
Organizing Medtech Innovation with Concept Maturity Levels
Mathias Béjean
1a
and Eliziane Siqueira
2
1
Institut de Recherche en Gestion (EA 2354), Université Paris Est, Place de la Porte des Champs, 94000, Créteil, France
2
MS Innovation by Design, ENSCI Les Ateliers, 48 rue Saint Sabin, 75011, Paris, France
Keywords: Medical Devices, Medtech, Innovation, Concept Maturity Levels.
Abstract: This paper presents an integrative approach to the maturation of concepts in the field of Medtech Innovation
by using Concept Maturity Levels (CMLs). CMLs have been introduced by JPL (NASA-Caltech) during the
last decade to cope with the early phases of space mission concept development. Extending well-known TRLs,
their strength is to evolve an innovative concept guided by an incremental set of assessment needs. The article
draws on an on-going research led in France where CMLs are being tested as a methodology for structuring
Medtech Innovation complexity. Exploratory results provide an emerging framework showing what could be
CMLs for Medtech Innovation. They also provide insights of why and how they could be implemented as a
solid basis to stimulate more formative and adaptive design and evaluation methods.
1 INTRODUCTION
The Medtech sector is a highly diversified and
complex one. According to MedTech Europe (2016),
it includes more than 500,000 medical technologies
ranging from familiar, everyday products such as
blood glucose meters, sticking plasters, syringes or
latex gloves, to high-tech medical technologies
including molecular diagnostics, total body scanners,
ultrasounds, life-supporting machines, implantable
devices (i.e. heart valves pacemakers),
neurostimulators and replacement joints for knees
and hips. Likewise, the industry structure brings into
play various economic actors ranging from small and
medium-sized companies to big technological firms
and high ranking research laboratories.
Another important characteristic of the medical
devices market is its dynamic nature. In average, a
medical device product has a life cycle ranging from
18 to 24 months, which forces companies to invest
constantly in research and development. This leads to
an increase in the relevance of development upstream
phases, where many Medtech experts try to anticipate
the different risks emerging from the complexity they
face. However, medical devices projects often fail or
result in products with no market-fit, for not having
sufficiently integrated the perceptions and insights of
end-users early enough (Habib et al., 2017).
a
https://orcid.org/0000-0001-6818-3008
Despite their strategic importance, the upstream
phases of medical devices development are still
insufficiently understood and documented. Available
approaches for exploration and evaluation often tend
to offer a sole snapshot of the product at the end of its
development cycle, neglecting the activities required
to incorporate the habits and needs of end users,
especially the patients. These facts and the complex
context mentioned above call for new approaches
which do not only evaluate the quality of a new
medical device and its market fit, but also clarify the
path to transform a promising idea into a solution that
is financially viable and easily adopted by patients
and their healthcare ecosystem.
This paper aims to fill this gap by studying an
integrative approach using “Concept Maturity
Levels” (CMLs) (Ziemer et al., 2013). CMLs are a
new metric inspired by Technology Readiness Levels
(TRLs) developed by NASA in the 80s. Allowing the
evaluation of knowledge robustness for a given
technology at a given moment, TRLs have become a
world-wide tool for project organization and
communication. CMLs extend TRLs by both adding
divergent phases to TRLs convergent orientation and
integrating needs (value proposition, end-users…) as
well as organizational aspects (costs, organization…)
to the technological ones.
To do so, the paper draws on an on-going research
led in the French context, where CMLs are being
Béjean, M. and Siqueira, E.
Organizing Medtech Innovation with Concept Maturity Levels.
DOI: 10.5220/0007697006210626
In Proceedings of the 12th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2019), pages 621-626
ISBN: 978-989-758-353-7
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
621

introduced to cope with Medtech innovation
complexity. After having provided the theoretical
background of the research, the article presents the
research context and methods used. Exploratory
results are then presented, leading to discuss the
opportunities and potential risks of implementing
CMLs for Medtech Innovation.
2 THEORETICAL
BACKGROUND
This section provides basic elements on the literature
on concept maturation activities in both management
and engineering sciences.
2.1 Innovation and concept maturation
In the field of innovation management, the streams of
“radical innovation” (O’Connor, 2008), “open
innovation” and “collaborative innovation”
(Chesbrough, 2003) have paid attention to the new
organizational forms of innovation, their strategies,
their processes, their business models. An important
aspect of recent literature concerns the more
“upstream” phases of exploration, including the
maturation and formulation of innovative concepts
(Markovitch et al., 2017).
During these maturation activities, it no longer
consists of evaluating and selecting ideas, as
advocated by “new product development” inspired by
project management (Cooper, 1994), but also of
structuring complete management systems intended
to “mature” concepts and the organizations which
sustain them to transform the starting intention into a
value proposition implemented into a new ecosystem
of uses (Hooge et al., 2016).
In this context, the strategic challenges are that of
formalization and instrumentation of new “upstream”
processes which are more agile and participative,
integrating a wide range of stakeholders, both internal
and external, including the end-users. Contemporary
approaches therefore call for novel approaches to
evolve and enrich innovative concepts throughout
their design process; CMLs are one of these.
2.2 Concept Maturity Levels (CMLs)
CMLs are a special metric developed by the JPL
Innovation Foundry (Caltech/NASA) for dealing
with the most early formulation phases of space
mission concept development. They are inspired by
Technology Readiness Levels (TRLs) already
developed by NASA in the 80’s. Allowing the
evaluation of knowledge robustness for a given
technology at a given moment, TRLs have become a
world-wide tool for project organization and
communication. CMLs aim at extending TRLs by
adding a divergent phase to their convergent
orientation and adding two more “drivers” to
technological maturity: the maturity of needs
understanding (value proposition, end-users…) and
the organizational maturity (costs, organization…).
Conceived as a generic language, CMLs aim to
assess a concept’s maturity making it possible to
select and prioritize the ones to support. JPL has
defined 8 different CMLs:
- CML 1: Cocktail Napkin
- CML2: Initial feasibility
- CML3: Area of application (Trade space)
- CML4: Design components (Point Design)
- CML5: Reference concept
- CML6: Integrated concept
- CML7:Preliminary referential implementation
- CML8: Integrated referential
3 RESEARCH CONTEXT AND
METHODS
3.1 Research Context
3.1.1 Context
This study emerged in the context of a partnership
between the French Forum of Living Labs in Health
& Autonomy (LLSA) and the INSERM CIC-IT
Network. Forum LLSA is a non-profit organization
which federates a community of over 30 Living Labs
and about 20 other members interested – and
generally involved – in codesign and living lab
approaches. CIC-IT Network brings together
Research Centers specialized in clinical research for
MedTech projects, providing support in clinical
protocols design, regulatory constraints and solution
assessment to project manager and enterprises.
The diversity of LLSA and CIC-IT members
reflects the one of the health ecosystem:
professionals, researchers, patients, manufacturers.
Recently, they formed a working group, named
“EVAL”. These members were both practitioners and
academics involved in use and/or clinical evaluation
before, during and after the design process of a
medical device. In February 2018, the group EVAL
decided to launch an intervention research based on
ClinMed 2019 - Special Session on Designing Future Health Innovations as Needed
622

the idea of implementing CMLs in the Medtech
sector. A research project team was set.
3.1.2 Case Selection
Regarding the case selection, the research goals were
to deepen the understanding of co-creation,
evaluation and project management best practices
applied in the lifespan of a concept maturation
process. Three criteria were established: organization
maturity, case maturity and trust relationships with
potential interviewees:
- Organizational Maturity: it was decided to
investigate cases managed by Living Labs and
CIC-IT with a well-established practice in the co-
creation and evaluation of medical devices. This
choice was based upon two rationales: the need to
clarify current design and management practices
and, as previously mentioned, to serve as a
stepping stone for the construction of a
methodology of evaluation.
- Project Maturity: it was agreed to study projects
that were further advanced in the development
cycle, i.e. that had already passed or were near to
pass regulatory certification (CE marking in these
cases). This characteristic would allow the study
to be based upon longitudinal cases, with rich
steps of development cycle and potentially a wide
range of relevant tools and best practices.
- Trust Relationships: more active members
regularly take part in the working group sessions.
As a consequence the suggested case studies were
those under direct or indirect responsibility of
those members. A potentially positive
consequence of this fact is that the trust
relationship between the Forum and the chosen
structures could allow the informants to feel more
at ease during interviews, possibly sharing project
pain points that would not otherwise been
communicated.
Considering these three criteria, five projects were
selected: Hemogyn 2 (CIC-IT, Grenoble), Motio
(Kyomed, Montpelier), Careware (Infoautonomie,
Nancy), Connected Glass (Evalab, Lille) and Modu-
Lab (CHL, Castres).
3.2 Data Collection
3.2.1 Selecting Informant’s Profile
Following guidelines suggested by Eisenhardt
(2007), the research team opted for interviewing
multiple informants for each case, preferably from
different organizations and having different roles in
the case. This approach limits biases, since the same
situation is described from different perspectives.
According to each project ecosystem, a list of
interviews was set to include the project manager, the
organization responsible, the operational team and
partners of development.
For each project, the responsible organization had
to contact participants of the project and arranged an
interview. Strategy during the interview was to assign
all investigators with slightly different roles.
According to Eisenhardt (1989), this allows the case
to be interpreted from different, sometimes divergent
perspectives, which has the potential to enhance
richness of the study. The lack of representation of the
voice of patients could consist in a source of
weakness of this research, and should be accounted
for in similar future studies.
3.2.2 Exploratory Phase
This paper presents an on-going research. At this
stage, it only concerns the exploratory phase of the
research, consisting of 17 interviews carried out
between June and July 2018, lasting from 30 min to
more than 2hours.
All interviews, except for two, followed a semi-
directive protocol. During the interview, a member of
the research team would introduce the purpose and
the process of the study, as well as the general goal of
the interview. During the interview, all of the
investigators would ask questions; however, the lead
of the interview was taken by the scientific
responsible of the study. The two other investigators
would take notes according to their own perspectives
of the case.
After obtaining consent, all the interviews were
registered by using a voice recorder.
3.3 Data Analysis
The first round of data analysis consisted of the
following steps: Interviews summary, Interviews
transcriptions, Defining CML criteria, Coding
interviews according to criteria:
- Interviews Summary: we consolidated our
impressions and notes in form of an interview
summary, produced shortly after the field study.
The aim was to serve as a quick reference to the
team, offering a way of recovering essential
information quickly, which proves to be useful in
studies composed of large amounts of interviews.
- Interviews Transcriptions: all interviews were
entirely transcribed, following sound recordings
by using the software o-transcribe.
Organizing Medtech Innovation with Concept Maturity Levels
623
- Confronting Field Data to CMLs: three
representative interviews were confronted, in
extenso, to the CML framework.
During data analysis, the main findings were
organized to elaborate a generic model that defines
the maturity of an innovative concept in the sector of
medical devices, as well as a generic process to
transform an initial concept idea into a functional
proven concept. In the following we refer to this
emerging framework as the “CML-FS framework”
(FS for “Forum Santé”). As already mentioned, this
is an on-going research and further research is needed
to strengthen and enrich this model. The next section
presents the CML-FS framework.
4 RESULTS
4.1 The CML-FS Framework
At this stage, the CML-FS framework defines 6
progressive levels, which describe the increasing
maturity of a healthcare concept:
- CML1-Framing the Idea: this includes the
understanding of social and health care
background to contextualize and prove solution’s
relevance. Building project team is another key
step in CML 1.
- CML2-Understanding Usage Requirements:
this includes that rapid prototyping and financing
plan have been identified as the main validation
steps in CML 2.
- CML3-Shaping the Design: this maturity level
requires listing the platform concept, regulatory
affairs and definition of usage scenarios as
essential milestones to give shape to the chosen
concept design.
- CML4-Fine-tuning the Design: this maturity
level must achieve pre-clinical trials and help
building clinical trials as well as use test
protocols.
- CML5-Clinical Trials, use Tests and
Certification: this maturity level consists of
preparing and executing clinical trials, if
applicable, as well as leading user tests.
Certification is the last critical step to this level.
- CML6-Planning Implementation: this maturity
level is achieved after completing activities
needed to consolidate product and commercial
specification to the industrial development of the
solution.
The division into six maturity levels is not arbitrary.
The findings allowed for grouping activities
according to chronologic order of main milestones
revealed during the interviews. We found six to be the
minimal number of activities chunks to be
represented in order to mature a concept. Every CML
phase could be further divided, resulting in more
levels. Further research will serve to validate the
model and its levels or to modify it if needed.
4.2 Towards a New Design Process
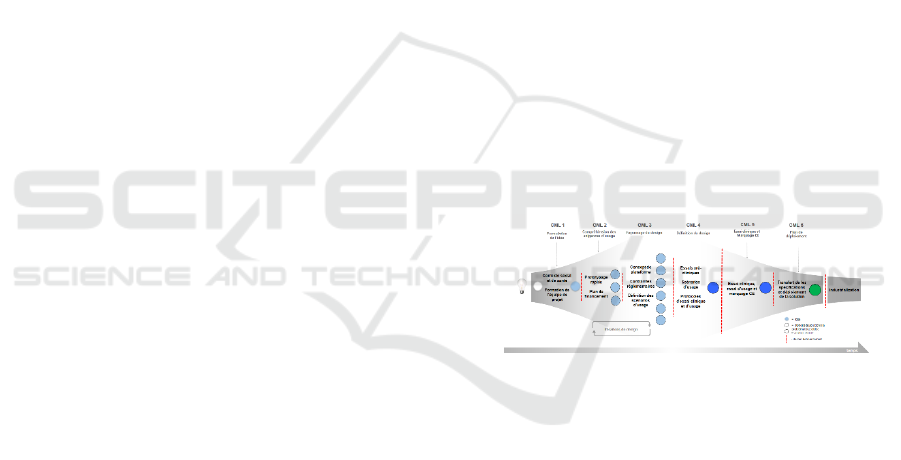
Figure 1 depicts the design process model
corresponding to the progressive nature of CML-FS
framework. It provides structure in the form of a
“diamond” including milestones and corresponding
activities per level, enabling the definition of a
concept development roadmap.
The diamond background (fading grey shape)
illustrates the diverging and converging moments in
the framework: levels 1 to 3 consists in the divergent
phase aiming at exploring the field, opening up the
perceptions about the chosen healthcare problem, and
allowing for problem reframing, if necessary.
At the end of CML 3, however, design iterations
end once few preferred design solutions are chosen.
Starting a convergent phase, the preferred solutions
are further matured and tested with users in CML 4.
Figure 1: The evolution of an innovative healthcare concept
over time.
It is relevant to notice the role of design iterations
between CML 2 and 3. This iterative process is
inherent to the divergent phase of design. According
to our interviewees, it is an essential step to identify
the problem at stake and discover which ideas are the
most relevant to figure it out. In practical terms, it
allows ideas to be developed and tested a number of
times, with weak ideas dropped along the way. The
result, at last, is one concept that has been evaluated
and refined several times before its launch, by a wide
range of stakeholders.
4.3 Opportunities and Potential Risks
Interesting information shown by the CML-FS
framework is the level of financing requested before
entering each CML phase. As per the studied projects,
ClinMed 2019 - Special Session on Designing Future Health Innovations as Needed
624

the largest amounts of financing are needed in the
transition between CMLs 4 and 5 in order to execute
clinical trials, use tests and apply for product
certification. Likewise, our research suggests that
research work needed to go from CML1 to 3 is still
lacking, at least in the French context. Using CMLs
might be a way to better analyze and structure these
early financing phases.
However, the CML-FS design model is merely
illustrative, aiming at warning project owners to
account for such expenses beforehand. A quantitative
estimation of financial needs is not in the scope of the
current exploratory research, given the broad
spectrum of products that could make use of this
framework. Each one of these products, according to
certification classification, would present
considerable variations in development budget and
financing needs, one of the current perceived risks
being to overlook this diversity of products and
situations.
5 CONCLUSIONS
Our exploratory research thus suggests that CMLs
could provide an integrative approach to the upstream
co-design difficulties, by opening new ways of
combining real-life data with results of clinical
investigations, or even exploring complex
polymorphic therapeutic solutions at different levels
of maturity. One of the main interest could for
instance be avoiding the so-called “techno push”
phenomenon, as applicable to the spatial domain and
the Medtech sector.
Furthermore, health projects are highly supported
by public funds. At the end, they deliver products and
services which are subsidized to a large extent.
Therefore, evaluation of these projects concerns not
only project manager, stakeholders involved but also
public authorities and policy makers.
The interest of using the CML approach will be
enforced by adding to the process description some
indicators that are likely to be available at an early
stage rather than requiring evidence of final impact.
This could enable the “clock speed” of the evaluation
cycle to increase, bringing it more in line with the
policy cycle.
As quoted in (Warwick and Nolan, 2014): “The
developmental evaluation approach [...] is
particularly well matched to the modern conception
of industrial policy where policy makers engage in an
iterative process of dialogue with business and others,
and there is a combination of top-down and bottom-
up approaches. Experimental methods are
increasingly being used in the evaluation of some
facets of industry and innovation policies, but there is
potential to do more.”
The use of experimentation and the iterative
approaches of developmental evaluation fit well not
only with the CML approach, but also with the notion
of a “smarter state”, which seeks to learn from the
market and the discovery process of entrepreneurs in
selecting appropriate targets for public policy.
ACKNOWLEDGEMENTS
Authors thank all the interviewed experts from
Hemogyn 2 (CIC-IT, Grenoble), Motio (Kyomed,
Montpelier), Careware (Infoautonomie, Nancy),
Connected Glass (Evalab, Lille) and Modu-Lab
(CHL, Castres). Special thanks also to the Forum
LLSA, the CIC Network and Altran Research
Department which all made this research possible.
REFERENCES
Chesbrough, H.W., 2003. Open innovation: the new
imperative for creating and profiting from technology,
Harvard Business School Press.
Cooper, R.G., 1994. Third-Generation New Product
Processes. Journal of Product Innovation Management,
11(1), pp.3–14.
Eisenhardt, K.M., 1989. Building theories from case study
research. Academy of Management Review, 14(4),
pp.532–550.
Eisenhardt, K.M., 2007. Theory building from cases:
opportunities and challenges. Academy of Management
Journal, 50(1), pp.25–32.
Habib, J., Béjean, M. & Dumond, J.-P., 2017. Appréhender
les transformations organisationnelles de la santé
numérique à partir des perceptions des acteurs.
Systèmes d’information & management, 22(1), pp.39–
69.
Hooge, S., Béjean, M. & Arnoux, F., 2016. Organizing for
Radical Innovation: The benefits of the interplay
between cognitive and organizational processes in KCP
workshops. International Journal of Innovation
Management, 20(04), p.1640004.
Markovitch, D.G., O’Connor, G.C. & Harper, P.J., 2017.
Beyond invention: the additive impact of incubation
capabilities to firm value. R&D Management, 47(3),
pp.352–367.
MedTech Europe, 2016. The European Medical
Technology industry in figures, Belgium.
O’Connor, G.C., 2008. Major Innovation as a Dynamic
Capability: A Systems Approach. Journal of Product
Innovation Management, 25(4), pp.313–330.
Warwick, K. & Nolan, A., 2014. Evaluation of Industrial
Policy: Methodological Issues and Policy Lessons. In
Organizing Medtech Innovation with Concept Maturity Levels
625

OECD Science, Technology and Industry Policy
Papers. Paris: Éditions OCDE.
Ziemer, J., Ervin, J. & Lang, J., 2013. Exploring Mission
Concepts with the JPL Innovation Foundry A-Team. In
AIAA Space 2013. San Diego, California.
ClinMed 2019 - Special Session on Designing Future Health Innovations as Needed
626
