi, E. J., … Kim, Y. K. (2016). Comparison of
uremic pruritus between patients undergoing
hemodialysis and peritoneal dialysis. Kidney Research
and Clinical Practice, 35(2), 107–113.
https://doi.org/10.1016/j.krcp.2016.02.002
Noor, Norhayati Mohamed., Aziz, Azila Abd., Sarmidi,
Mohamad Roji., Aziz, R. (2013). The Effect of Virgin
Coconut Oil loaded Solid Lipid Particles (VCO-SLPs)
on skin hydration amd skin elasticity. Jurnal
Teknologi, 62(1), 39–43.
Perry.A. Griffin., Potter, Patricia.A., Ostendorf, W. R.
(2014). Clinical Nursing Skills & Technique (Eighth
Edi). Canada: Elsevier Inc.
Robles-Mendez, J. C., Vazquez-Martinez, O., & Ocampo-
Candiani, J. (2015). Skin manifestations of chronic
kidney disease. Actas Dermo-Sifiliográficas (English
Edition), 106(8), 609–622.
https://doi.org/10.1016/j.adengl.2015.09.001
Roswati. (2013). Pruritus pada pasien Hemodialysis.
Cermin Dunia Kedokteran, 40(4), 260–264.
Sukartin, K. & S. (2005). Gempur Penyakit dengan VCO.
Jakarta: PT. AgroMedia Pustaka.
Unal, K. S., & Balci Akpinar, R. (2016). The effect of foot
reflexology and back massage on hemodialysis
patients’ fatigue and sleep quality. Complementary
Therapies in Clinical Practice, 24, 139–144.
https://doi.org/10.1016/j.ctcp.2016.06.004
Verallo-Rowell, V. M., Dillague, K. M., & Syah-
Tjundawan, B. S. (2008). Novel antibacterial and
emollient effects of coconut and virgin olive oils in
adult atopic dermatitis. Dermatitis : Contact, Atopic,
Occupational, Drug, 19(6), 308–315.
https://doi.org/10.2310/6620.2008.08052
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
344
