
Clinical Caremap Development: How Can Caremaps Standardise
Care When They Are Not Standardised?
Scott McLachlan
1,2
, Evangelia Kyrimi
2
, Kudakwashe Dube
1,3
and Norman Fenton
2
1
Health Informatics and Knowledge Engineering Research Group (HiKER), New Zealand
2
Risk and Information Management, Queen Mary University of London, London, U.K.
3
School of Fundamental Sciences, Massey University, Palmerston North, New Zealand
Keywords: Caremap, Care Map, Clinical Documentation, Clinical Careflow, Flow Diagrams.
Abstract: Caremaps were developed to standardise care. They have evolved from text-based descriptions to flow-based
diagrams. Standardising care is seen to improve patient safety and outcomes, and to reduce the costs of
providing healthcare services, but contemporary caremaps are not standardised. This research investigates
contemporary caremaps and proposes a standardised model for caremap content, structure and development.
The proposed model is evaluated through two case studies to create caremaps for; 1) obstetric care during
labour and birth, and; 2) management and for women with gestational diabetes mellitus, finding that it is an
effective method for creating standardise caremaps.
1 INTRODUCTION
Caremap is a term currently used to describe a
graphical representation of the sequence of patient
care activities to be performed for a specific medical
condition. Caremaps have existed in some form for
around forty years (Hampton, 1993; Zander, 2002;
Gemmel et al., 2008). The literature suggests they
originated in the nursing domain, incorporating and
extending the critical pathway method and bringing
established project management methodologies into
healthcare delivery (Chu and Cesnik, 1998);
(Gemmel et al., 2008); (Zander, 1992). Caremaps are
intended to standardise health services by organising
and sequencing care delivery, ensuring a standard of
care and timely outcomes using an appropriate level
of resources (Marr and Reid, 1992; Hampton, 1993;
Blegen et al., 1995; Bumgarner and Evans, 1999).
The caremap can also help track variance in clinical
practice, as it provides a simple and effective visual
method for identifying when treatment or patient
outcomes have deviated from the routine evidence-
based pathway (Marr and Reid, 1992), (Houltram and
Scanlan, 2004).
Terminological disagreement persists as to
whether caremaps are a separate format of clinical
tool (Zander, 1992; Kehlet, 2011; Solsky et al., 2016),
or simply another name for care pathways, clinical
pathways, critical pathways and care plans (Holocek
and Sellards, 1997; Campbell et al., 1998; O'Neill and
Dluhy, 2000; Li et al., 2014). This terminology
confusion is further exemplified when we observe
flow diagrams that internally describe themselves as
a “care map”, yet are captioned ‘clinical pathway’ by
the author such as observed in Figure 1 of (Thompson
et al., 2011) and Figure 5 on p45 of (Yazbeck, 2014).
Yazbeck (2014) goes on to present a range of similar
flow diagrams for care management, describing them
using a range of titles including ‘care map’, ‘care
pathway’, and ‘algorithm’.
Nursing caremaps from the early 1990’s
contained considerably more text than their
contemporary counterparts, and were presented as the
sum of two components: (1) identifying patient
problems and necessary outcomes within a time-
frame which are (2) broken down and described day-
by-day as tasks on a critical path, (Marr and Reid,
1992; Ogilvie-Harris et al., 1993). Later approaches
presented three components: (1) the flow chart
diagram; (2) the transitional text-based care map of
activities broken down day-to-day, and; (3) the
evidence base relied upon in their construction
(Houltram and Scanlan, 2004). It is these approaches
which may have resulted in the terminology
confusion that persists to today.
More recent caremaps have tended towards
representation as a flow diagram made up of clinical
McLachlan, S., Kyrimi, E., Dube, K. and Fenton, N.
Clinical Caremap Development: How Can Caremaps Standardise Care When They Are Not Standardised?.
DOI: 10.5220/0007522601230134
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 123-134
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
123

options for a particular condition and resulting in
multiple possible paths based on: (i)
symptomatology; (ii) diagnostic results, and; (iii)
how the patient responds to treatment (Chan et al.,
2005; BCCancer, 2012; deForest and Thompson,
2012). Caremap examples can be found in many
healthcare domains, including: paediatric surgery
(Chan et al., 2005), nursing (deForest and Thompson,
2012), oncology (BCCancer, 2012), diagnostic
imaging (WAHealth, 2013), obstetrics (Comreid,
1996) and cardiology (Hampton, 1993). Even within
these examples there exists significant variance in
complexity level, design approach, content and the
representational structures used. There is currently no
standardised method for the development or
presentation of a clinical caremap (Bumgarner and
Evans, 1999). Changes in format between like
documents and poorly designed materials increase
ambiguity and create confusion for the clinician
(Hubner et al., 2010), (Valenstein, 2008), (Wang et
al., 2013). Standardised approaches to documentation
ensure that each time a clinician approaches that type
of document, the content and format meet their
expectations, can be read quicker, are better retained,
and improves patient safety and outcomes (Christian
et al., 2006; Valenstein, 2008). For this reason our
paper asks: how can caremaps be an effective tool to
standardise healthcare when caremaps themselves are
not standardised?
The rest of this paper is organised as follows:
Section 2 discusses caremap terminology, history and
evolution. Section 3 defines the problem of
standardisation and Section 4 reviews related
literature. Section 5 presents the methodology and
results of a literature review on the primary elements
of caremaps. The proposed standardised caremap
model is described in Sections 6 and 7 and validated
in Section 8 through the conduct of two case studies
in the area of midwifery and obstetrics. The paper is
then summarised and concludes with proposals for
future work.
2 CAREMAPS: TERMS,
BACKGROUND AND CONTEXT
2.1 Caremap Terminology
Definitions drawn from literature of the early-mid
1990’s agree in principle that the caremap presents as
a graph or schedule of care activities described on a
timeline and performed as part of the patient’s
treatment by a multidisciplinary team to produce
identified outcomes (Marr and Reid, 1992; Hampton,
1993; Ogilvie-Harris et al., 1993; Blegen et al., 1995;
Wilson, 1995; Gordon, 1996; Hill, 1998; Zander,
2002). While the format of caremaps has changed
over the intervening decades, this general definition
is still appropriate.
Caremaps are observed under three different
titles: caremaps, CareMaps and care maps. The first
appears to have been the original title prior to the
Centre for Case Management (CCM) trademarking
CareMaps in the early 1990’s (Blegen et al., 1995;
Dickinson et al., 2000). In literature published after
1994 that uses caremaps, it is not uncommon to see
some mention of CCM or their trademark (Philie,
2001), although some don’t (Griffith et al., 1996;
Saint-Jacques et al., 2005). The use of care maps has
possibly come as a defence to any potential issues that
might have arisen from confusion with the trademark,
as we did not see authors using this third type in
context or with reference to CCM (Marr and Reid,
1992; Mackay et al., 2007; Royall et al., 2014).
2.2 Background of Caremaps
While there appear to be three descriptions for the
origin of caremaps, there are points of intersection
between each. The descriptions are:
(1) That caremaps resulted as an output of the CCM
in 1991 (Dickinson et al., 2000). CCM’s
CareMaps were similar in form and function to
existing clinical pathways and were applied to
specific patient populations that were commonly
treated in high numbers in hospitals (Dickinson et
al., 2000). This organisation then went on to
trademark the double-capitalised version
CareMap but had not within the first decade
undertaken any research to demonstrate
effectiveness of the concept whose invention they
claimed (Jones and Norman, 1998).
(2) That caremaps naturally evolved as an expansion
of earlier case management and care plans
(Zander, 2002).
(3) That caremaps were developed during the 1980’s
at the New England Medical Centre (NEMC)
(Wilson, 1995; Schwoebel, 1998).
There is some support for the notion that caremaps
had existed in the decade before the CCM’s
‘invention’ and trademark, in that it had been
observed that nurses were the primary users of
caremaps in the 1989 (Etheredge, 1989; Wilson,
1995).
Where the intersection occurs is: (a) between the
first two descriptions and in the way that staff of
HEALTHINF 2019 - 12th International Conference on Health Informatics
124

CCM have sought to elevate differences between
clinical pathways and their model of CareMaps;
identifying that the former represented a first-
generation concept while the latter improves on it by
adding consideration of variance and outcome
measurement (Morreale, 1997), and; (b) between the
last two in that each has some element in their story
suggesting caremaps came into existence in the
1980’s.
2.3 Caremap Evolution and Current
Context
Early caremaps were text-based and holistic. Rather
than focusing on just the immediate primary
diagnosis or intervention, nurses developed them to
focus on the entire scope of care that might be
necessary for the patient during their hospitalisation
event. These traditional caremaps considered
elements such as anxiety, rehabilitation, education,
prevention and coping strategies and were intended to
restore the patient to a normal quality of life (Marr
and Reid, 1992; Goode and Blegen, 1993; Ogilvie-
Harris et al., 1993; Wilson, 1995; Feigin, 1996).
In the second half of the 1990’s care providers
began to identify that creating caremaps was easier
for surgical procedures than other in-hospital care
intervention situations (DeJesse et al., 1995).
Evolution of caremaps in form and function was
expected as information technology and evidence-
based medicine developed (Wilson, 1995). Starting
from 1999 there began to be examples of transitional
caremaps; caremaps that whilst still being text-based,
have reduced their focus to interventions limited to
the primary diagnosis (Bumgarner and Evans, 1999;
Cholock, 2001; Philie, 2001).
As caremaps evolved into graphical
representations we begin to find contemporary
caremaps presented as a separate but complementary
component to the clinical pathway or clinical practice
guideline (Dickinson et al., 2000); (Saint-Jacques et
al., 2005). More recent caremaps are linked to or
provide a graphical flow representation for a clinical
practice guideline (CPG) or surgical event (Houltram
and Scanlan, 2004; Chan et al., 2005; Royall et al.,
2014). While retaining the purpose and flow, many of
those seen today annexed to CPGs have even dropped
the title (RWH, 2010; TCHaW, 2010; Thompson et
al., 2013; Reading et al., 2015). A summary of the
relevant elements of each caremap type is included in
Table 1.
3 THE PROBLEM:
STANDARDISING THE
CAREMAP AND ITS
DEVELOPMENT PROCESS
Proponents see standardisation of care processes as an
effective method for reducing healthcare service
delivery costs and variation, while increasing quality,
safety, efficacy and outcomes, improving the patient
experience and overall quality of life (Appleby et al.,
2011; Zarzuela et al., 2015). Yet we see that
healthcare remains one of the slowest industries to
adopt process standardisation or to demonstrate it has
positive impacts on patient safety and outcomes
(Leotsakos et al., 2014; Zarzuela et al., 2015; Binks,
2017). This in part is due to clinician resistance; with
attempts at care standardisation derided as
‘cookbook’ or ‘cookie cutter medicine’ that some say
Table 1: Summary and Comparison of Caremap Evolution Stages.
Traditional
(1980’s to mid-1990’s) *
Transitional
(Mid-1990’s to mid 2000’s) *
Contemporary
(2004 onwards) *
Primary Author Nurses Nurses and Doctors Doctors
Context Holistic Primary condition
Single diagnostic, screening and/or
intervention event.
Foci
Restoring the patient to
normal life
Outcomes, cost and resource consumption
Efficiency of care delivery and outcomes,
reduction of practice variation, bridge gap
between evidence and practice
Presentation Tex
t
-
b
ased Tex
t
-
b
ased with some early flow examples Flow diagram or graph
Status Independent document
Independent or sometimes incorporated
with CP document
Self-contained but often found appended
to/contained in CPG
CP = Clinical Pathway, CPG = Clinical Practice Guide
*All dates are approximate ranges
Clinical Caremap Development: How Can Caremaps Standardise Care When They Are Not Standardised?
125

can only be effective after they have set aside the
unique needs of individual patients (Giffin and Giffin,
1994; Rotter et al., 2008; Zarzuela et al., 2015;
Corbett, 2016). Given the current overuse issues and
financial crisis pervading healthcare service delivery
globally, standardisation of key documentation can
help clinicians deliver managed care, which is seen to
reduce incidences of inappropriate and ineffective
care, resource consumption and overall cost (Keyhani
et al., 2014; Martin, 2014).
Caremaps, clinical and critical pathways, clinical
flow diagrams and nursing care plans are observed
with vastly different content and appearance within
the same journal, from hospital to hospital, and
sometimes even from ward to ward in the same
hospital. While much literature presents caremaps
and other clinical documents such as clinical
pathways, and texts exist for the development of
traditional text-based caremaps, a gap exists with
regards to presenting a standard for the development
and structure of contemporary caremaps. This
research seeks to differentiate contemporary
caremaps from other forms of clinical documentation,
and to present one possible solution to standardising
their development, structure and content.
4 RELATED WORKS
There were numerous examples of contemporary
caremaps in the literature and annexed to hospital-
based clinical practice guidelines (CPGs).
Contemporary caremap literature tended to focus on
establishing the clinical condition that justified
creation of the caremap, such as: determination of
incidence, risk factors and patient outcomes (Chan et
al., 2005); diagnosis and stabilisation of patients with
an acute presentation (deForest and Thompson,
2012), and; protocolising of ongoing treatment
(Royall et al., 2014). Presentation or discussion of the
development process and elements for construction
were rare, and more often had to be inferred via a
thorough reading of each paper.
A single article was located that attempts to
describe a systematic process for contemporary
caremap development (Sackman and Citrin, 2014).
Authored by a veterinarian and a lawyer, this article
focuses more on standardising care process
representation into a clinical caremap for the purposes
of cost containment and provides the example of
mapping a surgical procedure (Sackman and Citrin,
2014). Given their focus and particular caremap
construction which, through their own exemplar
application only includes a temporally-ordered
single-path representation of the gross steps of patient
care, their paper might only be considered formative
at best. By their own admission they deliberately
limited the relevant data analysed during the input
design phase to only what is truly critical for
identifying and understanding outliers, which results
in its lack of clinical applicability and distinct lack of
detail surrounding each care process (Sackman and
Citrin, 2014). Their method requires significant work
to adequately support true standardised clinical
caremap development.
5 METHODOLOGY
Literature Review: A search using the terms
‘caremap’, ‘CareMap’, and ‘care map’ was conducted
across a range of databases. A citation search was also
performed on all included papers. This search yielded
1,747 papers. Once duplicates, papers not based in the
nursing, medical or healthcare domains and those
using the term “care map” in other contexts were
removed a core pool of 115 papers remained.
Development of Review Framework using Thematic
Analysis: Initially each paper was reviewed using
standard content and thematic analysis (Vaismoradi
et al., 2013) and concept analysis (Stumme, 2009) to
identify and classify terminology, construction and
content elements and infer development processes.
Methodology for Standardisation of Caremaps:
Literature reviews have a ground-level consensus
forming function allowing identification of
implementation techniques and the degree of accord
within a domain (Bero et al., 1998; Cook et al., 2013).
The literature pool was used to identify common
definition, structure and content elements of
caremaps. In addition, process steps that were
consistently described led us to a standardised
caremap development process.
Methodology for Evaluation of Proposed Standard
for Caremaps: Case Studies are a grounded
comparative research methodology with a well-
developed history, robust qualitative procedures and
process validation (McLachlan, 2017). The case
study approach provides a real-life perspective on
observed interactions and is regularly used in
information sciences (Lee, 1989; Cable, 1994;
Smithson, 1994; Peak et al., 2005). Case studies are
considered as developed and tested as any other
scientific method and are a valid method where more
rigid approaches to experimental research cannot or
do not apply (Eisenhardt, 1989; Tellis, 1997; Yin,
HEALTHINF 2019 - 12th International Conference on Health Informatics
126
2011). Both the standardised development process
and resulting caremap are evaluated using case
studies of examples from the author’s other works.
6 CONSENSUS FORMATION ON
CAREMAP: COMPOSITION
AND DEVELOPMENT PROCESS
The literature was used to establish consensus on
common structure, content and development
processes previously used in the creation of
caremaps, and which may be relevant in defining
standard caremap and development processes. The
case studies are used to evaluate and refine each. The
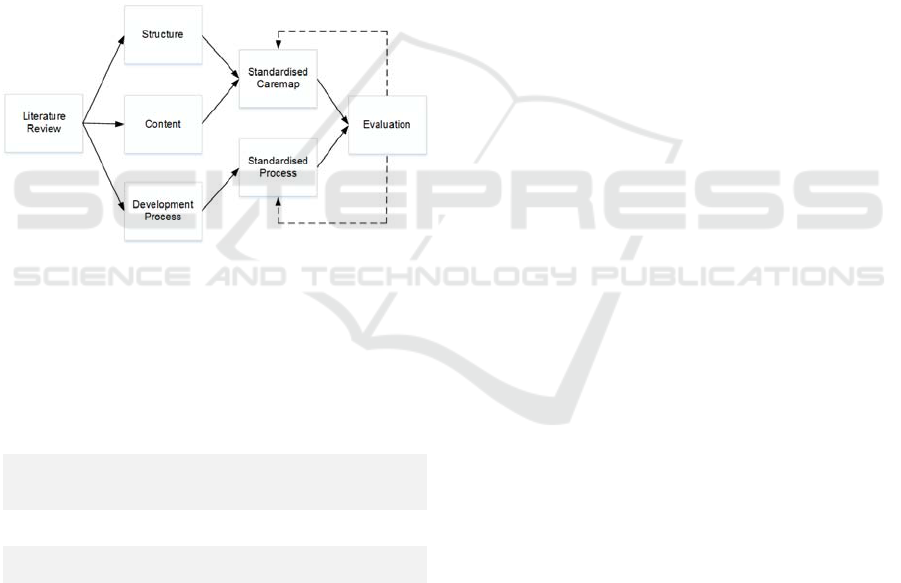
research was conducted following the overall
approach presented in Figure 1.
Figure 1: Research process – Consensus formation and
evaluation.
To address the stated aim of this paper, we
focused our research on tertiary care (hospital-borne)
caremaps and specifically the following three
components whose characteristics came out of the
thematic analysis and make up the review framework:
Structure
What is the representational structure and
notation for expressing contemporary
caremaps?
Content
What content types are consistently seen in
contemporary caremaps?
Development
What are the process steps followed for
developing contemporary caremaps?
6.1 Structure
As described in Table 1, caremaps have evolved from
wordy texts (Goode and Blegen, 1993; Gordon, 1996;
Holocek and Sellards, 1997; Bumgarner and Evans,
1999; Matula and Shollenberger, 1999; Philie, 2001)
to illustrative graphs (Chu and Cesnik, 1998;
Panzarasa et al., 2002; Houltram and Scanlan, 2004;
Li et al., 2014; Royall et al., 2014; Michelson et al.,
2018). Most contemporary caremaps present either as
monochromatic, i.e. black and white (Dickinson et
al., 2000; Chan et al., 2005; Ye et al., 2009;
Gopalakrishna et al., 2016) or full colour (Saint-
Jacques et al., 2005; Milne et al., 2013) flow
diagrams: a well-known process modelling tool
(Gilbreth and Gilbreth, 1921). Generally, each flow
diagram has its own boxes and notations, and the
most common is a rectangle that represents a process
step, usually called an activity. Contemporary
caremaps contain a set of activities representing
medical care processes. However, the literature
shows there is no consistency in the way that an
activity is represented. Different shapes such as
rectangular boxes with rounded (Thompson et al.,
2011) or square corners (Chu and Cesnik, 1998;
Panzarasa et al., 2002; Royall et al., 2014), plain text
(Dickinson et al., 2000), or even arrows
(Gopalakrishna et al., 2016) have been used. In some
cases, activities that lead to different mutually
exclusive pathways are presented by a diamond
(Panzarasa et al., 2002; Ye et al., 2009; van de
Klundert et al., 2010; Li et al., 2014). The flow from
one activity to another is illustrated with arrows
(Panzarasa et al., 2002; Houltram and Scanlan, 2004;
Chan et al., 2005; Milne et al., 2013), or simple lines
(Dickinson et al., 2000; Li et al., 2014). The literature
lacks a clear description as to whether a caremap
should have an entry and an exit point. In some cases
neither is present (Houltram and Scanlan, 2004;
Thompson et al., 2011; Royall et al., 2014), while in
others these points are an implicit (van de Klundert et
al., 2010; Li et al., 2014; Michelson et al., 2018) or
explicit part of the diagram (Panzarasa et al., 2002).
Finally, most of the reviewed caremaps contain
multiple pathways and they are often presented as
multi-level flow charts (Chu and Cesnik, 1998;
Panzarasa et al., 2002; Ye et al., 2009).
6.2 Content
Each activity in the caremap represents a specific
medical process. Diagnosis, treatment and ongoing
monitoring/evaluation are three medical activities
that are consistently observed (van de Klundert et al.,
2010; Thompson et al., 2011; Huang et al., 2012). It
is common for a caremap to contain a set of targeted
outcomes (Chu and Cesnik, 1998; Panzarasa et al.,
2002; Chan et al., 2005; Li et al., 2014; Royall et al.,
2014). Time, described either as a duration or inferred
from the step-by-step nature of the dynamic care
process, is often part of the caremap (Saint-Jacques et
al., 2005; Ye et al., 2009; van de Klundert et al., 2010;
Michelson et al., 2018). Finally, an explanation
Clinical Caremap Development: How Can Caremaps Standardise Care When They Are Not Standardised?
127
associated with the activities and/or arrows captured
in the caremap may be present (Houltram and
Scanlan, 2004; Chan et al., 2005; Saint-Jacques et al.,
2005), (Ye et al., 2009; Thompson et al., 2011; Milne
et al., 2013; Royall et al., 2014; Michelson et al.,
2018). The explanation helps to better describe an
activity or to justify the flow from one activity to
another.
6.3 Development Process
The development process of a contemporary caremap
is a subject that has gained significantly less attention
in the literature. Only 19 out of the 115 papers
provides any detail regarding the development
process. Of these only 6 describe the development
process with any deliberate nature or clarity (Giffin
and Giffin, 1994; Hydo, 1995; Thompson et al., 2011;
Huang et al., 2012; Lodewijckx et al, 2012). From the
rest, the steps to develop the caremap can only be
inferred (Hill, 1998; Dickinson et al., 2000; Panzarasa
et al., 2002; Royall et al., 2014).
7 TOWARDS
STANDARDISATION OF
CAREMAPS
7.1 Model for Standardised Caremap
Structure
Contemporary caremaps are presented as flow
diagrams. However, as described in Section 6.1 there
is neither a consistent caremap structure nor a good
representation of the elements included in a caremap.
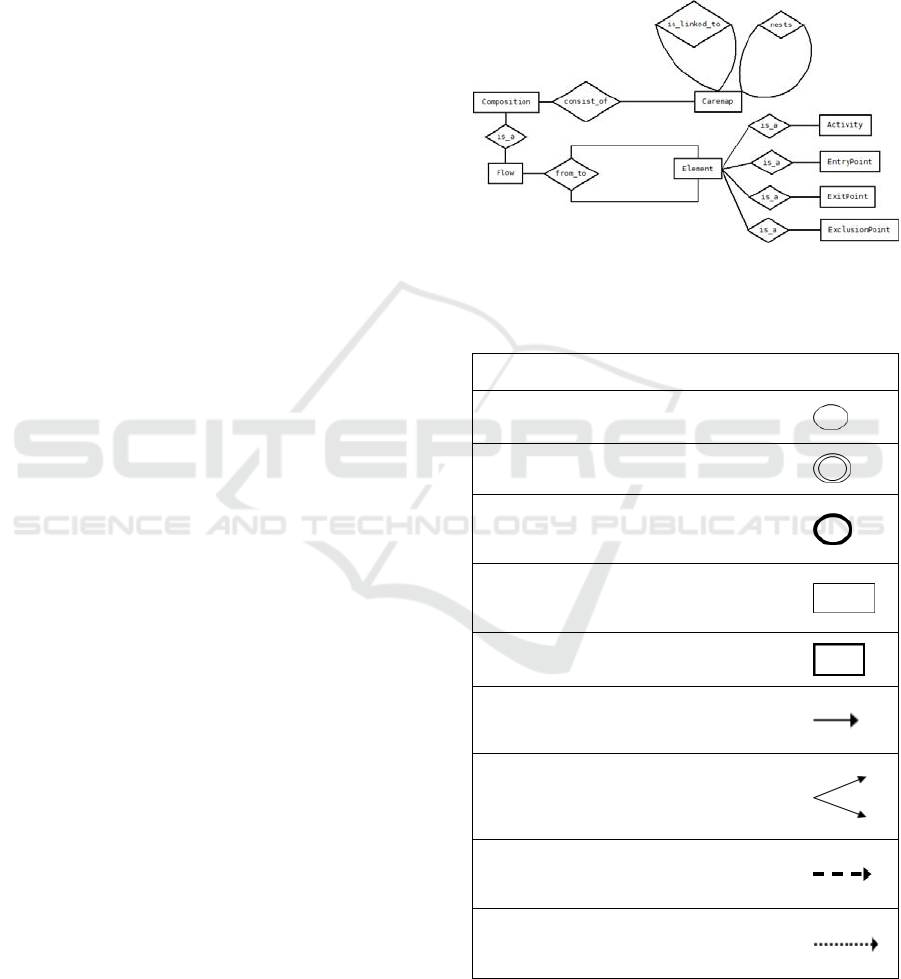
To resolve this problem an entity relationship model,
shown in Figure 2 that describes the relationship
among structural elements of a caremap,
demonstrated in Table 2, is proposed. The elements
are inspired by the standardised pictorial elements
seen in UML and hard state chart notations.
Following this, the standardised structural model of
the caremap is demonstrated in the content model
shown in Figure 3.
7.2 Model for Standardised Caremap
Content
The three main content types that were consistently
captured in the contemporary caremaps were
diagnosis, treatment and management/monitoring.
These are broad content types related to a set of
specific medical activities and data captured as shown
in Table 3. Following the structural model, an
exemplar content model is presented in Figure 3. The
three main content types represent different caremap
levels, while the described medical activities are the
components of that type of caremap. The proposed
standard content model represents the information
that should be captured in a caremap.
Figure 2: An Entity Relationship model for the caremap.
Table 2: Structural elements of caremaps and their
representational notation.
Element Descri
p
tion Notation
1
Entry
p
oint
Beginning of the caremap
2
Exit point End of the caremap
3
Exclusion
point
Exclusion from the caremap, as the
patient does not belong to the
tar
g
eted
p
o
p
ulation
4
Activity
A care or medical intervention that
is associated with a medical content
t
yp
e
(
see Table X in next section
)
5
Nested
Activity
An activity that has an underlying
caremap
6
Flow
Transition from one activity to
another
7
Multiple
pathways
Flow from an antecedent activity to
a number of successors from which
the clinician must choose the most
a
pp
ro
p
riate on
g
oin
g
p
ath
8
Nested
caremap
connection
Connection between an activity and
its nested caremap
9
Multi-level
caremap
connection
Connection between a series of
linked caremaps
HEALTHINF 2019 - 12th International Conference on Health Informatics
128

Figure 3: Content model for the caremap.
Table 3: Content type, activities and information captured
in caremap.
Content
Type
Activity
Data/Information
Captured
Diagnosis
Review patient records
Demographics
Medical histor
y
Collect patient history
Family history
Comorbidities
Ask personal, lifestyle
questions
Habits (risk factors)
Clinical examination
Signs
S
y
m
p
toms
Tar
g
eted exa
m
Dia
g
nostic test results
Disease assessment Dia
g
nosis
Treatment
Set
g
oals Ex
p
ected Outcomes
Consider different
interventions
Possible treatments
Consider potential
com
p
lications
Variances from expected
outcomes
Write prescription
Selected treatment
Treatment details
Monitoring
Review patient records
Previous test results
Previous s
y
m
p
toms
Clinical exa
m
Si
g
ns/S
y
m
p
toms
Tar
g
eted exa
m
Dia
g
nostic test results
Evaluate
g
oals Pro
g
ression
7.3 Model for Standardised Caremap
Development Process
Figure 4 presents the proposed development process
divided into six phases. During the initial phase the
conceptual framework should be decided, and a
multidisciplinary team assembled. The next phase
clarifies current practice and anticipated variance. A
review of available evidence is the final step prior to
production of the caremap. Once developed, it should
be evaluated and once agreed, implemented. As
Figure 4 shows, caremap development is a lifecycle
process. As new knowledge for the particular
condition or treatment or variance is identified, the
caremap should be reviewed (Huang et al., 2012).
Figure 4: Caremap development lifecycle.
Clinical Caremap Development: How Can Caremaps Standardise Care When They Are Not Standardised?
129
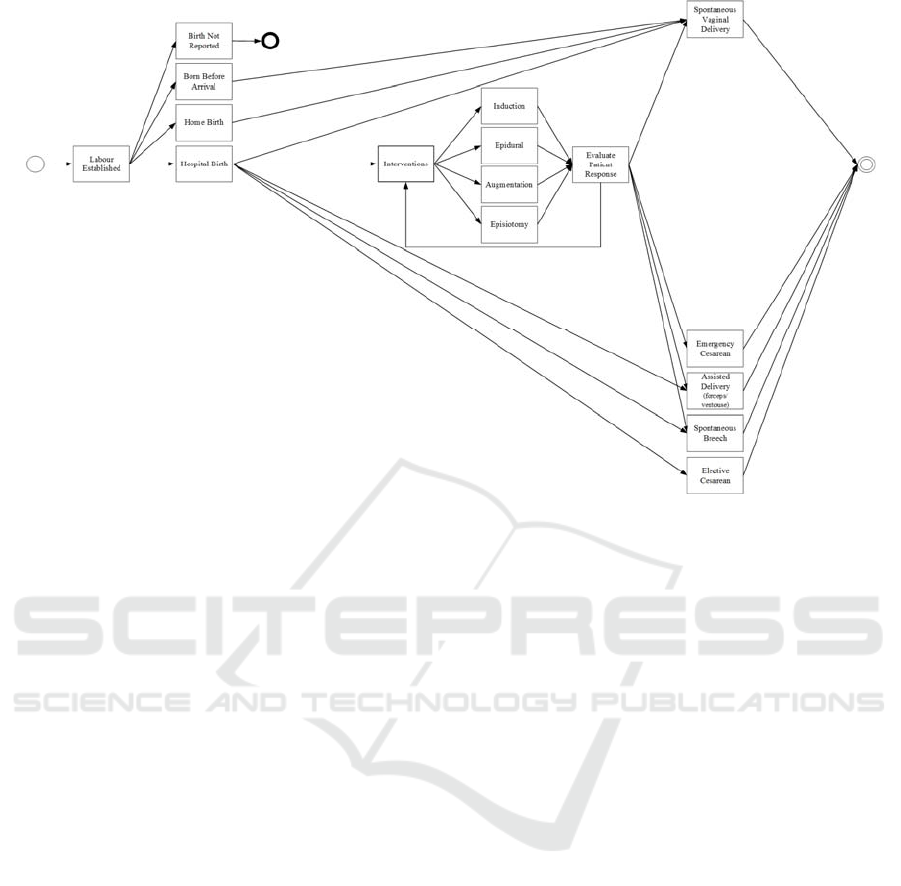
Figure 5: Labour and Birth Caremap.
8 EVALUATING THE
STANDARD
8.1 Study I: The Labour and Birth
Caremap
The labour and birth process represents an excellent
example for a first-pass evaluation case study to
assess the development process for caremaps. Labour
and birth has easily defined start and end points,
limited temporal variance, and a finite number of
easily identified treatment paths.
Inputs: Inputs for the labour and birth caremap were:
(a) clinical practice guidelines for intrapartum care at
Middlemore Hospital; (b) input and consensus of
midwives and obstetricians, and; (c) publicly
available incidence and treatment statistics from the
NZ Ministry of Health.
Development: An iterative development process
was used wherein the information scientist created an
initial version of the caremap based on the clinical
practice guideline (CPG) and evidence derived from
the treatment statistics. The initial caremap was
revised and refined during a number of sessions with
the clinicians. The resulting labour and birth caremap
for Middlemore Hospital is shown in Figure 5.
Validation: The Ministry of Health annually publish
Maternity and Newborn Data and Statistics for each
birthing unit and hospital. These statistics are
presented in the form of a contingency table whereby
the possible birthing outcomes and clinical
interventions are interrelated with a whole range of
demographic and clinical variables (maternal age at
birth, ethnicity, deprivation, maternal BMI and so
on). Using the 2014 release of these statistics, we
calculated the most likely treatment path that would
have been undertaken for all 8,731 birthing mothers
at one hospital unit. A state transition machine was
developed, digitised and realistic synthetic electronic
health records (RS-EHR) for all 8,731 women were
synthetically generated (McLachlan et al, 2016). The
treatment paths for each woman were digitally
compared against the caremap in Figure 5 to ensure a
valid path solution resolved for every recorded birth.
In this way we demonstrated that the caremap
represents the entire scope of patient presentations
and treatment options as performed by clinicians.
8.2 Study II: The Gestational Diabetes
Mellitus Management Caremap
As part of a project to design and build a population-
to-patient predictive learning health system (LHS) to
reduce clinical overuse and empower patients to
actively participate in their own care, Queen Mary
HEALTHINF 2019 - 12th International Conference on Health Informatics
130
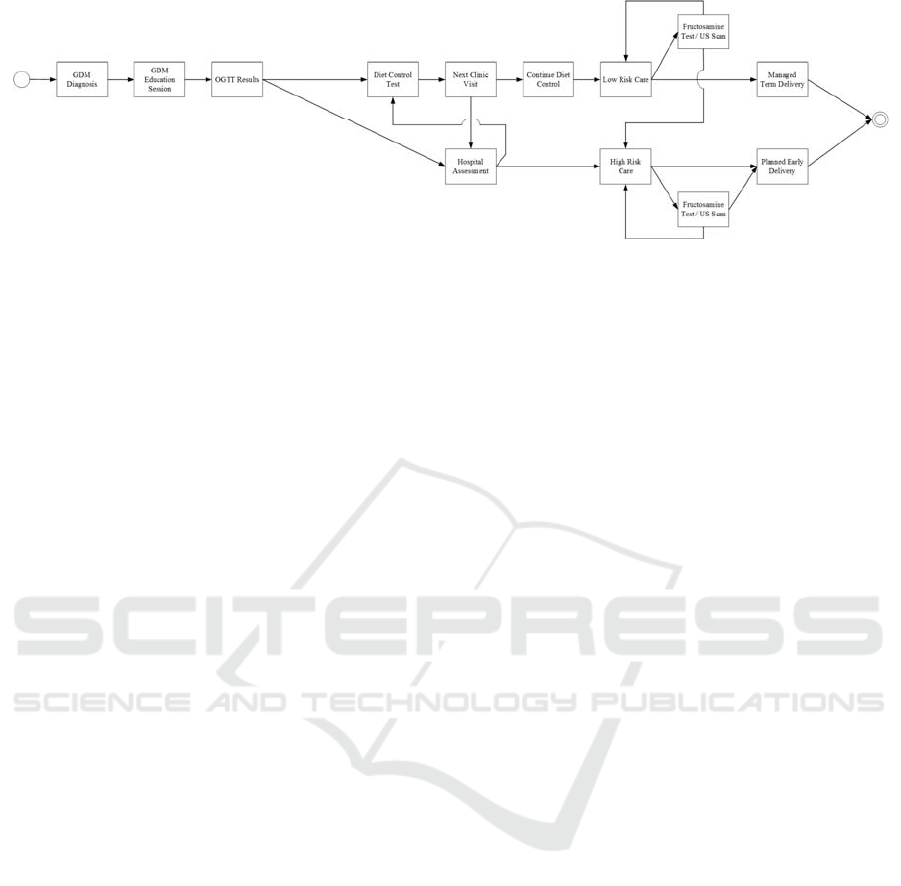
Figure 6: Gestational Diabetes Mellitus Management.
University of London’s PAMBAYESIAN project
(www.pambayesian.org) is creating a Bayesian
Network (BN) model (Fenton and Neil, 2018) to
predict treatment needs for individual mothers with
gestational diabetes mellitus (GDM). The process
initially required creation of three caremaps, for (1)
diagnosis; (2) management, and; (3) postnatal follow
up.
Inputs: Inputs for the labour and birth caremap were:
(a) clinical practice guidelines for care of women with
diabetes in pregnancy, and; (b) input and consensus
from midwives and diabetologists.
Development: An iterative development process
was used wherein the decision scientist and
midwifery fellow worked together to deliver an initial
version of the caremap based on the clinical practice
guidelines (CPG) and clinical experience. The initial
caremap was revised and refined during a number of
sessions with the clinicians. Figure 6 presents the
resulting clinical management caremap for GDM.
Validation: Validation was performed through
consultation seeking consensus from three
diabetologists with tertiary care experience treating
obstetric patients under the CPGs used in the
caremaps’ creation.
9 SUMMARY AND
CONCLUSIONS
Some see standardising of care as limiting their
ability to make decisions based on the patient
presenting before them, creating ‘cookie-cutter
medicine’. However, caremaps are a form of
standardised clinical documentation that improve
patient safety and outcomes while still allowing
clinicians to select the most appropriate path for their
patient. Caremaps evolved during the last three
decades from primarily text-based approaches
developed by nurses, to flow-based visual aids
prepared by doctors as representations of clinical
screening, diagnosis and treatment processes. These
contemporary caremaps are presented in a variety of
ways and with differing levels of content.
Contemporary caremaps lack standardisation.
This paper presents one solution for standardising
caremap structure and content, and an approach for
caremap development distilled directly from analysis
of the entire pool of literature. The development
process was evaluated and refined during the
development of caremaps for case studies in
obstetrics and midwifery: (a) labour and birth, and (b)
management of patients with GDM. The resulting
caremaps were validated by expert consensus, with
the labour and birth caremap also being developed as
a state transition machine enabling rapid digital
validation against a dataset of synthetic patients.
If used consistently, the methods presented in this
paper will bring standardisation to caremaps and
ensure that, as clinical staff move between busy units
in a tertiary care setting, they are not distracted from
the patient in effort to understand the care flow
model. Every caremap would be familiar and time can
be given over to treating their patient, not trying to
understand the document.
Future work should address a standard approach
for identifying and representing the decision points
within a caremap, digital imputation of the caremap,
and representation of caremap logic in other
computer-aware and algorithmic forms, including
Bayesian Networks or Influence Diagrams (Fenton
and Neil 2018). These can form part of a learning
health system and provide population-to-patient level
prediction.
ACKNOWLEDGEMENTS
SM, EK and NF acknowledge support from the
EPSRC under project EP/P009964/1:
Clinical Caremap Development: How Can Caremaps Standardise Care When They Are Not Standardised?
131

PAMBAYESIAN: Patient Managed decision-support
using Bayes Networks. KD acknowledges funding
and sponsorship for his research sabbatical at QMUL
from the School of Fundamental Sciences, Massey
University.
REFERENCES
Appleby, J., Raleigh, V., Frosini, F., Bevan, G., Gao, H., &
Lyscom, T. (2011). Variations in healthcare: The good,
the bad and the inexplicable. Report of The Kings
Fund.
BCCancer. (2012). Gallbladder: 3.Primary Surgical
Therapy. Sourced from: <http://www.bccancer.bc.ca/
books/gallbladder>.
Bero, L., Grilli, R., Grimshaw, J., Harvey, E., Oxman, A.,
& Thomson, M. (1998). Closing the gap between
research and practice: An overview of systematic
reviews of interventions to promote the implementation
of research findings. BMJ, 317(7156), 465-468.
Binks, C. (2017). Standardising the delivery of oral health
care practice in hospitals. Nursing Times, 113(11), 18-
21.
Blegen, M., Reiter, R., Goode, C., & Murphy, R. (1995).
Outcomes of hospital-based managed care: A
multivariate analysis of cost and quality. Managed
Care: Obstetrics and Gynaecology, 86(5), 809-814.
Bumgarner, S., & Evans, M. (1999). Clinical Care Map for
the ambulatory laparoscopic cholecystectomy patient.
Journal of PeriAnesthesia Nursing, 14(1), 12-16.
Cable, G. (1994). Integrating case study and survey
research methods: An example in information systems.
European Journal of Information Systems, 3(2).
Campbell, H., Hotchkiss, R., Bradshaw, N., & Porteous, M.
(1998). Integrated care pathways. BMJ: British Medical
Journal, 316(7125), 133.
Chan, E., Russell, J., William, W., Arsdell, G., Coles, J., &
McCrindle, B. (2005). Postoperative chylothorax after
cardiothoracic surgery in children. Annals of Thoracic
Surgery, 80, 1864-1871.
Cholock, L. (2001). Caremap for the management of
asthma in a paediatric population in a primary
healthcare setting. Thesis in fulfilment of the degree of
Master of Nursing, University of Manitoba, Canada.
Christian, C., Gustafson, M., Roth, E., Sheridan, T.,
Gandhi, T., Dwyer, K., Dierks, M. (2006). A
prospective study of patient safety in the operating
room. Surgery, 139(2), 159-173.
Chu, S., & Cesnik, B. (1998). Improving clinical pathway
design: Lessons learned from a computerised prototype.
Int. Journal of Medical Informatics, 51, 1-11.
Comreid, L. (1996). Cost analysis: Initiation of HBMC and
first CareMap. Nursing Economics, 14(1), 34.
Cook, J., Nuccetelli, D., Green, S., Richardson, M.,
Winkler, B., Painting, R., Skuce, B. (2013).
Quantifying the consensus on anthropogenic global
warming in the scientific literature. Environmental
Research Letters, 8(2).
Corbett, E. (2016). Standardised care vs. Personalisation:
Can they coexist? (Quality & Process Improvement,
Health Catalyst ed.). Available at:
<https://www.healthcatalyst.com/standardized-care-
vs-personalization-can-they-coexist> [Access date:
November 14, 2018].
deForest, E., & Thompson, G. (2012). Advanced nursing
directives: Integrating validated clinical scoring
systems into nursing care in the pediatric emergency
department. Nursing Research and Practice.
DeJesse, P., Bland, C., Fuller, O., & Macbride, J. (1995).
Managed care… A view from the inside. Medical
Marketing and Media, 30(5).
Dickinson, C., Noud, M., Triggs, R., Turner, L., & Wilson,
S. (2000). The antenatal ward care delivery map: A
team model approach. Australian Health Review, 23(3),
68-76.
Eisenhardt, K. (1989). Building theories from case study
research. Academy of Management Review, 14(4).
Etheredge, M. (1989). Collaborative care, Nursing Case
Management. American Hospital: Chicago Illinois.
Feigin, J. (1996). Medical Care Management. Allergy and
Asthma Proc, 17(6), 359-361.
Fenton, N., & Neil, M. (2018). Risk Assessment and
Decision Analysis with Bayesian Networks, 2nd Ed.
London, UK: CRC Press.
Gemmel, P., Vandaele, D., & Tambeur, W. (2008).
Hospital Process Orientation (HPO): The development
of a measurement tool. Total Quality Management &
Business Excellence, 19(12), 1207-1217.
Giffin, M., & Giffin, R. (1994). Market memo: Critical
pathways produce tangible results. Health Care
Strategic Management, 12(7), 17-23.
Gilbreth, F., & Gilbreth, L. (1921). Process Charts.
American Society of Mechanical Engineers, ARK:
/13960/t57d3tx71.
Goode, C., & Blegen, M. (1993). Developing a CareMap
for patients with a cesarean birth: A multidisciplinary
process. Journal of Perinatal and Neonatal Nursing,
7(2), 40-49.
Gopalakrishna, G., Langendam, M., Scholten, R., Bossuyt,
P., & Leeflang, M. (2016). Defining the clinical
pathway in cochrane diagnostic test accuracy reviews.
BMC medical research methodology, 16(1), 153.
Gordon, D. (1996). Critical pathways: A road to
institutionalizing pain management. Journal of Pain
and Symptom Management, 11, 252-259.
Griffith, D., Hampton, D., Switzer, M., & Daniels, J.
(1996). Facilitating the recovery of open-heart surgery
patients through quality improvement efforts and
CareMAP implementation. American Journal of
Critical Care, 5(5), 346-352.
Hampton, D. (1993). Implementing a managed care
Framework through Care Maps. Journal of Nursing
Administration, 23(5), 21-27.
Hill. (1998). The development of care management systems
to achieve clinical integration. Advanced Practice
Nursing Quarterly, 4(1), 33.
Holocek, R., & Sellards, S. (1997). Use of a detailed clinical
pathway for Bone Marrow Transplant patients. Journal
HEALTHINF 2019 - 12th International Conference on Health Informatics
132

of Pediatric Oncology Nursing, 14(4), 252-257.
Houltram, B., & Scanlan, M. (2004). Care maps: Atypical
antipsychotics. Nursing Standard, 18(36), 42-44.
Huang, B., Zhu, P., & Wu, C. (2012). Customer-Centered
Careflow Modeling Based on Guidelines. Journal of
Medical Systems, 36(5), 3307-3319.
Hubner, U., Flemming, D., Heitman, K., Oemig, F., Thun,
S., Diskerson, A., & Veenstra, M. (2010). The need for
standardised documents in continuity of care: Results
of standardising the eNursing summary. tudies in health
Technologies and Informatics, 160(2), 1169-1173.
Hydo, B. (1995). Designing an effective clinical pathway
for stroke. American Journal of Nursing, 95(3), 44-50.
Jones, A., & Norman, I. (1998). Managed mental health
care: Problems and possibilities. Journal of Psychiatric
and Mental Health Nursing, 5, 21-31.
Kehlet, H. (2011). Fast-track surgery: An update on
physiological care principles to enhance recovery.
Langenbeck’s Archives of Surgery, 396(5), 585-590.
Keyhani, S., Falk, R., Howell, E., Bishop, T., & Korenstein,
D. (2014). Overuse and systems of care: A systematic
review. Medical Care, 51(6).
Lee, A. (1989). A scientific method for MIS case studies.
MIS Quarterly, 33-50.
Leotsakos, A., Zheng, H., Croteau, R., Loeb, J., Sherman,
H., Hoffman, C., Munier, B. (2014). Standardisation in
patient safety: the WHO High 5’s project. Int. Journal
for Quality in Health Care, 26(2), 109-116.
Li, W., Liu, K., Yang, H., & Yu, C. (2014). Integrated
clinical pathway management for medical quality
improvement – based on a semiotically inspired
systems architecture. European Journal of Information
Systems, 23(4), 400-417.
Lodewijckx, C., Decramer, M., Sermeus, W., Panella, M.,
Deneckere, S., & Vanhaecht, K. (2012). Eight-step
method to build the clinical content of an evidence-
based care pathway: the case for COPD exacerbation.
Trials, 13, 229.
Mackay, D., Myles, M., Spooner, C., Lari, H., Typer, L.,
Blitz, S., Rowe, B. (2007). Changing the process of care
and practice in acute asthma in the emergency
department: Experience with an asthma care map in a
regional hospital. Canadian Journal of Emergency
Medicine, 9(5), 353-365.
Marr, J., & Reid, B. (1992). Implementing managed care
and case management: The neuroscience experience.
Journal of Neuroscience Nursing, 24(5), 281-285.
Martin, E. (2014). Eliminating waste in healthcare. ASQ
Healthcare Update, 14.
Matula, P., & Shollenberger, D. (1999). Total joint project:
Acute care to home care. Med-Surg Nursing, 8(2), 92.
McLachlan, S. (2017). Realism in Synthetic Data
Generation. A thesis presented in fulfilment of the
requirements for the degree of Master of Philosophy in
Science. School of engineering and Advanced
Technology, Massey University. Palmerston North,
New Zealand.
McLachlan, S., Dube, K., & Gallagher, T. (2016). Using the
Caremap with Incidence Statistics for Generating the
Realistic Synthetic Electronic Health Record.
Proceedings of the 2016 IEEE International Conference
on Health Informatics, ICHI’16.
Michelson, E., Huff, J., Loparo, M., Naunheim, R., Perron,
A., Rahm, M., . . . Berger, A. (2018). Emergency
Department Time Course for Mild Traumatic Brain
Injury Workup. he western journal of emergency
medicine, 19(4), 635-640.
Milne, T., Rogers, J., Kinnear, E., Martin, H., Lazzarini, P.,
Quinton, T., & Boyle, F. (2013). Developing an
evidence-based clinical pathway for the assessment,
diagnosis and management of acute Charcot Neuro-
Arthropathy: a systematic review. Journal of foot and
ankle research, 6(1), 30.
Morreale, M. (1997). Evaluation of a Care Map for
community-acquired pneumonia hospital patients.
Masters thesis. Queen’s University, Canada.
Ogilvie-Harris, D., Botsford, D., & & Hawker, R. (1993).
Elderly patients with Hip Fractures: Improving
outcome with the use of Care Maps with High-Quality
Medical and Nursing Protocols. Journal of Orthopaedic
Trauma, 7(5), 428-437.
O'Neill, E. S., & Dluhy, N. M. (2000). Utility of structured
care approaches in education and clinical practice.
Nursing Outlook, 48(3), 132-135.
Panzarasa, S., Maddè, S., Quaglini, S., Pistarini, C., &
Stefanelli, M. (2002). Evidence-based careflow
management systems: the case of post-stroke
rehabilitation. Computers and Biomedical Research,
35(2), 123-139.
Peak, D., Guynes, C., & Kroon, V. (2005). nformation
technology alignment planning: A case study.
Information and Management, 42.
Philie, P. (2001). Management of blood-borne fluid
exposures with a rapid treatment prophylactic caremap:
One hospital’s 4-year experience. Journal of
Emergency Nursing, 27(5), 440-449.
Potter, P. (1995). The uses of variance. In Z. K (Ed.),
Managing Outcomes though Collaborative Care: The
Application of CareMapping and Case Management.
American Hospital Publishing Inc.
Reading, S., Sanghi, A., Huda, B., Saravanamutha, J.,
Toms, G., Braggins, F., . . . McEaney, D. (2015).
Maternity Services: Diabetes - Pregnancy, Labour and
Peurperium. Barts Health NHS Trust, Barts Health.
Rotter, T., J, K., Koch, R., Gothe, H., Twork, S., van
Oostrum, J., & Steyerberg, E. (2008). A systematic
review and meta-analysis of the effects of clinical
pathways on length of stay, hospital costs and patient
outcomes. BMC Health Services Research, 8(265).
Royall, D., Brauer, P., Bjorklund, L., O’Young, O.,
Tremblay, A., Jeejeebhoy, K., . . . Mutch, D. (2014).
Development of a dietary management care map for
metabolic syndrome. Perspectives in Practice, 75(3),
132-139.
RWH. (2010). Bladder Management - Intrapartum and
Postpartum. The Royal Women’s Hospital, Guideline:
16/05/2017.
Sackman, J., & Citrin, L. (2014). Cracking down on the cost
outliers. Healthcare financial management, 68(3), 58-
63.
Clinical Caremap Development: How Can Caremaps Standardise Care When They Are Not Standardised?
133

Saint-Jacques H, B. V., J, W., Valcarcel, M., Moreno, P., &
Maw, M. (2005). Acute coronary syndrome critical
pathway: chest PAIN caremap: A qualitative research
study-provider-level intervention. Critical Pathways in
Cardiology, 4(3), 145–604.
Schwoebel, A. (1998). Care Mapping: A common sense
approach. Indian Journal of Pediatrics. Indian Journal
of Pediatrics, 65(2), 257-264.
Smithson, S. (1994). Information retrieval evaluation in
practice: A case study approach. Information
Processing and Management, 30(2).
Solsky, I., Edelstein, A., Brodman, M., Kaleya, R.,
Rosenblatt, M., Santana, C., . . . Shamamian, P. (2016).
Perioperative care map improves compliance with best
practices for the morbidly obese. Surgery, 160(6),
1682-1688.
Stumme, G. (2009). Formal Concept Analysis, in
Handbook on Ontologies. Springer: Berlin.
TCHaW. (2010). Abdominal Wall Defects in Neonates:
Initial, pre and post-operative management Practice
Guideline. The Children’s Hospital at Westmead,
Guideline No: 2010-0007 v2.
Tellis, W. (1997). Application of a case study methodology.
The Qualitative Report, 3(3).
Thompson, D., Berger, H., Feig, D., Gagnon, R., Kader, T.,
Keely, E., Vinokuruff, C. (2013). Clinical Practice
Guidelines: Diabetes and Pregnancy. Canadian Journal
of Diabetes, 37, S168-S183.
Thompson, G., deForest, E., & Eccles, R. (2011). Ensuring
diagnostic accuracy in pediatric emergency medicine.
Clinical Pediatric Emergency Medicine, 12(2), 121-
132.
Vaismoradi, M., H, T., & Bondas, T. (2013). Content
analysis and thematic analysis: Implications for
conducting a qualitative descriptive study. Nursing and
Health Sciences, 15(3), 398-405.
Valenstein, P. (2008). Formatting pathology reports:
applying four design principles to improve
communication and patient safety. Archives of
Pathology and Laboratory Medicine, 132(1), 84.
van de Klundert, J., Gorissen, P., & Zeemering, S. (2010).
Measuring clinical pathway adherence. Journal of
Biomedical Informatics, 43(6), 861-872.
WAHealth. (2013). Diagnostic Imaging Pathways:
Bleeding (First Trimester). Imaging Pathways, Western
Australia Health.
Wang, L., Miller, M., Schmitt, M., & Wen, F. (2013).
Assessing readability formula differences with written
health information materials: Application, results, and
recommendations. Research in Social and
Administrative Pharmacy, 9(5), 503-516.
Wilson, D. (1995). Effect of managed care on selected
outcomes of hospitalised surgical patients. Thesis in
fulfilment of the degree of Master of Nursing,
University of Alberta, Canada.
Yazbeck, A. (2014). Reengineering of business functions of
the hospital when implementing care pathways.
Doctoral Dissertation, Faculty of Economics,
University of Ljubljana.
Ye, Y., Jiang, Z., Diao, X., Yang, D., & Du, G. (2009). An
ontology-based hierarchical semantic modeling
approach to clinical pathway workflows. Computers in
biology and medicine, 39(8), 722-32.
Yin, R. (2011). Applications of Case Study Research. Sage
Publications.
Zander, K. (1992). Quantifying, managing and improving
quality: Part 1: How CareMaps link C.Q.I. to the
patient. The New Definition, 1-3.
Zander, K. (2002). Integrated care pathways: Eleven
international trends. Journal of Integrated Care
Pathways, 6, 101-107.
Zarzuela, S., Ruttan-Sims, N., Nagatakiya, L., &
DeMerchant, K. (2015). Defining standardisation in
healthcare. Mohawk Shared Services, 15.
HEALTHINF 2019 - 12th International Conference on Health Informatics
134
