
The Relationship between Healthy Housing Conditions and
Pulmonary Tuberculosis
Andri Setiya Wahyudi, Raufuddin and Ira Suarilah
Faculty of Nursing Universitas Airlangga, Kampus C Mulyorejo, Surabaya, Indonesia
Keywords: Healthy Housing Conditions, Behavior, Residential Density, Pulmonary Tuberculosis.
Abstract: Housing conditions are a factor that determine the state of hygiene and environmental sanitation. Housing
and environments that do not meet health requirements are risk factors regarding disease transmission, for
example, pulmonary tuberculosis. This research was conducted to determine the relationship between
healthy housing conditions and the incidence of tuberculosis in Palengaan, Pamekasan. This was an
observational study, based on its time and was a case-control study. Data analysis was conducted using a
Chi-square test with α = 0.05. This study assessed healthy housing conditions using the observation sheet
from the technical guidelines of the assessment regarding healthy housing conditions by the Directorate
General of Communicable Diseases Eradication and Environmental Health in 2002.The variables used,
resulting from the housing health assessment include: (a) house components; (b) sanitary facilities; and (c)
occupant behavior. Individual characteristics include: a) age; (b) gender; and (c) education, and residential
density. Based on the study results, the assessment for healthy housing conditions are associated with the
incidence of pulmonary TB; the Chi-square test indicated p = 0.000, OR = 35.10, and in three groups of
house health assessments, the behavior of occupants is associated with the incidence of pulmonary TB, with
the chi-square test p = 0.001, OR = 8.233. it can be concluded that houses with healthy conditions can
reduce the risk of pulmonary TB incidence and, in particular, poor behavior of occupants can increase the
risk of pulmonary TB incidence.
1 BACKGROUND
Public health is a science and the art of preventing
disease, prolonging life, and improving the
efficiency of life through efforts or attempts of
community organization. Community organization is
an effort to improve the environment and prevent
and combat contagious diseases. This is in line with
objectives for the prevention and improvement of
public health. The goal of public health is the whole
community, including individuals, families, and
groups both healthy and sick, especially those at
high risk in the community. Some special groups are
at risk and require supervision and guidance, for
example, patients with pulmonary tuberculosis.
Public health has basic components comprising of
humans, health (the healthy-sick concept), and the
environment.
Humans have needs that are continually evolving
and changing. Abraham Maslow in Mubarak (2009)
says that human needs are structured in a hierarchy
and the most basic needs (physiological) include
food, water, fresh air, temperature, free from illness,
rest, sleep, and activity. All these needs must be
prioritized, and a house is a means of manifestation
of these basic needs. This reflects work by Robert
Moroney in Mubarak (2009), who classifies human
needs and mentions houses as normative needs.
Human basic needs consist of food, clothing and
housing. Houses, also known as residences or homes
are a basic human needs. Every human being across
the world needs a place to live. The shape of housing
inhabited by each nation is different, and even in one
country or one city, housing can take various shapes.
Houses are become more varied; each component of
a house must fulfill health requirements, so the
inhabitants do not suffer hurt from any illness
(Azwar, 1995). The components of houses that
fulfill health requirements are expected to provide
comfort and can maintain the health of the
inhabitants; residents can avoid diseases, work
productively, and produce something meaningful.
Wahyudi, A., Raufuddin, . and Suarilah, I.
The Relationship between Healthy Housing Conditions and Pulmonary Tuberculosis.
DOI: 10.5220/0008330506570663
In Proceedings of the 9th International Nursing Conference (INC 2018), pages 657-663
ISBN: 978-989-758-336-0
Copyright
c
2018 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
657

The population of Indonesia is continually
increasing. In addition the population spread is
becoming more uneven, mainly because of the
urbanization that is becoming more rampant every
year. This rapid growth rate will automatically
increase the community's needs for shelter or
housing. With people’s increasing levels of need for
housing, this will increase the procurement of
housing in Indonesia, primarily in urban areas. This
has led to an increase in social problems and resulted
in a slum housing environment that does not meet
health requirements. Surabaya, which is also a
metropolitan city with rapid development and
becoming a common urbanization destination, is a
target of arising social problems. Problems arising
from the needs of the community needs to be
handled by the government immediately, including
the procurement of housing for the middle to lower
economic level of the community. According to the
United Nations Conference regarding the Problem of
the Human Environment (1972), more than 1 billion
people live below standard conditions and it is likely
that the situation will get worse in the future (WHO
SEARO, 1986; WHO Commission on Health and
Environment, 2001). The housing situation is a
factor that determines the condition of hygiene and
environmental sanitation. Overcrowding and narrow
housing results in high incidences of illness,
accidents, and other issues (Sukarni, 1995).
Based on the Household Health Survey (SKRT)
conducted in 1995 (DG PPM and PL, 2002), the 3rd
leading cause of death in Indonesia is tuberculosis.
Tuberculosis, commonly referred to as TB, is closely
related to unhealthy house sanitation conditions.
Meanwhile, according to the WHO report (2007) on
Global Tuberculosis Control Surveillance, Planning,
and Financing stated that Indonesia was ranked fifth
with the highest number of tuberculosis patients in
Southeast Asia after Bangladesh, Bhutan, DPR
Korea, and India.
WHO also reports that 10 to 20 million people
with tuberculosis in the world can transmit
tuberculosis. Because of pulmonary tuberculosis, the
mortality rate is around 3 million patients each year.
This situation is increasing and almost 75% are
found in low-socio-economic developing countries
(Alsagaaf, 2008).
The Annual Risk of Tuberculosis Infection
(ARTI) including the risk of transmission of
tuberculosis infection in Indonesia, is considered
quite high and varies between 1% and 3%. Areas
with an ARTI, numbers of 1% suggest that every
year, of 1,000 residents, ten will be infected. From
the infected people, only 10% will become
tuberculosis patients. Thus, it can be estimated that,
in an area with an ARTI of 1%, among 100,000
residents there will be 100 tuberculosis patients on
average per year, 50 of which will be positive acid-
fast bacilli (MOH, 2002).
In Indonesia, tuberculosis disease is still
developing. This is related to the deterioration of the
socio-economic conditions of society, public health
service facilities that are not yet optimal, the number
of people, which is continually increasing, many of
whom do not have permanent residence. The
development of the disease is not separate from
human behavior; mainly the behavior of the
inhabitants in the house (Sukarni, 1995).
Based on the Pamekasan district health office
report in 2011, there were as many as 759 people
suffering from tuberculosis during 2010. In
Pamekasan, from 2011 to May 2018, there were 610
residents who are known to suffer from tuberculosis.
The number of tuberculosis patients is mostly
incrasing in three districts: District Palengaan,
Pasean, and District Palengaan. The number of TB
patients in the Pamekasan District is high in East
Java, and the government are trying to implement
treatment. The government said, Pamekasan District
was ranked fifth in East Java regarding cases of TB,
after Sumenep, Lumajang, Malang, and Jember.
According to the latest data from the health services
for 2012 and 2013, there are three Community
Health Centre that successfully identified TB during
2012. Palengaan Health Community Center
identified 111 patients, the Pasean Health
Community Centre identified 96 patients, and there
were 68 patients identified by the Waru Community
Health Center. For the first quarter of 2013, 22
patients came from Pasean, 19 from Palengaan, and
17 from Batumarmar Community Health Center.
It takes six months of treatment to cure the
infectious disease. If within that six months of
treatment, one day is missed, the treatment must
then start all over again. Drugs are provided free of
charge at every health service center under the
health agency. A house that becomes a home and
shelter for its inhabitants, can guarantee their health.
A house assessed as having healthy conditions has
become a determining requirement for the health
status of its inhabitants. Components of a house and
its environment that do not meet health requirements
are risk factors and a source of transmission of
various types of diseases, especially environmental
diseases (Keman, 2005). Unhealthy housing
conditions will have a negative impact on human
health; one impacting result is tuberculosis. Efforts
to control risk factors that influence the occurrence
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
658

of health threats have been regulated in Kepmenkes
RI. 829/Menkes/SK/VII/1999 regarding housing
health requirements.
Previous studies, such as research by Nur
Yasiroh (2009) and Machrita Hanum (2010) only
analyze the relationship between each component,
i.e. the physical quality of the house with the
occurrence of pulmonary TB, including physical
qualities such as ventilation, room area, floors, and
walls. The health status of housing has not yet been
studied through conducting a healthy house
assessment in relation to the occurrence of
pulmonary tuberculosis. Therefore, the researchers
want to determine the relationship between TB
occurrence rates in the work area of Kedurus Health
Center, with the results of a healthy housing
assessment.
The purpose of this research is to analyze the
relationship between healthy housing conditions and
the occurrence of Pulmonary TB in the Palengaan
District of Pamekasan Regency.
2 METHODS
Case Control Research is an epidemiologically
designed study that examines the relationship
between exposure (factor research) and disease by
comparing case groups and control groups based on
their exposure status (Murti, 1997).
Case Population: Pulmonary TB patients with
positive BTA diagnosis in the Karang Pilang district
and undergoing examination at Kedurus Community
Health Center from January to December 2012.
Population control: Communities in the area who
did not have pulmonary TB during the same period
with the same age and sex and who were neighbors
of the patient in the case population.
Research variables: there are two types, which
are dependent variables and independent variables.
The dependent variable in this study is the
pulmonary TB patients with BTA positive test
results; the independent variable is comprised of
several components, such as: 1. house construction;
2. sanitation facility (clean water facility, latrine, and
waste disposal facility); 3. Inhabitants' behavior; and
4. The density of inhabitants (house ceiling, wall,
floor, bedroom window, window of family room,
ventilation, kitchen smoke hole, lighting).
3 RESULTS
3.1 Characteristics of the Respondents
3.1.1 Respondents’ Age
The case groups and control groups in this study
have the same proportion of age groups. In the case
and control groups, the largest age group is the 21 to
30-year age group, with nine respondents (29%).
The results of this study describe the distribution of
age almost evenly in each age group and the same
thing occurred in the case groups and control groups.
According to Crofton (2002), there is almost no
difference in the risks of developing pulmonary TB
before puberty. The highest occurrence of
pulmonary tuberculosis is usually during young
adulthood. In women, the prevalence peaks at age
40–50 years, and later decreases, whereas in men the
prevalence continues to increase until at least 60
years old.
The results of this study have the same
percentage between case groups and control groups.
This is because during the selection of controls,
matching techniques that equalized age were used,
therefore the researchers do not expect age to be
factor associated with the occurrence of pulmonary
TB. Thus, the results do not support the theory
presented by Crofton (2002). Based on other studies,
according to DG, PPM, & PL (1999), tuberculosis
can occur in all age groups, and not just in adults,
hence the matching results of this study.
3.1.2 Respondents’ Gender
The case group and control group in this study have
different gender proportions. In the case group, the
highest number of respondents is male with 19
respondents (61.3%), while in the control group, the
dominant respondents are also male respondents
with 19 respondents (61.3%).
Crofton (2002) mentions that there is almost no
difference in the risks between men and women of
infection with the TB bacteria regarding the age of
puberty. The number in males is quite high at all
ages, whereas, in women, it tends to decrease
beyond the age of fertility.
The equality of proportions in both groups is due
to the selection of controls using matching
techniques that equalized gender, therefore the
researchers do not expect gender to be one of the
factors associated with the occurrence of pulmonary
TB.
The Relationship between Healthy Housing Conditions and Pulmonary Tuberculosis
659
Based on the theory presented by Crofton (2002),
the risks between men and women are no different;
all people can suffer from Pulmonary TB. According
to Crofton's (2002) statement, the number of males
is greater, based on research results. This is true yet
still cannot be proven with certainty, because the
results of male control groups suggest a larger
number of those who do not suffer from pulmonary
TB.
3.1.3 Respondents’ Education
Level of education is not directly related to the
occurrence of infection by TB germs, but an
educated person and a high level of education will
usually be the same as for a capable person. Capable
means that the person tends to have sufficient
economy to provide adequate nutrition and healthy
housing although this is not yet ascertained. An
educated person has broad knowledge that can affect
a person's behavior. This also cannot be ascertained.
The results showed that the education level of
respondents has a different percentage. In the case
group, as well as the control group, the level of
education of respondents is the same, i.e.
respondents with junior high school education have
a large number in each group. However, the
numbers are not identical. In the case group there
were 25 respondents (80.6%) while in the control
group there were 30 respondents (96.8%).
The relationship between respondents’ education
status with the occurrence of pulmonary tuberculosis
was based on calculation results using a Chi-square
statistic test: (p) = 0.104> (α = 0.05), meaning H0
accepts that there is no relationship between
educational status and the occurrence of pulmonary
TB.
The higher level of education in the control
group indirectly illustrates that the control group
respondents have more ability and knowledge, but
based on the results of research with the analysis
using the Chi-square statistical test, the education
level of respondents is not related to the incidence of
pulmonary TB. In the case group, there were many
respondents who had completed junior high school.
Good education cannot directly affect one's behavior
or ability, so the unconfirmed theory is indeed
refuted by the results of this study.
3.2 House Health Assessment
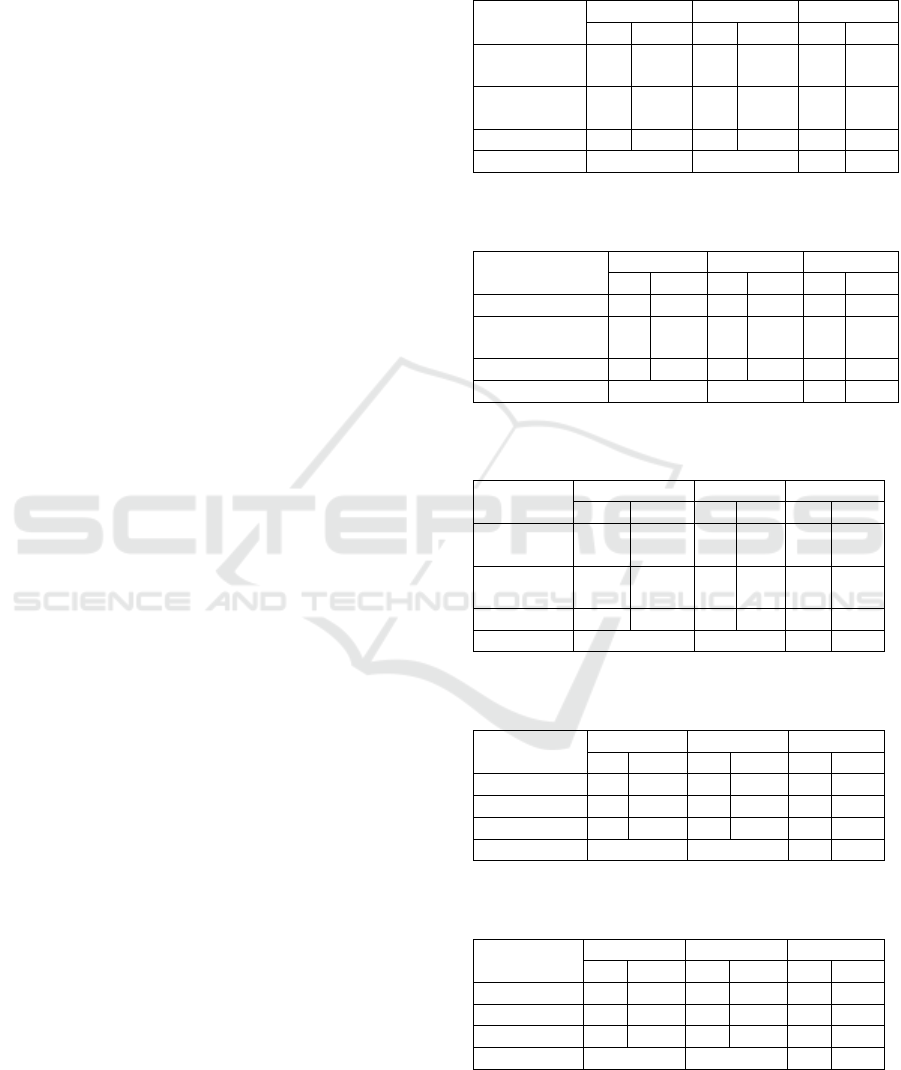
Table 1: The distribution of respondents based on the
house health assessment in Palengaan District.
Health
Assessment
Case
Control
Total
P
%
P
%
P
%
Healthy
House
5
16.1
27
87.1
32
51.6
Unhealthy
House
26
83.9
4
12.9
30
48.4
Total
31
100
31
100
62
100
P: 0.000
OR: 35.10
Table 2: The distribution of respondents based on house
components in Palengaan District.
House
components
Case
Control
Total
P
%
P
%
P
%
Healthy house
18
58.1
24
77.4
42
67.7
Unhealthy
house
13
41.9
7
22.6
20
32.3
Total
31
100
31
100
62
100
P: 0.174
Table 3: The distribution of respondents based on
sanitation facilities in Palengaan District.
Sanitation
facilities
Case
Control
Total
P
%
P
%
P
%
Healthy
house
30
96.8
31
100
61
98.4
Unhealthy
house
1
3.2
0
0
1
1.6
Total
31
100
31
100
62
100
P: 1.000
Table 4: The distribution of respondents based on
inhabitant’s behavior in Palengaan District.
Inhabitant’s
behavior
Case
Control
Total
P
%
P
%
P
%
Healthy
5
16.1
19
61.3
24
38.7
Unhealthy
26
83.9
12
38.7
38
61.3
Total
31
100
31
100
62
100
P: 0.001
OR: 8.233
Table 5: The distribution of respondents based on
residential density in Palengaan District.
Residential
density
Case
Control
Total
P
%
P
%
P
%
Dense
6
19.4
3
9.7
9
14.5
Sparse
25
80.6
28
90.3
53
85.5
Total
31
100
31
100
62
100
P: 0.473
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
660

4 DISCUSSION
Although houses may vary, each component of a
house must fulfill health requirements, so the
inhabitants do not suffer from any illnesses (Azwar,
1995). Components of houses that fulfil health
requirements should provide comfort and maintain
the health of inhabitants, so they can avoid disease,
work productively, and produce something
meaningful.
Housing conditions can determine the level of
hygiene and environmental sanitation. Overcrowded
and narrow housing results in high incidences of
illness, accidents, and other issues (Sukarni, 1995).
Based on Kepmenkes RI No. 829/Menkes/SK/
VII/1999, technical guidelines for the assessment of
healthy homes have been formed to improve housing
conditions. The home parameters evaluated in the
healthy house assessments include three groups of
assessment components, comprised of housing
components, sanitation facilities, and inhabitants
behavior. It aims to assess whether the house has
met the criteria of healthy housing conditions or the
opposite.
The results indicate that there are differences in
the proportion of home health assessments held by
the respondents in the two groups. The proportion of
The dominant evaluation in the case group
assessment was unhealthy, with 26 respondents
(83.87%). The same assessment in the control group
indicated only four (12.9%) respondents with
unhealthy housing. The result of statistical test
shows that P = 0.000 < (α = 0.05), which indicates
that there is a relationship between house health
status and Pulmonary TB incidence. Thus, the
results of this study support several theories that
have been described previously.
Environment is a factor that causes the
occurrence of disease. The environment referred to
in this case is the physical environment of the house.
Poor environment can certainly disrupt the balance
in the process of interaction, involving two other
factors: the agent and the host. The process runs
dynamically and if one is disturbed it can affect the
other, causing the occurrence of disease on the host
(Mubarak, 2009). Unhealthy environmental
conditions will also increase the disease-causing
agent to develop and will facilitate the process of
disease transmission, in this case, pulmonary TB.
The assessment of a healthy house includes three
important things, one of which is the components of
the house. The results of the component assessment
were obtained based on the total score of eight
variables comprising of ceilings, walls, floors,
bedroom windows, living room windows,
ventilation, kitchen smoke holes, and lighting. The
provision of residential health requirements
according to Kepmenkes No.829/Menkes/SK/VII/
1999; components and arrangement of houses are
also listed within it.
According to The American Public Health
Association (APHA) in Azrul Azwar, healthy
housing must be built in such a way that it can be
maintained, including the temperature of the
environment, and the meeting of basic physical
needs. This is to prevent heat loss or excessive heat
(body temperature) and to ensure lighting and home
ventilation is sufficient so that fresh air can be
experienced. According to the Directorate General
of Human Settlements (1997), healthy housing
should include foundations, walls, ceilings, floors, a
roof, and ventilation. Houses with good components
in accordance with health requirements, should
protect inhabitants from disease.
Results indicate that in the case group, there
were 18 respondents (58.10%) with healthy housing
and in the control group there were 24 respondents
assessed with healthy housing (77.4%). Thus, the
results of statistical tests show the value (p) =
0.174> (α = 0.05) means that H0 is accepted,
indicating that there is no relationship between the
healthy components of housing and the incidence of
pulmonary TB.
This result is because most of the respondents in
both the case and control groups have healthy house
components. This resulted in no significant
difference, so there was no relationship. The
assessment of healthy housing in the case group
occurred due to healthy criteria being met regarding
the eight variables. If one variable is badly rated, the
house can still be judged as healthy, because of the
high value of the other variables.
The components of a healthy house are
important, but they must also be accompanied by
healthy behavior and maintenance. House
components of just one example of physical
environmental factors. The physical environment
can have an effect if it is in an unhealthy condition,
so as much as possible it needs to remain in good
health, via a healthy maintenance process.
Behavioral factors and people's lifestyle today still
cause harm to health, hence a higher awareness is
required.
According to Krieger and Higgins (2002),
healthy housing should provide facilities and
infrastructure that includes the availability of clean
water and sanitation of waste disposal. The concept
of healthy housing involves the sociological and
The Relationship between Healthy Housing Conditions and Pulmonary Tuberculosis
661

technical approaches to risk factor management:
qualification, adaptation to the surrounding
environment, management and maintenance of the
house with the surrounding environment, and the
concept of healthy house, include the availability of
sanitation facilities and clean water, adequate means
for cooking and washing, means for the disposal of
human waste or other waste, and, most importantly,
the provision of drinking water (WHO Commission
on Environmental Health, 2001).
For the assessment of healthy housing in this
study, the second assessment group assessed the
availability of sanitation facilities in which there are
four variables. These variables include facilities for
clean water, sewerage, waste water disposal, and
garbage disposal.
Results indicate that almost all respondents in the
case group and control group have healthy sanitation
facilities. The results of the statistical test achieved
the value (p) = 1.00> (α = 0.05) and shows that there
is no relation between sanitation facilities and the
incidence of pulmonary TB. This is because the two
groups have no significant differences meaning that
there is no relationship.
The cause is like the components of the house
that have been analyzed beforehand between the
case group and the control group for the appropriate
availability of sanitation facilities; one inappropriate
variable does not affect the result of the assessment
because the other variables are appropriate and
considered healthy.
Pulmonary TB disease is closely related to poor
home sanitation, but the most influencing factors of
poor sanitation are the components of the house.
House sanitation assessments include four variables:
the availability of clean water, sewerage channels,
latrines, and waste. However, these are not the main
reasons for the transmission of pulmonary TB. Thus,
if the results of the assessment of home sanitation
meet the healthy criteria, this does not mean it can
be free from pulmonary TB. This is due to host
factors and other affecting environmental
components.
Behavior is the activity of an organism. Human
behavior is the activity of a human. Factors that
influence the emergence of behavior can be genetic
and environmental. Genetic factors are a basic
concept for the development of subsequent human
behavior, while the environment is the land
condition for the behavior it develops (Notoatmodjo,
2003).
According to Notoatmodjo (2003), health
behavior is a response of a person or organism
against the stimulus that is associated with an
incidence of disease, the health care system, food,
and environment. Stimulus in health behavior
consists of four basic elements. One of the key
elements is the behavior towards a disease.
The human response to a disease can be passive
in knowing and perceiving or it can be acting upon
that knowledge. This behavior towards corresponds
to levels of disease prevention including, among
other things, improving and maintaining health
behavior, disease prevention behavior as a response
to prevent the occurrence of disease, and behavior
related to the search for treatment, either through
health services or using traditional medicine.
The results indicate that there is a difference in
the percentages of inhabitants’ behavior between the
case group and the control group. In the case group
there were only five inhabitants (16.1%) who
demonstrated healthy behavior. In the control group
the number with healthy behavior was greater, at 19
respondents (61.3%). The results of the statistical
test show the value (p) = 0.001 < (α = 0,05),
meaning there is a relationship between the behavior
of inhabitants and incidences of Pulmonary TB.
Thus, the results of this study support several
theories that have been described previously.
Behavior is one example that can affect the host.
Behavior can increase or reduce sensitivity to illness
and, of course, bad behavior can degrade the health
status of the host (Mubarak, 2009).
This is of course in accordance with the
hypothesis of this study; relationships that occur and
increase the incidence of pulmonary TB. Thus, in
the process it will be conducted by one factor (host)
and will affect the process and other variables
(agents and environment) through the disease
(Pulmonary TB).
Healthy houses should have a bedroom width of
at least 8m
2
and it is recommended that no more
than two people use one bedroom space. The floor
area of the building must also be adjusted to the
number of inhabitants.
The area of the building should be at least 3m
2
for each family member (Notoatmodjo, 2003).
Residential density is the floor area of a room in
a house divided by the family members occupying
the room, so 4m
2
per person would meet the health
requirements for residential density. This is like the
opinion expressed by Lubis (1997), who states that
residential density is the number of people in a
living space compared to the floor area that has
exceeded existing provisions.
Based on the results of the research the seven
respondents (22.58%) in the case group lived in
densely populated houses, while three respondents
INC 2018 - The 9th International Nursing Conference: Nurses at The Forefront Transforming Care, Science and Research
662

(9.68%) in the control group lived in densely
populated houses for (p) = 0.30> (α = 0.05), which
indicates there is no relationship between the density
of residence and incidence of pulmonary TB.
Compared with previous research by Machrita
Hanum (2010), the results of this study are not the
same. Previous studies have suggested that
residential density is associated with pulmonary
tuberculosis incidence. This difference may be due
to the present research being conducted in non-
densely populated areas, so that between case groups
and control groups there are no significant
differences.
In other studies by Isye (2005) and Nur Yasiroh
(2009), the results indicate the same thing;
residential density is not related to healthy housing,
although the cause is different.
5 CONCLUSIONS
Home health assessments were based on the Chi-
square statistic test with the result (p) = 0,000 <α =
0.05, which indicates that house health is related to
pulmonary TB incidence. A healthy house can
reduce the incidence of pulmonary TB, while
unhealthy housing has a 35.10 times greater risk of
having pulmonary tuberculosis compared to healthy
houses.
Health Officers are expected to monitor and
improve sanitation of housing and settlements, and
to further improve counseling regarding a clean and
healthy life to create a healthy environment. In this
case, healthy behavior was assessed to maintain the
health of the house. Supervision should be
conducted once each year, then counseling is
provided at least three times a year in accordance to
the recommendations in the technical guidelines of
healthy housing.
REFERENCES
Alsagaf, H dan Mukty, A. 2009. Dasar dasar Ilmu
Penyakit Paru. Surabaya: Airlangga University Press.
Azwar, A. 1995. Pengantar Ilmu Kesehatan Lingkungan.
Jakarta: MutiaraSumber Widya.
Anonim. 1997. Rumah dan Lingkungan Pemukiman
Sehat. Jakarta: Ditjen CiptaKarya Departemen
Pekerjaan Umum R.I.
Crofton, J dan Norman,H. 2002. Tuberculosis Klinis. Edisi
II. Jakarta: WidyaMedika.
Depkes RI. 2002. Pedoman Nasional Penanggulangan
Tuberculosis. Jakarta: Departemen Kesehatan R.I.
Dinas Kesehatan Kabupaten Pamekasan, 2012. Laporan
Tahunan P3M
Ditjen PPM dan PL. 2002. Pedoman Teknis Penilaian
Rumah Sehat. Jakarta: Departemen Kesehatan R.I.
Keman, S. 2005. Jurnal Kesehatan Lingkungan Vol.2,
No.1. tentang KesehatanPerumahan. Surabaya:
Airlangga University Press.
Kepmenkes RI No. 829/ Menkes/ SK/ VII/ 1999 tentang
Persyaratan KesehatanPerumahan. Jakarta:
Departemen Kesehatan R.I.
Komisi WHO mengenai Kesehatan dan Lingkungan.
2001. Planet Kita KesehatanKita.
Kusnanto H (Editor). Yogyakarta: Gajah Mada University
Press.
Lubis, P. 1997. Perumahan Sehat Proyek Pengembangan
Pendidikan TenagaSanitasi Pusat. Jakarta: Depkes.
Mubarak, W dan Chayatin, N. 2009. Ilmu Kesehatan
Masyarakat: Teori danAplikasi. Jakarta: Salemba
Medika.
Mukono, 2006. Prinsip Dasar Kesehatan Lingkungan.
Edisi Kedua. Surabaya: Airlangga University Press.
Notoatmodjo, S. 2003. Ilmu Kesehatan Masyarakat
Prinsip-Prinsip Dasar.Jakarta : Rineka Cipta.
Notoatmodjo, S. 1993. Metodologi Penelitian Kesehatan.
Jakarta: Rineka Cipta.
Olivia, I. 2005. Hubungan Antara Keadaan Sanitasi
Lingkungan Rumah denganKejadian TB Paru. Skripsi.
Unair.
Panudju, B. 1999. Pengadaan Rumah Kota dengan Peran
Serta MasyarakatBerpenghasilan Rendah. Bandung:
Penerbit Alumni.
Sanropie, D. 1988. Pengawasan Penyehatan Lingkungan
Pemukiman. Jakarta: Departemen Kesehatan R.I.
Soedarsono. 2006. Aspek Pemberantasan Infeksi
Mycrobacterium tuberculose
Simposium Akbar Penyakit Tropik dan Infeksi. Surabaya:
YayasanPenerbitan FK UHT.
Soeparman. 1999. Ilmu Penyakit Dalam. Jilid II. Jakarta:
Balai Penerbit FK UI.
Sukarni, M. 1994. Kesehatan Keluarga dan Lingkungan.
Yogyakarta: Kanisius.
Undang –Undang RI No. 4 Tahun 1992 tentang
Perumahan dan Pemukiman.Jakarta
Yasiroh, N. 2009. Pengetahuan, Sikap, Tindakan dan
Lingkungan RumahPenderita TB Paru di Wilayah
Kerja Puskesmas Pegirian tahun 2008-2009.
Skripsi.Unair.
WHO. 2007. Global Tuberculosis Control Surveilance,
Planning, Financing-WHO Report. Geneva:
Switzerland
WHO. 2017. GLOBAL TUBERCULOSIS REPORT
2017. Geneva: Switzerland
The Relationship between Healthy Housing Conditions and Pulmonary Tuberculosis
663
