
An Italian Business Case for an eHealth Platform to Provide Remote
Monitoring and Coaching Services for Elderly with Mild Cognitive
Impairment and Mild Dementia
Monika Jurkeviciute
1
, Lex van Velsen
2
, Pietro Davide Trimarchi
3
, Ladan Sarvari
4
and Fabrizio Giunco
3
1
Centre for Healthcare Improvement, Chalmers University of Technology, Vera Sandbergs allé 8, Gothenburg, Sweden
2
Telemedicine cluster, Roessingh Research and Development, Roessinghsbleekweg 33b, Enschede, The Netherlands
3
IRCCS Fondazione Don Carlo Gnocchi, Via Don Luigi Palazzolo 21, Milan, Italy
4
Jonköping International Business School, Jönköping University, Gjuterigatan 5, Jönköping, Sweden
fgiunco@dongnocchi.it
Keywords: Business Case, eHealth Platform, Mild Cognitive Impairment, Mild Dementia, Elderly.
Abstract: The purpose of this study was to define a business case for an eHealth platform to provide remote monitoring
and coaching services for elderly with mild cognitive impairment and mild dementia in the Italian context.
107 patients with mild cognitive impairment and mild dementia were divided into the intervention and control
groups. The data was collected using standardized instruments Clinical Dementia Rating Scale (CDR) and
EuroQoL-5D-5L, and tailor-made instruments, such as surveys to technology and healthcare providers, and
semi-structured interviews to patients and healthcare professionals. The data that was not collected in the
study, was obtained from the scientific literature. Benefit/cost ratio was calculated for three years. The study
shows that a digital platform to provide remote monitoring and coaching services for elderly with mild
cognitive impairment and mild dementia can be cost-effective from the first year, and can improve care
without monetary loss for the healthcare provider. The key benefits show that the deterioration of the illness
is postponed, and that the satisfaction of the patients and the healthcare professionals increases. Therefore,
such an eHealth platform can be a worthy investment in Italy, and could be considered for wider nation-wide
adoption.
1 INTRODUCTION
The number of people living with dementia increases.
It is currently estimated to affect more than 40 million
people globally, whose care generates more than 800
billion USD in cost (Prince et al., 2015). This growth
will continue to strain healthcare systems worldwide.
One solution to cope with this situation could be to
widely use digital technologies (hereafter – eHealth)
that aim to improve outcomes (both clinical and
quality of life) and to save costs. While there is a
growing body of literature that examines effects of
eHealth to elderly patients with various levels of
severity of cognitive impairment, adoption of eHealth
into routine care is lagging (Swinkels et al., 2018).
One barrier concern limited resources in healthcare.
eHealth initiatives compete against one another and
other options for investment, while the return-on-
investment for this type of eHealth service remains
unclear. Before allocating funds, decision-makers
will create a thorough overview of which investments
can maximize impact on health and efficiency. If the
business case for eHealth in this context remains
vague, its adoption will falter.
Different reviews (Goldzweig et al., 2009; Kim et
al., 2017) reported a lack of published evaluations of
costs and benefits of eHealth implementations. A
similar gap of missing cost-benefit evaluations has
been noted for technology implementations in the
area of dementia (Westphal et al., 2010). Still in 2016,
it was reported that majority of the evaluations of
technology for people with dementia focus on usage,
usability, and adoption (Knapp et al., 2016). The
paucity of economic data is one of the biggest barriers
to the creation of business cases that are essential for
eHealth adoption.
28
Jurkeviciute, M., van Velsen, L., Trimarchi, P., Sarvari, L. and Giunco, F.
An Italian Business Case for an eHealth Platform to Provide Remote Monitoring and Coaching Services for Elderly with Mild Cognitive Impairment and Mild Dementia.
DOI: 10.5220/0007657700280037
In Proceedings of the 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2019), pages 28-37
ISBN: 978-989-758-368-1
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

A business case, as defined by Gambles (2017, p.
1), is “A recommendation to decision makers to take
a particular course of action for the organization,
supported by an analysis of its benefits, costs and
risks compared to the realistic alternatives, with an
explanation of how it can best be implemented”. In
this paper, we describe a business case for investment
in an eHealth platform to provide remote monitoring
and coaching services for elderly with mild cognitive
impairment (MCI) and mild dementia (MD). We
examine whether it could improve quality of care by
enhancing care outcomes and saving costs in Italy.
Hereby, we aim to add knowledge to the scarce body
of literature on which eHealth interventions have a
positive business case.
2 RELATED WORK
Cost-effectiveness or business case development
studies of non-pharmacological eHealth interventions
for treating MCI and MD are scarce. Most eHealth
studies have focused on clinical and social outcomes
(e.g. Van Mierlo et al., 2015; Ben-Sadoun et al.,
2016) and have shown positive outcomes to
caregivers, such as relatives, healthcare professionals,
or a healthcare organization. Less evidence is
available on clinical effectiveness of eHealth for the
elderly patients themselves, with various levels of
severity of cognitive impairment (Knapp et al., 2016).
Similarly, there are cost-effectiveness studies that
focus on non-pharmacological interventions without
involvement of eHealth (e.g. Gitlin et al., 2010; Willis
et al., 2018). The following paragraphs will
summarize the cost-effectiveness outcomes of non-
pharmacological eHealth interventions, obtained
from a small number of published studies.
The ISISEMD (Intelligent System for
Independent living and Self-care of seniors with
cognitive problems or Mild Dementia) project
introduced assistive technology for elderly people
with mild dementia living in the community. The
business case concluded that the system can only be
sustainable if provided at a large scale, at the level of
municipality or region (Mitseva et al., 2009).
On a general level, an economic modelling study
for dementia conducted by Knapp et al. (2016)
modelled three scenarios. The first scenario
considered postponement of care home admission. It
assumed that assistive and safety technologies can
delay care home admissions by 8 months (based on
Riikonen et al., 2010). Under this scenario, the
technology intervention would be cost-effective if it
postponed care home admissions by 8 months, and
reduced hours spent on care by the informal caregiver
by 20%. The second scenario considered reduction of
career’s stress. Impact in quality-adjusted life years
(QALY) was examined. It was assumed that
technology could reduce career’s stress and improve
career’s quality of life by 0,05 EQ-5D tariff that lasts
for 3 years (time of patient’s living in a community).
The technology intervention would be cost-effective
if it cost less than 13.000 British pounds, delayed care
home admissions by 8 months, reduced career’s
weekly hours by 15%, and increased career’s quality
of life by 0,05 QALY per year. The third scenario
aimed to find out how much benefit that is relative to
costs, the technology needs to generate in order to be
deemed cost-effective (from societal and health
perspectives). It was considered that the technology
costs 5000 British pounds over 4.5 years (time of
patient’s living in a community). Under this scenario,
the technology intervention would be cost-effective if
it postponed care home admission by 3 months and
reduced career’s weekly hours by 8%, and increased
career’s quality of life by 0,06-0,08 QALYs per year.
As it can be seen from the overview of the related
work, the cost-effectiveness studies on eHealth
intervention in dementia care are fragmented and
have not reached saturation of knowledge. It is
challenging to draw conclusions from the published
studies not only because the types of eHealth
analyzed are different and applied in different
contexts, but also the pace of technology
development is fast and monetary values (e.g. prices,
hourly tariffs) fluctuate over time. This leads to a
need for more cost-effectiveness studies related to
eHealth interventions in dementia care.
3 MATERIAL AND METHODS
3.1 Empirical Study
The business case was developed within a 3-year
project “Digital Environment for Cognitive
Inclusion” (DECI) funded by the European Union
(EU). The study was carried out in four countries, and
the study design was comparative, randomized,
stratified and prospective. The case analyzed in this
paper focuses on a business model to provide in-
house remote assistance services in the Italian
context, promoting independent living for elderly
people diagnosed with mild cognitive impairment and
mild dementia. The population was divided into an
intervention group and a control group. In Italy, 53
persons were randomized into the intervention group
(10 dropped-out), and 54 persons in the control group
An Italian Business Case for an eHealth Platform to Provide Remote Monitoring and Coaching Services for Elderly with Mild Cognitive
Impairment and Mild Dementia
29
that followed care as usual (5 dropped-out). The
intervention lasted for 6 months. Measurements took
place at a baseline and after 6 months.
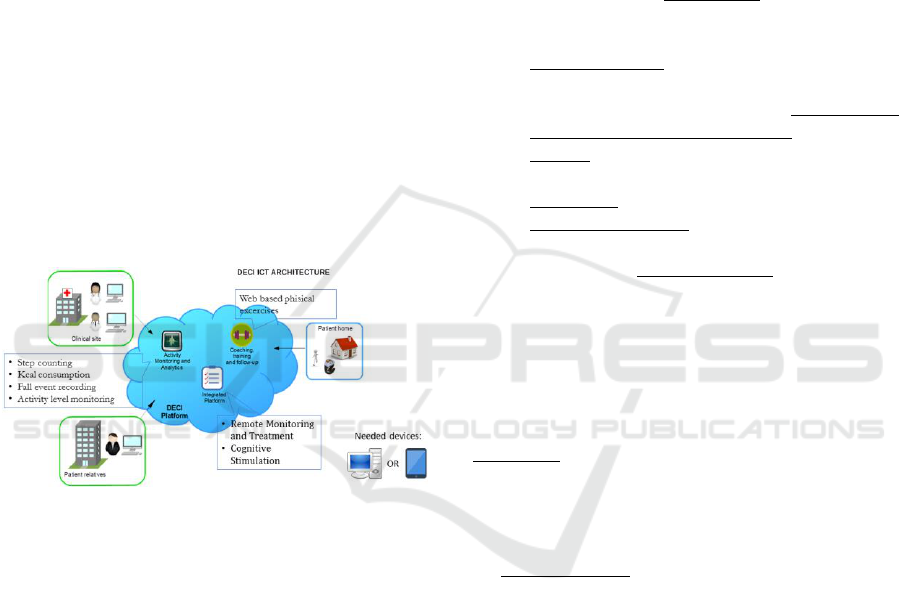
The Intervention group received a technology-
supported DECI care model, consisting of:
1. An integrated platform, installed on a tablet
that enables professionals to share information
about the patients, as well as patient-to-
professional communication.
2. Web-based physical and cognitive exercise
applications (an OTAGO-based falls
prevention program by Roessingh Research
and Development (The Netherlands) and
SmartBrain (Spain).
3. An activity monitoring system, supported by a
wearable device that records the number of
steps and the duration of active hours
throughout the day (Adamo watch by Consoft
Sistemi s. p. a.).
4. A case manager, in Italian case a social worker,
responsible for coordinating the care,
introducing and supporting a patient in using
the technology.
Figure 1: The DECI services.
The inclusion criteria for patients:
1. Age ≥ 60
2. Diagnosis of MCI or diagnosis of
Dementia according to DSM V criteria
3. Clinical Dementia Rating (CDR) ≤ 1
4. Living at home
5. Ability to provide informed consent or
availability of a proxy for informed
consent
3.2 Business Case Creation
The approach towards creating the business case was
based upon the TNO Business case model for
innovation in long-term care, created by an
organization TNO that aims to assess an innovation
and to demonstrate its value to government and
industry. The approach allows a multi-dimensional
assessment of changes in variables before and after
introduction of the innovation, and is intended to
inform decision makers of the added value of the
innovation.
The business case development starts with the
description of the innovation (also called as
boundaries of the innovation in the TNO approach).
Then, risks are discussed. Afterwards, it is necessary
to determine which of the variables are relevant to the
investigation and how to obtain the data. Variables
proposed by TNO to assess the before and after
situations include:
The cost of spent time by healthcare
professionals.
Consequences of using the innovation on the
quality of care (e.g., patient satisfaction,
quality of life, safety).
The impact of the innovation on prevention or
postponement of the health issue.
Income generated by providing the service
based on the innovation.
Investment for starting the innovation.
Operating expenses for using the innovation,
after initial investment.
Changes in quality of work by healthcare
professionals (e.g., job satisfaction)
In this study, we approached the business case from
the perspective of the healthcare organization (in this
case, a Memory clinic).
3.3 Data Collection and Analysis
Spent time (operationalized as the cost of time spent
by healthcare professionals for direct treatment) was
collected via a survey to the healthcare provider. A
total number was calculated by multiplying the
number of spent hours by the applicable hourly tariff.
Quality of care consisted of the time spent on
multi-disciplinary meetings for defining and refining
treatment plans, patient satisfaction, safety, and
quality of life. Data for time spent on multi-
disciplinary meetings for defining and refining
treatment plans was collected via a survey to the
healthcare provider. A total number was created by
multiplying the number of spent hours by hourly
tariffs. Multi-disciplinary team meetings and
refinement of care plans were not applicable to a
control group. Patient satisfaction was assessed via
semi-structured interviews with patients (purposeful
sample of n=10 for the intervention group and n=10
for the control group). Data was thematically
analyzed. Data regarding willingness to use the DECI
services in the future was collected through a
willingness-to-pay survey to the patients and their
informal caregivers. Third, quality of life of the
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
30

patients was assessed using a questionnaire
EuroQoL-5D-5L (EuroQoL Group, 1990; Wolfs et
al., 2007; Janssen et al., 2013). Data was analyzed
using SPSS software, Chi-square and one-way Anova
statistical tests. The confidence level was set at 0.05.
Safety data was collected using qualitative semi-
structured interviews with the patients of the
intervention group (n=10) supplemented by semi-
structured interviews with healthcare professionals
(n=4). Since safety aspects concerned the DECI
solution, this element was not applicable to a control
group. Data was thematically analyzed.
Prevent and postpone care consists of prevention
of falls due to the DECI services and postponement
of mild dementia. Since the falls data were not
collected in the project, assumptions were extracted
from relevant literature. People above 65 years fall,
on average, 0.33 times per year (Gillespie et al.,
2012). 9% of the falls require a GP visit, and 5% of
the falls lead to an emergency visit (Berg et al., 1997).
3% of the falls end in a fracture (assumed by the
project team). Completion of the OTAGO program
leads to prevention of 68% of falls (Thomas et al.,
2010). During analysis, a number of falls prevented is
calculated (% of falls prevented (68%) multiplied by
a targeted population size). Then, the total saved cost
due to prevented falls is calculated by summing up:
a) prevented GP consults (a number of falls prevented
multiplied by 9% and by the cost of a single GP
consult; b) prevented emergency room visits (a
number of falls prevented multiplied by 5% and by
the cost of a single emergency room visit; c)
prevented fractures (a number of falls prevented
multiplied by 3% and by the cost of a fracture
treatment. Data for the cost of a GP consult (15
euros), an emergency room visit (241 euros), and a
fracture treatment (2949 euros) were obtained
through a survey to the healthcare provider.
Data for postponement of mild dementia was
collected using Clinical Dementia Rating Scale
(CDR) (Morris et al., 1997) on patients at the baseline
and follow-up. Annual costs of treating MD were
obtained through a survey to the healthcare provider
and equals to 18.941 euros. During analysis, a
proportion of people who converted from MCI to MD
was calculated using changes in CDR from baseline
to follow-up. The conversion rate was assumed to
stay stable after 12 months. The saved costs due to the
postponement of MD were calculated by multiplying
the following elements: conversion rate from MCI to
MD, annual target population, and annual MD
treatment costs.
Income of a healthcare provider consists of annual
insurance reimbursement for healthcare services
provided. Data was obtained through a survey to the
healthcare provider. Hypothetical income related to
willingness to pay by a patient or an informal
caregiver was collected through a survey to the
patients and their informal caregivers. Data was
analyzed by calculating the average amounts that
would be paid by the patient or the informal
caregiver.
Investment relates to the cost of personnel for
server installation and configuration related to the
DECI services. Data was obtained through a survey
to the healthcare provider.
Operating expenses refer to the annual operating
expenses for the technology in the DECI services, to
be incurred by the healthcare provider (usage fees,
hardware, servers, maintenance, helpdesk, etc.). Data
was obtained through a survey to the technology
providers and the healthcare provider. Usage fees for
all the technologies are constant, except for the
smartwatch fee, which increases with the size of
patient population.
Quality of work refers to the satisfaction of
healthcare professionals using the innovation. Data
was obtained through semi-structured interviews with
the healthcare professionals (n=4). Same
professionals were involved in the care of the
intervention and control groups. Data was
thematically analyzed.
All benefits and costs that were possible to
convert into monetary magnitudes were entered into
the model which was set up in the MS Excel. Then,
the ratio between the monetary benefits and costs of
implementing DECI services were calculated for
situations after year 1, year 2, and year 3.
Ratio = Benefits / Costs
(1)
Consideration of all outcome categories determine
whether or not implementing the DECI service is a
worthy investment. The business case for the usual
care in the control group equals to zero, since several
categories of evaluation that result in monetary values
are not applicable, while other categories of costs and
benefits compensate each other. First, the usual care
does not involve technology innovation, which makes
the categories of investment and operating expenses
not applicable. Second, prevention of MD, GP
consults, falls, emergency room visits, and fractures
concern the innovation introduced, and are not
applicable to the control group. The only applicable
methodological categories that result in monetary
values are spent time and income. However, the cost
of time spent by the professionals are reimbursed
(income). Therefore, the business case for the usual
An Italian Business Case for an eHealth Platform to Provide Remote Monitoring and Coaching Services for Elderly with Mild Cognitive
Impairment and Mild Dementia
31
care in the control group equals to zero. However,
non-monetary qualitative results for the control group
are discussed, where applicable.
4 RESULTS OF A BUSINESS
CASE IN ITALY
In Italy, healthcare services are free-of-charge and
funded from tax payments. DECI services were an
extension of service offered by Centers for Cognitive
Disorders and Dementia in the region of Lombardy
(Milan) which have a primary responsibility to
diagnose and assess the stage of illness and to
determine the therapy. Every patient that met the
inclusion criteria visited the healthcare professionals
two times at the Memory Clinic of Istituto Palazzolo,
Fondazione Don Carlo Gnocchi Onlus (FDG) in
Milan: for inclusion and follow-up. Five
professionals were involved in the DECI services: a
geriatrician, two neuropsychologists, a social worker
(also acting as a case manager), and an engineer. The
case manager was engaged full-time in the study and
had a role to coordinate patient’s care with other
professionals, to answer the incoming messages
through the DECI platform, to check patient’s
adherence to prescribed physical and cognitive
therapies, to send reminders, to monitor the status of
the battery of the smartwatch, and to organize its
replacement. The geriatrician worked with tailoring
the physical activity program to fit the specific needs
of the patients. The neuropsychologists designed
therapies delivered via the cognitive stimulation
program.
It is important to note that we evaluate the
intervention as a whole, i.e. organizational and
therapeutic inputs, and not just technology.
Therefore, the outcomes reported cannot be attributed
to the technology only.
Table 1 shows the demographics of the patients
included in the study.
Projected Population Size
Based on the estimation of the project team, the
population size in Italy can be targeted at 100 patients
for year 1, 150 patients for year 2, and 175 patients
for year 3.
Table 1: Patient characteristics at baseline.
Intervention group
N=53
Age
77.64±5.27
Gender (F/M)
27/26
Diagnosis (MCI/MD)
39/14
MCI type (Amn/N-Amn)
19/20
Education years
9.21±4.27
MMSE (range 0-30)*
26.56±2.87
CDT (range 0-5)*
3.30±1.38
ADL *
5.64±0.92
I-ADL*
6.13±2.19
Control group
N=54
Age
78.98±5.98
Gender (F/M)
31/23
Diagnosis (MCI/MD)
36/18
MCI type (Amn/N-Amn)
16/20
Education years
9.02±4.15
MMSE (range 0-30)
26.18±2.96
CDT (range 0-5)
3.13±1.33
ADL
5.59±0.81
I-ADL
6.09±2.09
*CDT = Clock drawing test (Shulman, 2000)
MMSE (Mini-Mental State Examination) (Folstein et al.,
1975)
ADL (Activities of Daily Living) (Katz et al., 1970)
I-ADL (Instrumental Activities of Daily Living)
(Lawton et al., 1969)
4.1 Benefits
Prevent and Postpone Care
16% of the control sample and 6% of the intervention
sample converted to MD at a follow-up after 6
months. The rate of conversion is quite high since the
samples are small and the mean age of the patients in
the study was high, which affected the rate of
conversion (Visser et al., 2006). Hence, the data
shows that 10% fewer MCI patients converted to MD
in the intervention group, compared to the control
group. The costs that are prevented using the DECI
services relate to 10% additional prevention from
turning from MCI to MD. Hence, the preventable
costs equal to 196.337,16 euros in year 1. Every
consecutive year, the prevented costs rise due to a
rising number of patients who would use the DECI
services. The prevented cost in year 2 equals to
294.505,74 euros and 343.590,03 euros in year 3.
Income
Italian healthcare system does not reimburse the costs
incurred by using eHealth. Therefore, insurance
reimbursement would not differ between the DECI
services and usual care. In this study, income in the
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
32

intervention group will be interpreted as the insurance
reimbursement for the time spent by the healthcare
professionals providing usual care, and equals to
26.458 euros in year 1, 39.687 euros in year 2, and
46.301,50 euros in year 3.
Willingness-to-pay analysis showed that 60% of
the patients in the intervention group were willing to
pay, on average, 47 euros monthly for the DECI
services. It comprises, on average, 28,20 euros per
patient. 70% of their informal caregivers were willing
to pay, on average, 33 euros monthly. It comprises,
on average, 23,10 euros per informal caregiver.
However, the income that would come from the
patients or informal caregivers is not included in the
business case analysis in this study, since healthcare
is supposed to be free-of-charge in Italy.
Patient Satisfaction
All the control group patients expressed trust in
competence of the professionals and appreciated kind
approach that made them feel good. However, one
patient disliked to be charged for the visits, two
patients thought that the waiting time between a
contact and a visit was too long, and one patient found
the process too bureaucratic.
Patients in the intervention group perceived that
the key strengths of the DECI services were the
simplicity of its features and the stimulating physical
and cognitive exercises that helped them keep active.
The main challenges concerned starting using the
DECI technology and to learn navigating it.
Therefore, an IT helpdesk was identified as a
necessary addition to the service, that could reduce
the need for clinical staff and family members to
provide extra time for helping the patients learn the
IT system (a helpdesk is estimated to cost 10.800
euros for a population of 100 patients in year 1). Also,
the difficulty level of the physical and cognitive
exercises needs to be customized, based on the state
of the condition of the patient. The exercises were
often perceived as too easy. Since the cognitive and
physical training systems contain various levels of
difficulty, it was deemed to be a learning point for
clinical staff to select the right level for the patient.
Design and size of the activity monitoring device (a
wrist watch) needs to be improved to better suit the
routines and aesthetic preferences of the elderly
population (the watch was deemed to make people
feel they look sick, and the design was too youthful).
A willingness-to-pay survey showed that 83% of
the patients and 86% of the informal caregivers are
willing to use the DECI services in the future. Also,
90% of the patients and 89% of their informal
caregivers would recommend DECI to others.
Quality of Life
Analysis of proportions in each dimension, inside of
each group, to locate changes between the baseline
and the follow-up, did not yield statistically
significant results. In the intervention group: mobility
𝜒
2
(1)=0,051, p=0.822; self-care 𝜒
2
(1)=0,212,
p=0,645; usual activity 𝜒
2
(1)=0,080, p=0,777;
pain/discomfort 𝜒
2
(1)=0,720, p=0,396; anxiety
𝜒
2
(1)=0, p=1. In the control group: mobility
𝜒
2
(1)=0,809, p=0.368; self-care 𝜒
2
(1)=1,359,
p=0,244; usual activity 𝜒
2
(1)=0,970, p=0,325;
pain/discomfort 𝜒
2
(1)=2,256, p=0,133; anxiety
𝜒
2
(1)=1,142, p=0,285.
Analysis of changes in the EQ visual analogue
scale (VAS) between the baseline and follow-up did
not yield statistically significant results too:
intervention group p=0,450; control group p=0,910.
In-between groups analysis using one-way Anova to
locate a difference between the control and the
intervention groups did not yield statistically
significantly results, p=0,558.
Analysis of EQ index values used a Spanish value
set. Analysis of changes in the index values between
the baseline and the follow-up in each group did not
yield statistically significant results: intervention
group p=0,458; control group p=0,075. In-between
groups analysis of the index values using one-way
Anova to locate a difference between the control and
intervention groups did not yield statistically
significantly results, p=0,219. Intervention group,
mean QALY=-0,0139± 0,0903; control group, mean
QALY=-0,0448636±0,1404.
Quality of Work
In Italy, both groups were attended by the same
healthcare professionals involved in the study. All the
professionals indicated that introducing the case
manager role was highly beneficial, since it is a
dedicated contact person guiding the patients and
answering their questions. The role was deemed
useful for strengthening relationships between the
patients, informal caregivers, and healthcare
professionals. Professionals also appreciated the
infrastructure and technological features of DECI,
especially the ability to monitor the exercise and
performance of the patients remotely.
The DECI study demanded healthcare
professionals to spend, on average, 29,3 hours per
week. All the professionals reported an increased
workload, but it was deemed to be related to the
administration of the study. However, the quality of
work was perceived to have increased due to the
higher empowerment of the professionals by being
able to provide patients with useful tools. Healthcare
An Italian Business Case for an eHealth Platform to Provide Remote Monitoring and Coaching Services for Elderly with Mild Cognitive
Impairment and Mild Dementia
33

professionals also reported to have increased their
knowledge about cognitive impairment and patients’
statuses and needs. Moreover, the DECI services
made it easier to work cross-functionally through
facilitated data sharing in the DECI platform.
4.2 Costs
Spent Time and Quality of Care in Italy concerned the
following professional categories engaging with the
DECI services and multi-disciplinary meetings
(please note that this time does not overlap): doctor,
nurse practitioner, physiotherapist, technician, case
manager, psychologist. In total, the cost of time spent
by the professionals for the intervention group is
projected to 66.325,27 euros in year 1, 99.487,90
euros in year 2, and 116.069,22 euros in year 3. The
cost of time spent by professionals for the control
group is projected to 26.458 euros in year 1, 39.687
euros in year 2, and 46.301,50 euros in year 3.
Average costs per patient remain stable.
Investment (one-time) for the DECI services is
relatively small on the side of the hospital. The
investment includes the cost of staff of 140 euros for
establishing the ICT infrastructure.
Operating Expenses consist of the annual usage fees
for the DECI technology and the operating costs for
hosting the technology in the hospital.
The annual usage fee for all DECI technologies is
52.100 euros (including tax). The highest fee is paid
to the smartwatch provider due to the lease of
hardware. The usage fee for year 2 equals to 70.400
euros, and 79.550 euros for year 3.
The annual operating costs for all DECI
technologies equal to the total of 74.646 euros in year
1 and consists of the cost related to purchasing the
hardware (depreciation in 12 months), server hosting,
configuration of the tablets, personnel cost for
maintenance and helpdesk, licenses, 4G connectivity.
The annual operating costs for year 2 equals to
101.496 euros, and 114.921 euros for year 3.
Total annual operating expenses of the DECI
technology equal to 126.746 euros for year 1, then
171.896 euros for year 2, and 194.471 euros for year
3.
4.3 Safety
The majority of the interviewed patients and
healthcare professionals did not express any concerns
or observations the DECI services might be not safe.
However, two safety-related risks were reported.
First, the physical activity program OTAGO might
require supervision for an older population. One
healthcare professional expressed concerns that some
exercises put too high pressure on these patients. One
patient has also mentioned that some interaction with
a professional during the exercise session would have
been helpful, in order to make sure the exercises are
performed in a safe way. Second, one patient reported
that Adamo activity monitoring sensor caused an
allergic reaction to nickel and plastic.
4.4 Benefit/Cost Ratio
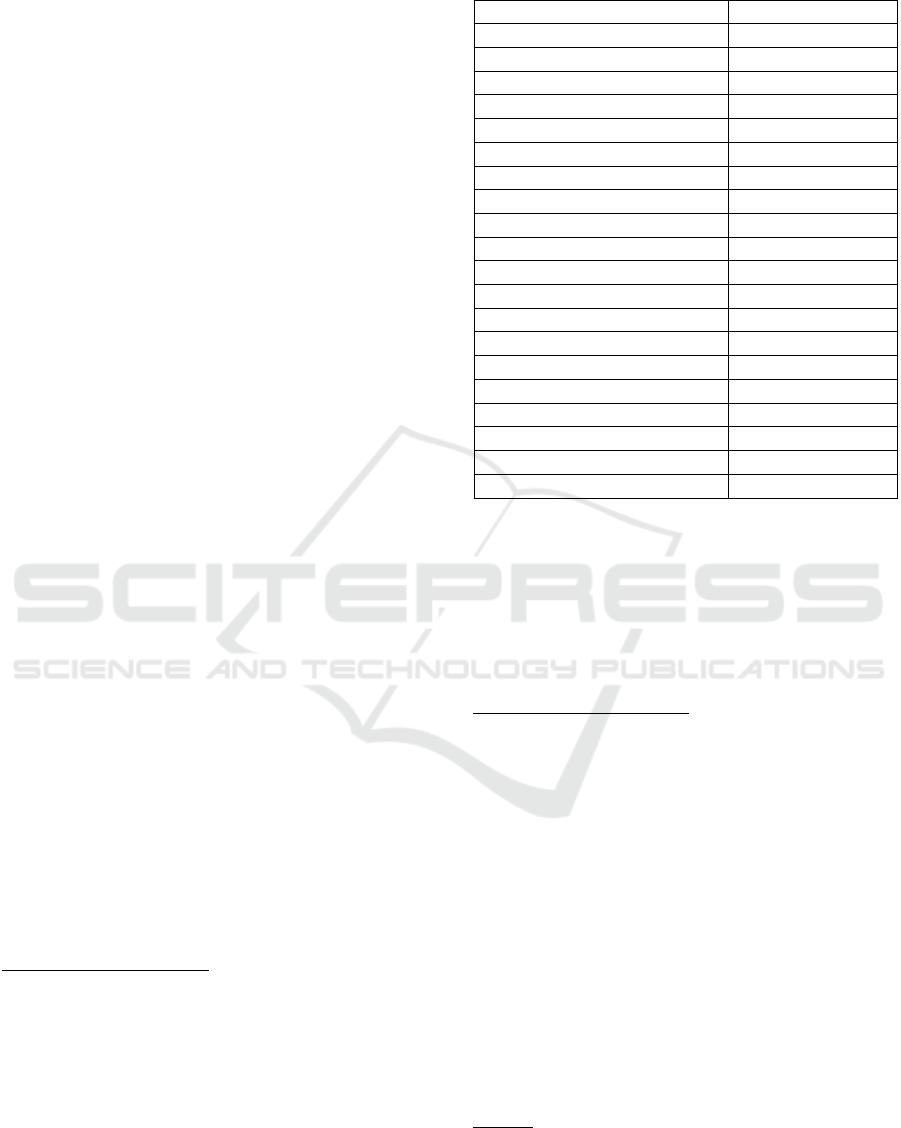
Table 2: Summary of the DECI scenario in monetary terms
(euros).
Total benefits
Total costs
Benefit/Cost
ratio
Year 1
222.795,16
193.211,27
1,15
Year 2
334.192,74
271.383,9
1,23
Year 3
389.891,53
310.540,22
1,25
As it can be seen from the Table 2, the business case
of the DECI services in Italy is positive from the first
year. Benefits in year 1 comprise 222.795,16 euros
and consist of preventable care costs 196.337,16
euros, and insurance reimbursement for the usual care
(income) 26.458 euros. Other categories of the
benefits were non-monetary, and therefore they were
not included in the calculation of the benefits.
Benefits for the year 2 and year 3 were calculated in
the same way.
The costs in year 1 comprise 193.211,27 euros and
consist of the cost of time spent by the professionals
66.325,27 euros, a one-time investment 140 euros,
and annual operating expenses 126.746 euros. Costs
for the year 2 and year 3 were calculated in the same
way, except the investment cost of 140 euros was not
included in the subsequent years, since it was a one-
time expense.
The benefit/cost ratio was calculated by dividing
the total cash benefits of the DECI services by the
total cash costs of the DECI services.
5 DISCUSSION
Future predictions of an increase in dementia patients
makes it important to assess new non-
pharmacological forms of care. In this study, we
assessed a business case of an eHealth platform to
provide remote monitoring and coaching services for
elderly with mild cognitive impairment and mild
dementia (DECI). We compared two different
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
34

scenarios, DECI and the usual care. The comparison
showed that the DECI services can be cost-effective
from the first year, and it is a more beneficial
alternative to usual care for elderly with mild
cognitive impairment and mild dementia. In the DECI
scenario, the cost increases compared to the usual
care due to a different care model that includes multi-
disciplinary work, usage of technology, and
coordination activities performed by the case
manager. However, the cost is partially reimbursed by
insurers and outweighed by both monetary and non-
monetary benefits.
From the patients’ point of view, DECI helped to
postpone a need for institutional care by reducing the
rate of conversion from MCI to MD. Such
postponement brings positive economic impact. The
study adds knowledge on how such non-
pharmacological intervention reduces the long-term
costs of care (Lin and Neumann, 2013). The findings
of this study were produced on a relatively small
sample of patients. In the future, the effects of similar
interventions to the costs for dementia management
could be investigated on a larger scale. However,
there was not enough evidence to suggest that there
were statistically significant changes in quality of life
of the patients. This result could be influenced by a
sample size, or a rather short duration of the
intervention that lasted for 6 months. In the future, it
might be worthwhile to explore other aspects of
quality of life than the ones covered by the instrument
EuroQoL-5D-5L.
Healthcare professionals felt more empowered by
a possibility to provide useful ICT tools of the DECI
services to patients so that they feel more in control
over their condition. Moreover, the DECI service has
the ability to save time for home visits by monitoring
patient’s performance remotely. The case manager
role, as part of DECI scenario, was perceived as a
must-have in the care process, as it helps to build
relationships with patients and facilitates
coordination of care.
Hence, it can be concluded that such an eHealth
platform, providing remote monitoring and coaching
services, is a worthwhile investment in the Italian
context, as care can be improved at no monetary loss
for the healthcare provider. Furthermore, Italian
authorities could consider assessing the possibility of
a region-wide implementation of the DECI solution.
When comparing this study with other published
cost-effectiveness studies on eHealth for elderly with
mild cognitive impairment and mild dementia, it is
challenging to draw conclusions. This is because the
types of eHealth analyzed are different and applied in
different contexts. Also, the pace of technology
development is fast and monetary values (e.g. prices,
hourly tariffs) are not stable over time. For example,
the ISISEMD project (Mitseva et al., 2009)
implementing assistive eHealth technologies
concluded that cost-effectiveness can only be reached
if it is provided at a large scale. The DECI services,
applying a different technology, can be cost-effective
on a scale of one organization and from year 1 itself.
Our study added knowledge about cost-effective
eHealth solutions that provide added value to elderly
with mild cognitive impairment and mild dementia.
5.1 Future Plans in the Italian Site
From 2019, a new model of Lombardy region health
system is going to be introduced. It will allow
reimbursement and delivery of home healthcare
services for elderly chronic patients suffering from
cognitive decline. This will enable to deliver services
also through ICT technologies (although the
hardware and software technology will not be
reimbursed). Based on this model, reimbursement for
the delivery of home care services with ICT tools will
exceed the usual care reimbursement. Such
developments at regional level will create an
opportunity to implement the DECI concept in the
usual care system.
Being part of the DECI research, the Memory
Clinic of Istituto Palazzolo, Fondazione Don Carlo
Gnocchi Onlus (FDG) has appreciated the DECI
concept and considers it beneficial compared to the
usual care. The site aims to ensure that chronic elderly
patients are followed in their clinical path, and more
patients in need of assistance can be reached.
Therefore, FDG has decided to adopt the DECI
approach. However, even though the business case
was positive, the site aims to reduce the cost of
technology even more. At first, the site will re-use the
hardware (tablets) that have already been used during
the DECI study. Since ICT will not be reimbursed and
will have to be covered at own expense by the site,
the strategy is to consider other similar and cheaper
software technologies that are already tested by the
site in other research projects. To manage the costs,
the site will create a strategy to balance the number of
patients in need of the service and the duration of the
service using technology. This way, the site expects
to maximize the reach and benefits for the patients in
need.
The principal risk for this future scenario is the
under- or no-use of the technologies from care staff
and patients, when they are implemented. This risk
could emerge because the use of ICT tools requires
changes in daily routines and activities for all the
An Italian Business Case for an eHealth Platform to Provide Remote Monitoring and Coaching Services for Elderly with Mild Cognitive
Impairment and Mild Dementia
35

stakeholders – healthcare providers, patients, and
their informal caregivers.
6 RECOMMENDATIONS AND
CONCLUSIONS
The aim of this study was to assess a business case for
an eHealth platform to provide remote monitoring
and coaching services for elderly with mild cognitive
impairment and mild dementia. A lack of economic
evidence leads to difficulties to decision-makers in
investing in eHealth solutions for dementia. Findings
from this study demonstrate that the eHealth platform
containing remote monitoring and coaching
functionalities is a worthwhile investment, with
benefits for people with mild cognitive impairment
and mild dementia, and also for the healthcare
provider.
To further enhance the business case, several
changes could be implemented to the DECI services:
(1) Patient or informal caregiver contribution.
Willingness-to-pay analysis showed that the
average monetary contribution by the
patients could comprise 28,20 euros. The
average contribution by the informal
caregivers could comprise 23,10 euros per
month.
(2) Healthcare insurance contribution. Financial
burden could be shared with insurers.
However, negotiations for eHealth
reimbursement would need to be started.
Since the positive monetary benefits of
DECI affect insurers, achieving contribution
from the insurers is deemed to be of good
potential.
Delimit the technology of the DECI solution to
software-only. Currently, the biggest part of the cost
is caused by the smartwatch technology and its usage
fees. And patients were not as satisfied with the
smartwatch as with the software technologies (mainly
due to the design issues). Eliminating the smartwatch
would substantially reduce the cost, thus making the
solution even more attractive for investment. For
activity monitoring, one could also resort to using the
accelerometers in patients' smartphones, which are
equally capable of registering physical activity.
7 LIMITATIONS
The main limitation of the study was the follow-up
period of 6 months, which affected the observed
outcomes in terms of health and quality of life. A
longer period could have possibly provided a more
meaningful evaluation. Another limitation was
related to the outcomes that could not be turned into
monetary values (both for costs and benefits). In such
cases, qualitative discussion is provided. Lastly, there
was a lack of preventable falls data since this data was
not collected in the study and had to be obtained from
the literature. However, the literature used is based on
the same OTAGO program in other studies.
ACKNOWLEDGEMENTS
The authors would like to express gratitude to
research consortium of the DECI project, financed by
European Union’s Horizon 2020 research and
innovation programme under grant agreement No
643588: Fondazione Politecnico di Milano, Consoft
Sistemi SpA, Fondazione Don Carlo Gnocchi Onlus
(Italy), Centre for Healthcare Improvement –
Chalmers University of Technology, Västra
Götalandsregionen (Sweden), Hospital Universitario
de Getafe - Servicio de Geriatría (Spain), Maccabi
Healthcare Services (Israel), Roessingh Research and
Development (The Netherlands).
REFERENCES
Ben-Sadoun G, Sacco G, Manera V, Bourgeois J, König A,
Foulon P, Fosty, B., Bremond, F., d’Arripe-
Longueville, F., and Robert, P., 2016. Physical and
Cognitive Stimulation Using an Exergame in Subjects
with Normal Aging, Mild and Moderate Cognitive
Impairment. Journal of Alzheimer’s Disease,
53(4):1299–314.
Berg, W. P., Alessio, H. M., Mills, E. M., & Tong, C., 1997.
Circumstances and consequences of falls in
independent community-dwelling older adults. Age and
ageing, 26(4), 261-268.
EuroQol Group. EuroQol—A new facility for the
measurement of health-related quality of life, 1990.
Health Policy (Amsterdam, Netherlands). 16(3):199.
Folstein, M. F., Folstein, S. E., and McHugh, P. R., 1975.
“Mini-mental state”: a practical method for grading the
cognitive state of patients for the clinician. Journal of
psychiatric research, 12(3), 189-198.
Gambles, I., 2017. Making the business case: Proposals that
succeed for projects that work. Routledge.
Gillespie, L. D., Robertson, M. C., Gillespie, W. J.,
Sherrington, C., Gates, S., Clemson, L. M., and Lamb,
S. E., 2012. Interventions for preventing falls in older
people living in the community. Cochrane database of
systematic reviews, (9).
ICT4AWE 2019 - 5th International Conference on Information and Communication Technologies for Ageing Well and e-Health
36

Gitlin, L. N., Hodgson, N., Jutkowitz, E., & Pizzi, L., 2010.
The cost-effectiveness of a nonpharmacologic
intervention for individuals with dementia and family
caregivers: the tailored activity program. The American
Journal of Geriatric Psychiatry, 18(6), 510-519.
Goldzweig, C. L., Towfigh, A., Maglione, M., and
Shekelle, P. G., 2009. Costs and benefits of health
information technology: new trends from the literature.
Health affairs, 28(2), w282-293.
Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M,
Scalone L, Swinburn P, and Busschbach J., 2013.
Measurement properties of the EQ-5D-5L compared to
the EQ-5D-3L across eight patient groups: A multi-
country study. Quality of Life Research, 22(7):1717-27.
Katz, S., Down, T.D., Cash, H.R., and Grotz, R.C., 1970.
Progress in the development of the index of ADL. The
Gerontologist, 10(1), 20-30.
Kim, K. I., Gollamudi, S. S., and Steinhubl, S., 2017.
Digital technology to enable aging in place.
Experimental gerontology, 88, 25-31.
Knapp, M., Barlow, J., Comas-Herrera, A., Damant, J.,
Freddolino, P., Hamblin, K., and Woolham, J., 2016.
The case for investment in technology to manage the
global costs of dementia. Policy Innovation Research
Unit, Personal Social Services Research Unit at the
London School of Economics and Political Science.
London.
Lawton, M.P., and Brody, E.M., 1969. Assessment of older
people: Self-maintaining and instrumental activities of
daily living. The Gerontologist, 9(3), 179-186.
Lin, P. J., and Neumann, P. J., 2013. The economics of mild
cognitive impairment. Alzheimer's & Dementia, 9(1),
58-62.
Mitseva, A., Kyriazakos, S., Litke, A., Papadakis, N., &
Prasad, N., 2009. ISISEMD: Intelligent System for
Independent living and self-care of SEniors with mild
cognitive impairment or Mild Dementia. The Journal
on Information Technology in Healthcare, 7(6), 383-
399.
Morris, J. C., 1997. Clinical dementia rating: a reliable and
valid diagnostic and staging measure for dementia of
the Alzheimer type. International psychogeriatrics,
9(S1), 173-176.
Prince, M. J., Wu, F., Guo, Y., Robledo, L. M. G.,
O'Donnell, M., Sullivan, R., and Yusuf, S., 2015. The
burden of disease in older people and implications for
health policy and practice. The Lancet, 385(9967), 549-
562.
Riikonen, M., Mäkelä, K., & Perälä, S., 2010. Safety and
monitoring technologies for the homes of people with
dementia. Gerontechnology, 9(1), 32-45.
Shulman, K. I., 2000. Clock‐ drawing: is it the ideal
cognitive screening test? International journal of
geriatric psychiatry, 15(6), 548-561.
Swinkels, I. C. S., Huygens, M. W. J., Schoenmakers, T.
M., Nijeweme-D'Hollosy, W. O., Van Velsen, L.,
Vermeulen, J., Schoone-Harmsen, M., Jansen, Y.J.,
Van Schayck, O.C., Friele, R., and de Witte, L., 2018.
Lessons Learned from a Living Lab on the Broad
Adoption of eHealth in Primary Health Care. Journal of
medical internet research, 20(3).
Thomas, S., Mackintosh, S., & Halbert, J., 2010. Does the
‘Otago exercise programme’reduce mortality and falls
in older adults?: a systematic review and meta-analysis.
Age and ageing, 39(6), 681-687.
Van Mierlo, L. D., Meiland, F. J. M., Van de Ven, P. M.,
Van Hout, H. P. J., Dröes R-M., 2015. Evaluation of
DEM-DISC, customized e-advice on health and social
support services for informal carers and case managers
of people with dementia; a cluster randomized trial.
International Psychogeriatrics. 27(8):1365–78.
Visser, P. J., Kester, A., Jolles, J., and Verhey, F., 2006.
Ten-year risk of dementia in subjects with mild
cognitive impairment. Neurology, 67(7), 1201-1207.
Westphal, A., Dingjan, P., and Attoe, R., 2010. What can
low and high technologies do for late-life mental
disorders? Current opinion in psychiatry, 23(6), 510-
515.
Willis, E., Semple, A. C., & de Waal, H., 2018. Quantifying
the benefits of peer support for people with dementia:
A Social Return on Investment (SROI) study.
Dementia, 17(3), 266-278.
Wolfs, C. A., Dirksen, C. D., Kessels, A., Willems, D. C.,
Verhey, F. R. and Severens, J. L., 2007. Performance of
the EQ-5D and the EQ-5D+C in elderly patients with
cognitive impairments. Health and Quality of Life
Outcomes, 14, 33.
An Italian Business Case for an eHealth Platform to Provide Remote Monitoring and Coaching Services for Elderly with Mild Cognitive
Impairment and Mild Dementia
37
