
Family Support for Better Self Care Behavior Patients with Type 2
Diabetes Mellitus
An Integrated Review
Made Mahaguna Putra, Kusnanto, Candra Panji Asmoro
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
Keywords : Diabetes Mellitus, Diabetes Management, Social Support, Family Support, Self Care Behavior.
Abstract : Diabetes mellitus is a serious disease in the world. Family support approach improving self-care behaviour
are important for diabetes management. The aims of this review are to identify family support for people
with diabetes mellitus from quantitative studies, and to examine and understanding self-care behaviour was
related with family support. A greater understanding of the strategies would help Indonesia nurses to
develop nursing systems for managing people with diabetes mellitus Methods: Multiple databases
(SCOPUS, MEDLINE and CINAHL) were searched for the period from 2008–2018 and
in the English article, We were reviewed the reference list of included studies and picked up additional
research. Results: This finding indicates that families are considered an important source of social support
for diabetic adults. Families positively affect the health of diabetic patients or interfere with or promote self-
care activities and alleviate the detrimental effects of stress on glycemic control. Conclusion: Self-care
behaviour can improved by family support. Family-based approach to chronic disease management is based
on family physical environment, diseases including educational, relational, and personal needs of patients
and families were emphasized.
1 BACKGROUND
Common chronic disorder of adults patients is Type
2 diabetes mellitus (T2DM). Over the last 5 years
the prevalence of diabetes in adults over the past 30
years has increased from 14.9% to 20.8% over the
past five years. T2DM is a disorder disease that
results in cognitive dysfunction and addiction, which
cause a significant burden on the healthcare and
social care resources. (Ishak et al., 2017).
Patients who are conducting education and
various management are essential to maintain
disruption and reduce complications. There is
significant evidence to support various interventions
to improve the outcome of diabetes. Diabetes self-
management is essential to reaching glycemic
manage and enhancing fitness effects (American
Diabetes Association, 2018). Self-management
refers back to the person’s capability to manage the
symptoms, treatment, physical and psycho
social outcomes and way of life changes inherent
to dwell with a persistent circumstance (Ishak et al.,
2017).
Effective self-management is crucial to adults
living with Type 2 diabetes. Self-management helps
maintain well-being and reduces the risk of
secondary complications, such as diabetic
retinopathy, cardiovascular diseases, peripheral
arterial disorder and amputation (Zhou et al., 2016).
Adherence to a diabetes self-management plan has
been associated with health literacy, motivation,
self-efficacy, mental health, and environmental
factors, such as social support and socio-economic
status (Ahola and Groop, 2013; Blackburn,
Swidrovich and Lemstra, 2013). A number of adults
with Type 2 diabetes report already receiving
diabetes-related support from family members
(Kovacs Burns et al., 2013; Nicolucci et al., 2016),
and many diabetes education interventions have
involved families in actively supporting adults living
with Type 2 diabetes with their self-management
plan (Hu et al., 2014; McElfish et al., 2015).
Lorig’s model for chronic disease self-
management (Lorig and Holman, 2003) and the
WHO framework for Innovative Care for Chronic
Conditions (World Health Organisation, 2002) both
identify that families and other social networks are
valuable in promoting positive health outcomes;
418
Putra, M., Kusnanto, . and Asmoro, C.
Family Support for Better Self Care Behavior Patients with Type 2 Diabetes Mellitus.
DOI: 10.5220/0008326104180427
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 418-427
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

however, neither conceptual model/framework
provides a clear explanation or theoretical basis for
how families can provide effective support.
Commonly cited theoretical models in previous
family-based interventions in diabetes are the Social
Cognitive and Family Systems Theory (Vongmany
et al., 2018) models; however, both of these models
focus on parent–child interactions or educator–
student interactions rather than adult–family
interactions (Schafer, McCaul and Glasgow, 1986;
Torenholt, Schwennesen and Willaing, 2014).
Some research have proven that a more level of
social assist correlates with better diabetes self-
management. Similarly, the international Diabetes
Federation confirms that terrible social help is a
predictor of terrible adherence to prescribe therapy.
This is steady with social cognitive concept,
emphasizing that self-management occurs in a
context that consists of formal healthcare vendors,
casual social community individuals and the bodily
environment (Schiøtz et al., 2011).
Most theories of health conduct exchange
required for diabetes self care performance include a
social help element (Tillotson and Smith, 1996;
Osborn and Egede, 2010), and family participants
are considered a significant source of social help for
adults with diabetes. Own family contributors can
provide many sorts of social guide (e.g., emotional,
informational, and appraisal support), instrumental
help (i.e., observable movements that make it
possible or less difficult for a man or woman to
perform wholesome behaviors) has been most
strongly associated with adherence to self
care behaviors throughout chronic diseases
(Dimatteo, 2004). In spite of correlation evidence
helping the importance of instrumental help,
interventions not often target own family support as
a way of promoting diabetes self
care behaviours between adults. Most diabetes
intervention trials have a look at the effect of
character education on glycemic manage, without
attractive or instructing own family contributors or
accounting for member of the family aid as a method
outcome (Norris, Engelgau and Narayan, 2001).
There were few interventions for adults with
diabetes including families, but that approach was
almost inconsistent and does not affect health
outcomes. Participants in the family intervention
reported a growth in own family individual
supportive behaviours and a lower in family
members’ nonsupportive behaviours.
Enhancements in self-reported diabetes self-
care behaviours, weight, and glycemic control have
been cited, although those found adjustments had
been no longer significant (Kang et al., 2010).
Gilliland et al. (GILLILAND et al., 2002) three -
arm intervention trial was conducted in adults and
relatives of diabetes, classes not participating in
one - to - one relatives who did not receive psycho
education, and American native community for
groups of operations. The intervention groups
established small will increase in glycemic control
relative to the manipulate group. Contributors have
been not randomized to condition, and the look at
did no longer verify the interventions’ outcomes on
diabetes self-care behaviours. Therefore, further
studies are needed to effectively perform family-
mediated therapy for adults with diabetes mellitus.
(Mayberry and Osborn, 2012).
Nonetheless, many qualitative and quantitative
observational studies have reported that families can
be influential on diabetes self-management (Weiler
and Crist, 2009; Guell, 2011; hu et al., 2013;
Samuel-Hodge et al., 2013; Oftedal, 2014; Choi et
al., 2015; Mayberry, Harper and Osborn, 2016), and
some have measured an association between family
behaviours and diabetes self-management (Epple et
al., 2003; Wen, Shepherd and Parchman, 2004;
Schiøtz et al., 2011; Sankar et al., 2015; Soto et al.,
2015). An examination of this evidence is required
to provide greater insights to optimize families’
involvement in diabetes self-management (Schafer,
McCaul and Glasgow, 1986; Inzucchi et al., 2012;
Torenholt, Schwennesen and Willaing, 2014; Baig et
al., 2015).
However, these reviews mainly focus on the
family support and self-care behaviour of diabetic
patients. It is important that nurses understand
family support for increase self-care behaviour
patient with diabetes. Identification of these family
behaviours as perceived by adults living with Type 2
diabetes, and how they affect self-management is an
important first step to designing better person-
centred self-management interventions involving
family members. The aim of the present review was
to identify the family support that have an impact on
patient with diabetes self-care behavior practices. By
understanding this strategy more deeply, Indonesian
nurses can develop a nursing system for behavior
management of diabetic patients and explore
research areas that need further investigation.
2 METHODS
This review was conducted as a Integrated Literature
Review, as described by (Souza and Carvalho,
2010). This type of review is a comprehensive
Family Support for Better Self Care Behavior Patients with Type 2 Diabetes Mellitus
419

methodological approach to the review and can
include experimental and non-experimental studies
to understand the phenomena analyzed. It also has a
wide range of purposes such as combining data from
theoretical and empirical literature, defining
concepts, reviewing theory and evidence, analyzing
methodological problems of specific topics.
Evidence-based practices support classification
systems according to the methodological approach
adopted based on research design such as: level 1
evidence from a result of meta-analysis of multiple
randomized controlled trials, level 2 of evidence
from individual studies such as experimental
design, for evidence from the quasi-experimental
research is level 3, descriptive (or non-experimental)
studies or adopts a qualitative approach has levels 4
for evidence, level 5 of evidence from case reports
or experience reports. According to healthcare
research and quality classification, Level 6 evidence
based on expert opinion (Burns, Rohrich and Chung,
2011).
Based on the subject matter studies were divided
into two categories. These were termed as study to
identify areas relating to family support and their
effectiveness, we selected reports on trials (e.g.
randomized clinical trials [RCT], quasi-experimental
design trials, and single group studies) and cross-
sectional studies that examined family support. We
aimed to identify the areas of strategies/
interventions for self-care behavior; we also selected
reports of qualitative research, through in-depth
interviews and descriptive studies, which explored
effective family support strategies for self-care
behavior.
Published work related to family support for
individuals with diabetes mellitus collected by
searching Scopus, Cinahl, and Medline web
database in Marh 2018. We searched abstracts and
titles of manuscripts written in English that were
published in the last 8 years (2008–2018) using key
words such as “family support”, AND “self-care
behavior”, AND diabetes management”, AND
“diabetes”, AND “nursing”. This search identified
159 reports.
Patients with type 2 or type 1 diabetes as the study
population ; they were written in English; They were
intervention studies for family support for diabetic
patients; they were descriptive studies exploring
patient preferences and evaluations of family
support strategies for self-care behaviour.
Published work was excluded if family support was
related to only glycemic control, it related to only
medication adherence, it related to only depressive
symptom, was not written in English; did not focus
on family support to self care behavior, was a scale
development study, case report with small sample
size (e.g. one or two cases;); or was a published
work review/opinion paper (n= 159). In the study
studied here, we examined the implementation of
family support for diabetic patients for self-
care behaviour and / or strategies for recognition as
effective diabetes management. We reviewed a
report focusing on self-care behaviour and other
variables on family support, participants,
instruments, survey research. These are reported
in Table 1.
3 RESULTS
3.1 Study Characteristics
Of the 159 studies reviewed, 11 met the criteria
for this study and were selected for further analysis.
The studies were conducted in the USA (n = 6), UK
(n = 1), Saudi Arabia (n = 1), Japan (n = 1),
Denmark (n = 1), and Malaysia (n = 1). There were
some kind of studies reported, such as RCT (n = 3),
quasi-experimental (n =1 ), descriptive studies (n =
6), and mixed method (n=1).
3.2 Effectiveness of Family Support
11 studies reported the effects of their family
support on self care behavior in individuals with
diabetes mellitus. Six studies found family support
interacting statistically significantly with self-
care behaviour. 2 studies reported that family
intervention statistically significantly made better
self care behavior.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
420
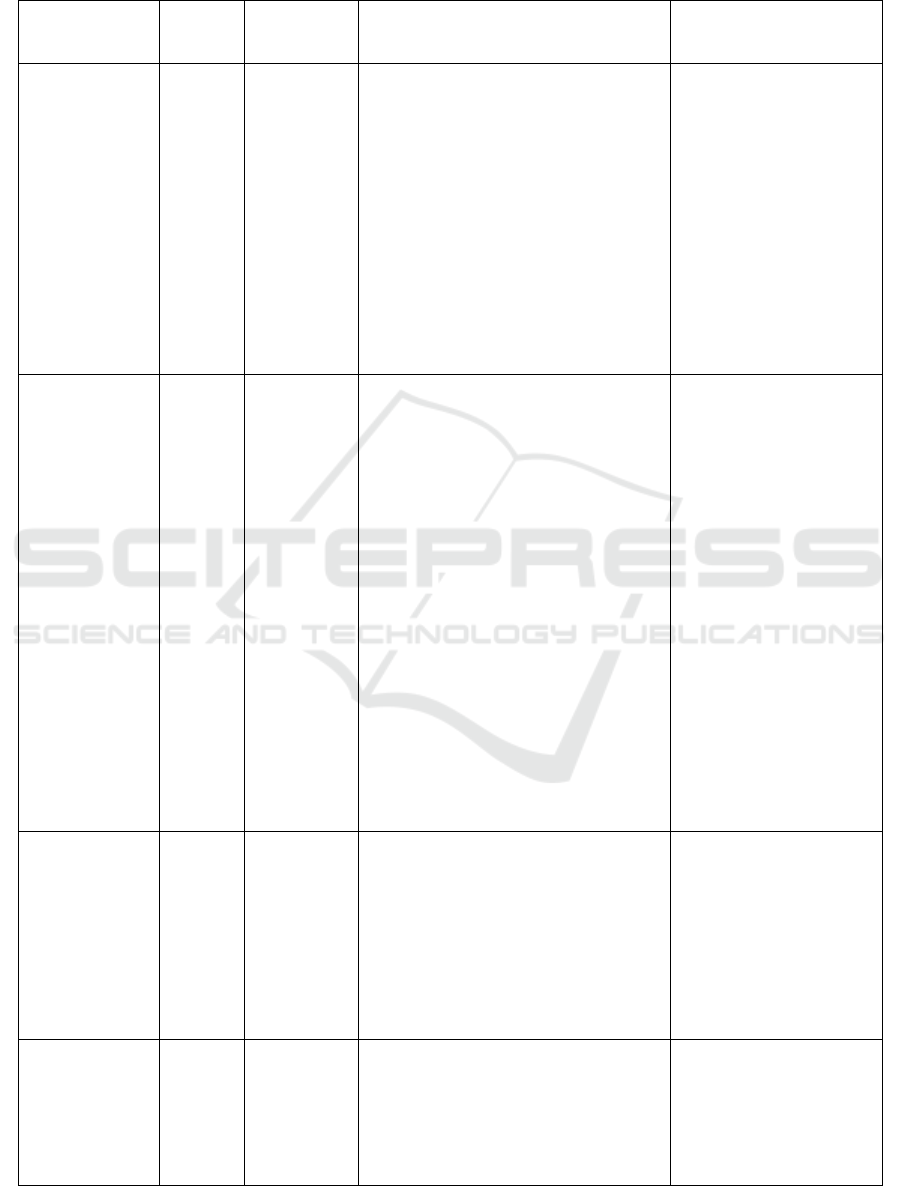
Table 1: Family support and self care bevavior.
(Author,
published year),
countr
y
Sample Design Instrument / Intervention of the study Main findings
(Herge et al.,
2012), USA
257
family
dyads
longitudinal
RCT
Background Information :
Demographic and medical information
were obtained through a 33-item
questionnaire developed by the research
team.
Family Organization : The 9 item
organization subscale from the Family
Environment Scale
Family Self-Efficacy : Diabetes Self-
Management Scale
Disease Management : The Diabetes
Behavior Rating Scale
Frequency of Blood Glucose Checks :
To assess frequency of Blood Glucose
checks
Family organizations with
metabolic controls
provide insight into the
potential pathway for
prevention / intervention
for better management of
diabetes.
(Ishak et al.,
2017), Malaysia
143
elderly
diabetes
patients
cross-
sectional
study
Diabetic characteristic section was
filled out by the investigator based on
the clinical history and medical records
of the patient.
Chronic kidney disease or neuropathy :
glomerular filtration rate (calculated
using Modified
Diet in Renal disease (MDRD)
equation)
Self-care practices among the elderly :
Malay Elderly Diabetes Self-Care
Questionnaire (MEDSCaQ)
Self-care Activity’ questionnaire :
Malay Version of the Morisky
Medication Adherence Scale (MMAS-
8)
Diabetes knowledge : The Malaysian
14-item version of the Michigan
Diabetes Knowledge Test (MDKT)
Depression : Malay version of the
geriatric Depression scale 14 (M-GDS-
14)
Family support were
significantly associated
with diabetes self-care in
elderly patients
(Watanabe et
al., 2010) Japan
112
with
type 2
diabetes
cross-
sectional
study
The questionnaire was originally
designed for evaluation of the effects of
Japanese family environment on out-
patient diet therapy and glycemic
control. Questionnaire items assessed
family diabetes enrollment, self
perception of diabetes nutritional
management, frequency and kind of
family support, and emotional response
to the support
Significant relationship
between the type of
nutritional support
(cooking or buying light
meals, advice or
encouragement) and
metabolic outcome.
(Schiøtz et al.,
2011), Denmark
2572
patients
with
Type 2
diabetes
cross-
sectional
study
Self-management behaviours :
Summary of Diabetes Self-care
Activities Scale
Patient activation : Patient Activation
Measure (PAM)
Emotional distress : ProblemAreas in
Diabetes scale (PAID-5)
Significant association
existed between poor
functional social network
and low frequency of foot
examinations (P =
0.0339)
Family Support for Better Self Care Behavior Patients with Type 2 Diabetes Mellitus
421
Social network : Structural and
functional aspects
Care received by participants : Patient
Assessment of Chronic Illness Care
(PACIC) scale
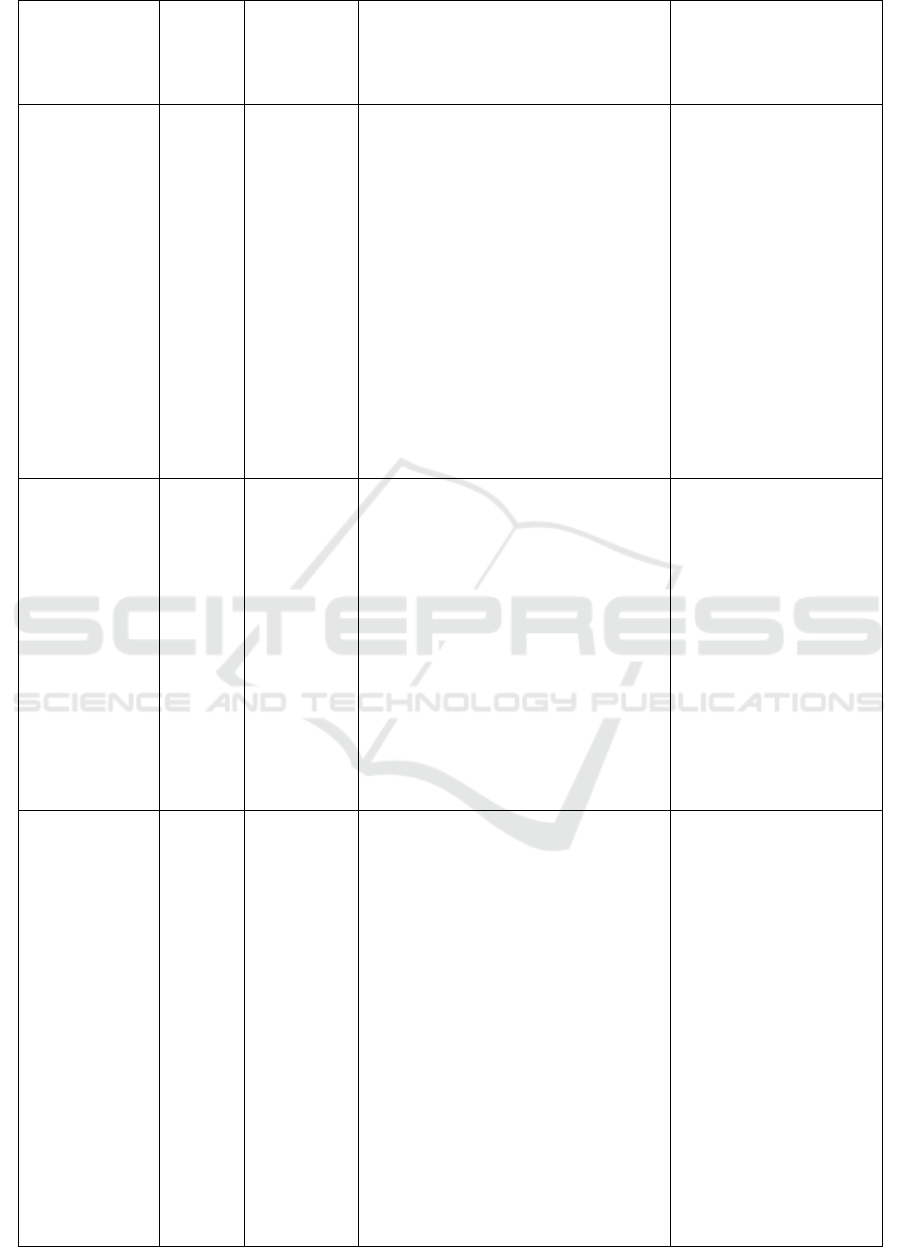
(Mayberry and
Osborn, 2012)
USA
Of those
eligible
who
consente
d to
participa
te (N =
75),
61% (n
=45)
attended
a focus
group
session
Mix method
(Qualitative
and
Quantitative
Family knowledge about diabetes
selfcare : assessed by asking
Family supportive and nonsupportive
behaviors : Diabetes Family Behavior
Checklist (DFBC)
Medication adherence : 12-item
Adherence to Refills and Medication
Scale (ARMS)
Glycemic control : the most recent
glycated hemoglobin (A1C) value in
the medical record
Perceiving family
members performed more
nonsupportive behaviors
was associated with being
less adherent to one’s
diabetes medication
regimen, and being less
adherent was associated
with worse glycemic
control. In focus groups,
participants discussed
family member support
and gave examples of
family members who
were informed about
diabetes but performed
sabotaging or
nonsu
pp
ortive behaviors.
(Murphy et al.,
2012) UK
305
adolesce
nts with
Type 1
diabetes
Randomized
trial
FACTS education programme
Biomedical measures : episodes of
severe hypoglycaemia, HbA1c was
measured every 3 months from baseline
Adolescent quality of life : Diabetes
Quality of Life Youth scale (DQOLY-
SF)
Adolescent well-being : World Health
Organization (WHO) Health Behaviour
in School Children (HBSC)
Diabetes management : Diabetes
Family Responsibility Questionnaire
(DFRQ)
Perception of their child’s diabetes
specific distress : Problem Areas in
Diabetes
(
PAID
)
scale
At 18 months there was
no significant difference
in HbA1C in either group
and no between-group
differences over time:
intervention group 75
mmol/ mol (9.0%) to 78
mmol / mol (9.3%),
control group 77 mmol/
mol (9.2%) to 80 mmol /
mol (9.5%). Adolescents
perceived no changes in
parental input at 12
months.
(Hu et al., 2014)
USA
Adult
patients
with
diabetes
(n = 36)
and
family
member
s (n =
37)
A quasi-
experimenta
l, 1 group
longitudinal
design.
Intervention : culturally tailored
diabetes educational program
Demographic forms : included family
history, health history, socioeconomic
information, and the number and
frequency of family members attending
the home visits and group meetings
Hemoglobin A1C : Bayer A1C NOW
kit
Fasting glucose and lipid profiles : A
Cholestech LDX machine (Alere, Inc.,
Waltham, MA)
Physical activity : Short International
Physical Activity Questionnaire (IPAQ)
Energy expenditure : estimated
metabolic equivalent task (MET)
Diet : Behavioral Risk Factor
Surveillance System (BRFSS)
Diabetes knowledge : Spoken
Knowledge in Low Literacy Patients
with Diabetes (SKILLD) scale.
A1C decreased by 4.9%
on average among
patients from pre-
intervention to 1 month
post-intervention. Patients
showed significant
improvements in systolic
blood pressure, diabetes
self-efficacy, diabetes
knowledge, and physical
and mental components of
health-related quality of
life.
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
422
Family support : Diabetes Family
Support Behavior Checklist (DFBC-II)
Diabetes self-efficacy : Stanford Self-
Efficacy Scale
Diabetes self-management : Summary
of Diabetes Self-Care Activities
(SDSCA)
Health-related quality of life : Health-
related quality of life
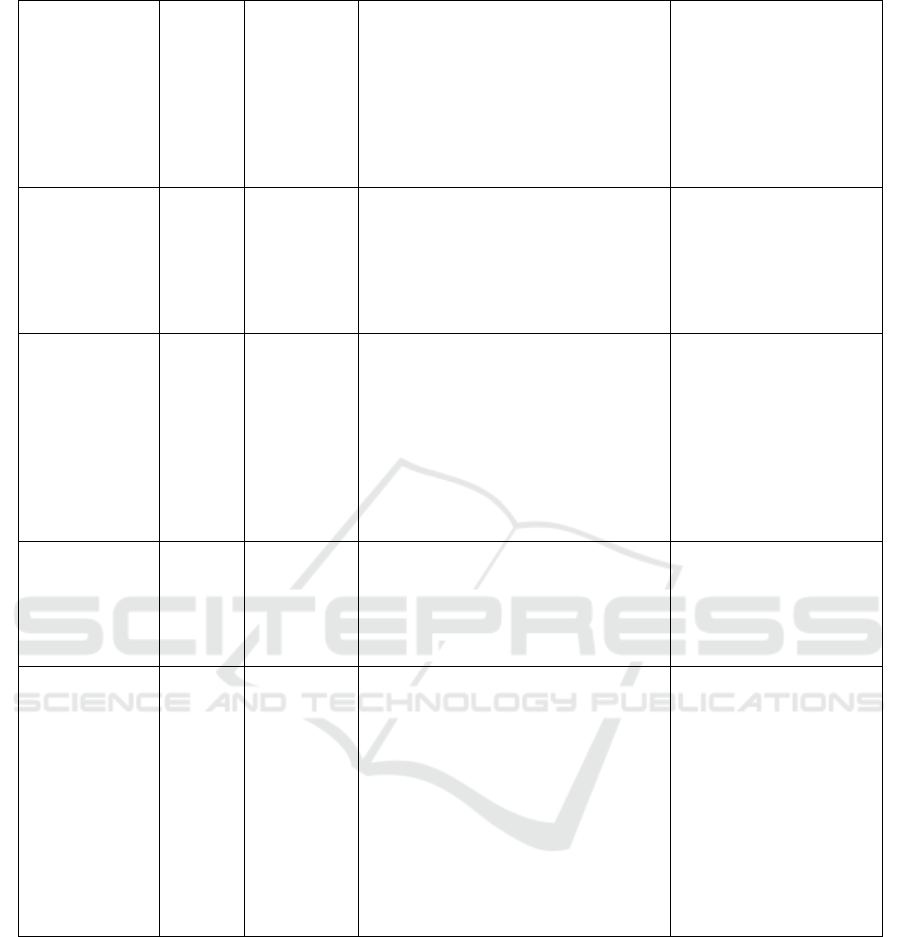
(Satterwhite and
Osborn, 2014)
USA
192
adults
with
type 2
diabetes
Cross-
sectional
study
Perceptions of family members’
supportive and obstructive behaviors :
Diabetes Family Behavior Checklist-II
(DFBC-II)
Self-care behaviors : Summary of
Diabetes Self-Care Activities (SDSCA)
Family members’
supportive and obstructive
behaviors were more
strongly related to
participants’ self-care and
explained more variation
(Aghili et al.,
2016) USA
380
adults
with
type 2
diabetes
Cross-
sectional
study
Clinical outcome variables : Total daily
calorie intake was assessed using a
single 24-hour recall.
Physical activity : International
Physical Activity Questionnaire
Diabetes self-care behaviour : self-
management profile for type 2 diabetes
A1C levels : ion exchange
chromatography (DS5 Analyzer, Drew
Scientific, Cumbria, United Kingdom)
Family and social support
was no independently
linked with A1C levels
(Badedi et al.,
2016) Saudi
Arabia
288
patients
with
T2DM
Cross-
sectional
study,
random
sample
All questionnaire created by an
interdisciplinary team from the Carver
College of Medicine, the College of
Pharmacy, and the College of Public
Health at the University of Iowa
Lower HbA1c levels
among patients who
received family support or
had close
relationship with their
p
h
y
sicians
(Song et al.,
2013) USA
83
middle-
aged
Kas
(Korean
America
ns) with
type 2
diabetes
Community
-based self-
help
intervention
program
with a
randomized
controlled
design.
Diabetes self-care activity : Summary
of Diabetes Self-Care Activities
(SDSCA).
Social support : social support
subscales of the Diabetes Care Profile
Self-efficacy : a modified form of the
Stanford Chronic Disease Self-efficacy
Scale
Unmet needs in social support was
created by summing the differences in
scores between social support needs
and the receipt of social support for
each of the 6 tasks.
Unmet needs for social
support are a significant
strong predictor of
inadequate type 2 diabetes
self-care activities, after
controlling for other
covariates.
4 DISCUSSION
This review provides insight into the diversity and
type of family behaviours that positively or
negatively affect diabetes self-management, for the
first time the "uncertain" family behavioral optimum
that diabetic patients can recognize as diabetic
patients Diabetes management barriers or promoters.
For example, some people welcomed this
information with reference to periodic reminders,
but others recognized this as "troubles",
strengthened non-compliance, and strengthened. If
this is correct, this interpretation is a window of
opportunity for intervention aimed at assisting
diabetes adults to recognize behaviors that are not
obvious and to help them become a facilitator, not a
self-management barrier.
We were reviewed published research which
examined the relationship between social support of
diabetes adults and self-care behaviour. Evidence of
beneficial effects of social support for self-care
behavior (multidimensional evaluation of family
support and social support) is emerging. Limited
evidence of being married with a partner was
Family Support for Better Self Care Behavior Patients with Type 2 Diabetes Mellitus
423

associated with worsening self-care behaviour. The
majority of statistical associations in the review were
significant. The main findings are the importance of
families in the management of type 2 diabetes. We
discovered that we believe that cooperating as a
couple with a common goal is supportive. It has
been shown that lack of support for patient self-care
behavior may interfere with patient efforts to
implement the necessary behavioral changes.
Much of a patient’s diabetes management takes
place within his/her family and social environment
(World Health Organisation, 2002). Addressing the
family environment for adults on diabetes is
important since this is the context in which the
majority of disease management occurs. Families as
two or more people who are somehow biologically,
legally and emotionally related defines family as two
or more people legally or emotionally related (Baig
et al., 2015). Thus, families may include nuclear,
extended, and relatives network members.
Family members can actively support and care
for patients with diabetes (CA et al., 2003). Most
individuals live within a household that has a great
influence on diabetes-management behaviors. A
survey of over 5000 adults with diabetes highlighted
the importance of improving well-being and self-
management by families, friends, colleagues
(Kovacs Burns et al., 2013). Family members are
often asked to share in the responsibility of disease
management. They can provide a variety of support
such as instrumental assistance to help patients to
appointment and help inject insulin, in overcoming
the illness of patients were assisted with social and
emotional support (Fisher et al., 1998; Wagner et
al., 2001). Through family communication and
attitudes, patients often have psychological well-
being, decisions to comply with medical
recommendations, and the ability to initiate and
maintain changes in diet and exercise often. Among
middle-aged and elderly people with type 2 diabetes,
long-term follow-up research reveals that
autonomous improvement of health status is related
to social support (Nicklett et al., 2013). Family unity
and family functions have also been found to be
positively correlated with patient self-care behaviour
and improvement in glycemic control (Griffith, Field
and Lustman, 1990; Walker et al., 2015).
Offering diabetes education only to patients with
type 2 diabetes may limit the effect on patients as
families may play a major role in disease
management. A family-based approach to chronic
disease management emphasizes the situation in
which the disease occurs, including family physical
environments, educational, relationship between
personal needs patient and family (Fisher et al.,
1998; Armour et al., 2005). Including family
intervention in educational intervention, support for
diabetic patients, development of healthy
family behaviours, self-management of diabetes (Hu
et al., 2014).
The self-management intervention of diabetes
can focus on family communication skills and may
need to teach positive ways to influence the patient's
health behaviour. Families may suffer from the
beloved person's diabetes (Fisher et al., 2002;
Gleeson-Kreig, Bernal and Woolley, 2002; Rosland
et al., 2010; Baig et al., 2015) knowledge on
diabetes is limited or I do not know how to support
loved ones (Carter-Edwards et al., 2001; Fisher et
al., 2002; Rosland et al., 2010; Keogh et al., 2011;
hu
et al., 2013). Family may also have
misunderstandings that they believe they know the
details of diabetes than they actually report, or They
do not understand the needs of family members in
diabetes management (Carter-Edwards et al., 2001;
White et al., 2009). The disease knowledge, the
strategy to change the family routine, the best way to
deal with the emotional side of the illness is part of
the self-management aspect of diabetes that the
family needs (Orvik, Ribu and Johansen, 2010).
Teaching families about the necessity of treating
diabetes will find out why these changes are
necessary, how to make these changes in the best
way, where to find additional information such as
healthy recipes and exercise routines By explaining
what to do. Effective family management can also
decrease the stress that families may experience
when dealing with a changing lifestyle or disease
progression (Baig et al., 2016). It is important to
provide family members with information about the
illness and possible treatment options, validate their
experiences as providers of support, helps to plan the
future and teaches some stress management skills
(Martire et al., 2010).
Carefully designed research is needed to evaluate
the benefits of diabetes self-management
intervention in patients and families (Martire, 2005).
How families manage chronic disease affects not
only the patient’s health, but the health of others in
the family as well (Fisher et al., 2002). Assessing
family members’ knowledge in diabetes self-care
and perceived ability to support their loved one with
diabetes may be important end points for diabetes
self-care interventions. Families may also be more
directly advantageous by relieving psychological
distress of beloved diabetes and by participating in a
health education program to improve their own
health behaviour (Trief et al., 2001; Fisher et al.,
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
424

2002; Sorkin et al., 2013). In addition, families with
high risk of diabetes may reduce the possibility of
developing diabetes due to improvement in lifestyle
habits and weight loss. In the review of randomized
controlled trials of chronic disease interventions, that
the benefits of families were scarcely evaluated
(Martire, 2005).
The knowledge of family support is essential for
diabetes management. This does not mean, that a
strong family relationship enhances family and
public compliance. The family dynamics described
in this review will not be restricted to diabetic
families, except for situations which are probably
caused by hypoglycemia. Therefore, our results are
potentially related to other chronically ill families
whose adherence to a particular lifestyle is
recommended. This is a potentially important
problem for future research.
5 CONCLUSIONS
We identified family support can improving self
care behavior. A family-based approach to chronic
disease management emphasizes the situation in
which the disease occurs, including family physical
environments, educational, relational, and patients
and families needs.
REFERENCES
. Aghili, R. et al. (2016) ‘Type 2 Diabetes : Model of
Factors Associated with Glycemic Control’, Canadian
Journal of Diabetes. Elsevier Inc., 40(5), pp. 424–430.
doi: 10.1016/j.jcjd.2016.02.014.
Ahola, A. J. and Groop, P. H. (2013) ‘Barriers to self-
management of diabetes.’, Diabetic medicine, 30(4),
pp. 413–420. doi: 10.1111/dme.12105.
American Diabetes Association (2018) ‘Introduction:
Standards of Medical Care in Diabetes—2018’,
Diabetes Care, 41(Supplement 1), pp. S1–S2. doi:
10.2337/dc18-Sint01.
American Diabetes Association (ADA) (2017) ‘Standard
of medical care in diabetes - 2017’, Diabetes Care, 40
(sup 1)(January), pp. s4–s128. doi: 10.2337/dc17-
S003.
Armour, T. A. et al. (2005) ‘The effectiveness of family
interventions in people with diabetes mellitus: a
systematic review.’, Diabetic Medicine, 22(10), pp.
1295–1305.
Badedi, M. et al. (2016) ‘Factors Associated with Long-
Term Control of Type 2 Diabetes Mellitus’, Journal of
Diabetes Research, 2016.
Baig, A. A. et al. (2015) ‘Family interventions to improve
diabetes outcomes for adults’, Annals of the New York
Academy of Sciences, 1353(1), pp. 89–112. doi:
10.1111/nyas.12844.
Baig, A. A. et al. (2016) ‘Family interventions to improve
diabetes outcomes for adults’, Ann N Y Acad Sci,
1353(1), pp. 89–112. doi: 10.1111/nyas.12844.Family.
Blackburn, D. F., Swidrovich, J. and Lemstra, M. (2013)
‘Non-adherence in type 2 diabetes: Practical
considerations for interpreting the literature’, Patient
Preference and Adherence, 7, pp. 183–189. doi:
10.2147/PPA.S30613.
Burns, P. B., Rohrich, R. J. and Chung, K. C. (2011) ‘The
levels of evidence and their role in evidence-based
medicine’, Plastic and Reconstructive Surgery,
128(1), pp. 305–310. doi:
10.1097/PRS.0b013e318219c171.
CA, C. et al. (2003) ‘Family predictors of disease
management over one year in Latino and European
American patients with type 2 diabetes.’, Family
Process, 42(3), p. 375–390 16p. Available at:
http://search.ebscohost.com/login.aspx?direct=true&d
b=c8h&AN=106692512&%5Cnlang=ja&site=eho
st-live.
Carter-Edwards, L. et al. (2001) ‘They Care But Don’t
Understand": Family Support of African American
Women With Type 2 Diabetes’, Diabetes Care, 24(3),
pp. 1144–1150.
Choi, S. E. et al. (2015) ‘Spousal Support in Diabetes
Self-Management Among Korean Immigrant Older
Adults’, Research in Gerontological Nursing, 8(2), pp.
94–104. doi: 10.3928/19404921-20141120-01.
Dimatteo, M. R. (2004) ‘Social Support and Patient
Adherence to Medical Treatment : A Meta-Analysis’,
Health Psychology, 23(2), pp. 207–218. doi:
10.1037/0278-6133.23.2.207.
Epple, C. et al. (2003) ‘The role of active family
nutritional support in Navajos’ type 2 diabetes
metabolic control’, Diabetes Care, 26(10), pp. 2829–
2834. doi: 10.2337/diacare.26.10.2829.
Fisher, L. et al. (1998) ‘The family and type 2 diabetes: a
framework for intervention.’, The Diabetes educator,
24(5), pp. 599–607. doi:
10.1177/014572179802400504.
Fisher, L. et al. (2002) ‘Depression and anxiety among
partners of European-American and Latino patients
with type 2 diabetes’, Diabetes Care, 25(9), pp. 1564–
1570. doi: 10.2337/diacare.25.9.1564.
GILLILAND, S. S. et al. (2002) ‘Strong in Body and
Spirit’, Diabetes Care, 25(1).
Gleeson-Kreig, J., Bernal, H. and Woolley, S. (2002) ‘The
role of social support in the self-management of
diabetes mellitus among a Hispanic population.’,
Public health nursing, 19(3), pp. 215–222. doi:
10.1046/j.0737-1209.2002.19310.x.
Griffith, L. S., Field, B. J. and Lustman, P. J. (1990) ‘Life
Stress and Social Support in Diabetes: Association
with Glycemic Control’, The International Journal of
Psychiatry in Medicine, 20(4), pp. 365–372. doi:
10.2190/APH4-YMBG-NVRL-VLWD.
Guell, C. (2011) ‘Diabetes management as a Turkish
family affair: Chronic illness as a social experience’,
Family Support for Better Self Care Behavior Patients with Type 2 Diabetes Mellitus
425

Annals of Human Biology, 38(4), pp. 438–444. doi:
10.3109/03014460.2011.579577.
Herge, W. M. et al. (2012) ‘Family and Youth Factors
Associated With Health Beliefs and Health Outcomes
in Youth With Type 1 Diabetes’, Journal of Pediatric
Psychology, 37(9), pp. 980–989.
hu, J. et al. (2013) ‘Perceptions of Barriers in Managing
Diabetes: Perspectives of Hispanic Immigrant Patients
and Family Members’, The Diabetes Educator, 39(4),
pp. 494–503. doi: 10.1177/0145721713486200.
Hu, J. et al. (2014) ‘A Family-Based Diabetes Intervention
for Hispanic Adults and Their Family’, The Diabetes
Educator, 40(1). doi: 10.1177/0145721713512682.
Inzucchi, S. E. et al. (2012) ‘Management of
hyperglycemia in type 2 diabetes: A patient-centered
approach’, Diabetes Care, 35(6), pp. 1364–1379. doi:
10.2337/dc12-0413.
Ishak, N. H. et al. (2017) ‘Diabetes self-care and its
associated factors among elderly diabetes in primary
care’, Journal of Taibah University Medical Sciences.
Elsevier Ltd, 12(6), pp. 504–511. doi:
10.1016/j.jtumed.2017.03.008.
Kang, C. et al. (2010) ‘Comparison of family partnership
intervention care vs . conventional care in adult
patients with poorly controlled type 2 diabetes in a
community hospital : A randomized controlled trial’,
International Journal of Nursing Studies. Elsevier Ltd,
47(11), pp. 1363–1373. doi:
10.1016/j.ijnurstu.2010.03.009.
Keogh, K. M. et al. (2011) ‘Psychological family
intervention for poorly controlled type 2 diabetes.’,
The American journal of managed care, 17(2), pp.
105–113.
Kovacs Burns, K. et al. (2013) ‘Diabetes Attitudes,
Wishes and Needs second study (DAWN2TM): Cross-
national benchmarking indicators for family members
living with people with diabetes’, Diabetic Medicine,
30(7), pp. 778–788. doi: 10.1111/dme.12239.
Lorig, K. R. and Holman, H. R. (2003) ‘Self-management
education: History, definition, outcomes, and
mechanisms’, Annals of Behavioral Medicine, 26(1),
pp. 1–7. doi: 10.1207/S15324796ABM2601_01.
Martire, L. M. (2005) ‘The“ Relative” Efficacy of
Involving Family in Psychosocial Interventions for
Chronic Illness: Are There Added Benefits to Patients
and Family Members?’, Families systems health,
23(3), p. 312. doi: 10.1037/1091-7527.23.3.312.
Martire, L. M. et al. (2010) ‘Review and meta-analysis of
couple-oriented interventions for chronic illness’,
Annals of Behavioral Medicine, 40(3), pp. 325–342.
doi: 10.1007/s12160-010-9216-2.
Mayberry, L. S., Harper, K. J. and Osborn, C. Y. (2016)
‘Family behaviors and type 2 diabetes: What to target
and how to address in interventions for adults with low
socioeconomic status’, Chronic Illness, 12(3), pp.
199–215. doi: 10.1177/1742395316644303.
Mayberry, L. S. and Osborn, C. Y. (2012) ‘Family
Support, Medication Adherence, and Glycemic
Control Among Adults With Type 2 Diabetes’,
Diabetes Care, 35(6), pp. 1239–1245. doi:
10.2337/dc11-2103.
McElfish, P. A. et al. (2015) ‘Family Model of Diabetes
Education With a Pacific Islander Community’, The
Diabetes Educator, 41(6), pp. 706–715. doi:
10.1177/0145721715606806.
Murphy, H. R. et al. (2012) ‘Education and Psychological
Issues Randomized trial of a diabetes self-
management education and family teamwork
intervention in adolescents with Type 1 diabetes’,
Diabetic Medicine, 29(8), pp. 249–254. doi:
10.1111/j.1464-5491.2012.03683.x.
Nicklett, E. J. et al. (2013) ‘Direct social support and long-
term health among middle-aged and older adults with
type 2 diabetes mellitus’, Journals of Gerontology,
Series B: Psychological Sciences and Social Sciences,
68(6), pp. 933–43. doi: 10.1093/geronb/gbt100.
Nicolucci, A. et al. (2016) ‘Diabetes Attitudes, Wishes
and Needs Second Study (DAWN2TM):
Understanding Diabetes-Related Psychosocial
Outcomes for Canadians with Diabetes’, Canadian
Journal of Diabetes, 40(3), pp. 234–241. doi:
10.1016/j.jcjd.2015.11.002.
Norris, S. L., Engelgau, M. M. and Narayan, K. M. V.
(2001) ‘Effectiveness of Self-Management Training in
Type 2 Diabetes A systematic review of randomized
controlled trials’, Diabetes Care, 24(3).
Oftedal, B. (2014) ‘Perceived support from family and
friends among adults with type 2 diabetes’, European
Diabetes Nursing July, 11(2), pp. 43–48. doi:
10.1002/edn.247.
Orvik, E., Ribu, L. and Johansen, O. E. (2010) ‘Spouses’
educational needs and perceptions of health in partners
with type 2 diabetes’, European Diabetes Nursing,
7(2), pp. 63–69. doi: 10.1002/edn.159.
Osborn, C. Y. and Egede, L. E. (2010) ‘Validation of an
Information-Motivation-Behavioral Skills model of
diabetes self-care (IMB-DSC)’, Patient Education and
Counseling, 79(1), pp. 49–54. doi:
10.1016/j.pec.2009.07.016.
Rosland, A. M. et al. (2010) ‘Family influences on self-
management among functionally independent adults
with diabetes or heart failure: Do family members
hinder as much as they help?’, Chronic Illness, 6(1),
pp. 22–33. doi: 10.1177/1742395309354608.
Samuel-Hodge, C. D. et al. (2013) ‘Family diabetes
matters: A view from the other side’, Journal of
General Internal Medicine, 28(3), pp. 428–435. doi:
10.1007/s11606-012-2230-2.
Sankar, U. V. et al.
(2015) ‘The adherence to medications
in diabetic patients in rural Kerala, India’, Asia-Pacific
Journal of Public Health, 27(2), p. NP513-NP523.
doi: 10.1177/1010539513475651.
Satterwhite, L. and Osborn, C. Y. (2014) ‘Family
involvement is helpful and harmful to patients ’ self-
care and glycemic control Suppor tive Behaviors
Obstru ctive Behaviors’, Patient Education and
Counseling. Elsevier Ireland Ltd, 97(3), pp. 418–425.
doi: 10.1016/j.pec.2014.09.011.
Schafer, L. C., McCaul, K. D. and Glasgow, R. E. (1986)
‘Supportive and nonsupportive family behaviors:
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
426

Relationships to adherence and metabolic control in
persons with type I diabetes’, Diabetes Care, 9(2), pp.
179–185. doi: 10.2337/diacare.9.2.179.
Schiøtz, M. L. et al. (2011) ‘Social support and self-
management behaviour among patients with Type 2
diabetes’, Diabetic Medicine, 29(5), pp. 654–661. doi:
10.1111/j.1464-5491.2011.03485.x.
Song, Y. et al. (2013) ‘Unmet Needs for Social Support
and Effects on Diabetes Selfcare Activities in Korean
Americans With Type 2 Diabetes’, Diabetes Educator,
38(1), pp. 77–85. doi:
10.1177/0145721711432456.Unmet.
Sorkin, D. H. et al. (2013) ‘Unidas por La Vida (United
for Life): Implementing A Culturally-Tailored,
Community-Based, Family-Oriented Lifestyle
Intervention’, Journal of Health Care for the Poor and
Underserved, 24(2), pp. 116–138. doi:
10.1353/hpu.2013.0103.
Soto, S. C. et al. (2015) ‘An Ecological Perspective on
Diabetes Self-care Support, Self-management
Behaviors, and Hemoglobin A1C Among Latinos’,
The Diabetes Educator, 41(2), pp. 214–223. doi:
10.1177/0145721715569078.
Souza, M. T. De and Carvalho, R. De (2010) ‘Integrative
review : what is it ? How to do it ? Revisão
integrativa : o que é e como fazer’, Einstein (São
Paulo), 8(1), pp. 102–106.
Tillotson, L. and Smith, M. (1996) ‘Locus of control,
social support, and adherence to the diabetes
regimen.\n’, Diabetes Education, 22(2), pp. 133–9.
Torenholt, R., Schwennesen, N. and Willaing, I. (2014)
‘Lost in translation-the role of family in interventions
among adults with diabetes: A systematic review’,
Diabetic Medicine, 31(1), pp. 15–23. doi:
10.1111/dme.12290.
Trief, P. M. et al. (2001) ‘The marital relationship and
psychosocial adaptation and glycemic control of
individuals with diabetes’, Diabetes Care, 24(8), pp.
1384–1389. doi: 10.2337/diacare.24.8.1384.
Vongmany, J. et al. (2018) ‘Family behaviors that have an
impact on the self-management activities of adults
living with Type 2 diabetes: a systematic review and
meta-synthesis’, Diabetic Medicine, 35(2), pp. 184–
194. doi: 10.1111/dme.13547.
Wagner, E. H. et al. (2001) ‘Improving chronic illness
care: Translating evidence into action’, Health Affairs,
20(6), pp. 64–78. doi: 10.1377/hlthaff.20.6.64.
Walker, R. J. et al. (2015) ‘Quantifying Direct Effects of
Social Determinants of Health on Glycemic Control in
Adults with Type 2 Diabetes’, Diabetes Technology &
Therapeutics, 17(2), pp. 80–87. doi:
10.1089/dia.2014.0166.
Watanabe, K. et al. (2010) ‘The Role of Family
Nutritional Support in Japanese Patients with Type 2
Diabetes Mellitus’, Internal Medicine, 49(11), pp.
983–989. doi: 10.2169/internalmedicine.49.3230.
Weiler, D. M. and Crist, J. D. (2009) ‘Diabetes self-
management in a latino social environment’, Diabetes
Educator, 35(2), pp. 285–292. doi:
10.1177/0145721708329545.
Wen, L. K., Shepherd, M. D. and Parchman, M. L. (2004)
‘Family Support, Diet, and Exercise Among Older
Mexican Americans With Type 2 Diabetes’, The
Diabetes Educator, 30(6).
White, P. et al. (2009) ‘Understanding type 2 diabetes:
Including the family member’s perspective’, Diabetes
Educator, 35(5), pp. 810–817. doi:
10.1177/0145721709340930.
World Health Organisation (2002) Innovative care for
chronic conditions: building blocks for action: global
report, World Health Organisation. Geneva: WHO.
Zhou, B. et al. (2016) ‘Worldwide trends in diabetes since
1980: A pooled analysis of 751 population-based
studies with 4.4 million participants’, The Lancet.
NCD Risk Factor Collaboration. Open Access article
distributed under the terms of CC BY, 387(10027), pp.
1513–1530. doi: 10.1016/S0140-6736(16)00618-8
Family Support for Better Self Care Behavior Patients with Type 2 Diabetes Mellitus
427
