
Successful Deployment of Cloud-hosted Services and Performance
Management for Community Care
Benjamin Eze
1,3
, Craig Kuziemsky
2
, Jamie Stevens
3
, Paul Boissonneault
3
and Liam Peyton
1
1
School of Electrical Engineering and Computer Science, University of Ottawa, 800 King Edward Ave, Ottawa, Canada
2
Telfer School of Management, University of Ottawa, 55 Laurier Ave E, Ottawa, Canada
3
Champlain Local Health Integration Network (LHIN), 4200 Labelle St, Ottawa, Canada
Keywords: Healthcare Interoperability, Data Aggregation, Surveillance, Performance Management, Community Care,
Cloud Computing, Regional Health Authority.
Abstract: Achieving systematic performance management of care processes across a health region requires an
architecture that balances interoperability and data standardization with data governance and privacy
compliance. This paper presents a case study of a successful pilot of cloud-hosted performance management
for community care by a Regional Health Authority mandated with coordinating home care amongst 54
Community Support Services agencies. Cloud-hosted data services enabled data integration to a common
data model. Formal data sharing agreements and privacy definition documents controlled aggregation and
data masking to protect privacy while enabling accurate and comprehensive performance management
services for all agencies.
1 INTRODUCTION
Community healthcare is diverse with multiple
settings, actors, data sources and communication
channels (Eze et al., 2017a). Regional health
authorities (RHA) charged with ensuring quality of
care and population health would like to measure, on
a continuous basis, performance management across
the entire healthcare ecosystem. This is challenging
because of the aforementioned distributed nature of
healthcare delivery (Foldy et al., 2014).
To date, hospitals have provided much of the
healthcare outcome data through data sources such as
discharge summaries, referrals, emergency room
visits, wait times and procedures. However, this data
only tracks isolated hospital-based events and not
patient outcomes at the health systems level (Veillard
et al., 2010). Healthcare delivery to support complex
patient care such as chronic illness takes place in the
community and is an ongoing process rather than an
isolated event. Monitoring system performance for
community care is challenging because of the need to
track and measure care delivery across settings
(Durovich and Roberts, 2018; Maruthappu et al.,
2015; Roughead et al., 2011).
Health system management is often coordinated
at an RHA level (Molinari, 2014) that has the goal of
delivering a cost-effective and high-quality
collaborative environment (Sabooniha et al., 2012).
Yet quality management and system accountability
are challenging because of the diverse settings in
which healthcare delivery is provided (Denis, 2014).
Performance management requires a systematic
framework that enables continuous data integration
and monitoring of care processes (Lemieux-Charles
and Greengarten, 2014). Cloud computing is one
potential infrastructure for developing interoperable
healthcare solutions (Andry et al., 2015; Bhaskaran et
al., 2013; Li and Guo, 2015). There is a need for
studies that describe actual implementation of cloud
computing systems and how issues such as privacy
and data sharing were managed (Griebel et al., 2015).
This paper presents a case study of a successful
pilot of cloud-hosted performance management for
community care at by a RHA mandated coordinating
home care amongst 54 Community Support Services
(CSS) agencies. A cloud-hosted system owned and
managed by the health authority solves
interoperability and security issues when you want 54
community care organizations to share data. Cloud-
hosted data services enabled data integration to a
common data model. Formal data sharing agreements
248
Eze, B., Kuziemsky, C., Stevens, J., Boissonneault, P. and Peyton, L.
Successful Deployment of Cloud-hosted Services and Performance Management for Community Care.
DOI: 10.5220/0007365902480255
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 248-255
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

and privacy definition documents controlled
aggregation and data masking to protect privacy
while enabling accurate and comprehensive
performance management services for all agencies.
2 BACKGROUND
Community healthcare is the delivery of healthcare
services outside hospitals to manage chronic illness,
and provide services like rehabilitation support,
nursing, physiotherapy, and end of life care to
patients (CIHR, 2017). Community healthcare is
delivered to clients of all ages whose illness or
condition necessitates long-term health care delivery
at home. The purpose of healthcare performance
management as it relates to community care is to
measure the extent that quality of care goals are
achieved through the delivery of healthcare processes
(Vanhaecht et al., 2007).
Patient needs are met through service-level
planning and coordinated care delivery provided by
health care providers in community settings such as
public health units and community services agencies,
(CIHR, 2017). Continuous efforts are being made to
provide good quality and cost-effective care with
support from government and non-profit
organizations (Boissonnealth and Lafreniere, 2014).
As patient needs may need to be coordinated across
different settings and providers, it is critical to build a
strong collaboration platform for all aspects of
community healthcare to coordinate service delivery
to patients while also monitoring outcomes such as
cost-effectiveness (Berler and Apostolakis, 2014).
2.1 Regional Health Authorities
Community care is typically governed by an RHA. In
Ontario, Canada for example, the Regional Health
Authority is the Local Health Integration Network
(LHIN, 2018), with the mandate to plan, integrate and
fund local healthcare in a region. Ontario has 14
Local Health Integration Networks that target each
sub-region within the province.
Norway employs a similar model with 4 main
RHAs, each with many subsidiaries (Ringard et al.,
2013). For both Ontario and Norway, the RHA is
responsible for patient treatment, medical staff,
planning, research, and development, as well as
support and training for patients and their caregivers.
RHAs are associated with improved healthcare
outcomes, healthcare equality, increased life
expectancy, improved coordination and reduced cost
to healthcare services (Vida et al., 2012).
2.2 Complex Patients
Patient complexity can be due to factors such as
comorbid health conditions that make patient care
management very challenging (Grant et al., 2011).
Providing care for complex patients is putting
increased strain on healthcare budgets and service
delivery performance goals such as wait times
(Sheikh et al., 2015). As a consequence, there is a
growing need to transform the health care system and
the services it delivers to more efficiently provide
care for complex patients (Sabooniha et al., 2012).
Government and healthcare organizations want
better accountability for money spent on healthcare
delivery (Bohmer, 2016), which requires
performance management of care processes across all
stakeholders in the healthcare ecosystem (Berwick et
al., 2008). Achieving this requires coordination and
integration of data across disparate healthcare
information systems (Sabooniha et al., 2012).
Complex patient management is challenging and
expensive as it requires care and service delivery
from a variety of providers (Mcgregor et al., 2016).
Further, complex patients may be managed using
multiple clinical practice guidelines which may have
conflicting recommendations about medications or
treatments (Wilk et al., 2017).
2.3 Performance Management
Performance management provides a mechanism for
translating strategic objectives and business goal to
operational processes (Kemper et al., 2013).
Performance management involves planning, setting
expectations, continuous monitoring of performance,
developing the capacity to perform, as well as rating
and rewarding of performance (OPM.GOV, 2017).
Continuous monitoring of KPIs is key to effective
monitoring and management of strategic goals
(Sanchez and Robert, 2010). However, each strategic
goal also needs to be linked to these KPIs to measure
the extent that the performance of the organization is
achieving goals (Kuziemsky et al., 2010).
Heterogeneous data silos and inconsistent patient
identity approaches, coupled with patient privacy
regulations, limit our ability to correlate data for
complex patients as part of performance management
(Eze et al., 2016). This results in the inability of
stakeholders to coordinate care delivery across
multiple healthcare domains (Adler-Milstein and Jha,
2012). Attempts to address these factors often lead to
unintended consequences (e.g., social, legal and
workflow consequences) that arise from technology-
mediated connectivity (Kuziemsky et al., 2016).
Successful Deployment of Cloud-hosted Services and Performance Management for Community Care
249
2.4 Cloud Computing
Cloud computing is a distributed, configurable
approach for generating ubiquitous access to a pool
of convenient, on-demand computing resources
(compute, storage, platform, application and services)
through a web interface. Cloud computing has been
shown to provide for regional, national and
international data aggregation using a broad range of
topologies that could integrate various devices, data
sources and services very quickly in a scalable and
cost-effective manner (Andry et al., 2015). In
addition, Cloud infrastructure provides an infinitely
scalable storage for very data-intensive applications
(Bhaskaran et al., 2013; Ochian et al., 2014).
Cloud deployment models are differentiated by
the location of the infrastructure, the user of the
infrastructure and the entity that manages the
infrastructure (Furht and Escalante, 2010). There are
three deployment models of cloud computing –
Private, Public, and Hybrid Clouds. A private cloud
is operated by a single organization, which has full
control over the infrastructure, data, security, and
quality of service (QoS). The public cloud is operated
by a 3
rd
party and can be used by with applications
mixed together on cloud servers, storage systems, and
networks (Eze et al., 2016). Finally, a hybrid cloud is
a mix of public and private clouds. In the hybrid
cloud, data and applications are distributed across
both public and private clouds using secure data
bridges (Ma et al., 2014).
A private cloud provides the owners full control
over everything – compute, storage, networking, as
well as the quality of service. While having full
control increases the complexity associated with the
development and deployment of a cloud application
and services, it provides better security and
confidentiality with user data. Unfortunately,
compared to other cloud deployment models, a
private cloud is more expensive (Ma et al., 2014).
The public cloud provides the lowest Total Cost
of Ownership (TCO) of the cloud types but also
provides the least control. Also, data security cannot
be guaranteed since cloud resources are shared by
many organizations. Public clouds are also prone to
resource contention issues, SLA breaches, and
service disruptions. For healthcare organizations with
high volumes of highly sensitive data, this would not
be acceptable since it violates data privacy laws in
many countries (Furht and Escalante, 2010;
Gazzarata et al., 2015).
3 PILOT PROJECT
The Champlain Local Health Integration Network
(LHIN) provides at-home care services for patients in
a metropolitan area with a population of over 1.2
million. About 60,000 annual active patients are
receiving over two dozen community care services
from the LHIN and its 54 Community Support
Services (CSS) agencies.
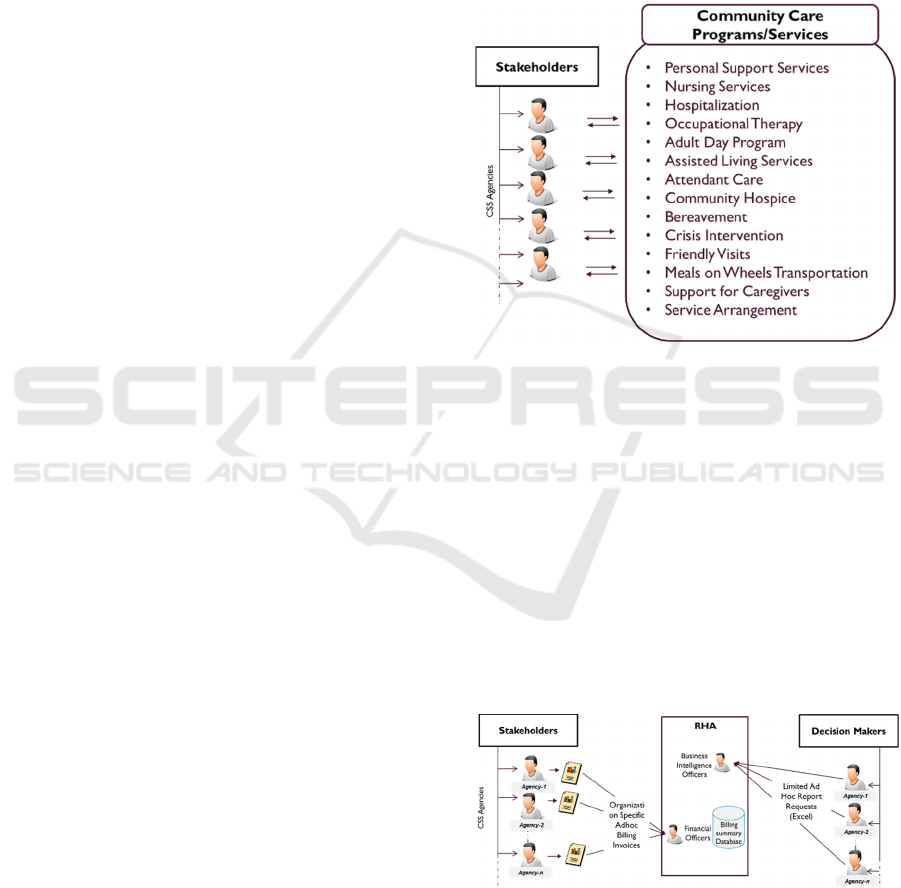
Figure 1: CSS Agencies and Spectrum of Services.
Fig. 1 shows examples of some of these services.
Services provided by these CSS agencies are intended
to improve the quality of life of patients with complex
and chronic health conditions.
3.1 Lack of Performance Management
The lack of performance management of community
care in the Champlain LHIN before the pilot project
is depicted in fig. 2. CSS agencies target specific
populations with niche community services. Usually,
these agencies are small organizations with limited
budgets and their own small ad-hoc IT systems.
Figure 2: Lack of Performance Management.
As a result, there is minimal interoperability and
limited performance management. Data collection is
limited to ad-hoc invoices (typically in MS Excel
HEALTHINF 2019 - 12th International Conference on Health Informatics
250
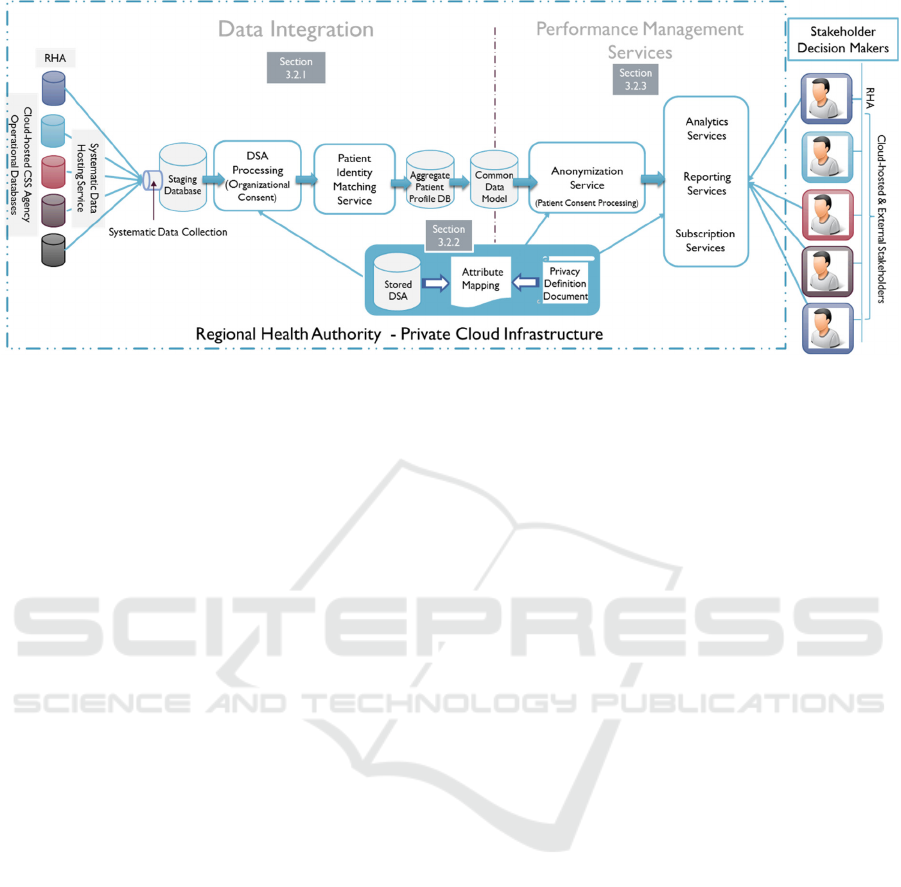
Figure 3: Cloud-based Performance Management Architecture for Community Care.
format) for services rendered by each agency and
usually submitted by email to the RHA financial
officers to process payments. The RHA depends on
ad-hoc reports, mostly prepared for funding and
budgeting needs.
Each CSS agency has their own data silo resulting
in service duplication and limited coordination of care
delivery.
3.2 Architecture
The multi-tenanted private cloud architecture shown
in figure 3, hosts, for each of the 54 CSS agencies,
their patient management applications and
operational databases, while providing data
integration and performance management services.
This preserves the autonomy of each CSS agency,
allowing for quick adoption by each organization.
As depicted in figure 3, the LHIN CSS agencies
that want to participate in the performance
management architecture must sign a Data Sharing
Agreement (DSA) and provide patient consent.
These are formally defined and enforced using
Privacy Definition Documents (PDD). The three
aspects of data integration, privacy compliance and
performance management are described in detail in
the sections that follow.
3.2.1 Data Integration to a Common Data
Model
A Systematic Data Hosting Service ensures that the
data from each CSS agency is in a secure, controlled
environment. This provides the trust needed to allow
systematic data integration into a Common Data
model to support Performance Management services.
As shown in Figure 3, each organization’s patient
management application is hosted in a load balanced
cloud-hosted virtual machine (VM) using a cloud-
hosted Microsoft SQL Server database cluster. Users
from each organization access their respective
application instances through a remote VPN service
using an SSL VPN Client.
A Systematic Data Collection Service connects to
the MS SQL Server cluster and systematically
collects data from each database instance. This
service supports heterogeneous data sources through
data integration (Platform-as-a-Service) PaaS
containers customized for the RHA and 54 CSS
agencies. Data from a particular CSS is only collected
if there is a signed DSA in place as described in
section 3.2.2. The major challenge with this
architecture is that CSS agencies and the Champlain
LHIN do not share a common patient identifier such
as government-issued health card number (HCN). In
addition, identity attributes of the patient like first and
last names, date of birth, gender, phone numbers, and
addresses are not collected in a consistent manner
across the agencies. It is therefore difficult to match
data from different databases for the same patient.
Imposing a common region-wide patient identifier
would be a costly long-term initiative and was
therefore not a viable short-term option. Instead, a
patient-identity matching service was provided.
After evaluating the data sets across the agencies,
we came to three conclusions about identity
matching. First, each agency had an identifier specific
to their database for the patient. Second, agency data
could have data entry errors. Third, patient identity
matching could leverage attributes like current and
historical addresses, phone numbers, to fine-tune and
verify matches.
Successful Deployment of Cloud-hosted Services and Performance Management for Community Care
251
A probabilistic matching algorithm was
implemented to address identity matching for the
infrastructure. This algorithm derives from existing
work in probabilistic record linkage domain like the
Expectation-Maximization (EM) algorithm
(Dempster et al., 1977), as well as the theories of
record linkage (Fellegi and Sunter, 1969) This
algorithm is described in details in a previous
publication (Eze et al., 2017).
It addresses the record
linkage problem by dividing a data set into blocks to
minimize comparisons to only records within the
same block. A block is a combination of one or more
identifier attributes with an associated weight. The
matching process accumulates matches across all
block passes for each patient identity attributes to
determine the matches that are full, partial or
ambiguous or non-matches.
Patient Identity Matching is carried out on all
patient-level records across all the incoming data
streams based on published matching rules. At the
end of the process, a global identifier is issued to each
cluster of profiles belonging to the same patient
across the collaborating organizations. This identifier
is then used to map the rest of their data into the
Common Data Model (CDM).
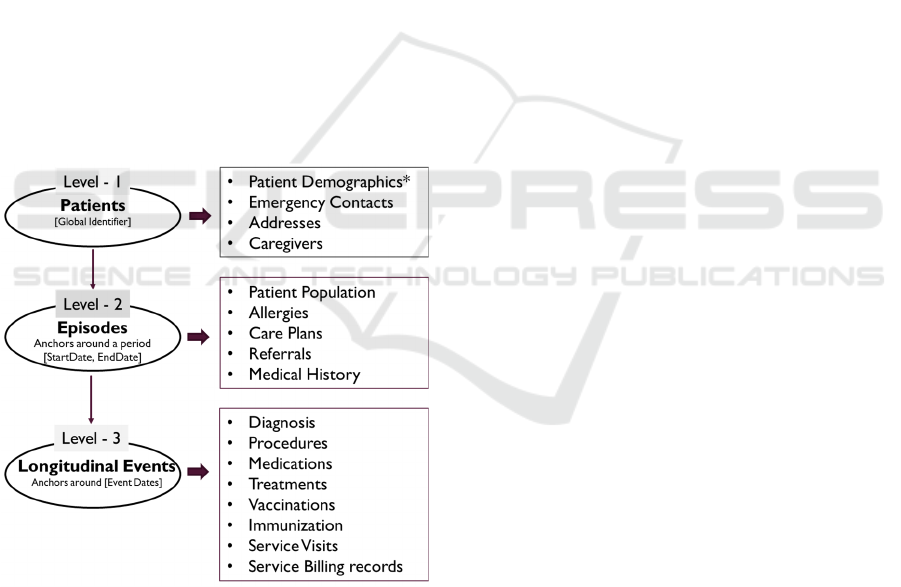
Figure 4: Common Data Model Depicted.
The CDM uses a hierarchical model (fig. 4). Data
elements found in each source database must be
organized into this hierarchical model. The 1
st
level is
patient-centric data with patient identifiers,
demographic data, contact details – phone numbers
and addresses, personal and emergency contacts,
caregivers, family physicians. The 2
nd
level captures
episodes of care and data that map to each episode of
care like the patient population (a categorization of
patients into population groups with similar care
needs), referrals, care plans, and medication history.
The 3
rd
level is longitudinal events and maps to data
on the care episodes defined at the 2
nd
level. These
include service visits for home care, diagnoses and
medications.
3.2.2 Data Sharing Agreements and Privacy
Definition Documents
An essential need for community care data integration
and performance management services is adherence
to privacy legislation. Since the CSS agencies are
independent organizations, they are not under any
mandates to provide data to the LHIN apart from
billing and support reports. Binding agreements that
protect patient privacy and confidentiality need to be
signed between these organizations to allow their data
to be shared.
Privacy compliance is addressed through the
creation of formal Data Sharing Agreements (DSA)
for organizations and a Privacy Compliance
Definition Document (PCDD) that captures both
organizational and patient consent to configure and
regulate the processing of data.
DSAs consents
regulate each incoming data stream from a CSS
agency. The PCDD applies globally (across all data
streams), locally (specific to each organization data
stream), and partially (controlling access to specific
data entities and attributes). Enforcing these consents
can result in complete removal of patient data from
the common data model. In some cases, there could
be full or partial anonymization (data masking,
generalization, suppression) of patient data to meet
set risk thresholds for the infrastructure.
For this pilot project, an all-or-nothing type of
privacy compliance was implemented. The PCDD
provides meta-data on data elements that describe
their semantic types, determining how the privacy of
each attribute should be addressed. It also specifies
fields that needs be nulled, removed, or even masked
based on DSAs to ensure that restricted data never
makes it to the CDM.
All stakeholders that signed the DSA, including
the RHA, have access to all aggregate reports from
the CDM. They and the RHA are also able to see
patient-level report across all agencies except for
those patients that did not consent.
While the all or nothing approach provides good
privacy protection, it does impair the accuracy and
completeness of performance management reporting.
An anonymization service that improves accuracy
HEALTHINF 2019 - 12th International Conference on Health Informatics
252

and completeness is part of proposed future
enhancements to the architecture.
3.2.3 Performance Management Services
Our architecture supports four performance
management services – anonymization, analytics,
reporting, and subscription services. For this pilot
project, three performance management services
were leveraged – anonymization, reporting and
subscription services.
A simplified anonymization model - where all
patients that opted out of data sharing are
automatically excluded from performance
management by the data collection service, was
leveraged. Agencies only see aggregate service data
for patients in their circle of care. Patient-level data
from patients that belong to other providers are
excluded. All performance management reports are
made available to only those participating agencies
that have signed the DSA.
The reporting service use two hosted MS SQL
Server Reporting Services (SSRS) that mirror each
other. Each analytics report created is published on
both servers. Personnel from the LHIN and the
agencies use the reporting portal to access the
standard reports made available to them. Since SSRS
has Web services support, these reports can also be
streamed dynamically, using the subscription service.
Shared Services Subscription service is the
component of the framework that closes the loop
regarding pushing information from the shared data
model to the stakeholders and decision makers at all
levels across all collaborating organizations and their
partners. It is also the component of the performance
management framework that supports process
interoperability described in (Benson, 2012;
Kuziemsky, 2013). The subscription service
leverages data from the CDM and LDAP to provide
knowledge, collaborative, and operational data
needed for performance management of community
care processes.
The key features of the subscription service that
make it adaptable to a cloud computing environment
include 1) Support for dynamic data-driven
subscriptions with declarative and SQL executable
definitions for subscribers and report parameters. All
settings for subscriptions and reports are in
configurable XML definitions hosted in a source
repository. 2) The ability to dynamically package and
deliver multiple reports to users in these different
formats – HTML, MS Word, MS Excel, and Acrobat
PDF. 3) Support for multiple delivery modes – email,
file system, and calendar appointments. 4) Dynamic
scheduling – daily, day periods, weekdays, weekly,
monthly, and quarterly, specific days of the week,
month, quarter. 5) Supports rich failure notifications
for administrators.
For each report developed and published, a
custom report definition file that allows the
subscription service to dynamically stream the report
in many formats is also published to the resource
library. They are created by Business Intelligence
officers with more in-depth knowledge of the model
and the framework. The key utility of the subscription
service is its ability to dynamically package and
deliver multiple reports in various formats through
multiple delivery mechanisms to data recipients.
4 PRELIMINARY EVALUATION
The pilot project is considered a success within the
LHIN. 48 of the 54 the CSS agencies with over
150,000 patients are currently cloud-hosted. 17
agencies with about 30,000 patients have signed the
DSA and currently participate in the performance
management infrastructure. There are nightly data
collection and aggregation of the data across the CSS
operational databases to the Common Data Model.
There are nightly patient identity matching and
progressive clustering of patient profiles. Identity
matching results show that at least 25,000 patients
have matches from another agency or the LHIN with
about 3,000 ambiguous matches that would require
manual approval. However, research has been done to
suggest improvements to the identity management
framework (Eze et al., 2017b).
There are up to 8 active report subscriptions set
up for the LHIN and CSS Agency contacts that
publish and emails various reports. The subscription
service has been adopted by the LHIN and is used to
package and send via email and file transfer, hundreds
of reports to LHIN employees multiple times a day.
Data quality feedback is provided to CSS agencies on
various data quality issues with patient profiles that
need addressing.
The current implementation uses an all-or-
nothing approach to address privacy consent (Eze et
al., 2018). Ongoing research is looking at extending
this through a privacy compliance framework that
leverages anonymization to provide more complete
and accurate reports.
Successful Deployment of Cloud-hosted Services and Performance Management for Community Care
253

5 CONCLUSION
Modern healthcare delivery is about connected
healthcare delivery and patient care management
across providers and settings. Achieving these require
modern approaches to supporting patient care.
Though there are many architectures for patient
management, implementation has remained the last
mile problem. But this is not a technological problem
per se but rather an issue that encompasses multiple
areas such as software design, patient needs, technical
interoperability, privacy considerations, patient data
interoperability (e.g. standards), and governance
agreements across settings.
This paper describes an initial deployment of a
cloud-based performance management system. A
multi-tenanted private cloud infrastructure with
cloud-hosted data services provide a trusted
environment which can enable secure, well-regulated
systematic data integration to a common data model
(CDM) to facilitate comprehensive performance
management for community care. Formal data
sharing agreements (DSA) and a privacy compliance
definition document (PCDD) provide a robust
mechanism for controlled aggregation and data
masking to protect privacy while enabling accurate
reporting.
ACKNOWLEDGEMENTS
This work was supported by the National Science
and Engineering Research Council of Canada
REFERENCES
Adler-Milstein, J., Jha, A.K., 2012. Sharing clinical data
electronically: A critical challenge for fixing the health
care system. JAMA - J. Am. Med. Assoc.
Andry, F., Ridolfo, R., Huffman, J., 2015. Migrating
healthcare applications to the cloud through
containerization and service brokering, in: 8th
International Conference on Health Informatics,
Proceedings;. SciTePress, 164–171.
Benson, T., 2012. Why Interoperability is Hard. In
Principles of Health Interoperability HL7 and
SNOMED SE - 2, 21–32. Springer London.
Berler, A., Apostolakis, I., 2014. Research Perspectives on
the Role of Informatics, Health Policy and
Management, El Morr, C. (Ed.), IGI Global, 168–207.
Berwick, D.M., Nolan, T.W., Whittington, J., 2008. The
triple aim: care, health, and cost. Health Aff. 27, 759–
769.
Bhaskaran, S., Suryanarayana, G., Basu, A., Joseph, R.,
2013. Cloud-Enabled Search for Disparate Healthcare
Data,2013 IEEE International Conference on Cloud
Computing in Emerging Markets IEEE, pp. 1–8. h
Bohmer, R.M.J., 2016. The hard work of health care
transformation. N. Engl. J. Med. 375, 709–711.
Boissonnealth, P., Lafreniere, N., 2014. Deploying
Information Systems throughout the Community Care
Sector of the Champlain Region, in: E-Health 2014
Conference, Vancouver, BC. British Columbia.
CIHR, 2017. Community-Based Primary Health Care, Can.
Institutes Heal. Res., accessed 10.15.17 at
http://www.cihr-irsc.gc.ca/e/43626.html
Dempster, A.P., Laird, N.M., Rubin, D.B., 1977. Maximum
likelihood from incomplete data via the EM algorithm.
J. R. Stat. Soc. Ser. B 1–38.
Denis, J.-L., 2014. Accountability in healthcare
organizations and systems. Healthc. Policy 10, 8–9.
Durovich, C., Roberts, P., 2018. Designing a Community-
Based Population Health. Popul. Health Manag. 21.
Eze, B., Kuziemsky, C., Lakhani, R., Peyton, L., 2016.
Leveraging Cloud Computing for Systematic
Performance Management of Quality of Care. Procedia
Comput. Sci. 98, 316–323.
Eze, B., Kuziemsky, C., Peyton, L., 2017a. Cloud-based
performance management of community care services.
J. Softw. Evol. Process.
Eze, B., Kuziemsky, C., Peyton, L., 2017b. A Patient
Identity Matching Service for Cloud-based
Performance Management of Community Healthcare,
in: Procedia Computer Science.
Eze, B., Kuziemsky, C., Peyton, L., 2018. Operationalizing
Privacy Compliance for Cloud-Hosted Sharing of
Healthcare Data, in Software Engineering in
Healthcare Systems (SEHS). pp. 18–25.
Fellegi, I.P., Sunter, A.B., 1969. A theory for record
linkage. J. Am. Stat. Assoc. 64, 1183–1210.
Foldy, S., Grannis, S., Ross, D., Smith, T., 2014. A Ride in
the Time Machine:
Information Management
Capabilities Health Departments Will Need. Am. J.
Public Health 104, 1592–1600.
Furht, B., Escalante, A., 2010. A Handbook of Cloud
Computing, in: A Handbook of Cloud Computing.
Springer US, pp. 3–19.
Gazzarata, G., Gazzarata, R., Giacomini, M., 2015. A
Standardized SOA Based Solution to Guarantee the
Secure Access to EHR. Procedia Comput. Sci. 64,
1124–1129.
Grant, R.W., Ashburner, J.M., Hong, C.C., Chang, Y.,
Barry, M.J., Atlas, S.J., 2011. Defining patient
complexity from the primary care physician’s
perspective: a cohort study. Ann. Intern. Med. 155.
Griebel, L., Prokosch, H.U., Köpcke, F., Toddenroth, D.,
Christoph, J., Leb, I., Engel, I., Sedlmayr, M., 2015. A
scoping review of cloud computing in healthcare. BMC
Med. Inform. Decis. Mak.
Kemper, H.G., Rausch, P., Baars, H., 2013. Business
Intelligence and Performance Management:
Introduction. Bus. Intell. Perform. Manag. 3–10.
HEALTHINF 2019 - 12th International Conference on Health Informatics
254

Kuziemsky, C., Liu, X., Peyton, L., 2010. Leveraging goal
models and performance indicators to assess health care
information systems, Quality of Information and
Communications Technology Conference, 222–227.
Kuziemsky, C.E., Randell, R., Borycki, E.M., others, 2016.
Understanding Unintended Consequences and Health
Information Technology. IMIA Yearb. 53–60.
Lemieux-Charles, L., Greengarten, M., 2014. Performance
management systems and the reality of Canadian
healthcare organizations from industrial to learning
models. Heal. Q 17, 5–7.
LHIN, 2018. Local Health Integration Network accessed
15.10l.18 at http://www.lhins.on.ca/
Li, Y., Guo, Y., 2015. Wiki-Health: From Quantified Self
to Self-Understanding. Futur. Gener. Comput. Syst. 8
Ma, J., Peng, C., Chen, Q., 2014. Health Information
Exchange for Home-Based Chronic Disease Self-
Management -- A Hybrid Cloud Approach, 4 5th
International Conference on Digital Home. 246–251.
Maruthappu, M., Hasan, A., Zeltner, T., 2015. Enablers and
Barriers in Implementing Integrated Care. Heal. Syst.
Reform.
Mcgregor, J., Mercer, S.W., Harris, F.M., 2016. Health
benefits of primary care social work for adults with
complex health and social needs: A systematic review.
Heal. Soc. Care Community.
Molinari, C., 2014. Does the Accountable Care Act aim to
promote quality, health, and control costs or has it
missed the mark? Comment on “Health system reform
in the United States”. Int. J. Heal. policy Manag.
Ochian, A., Suciu, G., Fratu, O., Voicu, C., Suciu, V., 2014.
An overview of cloud middleware services for
interconnection of healthcare platforms,
Communications Conference, 1–4.
OPM.GOV, 2017. Performance Management Overview
[WWW Document]. URL https://www.opm.gov/
policy-data-oversight/performance-
management/overview-history/ (accessed 20.10.18).
Ringard, Å., Sagan, A., Sperre Saunes, I., Lindahl, A.K.,
2013. Norway: health system review. Health Syst.
Transit. 15, 1–162.
Roughead, E.E., Kalisch, L.M., Ramsay, E.N., Ryan, P.,
Gilbert, A.L., 2011. Continuity of care: When do
patients visit community healthcare providers after
leaving hospital? Intern. Med. J. 41, 662–667.
Sabooniha, N., Toohey, D., Lee, K., 2012. An evaluation of
hospital information systems integration approaches,
Advances in Computing, Communications and
Informatics. ACM Press, New York, New York, USA,
p. 498.
Sanchez, H., Robert, B., 2010. Measuring Portfolio
Strategic Performance Using Key Performance
Indicators. Proj. Manag. J. 41, 64–73.
Sheikh, A., Sood, H.S., Bates, D.W., 2015. Leveraging
health information technology to achieve the “triple
aim” of healthcare reform.
J. Am. Med. Inform. Assoc.
22, 849–856.
Vanhaecht, K., De Witte, K., Depreitere, R., Van Zelm, R.,
De Bleser, L., Proost, K., Sermeus, W., 2007.
Development and validation of a care process self-
evaluation tool. Heal. Serv. Manag. Res. 20, 189–202.
Veillard, J., Huynh, T., Ardal, S., Kadandale, S., Klazinga,
N., Brown, A., 2010. Making Health System
Performance Measurement Useful to Policy Makers:
Aligning Strategies, Measurement and Local Health
System Accountability in Ontario. Healthc. Policy.
Vida, M., Lupse, O., Stoicu-Tivadar, L., 2012. Improving
the interoperability of healthcare information systems
through HL7 CDA and CCD standards, 7th
International Symposium on Applied Computational
Intelligence and Informatics, 157–161.
Wilk, S., Michalowski, M., Michalowski, W., Rosu, D.,
Carrier, M., Kezadri-Hamiaz, M., 2017. Comprehensi-
ve mitigation framework for concurrent application of
multiple clinical practice guidelines. J. Biomed. Inform.
66.
Successful Deployment of Cloud-hosted Services and Performance Management for Community Care
255
