
Hospital Bed Management Practices: A Review
Flannag
´
an Noonan
1
, Jacinta O’Brien
1
, Eilish Broderick
1
, Ita Richardson
2
and Joseph Walsh
1
1
School of STEM, Institute of Technology Tralee, South Campus, Tralee, Ireland
2
Department of Computer Science & Information Systems, University of Limerick, Limerick, Ireland
ita.richardson@lero.ie
Keywords:
Bed Management, Hospital Stay, Hospital Discharge Initiatives.
Abstract:
This paper reviews current literature on the bed management role seeking to highlight developments most
likely to increase efficiency. A reduction in the number of in-patient beds due in part to innovative surgical
techniques is causing increased pressure on a very finite resource. This requires a greater emphasis on the bed
management role and the wider hospital team. A number of studies are presented describing initiatives imple-
mented to support bed management both operationally, procedurally and from a decision support approach.
Finally, literature on people, process technology approaches in healthcare is presented, which could support a
sustainable improvement in the role.
1 INTRODUCTION
The trend in Europe over the last ten years is towards a
reduction in in-patient beds in hospitals. Figure 1 be-
low illustrates the public hospital in-patient bed own-
ership for the larger European states between 2007
and 2015 (Eurostat, 2017).
The reduction is driven by an improvement in sur-
gical techniques leading to a reduction in length
of stay (LOS). In a report produced on the NHS
(Audit-Commission, 2003), it is highlighted that even
though acute beds reduced in England from 123,000
to 107,000, the number of admissions rose due to
reducing length of stay. There is a cost associated
with ‘unoccupied’ beds as reported in (Webster et al.,
2011) which contributes towards bed number reduc-
tions. With an increasing population in Europe, the
management of the decreasing hospital bed resource
becomes more critical.
The aims of this paper are, firstly to present an
overview of the areas of current bed management
practice that contribute to the management of the
bed resource and patient throughput, secondly, to
highlight the challenges present in bed management,
thirdly, to identify those areas that significantly con-
tribute to an improvement and finally suggest a re-
search area as a focus for providing sustainable gains
in efficiency and patient satisfaction.
Section 2 discusses the issues surrounding the bed
management role and its implementation and notes
the contrast of elective and medical patient bed allo-
cation and presents a high level view of the bed man-
agement process. Section 3 reviews trends in address-
ing the issues with a view to increasing the efficiency
of patient placement, through focus on the admission
and discharge elements of the process, pooling capac-
ity and modelling and decision support systems. Sec-
tion 4 identifies work on providing a people, process,
technology approach and the challenges therein high-
lighting the success in manufacturing and software in-
dustries using these techniques. Section 5 concludes
the paper.
2 BED MANAGEMENT ISSUES
The bed management role is at the forefront of effi-
cient use of a critical but limited hospital resources
and timely allocation of beds to patients admitted to
hospitals can turn a stressful experience into a com-
forting and positive experience that will have a pos-
itive effect on patients’ well being. The work of
(Boaden et al., 1999) refer to papers from the early
1990s to claim that “the effective management of beds
as a resource has always been an issue with the NHS”.
2.1 Competing Demands
The bed management role seeks to marry the hospi-
tal bed supply with the hospital bed demand (Boaden
326
Noonan, F., O’Brien, J., Broderick, E., Richardson, I. and Walsh, J.
Hospital Bed Management Practices: A Review.
DOI: 10.5220/0007387403260331
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 326-331
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All r ights reserved
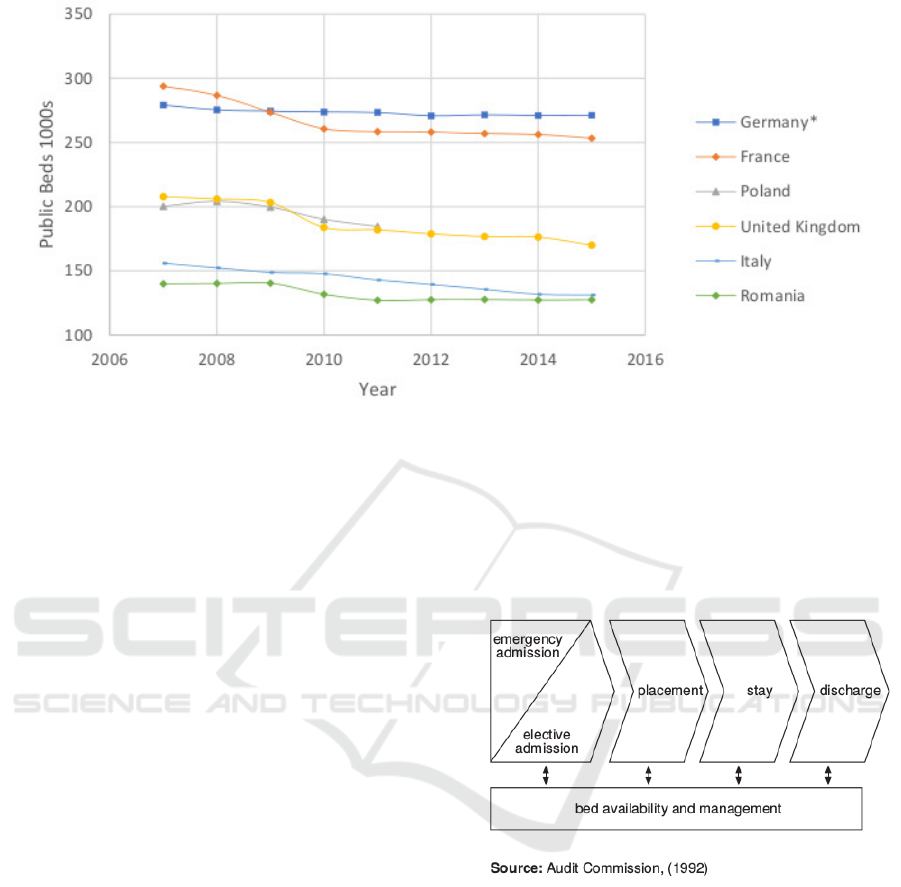
Figure 1: Changes in inpatient bed numbers for a subset of European countries.
et al., 1999). At the top level, two competing demand
streams exist, elective patients and medical emer-
gency patients. The admission of the elective patient
would appear to be more controlled as in most in-
stances the procedures are well defined and in the case
of private patients, is funded by standard insurance
packages with set times defined for individual proce-
dures. Elective day-case patients similar to elective
surgical patients are considered well defined and gen-
erally have dedicated bed resource allocated. How-
ever, (Ortiga et al., 2012) states that numerous case
studies indicate elective admissions cause the greatest
variation as they are more unpredictable and this is
supported by (Allder et al., 2010a). In (Sant et al.,
2015) it is shown that the Day Care Unit in a fo-
cus hospital had 3.9% of patients who were not dis-
charged as planned. In contrast (Allder et al., 2010a)
states that the vast majority of emergency patients re-
quire a very short LOS.
2.2 Other Considerations
The report (Audit-Commission, 2003) covers a range
of issues that affect the placing of patients in beds in
a hospital, such as, speed of admission, admitting a
patient to an appropriate ward, providing single sex
wards, isolation requirements, avoiding cancellation
of elective surgical procedures due to restrictions on
beds. This is not an exhaustive list but servers to il-
lustrate the breath of issues faced by the bed manage-
ment role. Fundamentally the bed management role
is to make the best use of existing beds.
2.3 Process
Figure 2 below, provided in (Boaden et al., 1999), but
reproduced from an earlier Audit Commission report,
illustrates a high level view of the bed management
process.
Figure 2: The bed management process (Boaden et al.,
1999).
The bed resource is constrained until a patient exits
the process through discharge and the bed they oc-
cupied is made available for the next patient. When
emergency admissions are high, such as in the win-
ter period there is a motivation to reduce the num-
ber of elective procedures as suggested in (Audit-
Commission, 2003; Proudlove et al., 2003; Ortiga
et al., 2012). This is particularly true in public hospi-
tals where public perception of long emergency room
waiting times can create pressure to address this is-
sue. This also has impact in terms of the waiting list
times being extended. An exploration of this issue
(Proudlove et al., 2003) highlights the bed manage-
ment role in maintaining a stock of beds but raises
Hospital Bed Management Practices: A Review
327
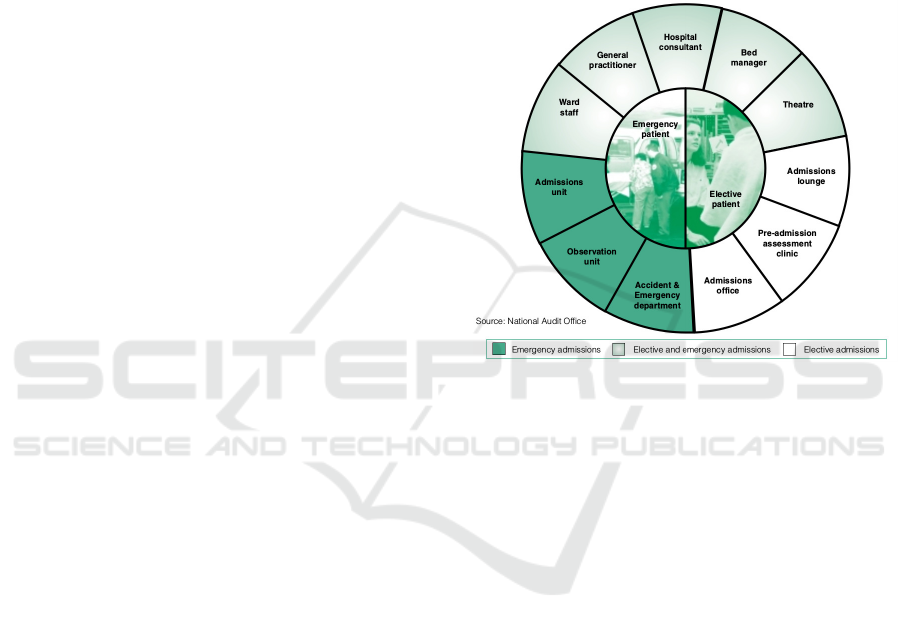
the point that due to the routine hours of the hospi-
tal in general and the bed management presence in
particular, capacity can decrease due to out of hours
admissions.
Many papers (Allder et al., 2010a; Allder et al.,
2010b; Zhu, 2011; Wertheimer et al., 2014; Patel
et al., 2017) raise the issue of patients being admitted
at a time prior to the normal patient discharge time
occurring. This gives rise to an apparent shortage of
beds. This further impacts the patient experience, in
that they are provided with temporary accommoda-
tion only to be moved again to their final destination.
This creates an air of uncertainty for them which can
cause distress or angst and impacts their recovery time
and hence LOS. This can exacerbate bed shortages.
3 BED MANAGEMENT TRENDS
Figure 2 provides a simple linear view of the pa-
tient journey in terms of the bed management process.
Within the bed management role there is most scope
to affect change in the admission or discharge areas.
3.1 Addressing Discharge
Discharge is a common process element to target.
Some of the studies mentioned above (Wertheimer
et al., 2014; Patel et al., 2017; Cho et al., 2017)
and others (Mustafa and Mahgoub, 2016; Zhu, 2011;
Webber-Maybank and Luton, 2009) suggest tackling
this problem by focussing on early discharge. Other
sources (Petitgout, 2015) suggest a dedicated dis-
charge planning function as as a solution. However in
their study (Mabire et al., 2018) on nursing discharge
planning, it is shown that for older patients, being dis-
charged to home, there is an increase in length of stay
without additional benefits to the patient. They also
added that nursing discharge planning is a complex
intervention and difficult to evaluate. In (NHS, 2004),
it is highlighted that 80% of discharges are ‘simple’
discharges and that the focus should be on completing
these in a timely fashion for best efficiency. The re-
port also suggests that the focus on discharge should
begin immediately with a discharge date set within
twenty-four hours of the patients’ arrival in hospital.
Another area of improvement it suggests is extend-
ing discharges as a seven-day activity. This is also
echoed in other reports (Audit-Commission, 2003;
Allder et al., 2010a) where its impact is illustrated by
the LOS of a patient being correlated to the day of
admission.
3.2 Discharge Initiatives
Three very similar studies are discussed (Wertheimer
et al., 2014; Patel et al., 2017; Mustafa and Mahgoub,
2016) that apply interventions to the discharge pro-
cess to bring about earlier discharge. All signify the
importance of teamwork and the role of the multi-
disciplinary team in discharge. Figure 3 illustrates the
broad roles that are involved in treating a patient, for
both elective and emergency patients (NAO, 2000).
Figure 3: The roles involved in patient treatment (NAO,
2000).
A study (Wertheimer et al., 2014) states that all the
stakeholders and staff involved in the launch of an ini-
tiative to increase the discharges before noon (DBN)
were invited to a kick-off meeting. This was imple-
mented to educate everyone involved in the impor-
tance of the issue and the plan for improvement. The
focus was on it being a multi-disciplinary team re-
sponsibility to achieve discharges. Two separate ar-
eas were involved in the initiative and competition
was fostered between the two areas towards achieving
the goal. The main tools were a checklist and a web-
site using automated emails to provide updates. Daily
meetings were used to focus on the current day’s dis-
charges, plan the following day’s discharges and keep
everybody apprised of performance. The paper re-
ports that there was an increase in the number of dis-
charges before noon with an earlier average discharge
time over a 13-month period after the intervention. A
further outcome was a reduction in the average LOS
and unexpectedly a reduction in the number of 30-
Day re-admissions. The latter was not considered
statistically significant. These two factors were very
positive as there was concern that attempts to keep
patients an extra day to help achieve the discharge
before noon may occur. The other concern was that
HEALTHINF 2019 - 12th International Conference on Health Informatics
328

patients could be discharged before they were fully
ready to be discharged resulting in them requiring
hospitalisation again due to early discharge. The fig-
ures proved this not to be the case.
A further study (Mustafa and Mahgoub, 2016), had
a similar outcome and improvement rate to the study
above (increase from 7% to 34% versus an improve-
ment above from 11% to 38%). A multi-disciplinary
discharge team was formed to study the problem. A
list of possible causes was drawn and a Pareto chart
compiled to highlight the major sources of delay. A
number of Plan-Do-Study-Act (PDSA) cycles were
conducted over a 26-month period. It was noted in
the report that sustainability was a challenge due to
the requirement for regular feedback which was time
consuming. The suggestion was that with automation,
this feedback would become easier and thus more sus-
tainable. There was no report of LOS improvement
but the report did state that it did not degrade.
(Patel et al., 2017) followed the same pattern. As in
(Mustafa and Mahgoub, 2016), a multi-disciplinary
team was established to identify the key reasons for
delayed discharge. Each quality improvement initia-
tive contained an education, process change and audit
and feedback element using PDSA cycles. The DBN
rate increased from 10.4% before the intervention to
19.7% after 24-months. DBN to skilled nursing fa-
cilities had a more dramatic change from a baseline
rate of 14% to 33.2% after 24-months. The average
LOS (from 5.88 to 5.60) and 30-Day readmission rate
(17.5% to 17.0%) remained relatively stable over the
period of the intervention. The report commented on
the challenges of sustaining the improvements in an
academic environment with rapid staff turn-over, the
commitment of resource to regular meetings and cre-
ation of audit tools and feedback mechanisms.
3.3 Addressing Admission & Discharge
An approach applying interventions in both the ad-
missions and discharge areas of the bed management
process is reported in (Ortiga et al., 2012). The
primary intervention mechanism at admission was
the change to admitting patients on the same day of
surgery for a large percentage of patients. This had
an obvious reduction in LOS due to the elimination
of the pre-surgery stay for these patients. The inter-
ventions at the discharge area were similar to those
reported above. The elective patient LOS reduced
from 4.85 days prior to intervention and 4.54 days
two years later. The global LOS reduced from 8.56
days to 7.93 days over the same period excluding day
surgery patients.
3.4 Communication
Technology has a role to play in bed management
and real-time information through the use of technol-
ogy can aid decision making (Roswo et al., 2003).
This report provides case studies on the implemen-
tation of technology to assist in the bed management
role. A key benefit stated in the report is the ability to
make information available enterprise wide allowing
for quick decision making and feedback. Infosys, an
IT consultancy company promote combining technol-
ogy with process engineering to provide a solution to
the complexity of the bed management role in their
(Balaji and Brownlee, 2009) report. Technology is
referred to in a general way with an emphasis on pro-
cess engineering. A further industrial report on pro-
cess engineering aimed at increasing patient through-
out is presented in (Kobis and Kennedy, 2006). This
is more a high-level view but does emphasise both a
process viewpoint and the need for a organisational
resolve to succeed.
3.5 Modelling
Another approach is to implement modelling to help
with decision making and decision support systems.
One such approach is detailed in (Teraiya and Mak-
wana, 2015) which applies a mathematical model, on
an assumption of a Poisson probability distribution
rate arrival of patients. The approach was to gather
data over a period and apply the data to the model to
predict the arrival rate of patients and their LOS to
help with accommodating them.
A similar approach was adopted (Griffiths et al.,
2013), for an CCU, to increase throughput, smooth
daily bed occupancy, predict occupancy levels over
the coming days and identify staffing levels to better
manage costs. This approach again used historic data
as an input to the model.
In (Matos and Rodrigues, 2011), the paper promotes
modelling annual data for prediction and augmenting
the modelling with information technology systems to
provide hospital personnel with the information nec-
essary to increase resource effectiveness. Another
study (Baru, 2015) creates a decision support simu-
lation model and uses hospital data to test a number
of hypotheses and compare actual and simulated LOS
and used statistical techniques to validate the model.
A slightly different approach is taken in (Schmidt
et al., 2013) for a decision support system for bed
management, where cost factors include ward occu-
pancy, change of ward occupancy assignment delay
and an affinity cost that allows an administrator to
define a cost. A simulation was created from ac-
Hospital Bed Management Practices: A Review
329

tual hospital data and the output compared to the ac-
tual assignment. One of the limitations noted is that
the software looked at only one resource, bed capac-
ity, whereas in reality multiple other resources would
need to be factored in as part of the placement plan-
ning.
The concept of modelling is taken a step further in
(Bolt and Sparks, 2013) where a surveillance tree
methodology is used to predict changes in presenta-
tions in hospital emergency rooms to allow imple-
mentation of the management of the change. The
surveillance tree methodology is shown to be more
robust in unknown sub-populations over an exponen-
tially weighted moving average (EWMA) model for a
similar population.
Modelling is also used to manage the allocation of
beds in clinical specialisations in a hospital. A multi-
attribute value theory model is proposed in (Tsai and
Lin, 2014) to improve the quality of patient-bed as-
signment in terms of ward specialisation compliance.
This too is the subject of a proposed model by (Lee
et al., 2017) to partition clinic services in the hospi-
tal to provide an efficient means of allocating beds to
the medical specialisations. They address the issue
of how many specialisations to form, the number of
beds to allocate to each specialisation and how to par-
tition services amongst the specialisations using a two
stage framework. The method provide balanced mod-
els for the trade-off between pooling capacity and fo-
cused care using a initial clustering of services while
the subsequent stage performs optimisation of the fea-
sible solutions returned by the initial stage.
4 PEOPLE, PROCESS &
TECHNOLOGY
In the previous sections, a number of initiatives have
been highlighted with regard to improving patient
throughput in hospitals, in an environment of reduc-
ing bed numbers. The sustainability of such issues
was reported as challenging due to the commitment
and effort required to keep the initiatives going while
performing a primary role in caring for patients.
A argument is put forward (Sherer et al., 2017) that
implementing coordination in healthcare is more dif-
ficult due to the many external influences including
payment and regulatory mechanisms, privacy con-
straints and the level of professional control amongst
others.
The report introduces the control theory interdepen-
dence types of ‘pooled’, ‘sequential’ and ‘recipro-
cal’, in order of complexity and the associated coor-
dination mechanisms of ‘standardisation’, ‘plan’ and
‘mutual adjustment’. The report goes on to state
that while care monitoring is achievable at the pooled
level, for care coordination a reciprocal level of in-
terdependence needs to be achieved. This is only
achieved through a very high level of information
sharing.
A comparison in this report, between industry’s suc-
cessful coordination re-engineering and the additional
challenges associated with implementation in health-
care is echoed in (Husby, 2012). In this second study,
the adoption of the ‘lean’ concept used so success-
fully in manufacturing and software is promoted us-
ing hoshin. The paper states that the adoption of the
lean techniques has potential to facilitate coordina-
tion in the healthcare environment but needs signifi-
cant capabilities and management to achieve success.
The study proffers a practical approach for undertak-
ing a hoshin initiative. It also underpins the critical-
ity of improving coordination in people process tech-
nology as increased technology deployment is driving
increasing health costs without a matched impact in
care.
5 CONCLUSION
This paper has examined bed management and shown
it to be a key area to increase patient throughput thus
making a scarce resource available to more people.
The trend for decreasing bed numbers, with increas-
ing population can only serve to increase pressure on
the bed resource. An increased efficiency can help to
counter this pressure.
There is a constant application of initiatives to work
towards a more efficient use of bed resource but the
effort of sustaining them is an issue.
This paper’s contribution is to highlight the need for
sustainable solutions in addressing bed management.
It further suggests, a holistic approach to looking at
people, processes and technology to create greater co-
ordination in the healthcare sector as successfully ap-
plied in manufacturing and software could be the key
to providing the sustainability required to maximise
efficiency of the bed resource.
ACKNOWLEDGEMENTS
This work was supported with the financial support
of the Science Foundation Ireland grant 13/RC/2094
and co-funded under the European Regional Develop-
ment Fund through the Southern & Eastern Regional
Operational Programme to Lero - the Irish Software
Research Centre (www.lero.ie)
HEALTHINF 2019 - 12th International Conference on Health Informatics
330

REFERENCES
Allder, S., Silvester, K., and Walley, P. (2010a). Managing
capacity and demand across the patient journey. Clin-
ical Medicine, 10(1):13 – 15.
Allder, S., Silvester, K., and Walley, P. (2010b). Under-
standing the current state of patient flow in a hospital.
Clinical Medicine, 10(5):441–444.
Audit-Commission (2003). Bed Management: Review of
National Findings.
Balaji, R. and Brownlee, M. (2009). Bed management op-
timization. Technical report, Infosys.
Baru, R. (2015). A decision support simulation model for
bed management in healthcare. Master’s thesis, Mis-
souri University of Science and Technology.
Boaden, R., Proudlove, N., and Wilson, M. (1999). An ex-
ploratory study of bed management. Journal of Man-
agement in Medicine, 13(4):234–250.
Bolt, S. and Sparks, R. (2013). Detecting and diag-
nosing hotspots for the enhanced management of
hospital emergency departments in queensland, aus-
tralia. BMC Medical Informatics and Decision Mak-
ing, 13(132).
Cho, H., Desai, N., Florendo, A., Marshall, C., Michalski,
J., and amd A. Dunn, N. L. (2017). E-dip: Early dis-
charge project: A model for throughput and early dis-
charge for 1-day admissions. https://bmjopen qual-
ity.bmj.com/content/5/1/u210035.w4128. Accessed
2017-11-16.
Eurostat (2017). Hospital beds by hospital ownership.
http://appsso.eurostat.ec.europa.eu/nui/show.do?data
set=hlth rs bds2&lang=eng. Accessed 2017-12-18.
Griffiths, J., Knight, V., and Komenda, I. (2013). Bed man-
agement in a critical care unit. IMA Journal of Man-
agement Mathematics, 24:137–153.
Husby, B. (2012). Integrating people, process and tech-
nology in lean healthcare. PhD thesis, University of
Michigan.
Kobis, D. and Kennedy, K. (2006). Capacity management
and patient throughput: putting the problem to bed.
Healthcare Financial Management, 60(10):88–92.
Lee, E., Shapoval, A., and Wang, Z. (2017). Inpatient bed
management to improve care delivery.
Mabire, C., Dwyer, A., Garnier, A., and Pellet, J. (2018).
Meta-analysis of the effectiveness of nursing dis-
charge planning interventions for older inpatients dis-
charged home. Journal of Advanced Nursing, 74(4).
Matos, J. and Rodrigues, P. (2011). Modeling decisions for
hospital bed management: A review. HEALTHINF
2011 - International Conference on Health Informat-
ics.
Mustafa, A. and Mahgoub, S. (2016). Understanding and
overcoming barriers to timely discharge from the pe-
diatric units. https://bmjopenquality.bmj.com/ con-
tent/5/1/u209098.w3772. Accessed 2017-09-25.
NAO (2000). Inpatient admissions and bed management in
nhs acute hospitals. Technical report, National Audit
Office.
NHS (2004). Achieving timely ‘simple’ discharge from
hospital a toolkit for the multi-disciplinary team.
http://webarchive.nationalarchives.gov.uk/200411231
20000/http://www.dh.gov.uk/assetRoot/04/08/83/67/
04088367.pdf. Accessed 2017-09-19.
Ortiga, B., Salazar, A., Jovell, A., Escarrabil, J., Marca, G.,
and Corbella, X. (2012). Standardizing admission and
discharge processes to improve patient flow: A cross
sectional study. http://www.biomedcentral.com/1472-
6963/12/180. Accessed 2017-12-11.
Patel, H., Morduchowicz, S., and Mourad, M. (2017). Us-
ing a systematic framework of interventions to im-
prove early discharges. The Joint Commission Journal
on Quality and Patient Safety, 43(4):189–196.
Petitgout, J. M. (2015). Discharge coordinator to improve
the patient discharge experience. Journal of Pediatric
Health Care, 29(6):509–517.
Proudlove, N., Gordon, K., and Boaden, R. (2003). Can
good bed management solve the overcrowding in ac-
cident and emergency departments? Emergency
Medicine Journal, 20(1):149–155.
Roswo, E., Adam, J., Coulombe, K., Race, K., and Ander-
son, R. (2003). Virtual instrumentation and real-time
executive dashboards: Solutions for health care sys-
tems.Nursing Administration Quarterly, 27(1):58 – 76.
Sant, J., Abela, G., and Farrugla, D. (2015). Delayed dis-
charges and unplanned admissions from the day care
unit at mater dei hospital, malta. Malta Medical Jour-
nal, 27(2):26–30.
Schmidt, R., Geisler, S., and Spreckelsen, C. (2013). De-
cision support for hospital bed management using
adaptable individual length of stay estimations and
shared resources. BMC Medical Informatics and De-
cision Making, 13(3).
Sherer, S., Meyerhoefer, C., and Levick, D. (2017).
Challenges to aligning coordination technology with
organizations, people and processes in healthcare.
https://scholarspace.manoa.hawaii.edu/handle/10125/
41586. Accessed 2018-02-22.
Teraiya, Y. and Makwana, P. (2015). A study of bed man-
agement the model in a hospital. The Joint Commis-
sion Journal on Quality and Pateint Safety, 3(5):489–
490.
Tsai, P. and Lin, F. (2014). An application of multi-attribute
value theory to patient-bed assignment in hospital ad-
mission management: an empirical study.
Webber-Maybank, M. and Luton, H. (2009). Making ef-
fective use of predicted discharge dates to reduce the
length of stay in hospital. Nursing Times, 105(15).
Webster, J., Davies, H., Stankiewicz, M., and Fleming, L.
(2011). Estimating the time involved in managing the
’unoccupied bed’: a time and motion study. Nursing
Economics, 29(6):317–322.
Wertheimer, B., JHacobs, R., Bailey, M., Holstein, S., Chat-
field, S., Ohta, B., and amd K. Hochman, A. H.
(2014). Discharge before noon: An achievable hospi-
tal goal. Journal of Hospital Medicine, 9(4):210–214.
Zhu, Z. (2011). Impact of different discharge patterns on
bed occupancy rate and bed waiting time: a simulation
approach. Journal of Medical Engineering & Technol-
ogy, 35(6-7):338–343.
Hospital Bed Management Practices: A Review
331
