
Mind-Body-Spiritual Care for Coronary Heart Disease Patients
A Systematic Review
Ninuk Dian Kurniawati, Nursalam
Faculty of Nursing, Universitas Airlangga, Kampus C UNAIR, Mulyorejo, Surabaya, Indonesia
Keywords: Mind-Body-Spiritual, Nursing, Care, Coronary Heart Disease, Acute Coronary Syndrome, Distress.
Abstract: Background. Coronary heart disease (CHD) patients hospitalized for acute coronary syndrome may
experience bio-psycho-spiritual distress. The objective of this study was to assess evidence of nursing care
or other interventions addressing the patient’s bio, psycho, and spiritual issues and determine the efficacy of
the existing intervention tailored to tackle the issues. Methods. A comprehensive search was carried out on
various databases i.e. PubMed (Medline), Embase, CINAHL, Scopus, Springerlink, PsycInfo, ProQuest,
EBSCOHost, Web of Science Clarivate Analytic and Science Direct. Unpublished studies were also
searched from libraries and university repositories. Results. Seventeen out of 1215 papers meeting inclusion
criteria were included in the review. The study encompassing mind, body, and spiritual nursing care was
very limited in number, most reviewed papers were not on nursing care and examined the individual
intervention. All reviewed studies reported positive results. Nevertheless, the reviewed studies were very
diverse in terms of intervention (dose, the method of delivery, length of follow up), the patients’ condition
treated, and outcome measured makes it difficult to conclude on a certain nursing care model and its
effectiveness for the CHD patients. Conclusion. Further study is necessary to develop the best nursing care
model for coronary heart disease patients and to examine its effectiveness in alleviating patients’ issues.
1 BACKGROUND
Patients with coronary heart disease (CHD) may
experience psychological distress and also physical
issues. A study conducted at three hospitals in
Surabaya, Indonesia revealed that patients with CHD
hospitalized for acute coronary syndrome
experienced psychological stress, ranging from mild
to severe in scale, as well as other issues
(Kurniawati, Nursalam & Suharto, 2017).
Psychological distress stemmed from the illness-
related issues, the hospital environment, the other
patients’ condition and separation from family or
relatives; whereas the other dominant issues were a
hemodynamic imbalance, discomfort, and pain
(Kurniawati et al., 2017). Physical stress
experienced by CHD patients included unstable
airways, oxygenation, and hemodynamic
disturbance. Psychological stress might be caused by
a critical condition, death risk, social isolation and
an alien environment (Elliot, Aitken & Chaboyer,
2007). Psychological issues when left untreated will
negatively affect CHD patients. A study involving
100 respondents confirmed the relationships
between psychological problems and biological
markers of inflammation that play a significant role
in exacerbating the CHD, namely IL-1β, IL-6, and
TNF-α (Miller, Freedland, Carney, Stetler & Banks,
2003). Another study of 82 AMI and CABG
survivors concluded that psychological distress
correlated negatively with health-related quality of
life (HRQOL), post-traumatic distress symptoms,
and mental health outcomes (Bluvstein, Moravchick
& Sheps, 2013).
Patients' spiritual need should not be neglected
by the nurse. A systematic review of 54 studies
comprising 12,327 patients concluded that many
patients want their doctor to address their spiritual
needs during the medical consultation (Best, Butow
& Olver, 2015). Similarly, a cross-sectional study in
Palestina found that providing spiritual care was
very important to 275 cardiac patients treated at a
coronary care unit (Abu-El-Noor & Abu-El-Noor,
2014). Another study found that both psychological
and spiritual care have a strong relationship with a
patient’s satisfaction (Clark, Drain & Malone, 2003).
Therefore, spiritual care is an important aspect that
cannot be overlooked.
394
Kurniawati, N. and Nursalam, .
Mind-Body-Spiritual Care for Coronary Heart Disease Patients.
DOI: 10.5220/0008325803940405
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 394-405
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Interventions that include the physical,
psychological and spiritual (mind-body-spiritual)
aspects will help the patient overcome the physical
and psychological stress optimally. Yet, to the best
of our knowledge, a systematic review regarding this
intervention is not available.
Some systematic reviews and meta-analyses
have examined the mind-based intervention and
concluded the efficacy of the intervention in
reducing stress of healthy individuals (Khoury,
Sharma, Rush & Fournier, 2015), psychological,
physical, and bio-molecular parameters of HIV
patients (Yang, Liu, Zhang, & Liu, 2015), and
patients with vascular disease (Abbott et al., 2014).
The mechanism by which the mind-based
interventions affect wellbeing has also been studied,
where a systematic review and meta-analysis of 20
studies found several factors underlying mind-based
intervention, i.e. cognitive and emotional reactivity,
mindfulness, anxiety reduction, ability in digesting
the problem, self-compassion and psychological
flexibility (Gu, Strauss, Bond & Cavanagh, 2015).
To date, there is no review that examines evidence
of mind body-spiritual nursing care for CHD
patients.This systematic review evaluates evidence
of a nursing care model addressing a patient’s issues
and determines the efficacy of the existing model
tailored to tackle the issues.
2 METHODS
The systematic review was guided by PRISMA
protocol (Preferred reporting items for systematic
review and meta-analysis) (Moher et al., 2009).
2.1 Identification of Studies
Searches of both published and unpublished studies
were conducted by the authors. The search for
published studies was done comprehensively using
several keywords: “coronary heart disease” OR
“acute coronary syndrome” OR “heart attack” OR
“hemodynamic” OR “pain”, “nurse” OR “nursing
care”, “mind*”, “body”, “spirit*”, “distress”,
“holistic”, “quality of life” OR self-efficacy, and
“well being.” The search was carried out on various
databases i.e. PubMed (Medline), Embase,
CINAHL, Scopus, Springerlink, PsycInfo, ProQuest,
EBSCOHost, Web of Science Clarivate Analytic and
Science Direct. Unpublished studies were also
searched from libraries and university repositories.
Several MeSH terms used to locate articles were
heart disease, meditation, stress, yoga,
catecholamines, hormones, hypnosis, guided
imagery, spiritual, mindfulness, body, clinical trial,
coronary artery disease, adult, and human. The
search terms were formulated using the PICO
framework, where P (population) was patients with
coronary heart disease with acute coronary
syndrome, I (intervention) was nursing intervention
or nursing model consisted of mind-body spiritual,
or mind-body or spiritual nursing, C (comparison)
was standard care or other relevant care, and O
(outcomes) was either physical, psychological, bio-
molecular or quality of life. The searches were limit
to publication in English or Bahasa Indonesia and
year of publication of 2000 up to February 2018.
2.2 Study Selection
The titles and abstracts of citations identified by
searches were examined by two reviewers
independently; disagreements about the study were
resolved by consensus among the authors.
2.2.1 Inclusion and Exclusion Criteria
Some criteria were imposed for study selections: 1)
an experimental or observational study, 2) adult
sample, 3) patients with coronary heart disease or
acute coronary injury, 4) addressing bio-psycho-
social-spiritual issues, 5) the intervention(s) was
mind-body-spiritual or mind-body. Studies falling
under these criteria were excluded from the review:
1) reviews, 3) qualitative study, and 4) the outcome
measures did not relate to health.
2.2.2 Quality Assessment
Assessment of methodological quality of studies
meeting the inclusion criteria was conducted using
the CONSORT (consolidated standards of reporting
trials) checklist (Schulz, Altman, Moher & Group,
2010) or STROBE (strengthening the reporting of
observational studies in epidemiology) checklist
(von Elm et al., 2008). Critical appraisal was guided
by the JAMA (Journal of American Medical
Association) guides for quantitative studies (Guyatt,
Sackett & Cook, 1993, 1994). The critical appraisal
and study quality assessment were carried out by the
authors independently; and, as previously stated, any
discrepancies between the authors’ decisions were
resolved by consensus.
Mind-Body-Spiritual Care for Coronary Heart Disease Patients
395
2.2.3 Types of Interventions
Studies are considered eligible if the intervention
given was mind-body spiritual or mind-body or
spiritual care for patients.
2.2.4 Types of Outcome Measures
Outcome measures were stress reduction, spirituality
enhancement, biomolecular markers, pain reduction,
and regulation of hemodynamic parameters e.g.
blood pressure, heart rate, oxygenation. The other
outcome measures were the quality of life and
perceived self-efficacy.
2.2.5 Length of Follow-up
Studies that measure the outcome shortly after the
intervention or long after the intervention (up to 1
year) were both included in the review.
3 RESULTS
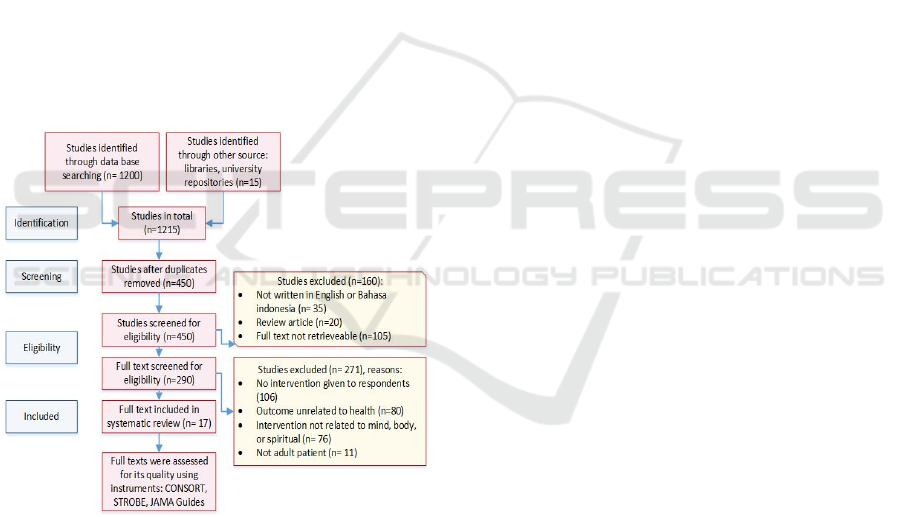
Diagram 1: Study selection based on PRISMA
statement.
As can be seen from Diagram 1, 1200 studies were
yielded from the electronic search while an
additional 15 studies were found from the manual
search. The first screening process managed to
remove 765 articles because they were identified as
duplicates. A first screening process based on
language, type of article, and availability of its full
text was able to exclude 160 articles. The remaining
290 studies were then screened for eligibility based
on some inclusion and exclusion criteria, i.e.
outcome measures, type of intervention, and sample
characteristics. Seventeen studies were included in
the review.
3.1 Study Characteristics
Table 1 summarizes articles included in the
systematic review; 4 articles were published
between 2000 and 2007 and the remaining were
published or conducted from 2010 to 2017. Studies
were conducted in diverse locations: Asia, America,
and Europe. Eleven studies were RCT and the rest of
them were not RCT experiments. Eight studies used
standard care groups, 2 articles from the same study
employed waitlist control, 2 with placebos, 1 with
self-help booklet, and 2 studies not using a control
group. Patients recruited in the studies vary slightly,
with 3 studies recruiting CHD patients peri-
operatively, 3 during acute coronary syndrome
(ACS) attack, and the remaining recruited
hospitalized CHD patients or CHD patients in the
community.
3.2 Intervention Characteristics
It was difficult to find a specific nursing intervention
or nursing care model addressing comprehensively
patients’ mind, body and spiritual needs. Table 1
summarizes the characteristics of intervention given
to the patients to address the mind, body, or spiritual
issues of the patients. There are a wide variety of
interventions given to the patients, ranging from
mindfulness exercises, yoga, spiritual mantram,
nursing care, and other interventions.
The majority of interventions were mindfulness
exercise or spiritual intervention alone, or a
combination of mind and spiritual, which were
delivered individually to the respondents; only one
intervention involved group meetings. Additionally,
most interventions were provided in healthcare
settings, only 5 interventions were given for
outpatients.Most included studies reported frequency
and dose of intervention given to respondents. The
dose ranging from 20 minutes up to 24 hours a day
with frequency ranging from once a day until
continuously during the day. The length of
intervention and follow up ranges from 3 days to 1
year. Some interventions were provided by nurses or
other healthcare professionals, the rest were done by
the respondents independently. Most of these
interventions were directed to tackle a single or
group of patients’ issues, but none of them were
tailored to overcome the mind, body, and spiritual
issues of patients comprehensively.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
396

Table 1: The Study and Intervention Characteristics.
No Study &
Setting
Design Sample Intervention (s) Contr
ol
Outcome
(s)
Findings
1. Bakara et al.
(2013)
Indonesia
Quasi
experim
ent
42 ACS
patients
not in
ACS
attack,
hospitaliz
ed ≥24 h,
fully
awake,
with
depression
, anxiety,
or stress;
treatment
group
(n=23, 4
D.O),
control
group
(
n=19
)
Self-emotional
freedom
technique 15 m
in duration once
only, guided by
trained
personnel
Standa
rd
care
Depressio
n, anxiety,
stress.
Significant
difference in mean
score of anxiety and
stress. No
significant
difference at
depression score
2. Bakar
(2017)
Indonesia
Quasi
experim
ent
20 ACS
patients :
Treatment
group
Control
group
Islamic nursing
care model
characterized by
maintaining
confidence,
compassion, and
com
p
etence.
Standa
rd
nursin
g care.
Psychospi
ritual
comfort
and
cortisol
level.
The nursing care
significantly
enhanced patients’
psychospiritual
comfort but it did
not attenuate the
level of cortisol.
3. Carneiro et
al. (2017)
Brazil
RCT,
double
blind
41
patients
with ACS
and other
cardiovasc
ular
disease,
allocated
randomly
into 3
groups
(@16
patients):
Spirit
passé
group
Sham
group
Placebo
group
• Spirits “passé”
group and
Sham: 10 min
sessions 3
consecutive
days,
instructed to
direct thought
at Jesus with
wishes of
healing
• Spirits group:
spirit healers
and
respondents
moved hands
longitudinally
from head to
toe for 5 m,
followed by
laying hands
over
respondents’
head and
chest.
• Sham: healer
transmitting
sincere wishes.
Placeb
o: 10
min
sessio
ns for
3
consec
utive
days
receivi
ng no
interv
ention
.
Depressio
n, anxiety,
pain
intensity,
physiologi
c
parameter
s (HR,
SpO2).
Spirit passé
significantly
effective in
reducing anxiety,
muscle tension,
improving SpO2
and well-being.
Mind-Body-Spiritual Care for Coronary Heart Disease Patients
397

4. Delui, Yari,
Khouyinezh
ad, Amini,
& Bayazi,
(2013)
Mashad,
Iran
Quasi-
experim
ent
45 CHD
patients
with
depression
(18
female, 27
male), age
40-65 y,
divided
into:
Relaxatio
n group
Meditatio
n group
Control
group
• Relaxation
group: 10
sessions of
Jacobson’s
progressive
muscle
relaxation,
@20-25 min, 3
times a day
with an
educational
CD.
• Meditation
group: 10
sessions of
mindfulness
meditation
technique,
@20-25 min, 3
times a day
with an
educational
CD.
Standa
rd
interv
ention
.
Depressio
n, systolic
blood
pressure,
diastolic
blood
pressure,
heart rate,
and
anxiety.
• Significant
reduction in
depression, BP
(systolic and
diastolic) and HR
in meditation
group.
• No significant
difference in BP,
HR, anxiety and
depression
between groups.
• A significant
reduction in
depression scores
of meditation
compared to
control group.
5. Ikedo,
Gangahar,
Quader &
Smith
(2007)
The USA
RCT 78 CHD
patients
underwent
cardiac
surgery,
divided
into:
Relaxatio
n group
(n=27)
Prayer
group
(n=24)
Control
group (n =
27
)
Given
headphones
connected to a
CD player: 1
group listened
to prayer during
the surgery, the
other listened to
relaxation
technique.
Placeb
o
Tension/a
nxiety,
depression
, anger,
No difference on all
aoutcome measures
6. Kim, Cho,
& Cho
(2017)
Busan,
Korea
Prospect
ive
cohort
34 female
patients,
mean age
52 with
microvasc
ular
angina.
• Mindfullness-
based stress
reduction for 8
consecutive
weeks,
comprises 2.5
hour weekly
practice of
mindfulness
training, body
scan, sitting
meditation, and
hatha yoga),
education (15-
30 persons of
group learning),
and 1 hour
daily practice
(meditation,
yoga, and
awareness
Baseli
ne
value
Endotheli
al
function,
Left
ventricula
r function,
reactive
brachial
flow-
mediated
dilatation.
Emotional
stress.
Mindfulness based
stress reduction
reduces all stress
parameters
(somatization,
phobic anxiety,
paranoid ideation,
and psychoticism)
except hostility,
systolic BP and
endothelial and
myocardial
function.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
398
training).
• Anti-anginal
medication.
7. Lukman,
Akbar, &
Ibrahim
(2012)
Indonesia
Quasi
experim
ent
42 adult
with ACS
Zikr asmaul
husna (Islamic
spiritual
mantram of the
God’s Holy
names) repeat
several times a
day.
None Anxiety Significant
reduction of anxiety
level.
8. Robert
McComb,
Tacon,
Randolph,
& Caldera,
(2004)
The USA
RCT 18 women
(mean age
60 years)
with
angina,
CHF,
hypertensi
on and
valve
disorder.
• Mindfulness
based stress
reduction
program: 2 h at
night each
week over 8 w
consisted of the
body scan,
sitting
meditation, and
hatha yoga.
• Additional
experential
learning
regarding stress
responses.
Wait
list
Stress
hormones,
sub-
maximal
stress
response
&
physical
functionin
g.
No significant main
effect or interaction
for the stress
hormones and
submaximal stress
response.
There was
significant effect
between group for
ventilation and
breathing
frequency.
9. Manchanda
et al. (2000)
India
RCT 42 men
with
angiograp
hically
proven
coronary
artery
disease
(CAD)
divided
equally to
treatment
and
control
g
rou
p
.
Yoga, control of
risk factors, diet
control and
moderate
aerobic exercise
1 year follow
up.
Standa
rd
care:
risk
factor
contro
l and
AHA’
s step
I diet
Number
of angina
attacks,
lipid
profile,
exercise
capacity,
body
weight.
Significant different
in all parameters
10. Momeni,
Omidi,
Raygan, &
Akbari
(2016)
Kashan,
Iran
RCT,
single
blind
60 cardiac
patients
8 of 2.5 h
sessions of
MBSR
comprises
structured
educational
program and
formal
meditation
(mindful body
scan, sitting
meditation,
walking
meditation, and
yoga).
Standa
rd
interv
ention
, no
psych
ologic
al
interv
ention
.
BP,
perceived
stress,
anger
measured
at pre and
post
interventi
on.
MBSR significantly
reduced anxiety,
stress, anger,
systolic BP.
Mind-Body-Spiritual Care for Coronary Heart Disease Patients
399
11. Mufarokhah
, Putra, &
Dewi (2016)
Indonesia
Quasy
experim
ent
Pre-post
test
28 ACS
patients
5 sessions of
health education
2x/w @ 30 m,
followed by
individual
counselling at
patients’ home
for 1 wee
k
.
None Coping,
medicatio
n
adherence.
Significant
difference for
coping and
medication
adherence.
12. Nyklíček,
Dijksman,
Lenders,
Fonteijn, &
Koolen
(2014)
The
Netherlands
RCT 114 adults
(94 male
and 20
female),
mean age
of 55 y.o
patient
underwent
primary
coronary
interventi
on.
• A brief
mindfulness
training: 90–
120 m weekly:
(1) psycho-
education: role
of behavior,
bodily
sensations,
emotions, and
thoughts (2)
psycho-
education: role
of mindfulness
and non-
judgmental
acceptance in
stress reduction,
(3) mindfulness
practices
(4) discussion of
one’s
experiences
while doing the
practices.
• Dail
y
p
ractice
Self-
help
bookle
t
Anxiety,
depression
, stress,
vitality,
mindfulln
ess.
No significant
effect on stress &
anxiety, depression,
and vitality.
Significant effect
on psychological
QOL, but not the
physical QOL.
13. Parswani,
Sharma, &
Iyegar
(2013)
Bangalore,
India
RCT 30 male
CHD
patients
allocated
randomly
to MBSR
and
control
group
• MBSR: 1-
1.5h/w for 8
respective
weeks of
mindfulness
meditation.
• 30 m daily
exercise of
mindfulness
meditation and
body scan
meditation,
guided by audio
cassette with
recorded
instruction.
• Instructed to
maintain health
behavior, i.e.
regular
exercise, diet.
Usual
treatm
ent:
Instru
cted to
mainta
in
health
behavi
or, i.e.
regula
r
exerci
se,
and
mainta
in
diet.
Hospital
anxiety
and
depression
, stress,
BP, BMI
measure at
pre, post-
test and 3
months
follow up.
Significant
reduction of
anxiety, depression,
BMI, systolic BP.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
400
14. Schneider et
al., (2012)
Fairfield,
Iowa, The
USA
RCT 201 black
CHD
patients of
both sexes
with
angiograp
hic
evidence
of
coronary
artery
stenosis.
• A 7-step
course
instruction:
1.5-2-h of
transcendenta
l meditation.
• Transcendent
al meditation:
20 m twice a
day.
• Follow up
and
maintenance
meetings up
to average of
5.4 years
Cardio
vascul
ar
health
educat
ion 20
m a
day
heart-
health
y
behavi
or.
Time to
first
mortality
BP
psychosoc
ial stress
factors;
and
lifestyle
behaviors.
Significant
reduction of
mortality risk, MI,
and stroke in CHD
patients. These
changes were
associated with
lower BP and
psychosocial stress
factors.
15. Stein et al.
(2010)
The USA
RCT 43 CABG
or CABG
plus valve
replaceme
nt
patients:
TG
(n=25)
divided
into 2
groups: 14
in the
guided
imagery
group, 11
in the
music-
only
group, CG
(n=18)
Asked to listen
to audiotapes at
least once a day,
every day, for 1
week
throughout the
preoperative
preparation and
more often if
they desired and
intraoperatively,
and again 6
months
postoperatively.
Standa
rd
care
Anxiety,
depression
, mood
disturbanc
e, anger,
fatigue,
confussio
n, and
bewilderm
ent.
No significant
difference in post
operative or 6
month follow up of
any aoutcome
measures.
16. Tacón,
McComb,
Caldera, &
Randolph
(2003)
The USA
RCT 18 heart
disease
women
(angina,
hypertensi
on, valve
disorder).
Kabat-Zinn's
mindfulness-
based stress
reduction
program: 2 h
per week plus
additional
homework
practice for
respective 8
weeks.
Wait
list
contro
l
Anxiety,
emotional
control,
coping
styles, and
health
locus of
control.
Significant
reduction of
anxiety, emotional
control and coping.
17. Warber et
al. (2011)
Michigan,
the USA
RCT
58 ACS
patients
with
depression
, recruited
from
advertise
ment and
enrolled,
41 of
which
completed
the
• Four day
workshop:
Group 1: A
spiritual
retreat
(imagery,
meditation,
drumming,
journal
writing, and
nature-based
activities).
Group 2:
Standa
rd
care
Depressio
n, spiritual
well-
being,
perceived
stress, and
hope.
Depression was not
significantly
different among
groups, hope was
significantly higher
in the intervention
group.
Mind-Body-Spiritual Care for Coronary Heart Disease Patients
401
Note: ACS: Acute coronary syndrome, AHA: American Heart Association, BP : Blood pressue, CHD:
coronary heart disease, HR: heart rate, h: hour(s), m: minute(s), MBSR: Mindfulness-based stress reduction
program, MI: myocardial infarction, w: week(s), y: year(s).
3.3 Outcomes
Most studies have proven the effectiveness of the
interventions included in the systematic review,
including psychological or biological parameters.
The positive psychological results reported in the
studies were reducing anxiety, depression, stress
(Bakara et al., 2013; Carneiro et al., 2017; Delui,
Yari, Khouyinezhad, Amini & Bayazi, 2013; Ikedo,
Gangahar, Quader & Smith, 2007; Lukman, Akbar
& Ibrahim, 2012; Momeni, Omidi, Raygan &
Akbari, 2016a; Nyklíček, Dijksman, Lenders,
Fonteijn & Koolen, 2014; Parswani, Sharma &
Iyegar, 2013; Stein et al., 2010; Tacón, McComb,
Caldera & Randolph, 2003; S L Warber et al., 2011),
increasing psycho-spiritual comfort (Bakar, 2017),
coping (Mufarokhah, Putra & Dewi, 2016), spiritual
wellbeing (Warber et al., 2011), and anger,
confusion, fatigue (Ikedo et al., 2007) and hope
(Warber et al., 2011). The reported positive
biological parameters include stress hormones
(Robert McComb, Tacon, Randolph & Caldera,
2004), hemodynamic parameters (Carneiro et al.,
2017; Delui et al., 2013; Momeni et al., 2016a;
Parswani et al., 2013), myocardial infarction attack
and cardiac revascularization (Schneider et al.,
2012) and cardiovascular function (Kim et al.,
2013).
4 DISCUSSION
To the best of our knowledge, this is the first
systematic review of mind, body and spiritual
nursing care aimed at improving CHD patients’
mind, body, and spiritual wellness. This systematic
review followed the PRISMA statement as a
guideline in conducting the systematic review.
Seventeen articles from 16 studies were included in
the review.
This review confirmed the findings of previous
systematic reviews assessing psychological
intervention both for a healthy or sick individual of
various medical conditions that for mindfulness
alone, mind-body combination, mindfulness or
spiritual intervention alone or in combination
showed positive results for CHD patients with
various conditions (perioperative, hospitalized, at
home).
The strengths of the studies included in the
review were the clarity of reporting in terms of the
intervention provided for the respondents and the
ability for the examination of the study quality by
the authors.
Despite the aforementioned strengths of the
studies under review, there are some weaknesses of
the available studies, specifically the study designs
and the types of intervention given to the patients
under study.
Only eleven of 17 articles included in the review
employed the research design of randomized control
trial (RCT). Because the reviewed studies examine
the effectiveness of an intervention or group of
interventions, the most appropriate study design is
RCT; another study design may lead to bias because
the maturation effect cannot be examined. Not all
reviewed papers used a control group. This may lead
to outcome bias because it cannot be compared with
others.
Another issue is the rigorous approach to
conducting and analyzing findings of the studies.
Some RCT studies failed to conceal from the
respondents, or the investigators, or both, the group
treatment
course.
Lifestyle
Change
Program
(nutritional
education,
exercise, and
stress
management).
• Bi-weekly
follow up
phone calls-3
consecutive
months.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
402

to which the respondents had been allocated. This
may lead the investigator to tend to overestimate the
effect of the treatment. The small sample size used
in some studies (Bakar, 2017; Mufarokhah et al.,
2016; Robert-McComb et al., 2004; Tacón et al.,
2003) also poses a generalizability issue of the
studies’ findings. It was difficult to specify the
correct number for a sample size because the authors
did not report the power calculation to set the sample
size used in their studies.
Among the studies that used a comparator group,
some used a placebo, a standard treatment group, a
self-help intervention, and a waitlist. The standard
treatment group is the best choice for the type of
intervention (related to mind-body or mind-body-
spiritual) because it is ethically acceptable and
appropriate to the CHD patients. The use of a
waitlist as control group (Robert-McComb et al.,
2004; Tacón et al., 2003) may also carry the
potential for bias because the author might
overestimate the effect size, the other problem with
waitlist control is that the generalizability of the
study is limited only to the population who agreed to
wait for the intervention.
Finally, determining what is and is not a mind-
body-spiritual nursing care is impossible because
there is no study that demonstrates the
comprehensive mind, body, spiritual nursing care
found to be reviewed.
4.1 Implication for Practice
This systematic review enabled us to conclude on a
specific nursing intervention addressing mind, body,
and spiritual issues experienced by CHD patients
due to the limited supporting evidence gathered from
the review.
4.2 Implication for Research
Further study to examine a nursing care that is
tailored to address CHD patients’ mind, body, and
spiritual issues is warranted.
4.3 Limitation
The limitations of this systematic review related to
the study quality. Some reviewed studies failed to
report the randomization process, the blinding
process or others.
4.4 Conflict of Interest
The authors declare that there is no conflict of
interest.
5 CONCLUSIONS
The study examined a comprehensive mind, body,
and spiritual nursing care for CHD patients that is
yet available. Although all reviewed papers reported
positive results, there were a wide variety of
interventions provided by various professionals,
making it difficult to conclude on a certain nursing
care model and its effectiveness for the CHD
patients.
Further study is required to develop the best
nursing care model for coronary heart disease
patients and to examine its effectiveness in
alleviating patients’ issues.
REFERENCES
Abbott, R. A., Whear, R., Rodgers, L. R., Bethel, A.,
Thompson Coon, J., Kuyken, W., … Dickens, C.
(2014). Effectiveness of mindfulness-based stress
reduction and mindfulness based cognitive therapy in
vascular disease: A systematic review and meta-
analysis of randomised controlled trials. Journal of
Psychosomatic Research, 76(5), 341–351.
https://doi.org/10.1016/j.jpsychores.2014.02.012
Abu-El-Noor, M. K., & Abu-El-Noor, N. I. (2014).
Importance of Spiritual Care for Cardiac Patients
Admitted to Coronary Care Units in the Gaza Strip.
Journal of Holistic Nursing, 32(2), 104–115.
https://doi.org/10.1177/0898010113503905
Bakar, A. (2017). Pengembangan Model Asuhan
Keperawatan (Caring) Islami Terhadap Nyaman
Psikospiritual Pada Pasien Jantung Koroner. PhD
Thesis. Universitas Airlangga.
Bakara, D. M., Ibrahim, K., Sriati, A., Bengkulu, P. K.,
Keperawatan, F., & Padjadjaran, U. (2013). Efek
Spiritual Emotional Freedom Technique terhadap
Cemas dan Depresi , Sindrom Koroner Akut Effect of
Spiritual Emotional Freedom Technique on Anxiety
and Depresseion in Patients with Acute Coronary
Syndrome. Padjajaran Nursing Journal, 1(April
2013), 48–55.
Best, M., Butow, P., & Olver, I. (2015). Do patients want
doctors to talk about spirituality? A systematic
literature review. Patient Education and Counseling,
98(11), 1320–1328.
https://doi.org/10.1016/j.pec.2015.04.017
Bluvstein, I., Moravchick, L., & Sheps, D. (2013).
Posttraumatic Growth , Posttraumatic Stress
Mind-Body-Spiritual Care for Coronary Heart Disease Patients
403

Symptoms and Mental Health Among Coronary Heart
Disease Survivors, 164–172.
https://doi.org/10.1007/s10880-012-9318-z
Carneiro, É. M., Barbosa, L. P., Marson, J. M., Terra, J.
A., Martins, C. J. P., Modesto, D., … Borges, M. de F.
(2017). Effectiveness of Spiritist “passe” (Spiritual
healing) for anxiety levels, depression, pain, muscle
tension, well-being, and physiological parameters in
cardiovascular inpatients: A randomized controlled
trial. Complementary Therapies in Medicine, 30, 73–
78. https://doi.org/10.1016/j.ctim.2016.11.008
Clark, P. A., Drain, M., & Malone, M. P. (2003).
Addressing patients’ emotional and spiritual needs.
Joint Commission Journal on Quality and Safety,
29(12), 659–670. https://doi.org/10.1016/S1549-
3741(03)29078-X
Delui, M. H., Yari, M., Khouyinezhad, G., Amini, M., &
Bayazi, M. . (2013). Comparison of Cardiac
Rehabilitation Programs Combined with Relaxation
and Meditation Techniques on Reduction of
Depression and Anxiety of Cardiovascular Patients.
The Open Cardiovascular Medicine Journal, 7(1), 99–
103. https://doi.org/10.2174/1874192401307010099
Elliot, D., Aitken, L. M., & Chaboyer, W. (2007).
ACCCN’s Critical Care Nursing. Marrickville:
Elsevier Australia.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How
do mindfulness-based cognitive therapy and
mindfulness-based stress reduction improve mental
health and wellbeing? A systematic review and meta-
analysis of mediation studies. Clinical Psychology
Review, 37, 1–12.
https://doi.org/10.1016/j.cpr.2015.01.006
Guyatt, G. ., Sackett, D. ., & Cook, D. . (1993). Users’
guide to the Medical Literature: II. How to Use an
Article About Therapy or Prevention: A. Are the
Results of the Study Valid. The Journal of the
American Medical Association, 270(21), 2598–2601.
Guyatt, G. ., Sackett, D. ., & Cook, D. . (1994). Users’
Guides to the Medical Literature: II. How to Use an
Article About Therapy or Prevention: B. What were
the Results and Will They Help Me in Caring for My
Patients? The Journal of the American Medical
Association, 271(1), 59–63.
Ikedo, F., Gangahar, D., Quader, M., & Smith, L. (2007).
The effects of prayer, relaxation technique during
general anesthesia on recovery outcomes following
cardiac surgery. Complementary Therapies in Clinical
Practice, 13(2), 85–94.
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C.
(2015). Mindfulness-based stress reduction for healthy
individuals: A meta-analysis. Journal of
Psychosomatic Research, 78(6), 519–528.
https://doi.org/10.1016/j.jpsychores.2015.03.009
Kim, B. J., Cho, I. S., & Cho, K. I. (2017). Impact of
mindfulness based stress reduction therapy on
myocardial function and endothelial dysfunction in
female patients with microvascular angina. Journal of
Cardiovascular Ultrasound, 25(4), 118–123.
https://doi.org/10.4250/jcu.2017.25.4.118
Kim, S. H., Schneider, S. M., Bevans, M., Kravitz, L.,
Mermier, C., Qualls, C., & Burge, M. R. (2013).
PTSD symptom reduction with mindfulness-based
stretching and deep breathing exercise: Randomized
controlled clinical trial of efficacy. Journal of Clinical
Endocrinology and Metabolism, 98(7), 2984–2992.
https://doi.org/10.1210/jc.2012-3742
Kurniawati, N. ., Nursalam, & Suharto. (2017). Mind-
Body-Spiritual Nursing Care in Intensive Care Unit. In
Advances in Health Sciences Research: 8th
International Nursing Conference (Vol. 3, pp. 223–
228). Amsterdam: Atlantis Press.
Lukman, R., Akbar, M., & Ibrahim, K. (2012). Pengaruh
Intervensi Dzikir Asmaul Husna Terhadap Kecemasan
Klien Sindroma Koroner Akut di RSUP Dr.
Mohammad Hosein Palembang. Unpad Repository.
Retrieved from
http://lukmanrohimin.blogspot.com/2012/01/pengaruh
-intervensi-zikir-asmaul-husna.html
Manchanda, S., Narang, R., Reddy, K., Sachdeva, U.,
Prabhakaran, D Dharmanand, S., Rajani, M., &
Bijlani, R. (2000). Retardation of coronary
atherosclerosis with yoga lifestyle intervention. The
Journal of the Association of Physicians of India,
48(7), 687–694.
Miller, G. E., Freedland, K. E., Carney, R. M., Stetler, C.
A., & Banks, W. A. (2003). Cynical Hostility,
Depressive Symptoms, and the Expression of
Inflammatory Risk Markers for Coronary Heart
Disease. Journal of Behavioral Medicine, 26(6), 501–
515. https://doi.org/10.1023/A:1026273817984
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G.,
Altman, D., Antes, G., … Tugwell, P. (2009).
Preferred reporting items for systematic reviews and
meta-analyses: The PRISMA statement. PLoS
Medicine, 6(7). https://doi.org/ 10.1371/
journal.pmed.1000097
Momeni, J., Omidi, A., Raygan, F., & Akbari, H. (2016a).
The effects of mindfulness-based stress reduction on
cardiac patients’ blood pressure, perceived stress, and
anger: a single-blind randomized controlled trial.
Journal of the American Society of Hypertension,
10(10), 763–771.
https://doi.org/10.1016/j.jash.2016.07.007
Momeni, J., Omidi, A., Raygan, F., & Akbari, H. (2016b).
The effects of mindfulness-based stress reduction on
cardiac patients’ blood pressure, perceived stress, and
anger: a single-blind randomized controlled trial.
Journal of the American Society of Hypertension,
10(10), 763–771.
https://doi.org/10.1016/j.jash.2016.07.007
Mufarokhah, H. M., Putra, S., & Dewi, Y. (2016). Self
Management Program Meningkatkan Koping, Niat
dan Kepatuhan Berobat Pasien PJK Setelah Pemberian
Self Management Program. Jurnal NERS, 11(1), 56.
https://doi.org/10.20473/jn.V11I12016.56-62
Nyklíček, I., Dijksman, S. C., Lenders, P. J., Fonteijn, W.
A., & Koolen, J. J. (2014). A brief mindfulness based
intervention for increase in emotional well-being and
quality of life in percutaneous coronary intervention
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
404

PCI) patients: The MindfulHeart randomized controlled
trial. Journal of Behavioral Medicine, 37(1), 135–144.
https://doi.org/10.1007/s10865-012-9475-4
Parswani, M. ., Sharma, M. ., & Iyegar, S. . (2013).
Minfulness-based stress reduction program in
coronary heart disease: a randomized control trial.
Internation Journal of Yoga, 6(2), 111–117.
Robert McComb, J. J., Tacon, A., Randolph, P., &
Caldera, Y. (2004). A Pilot Study to Examine the
Effects of a Mindfulness-Based Stress-Reduction and
Relaxation Program on Levels of Stress Hormones,
Physical Functioning, and Submaximal Exercise
Responses. The Journal of Alternative and
Complementary Medicine, 10(5), 819–827.
https://doi.org/10.1089/acm.2004.10.819
Schneider, R. H., Grim, C. E., Rainforth, M. V., Kotchen,
T., Nidich, S. I., Gaylord-King, C., … Alexander, C.
N. (2012). Stress reduction in the secondary
prevention of cardiovascular disease: Randomized,
controlled trial of transcendental meditation and health
education in blacks. Circulation: Cardiovascular
Quality and Outcomes, 5(6), 750–758.
https://doi.org/10.1161/CIRCOUTCOMES.112.96740
6
Schulz, K. F., Altman, D. G., Moher, D., & Group, C.
(2010). CONSORT 2010 statement: updated
guidelines for reporting parallel group randomised
trials. PLoS Medicine, 7(3), e1000251.
https://doi.org/10.1371/journal.pmed.1000251
Stein, T., Olivo, E., Grand, S., Namerow, P., Costa, J., &
Oz, M. (2010). A pilot study to assess the effects of a
guided imagery audiotape intervention on
psychological outcomes in patients undergoing
coronary artery bypass graft surgery. Holistic Nursing
Practice, 24(4), 213–222.
https://doi.org/10.1097/HNP.0b013e3181e90303
Tacón, A., McComb, J., Caldera, Y., & Randolph, P.
(2003). Mindfulness meditation, anxiety reduction,
and heart disease: a pilot study. Family and
Community Health, 26(1), 25–33.
von Elm, E., Altman, D. G., Egger, M., Pocock, S. J.,
Gøtzsche, P. C., & Vandenbroucke, J. P. (2008). The
Strengthening the Reporting of Observational Studies
in Epidemiology (STROBE) statement: guidelines for
reporting observational studies. Journal of Clinical
Epidemiology, 61(4), 344–349.
https://doi.org/10.1016/j.jclinepi.2007.11.008
Warber, S. L., Ingerman, S., Moura, V. L., Wunder, J.,
Northrop, A., Gillespie, B. W., … Rubenfire, M.
(2011). Healing the heart: a randomized pilot study of
a spiritual retreat for depression in acute coronary
syndrome patients. Explore, 7(4), 222–233.
Warber, S. L., Ingerman, S., Moura, V. L., Wunder, J.,
Northrop, A., Gillespie, B. W., … Rubenfire, M.
(2011). Healing the Heart: a Randomized Pilot Study
of a Spiritual Retreat for Depression in Acute
Coronary Syndrome Patients. Explore
, 7(4), 222–233.
Yang, Y., Liu, Y. H., Zhang, H. F., & Liu, J. Y. (2015).
Effectiveness of mindfulness-based stress reduction and
mindfulness-based cognitive therapies on people living
with HIV: A systematic review and meta-analysis.
International Journal of Nursing Sciences, 2(3), 283–294
Mind-Body-Spiritual Care for Coronary Heart Disease Patients
405
