
Modeling and Simulation
of the Hospital-at-Home Service Admission Process
Ilaria Angela Amantea
1
, Marzia Arnone
1
, Antonio Di Leva
1
, Emilio Sulis
1
,
Dario Bianca
2
, Enrico Brunetti
2
and Renata Marinello
2
1
Computer Science Department, University of Torino, 185 Corso Svizzera, 10149, Torino, Italy
2
City of Health and Science, 88 corso Bramante, 10126, Torino, Italy
Keywords:
Business Process Analysis, Hospital-at-Home, Modeling and Simulation, Healthcare.
Abstract:
This article focuses on the analysis of the admissions to hospital-at-home service within the framework of
Business Process Management. While traditional process analysis deal with internal hospital services, having
a particular and specific scenario, e.g. a ward of an hospital, here we investigate a quite innovative service with
a strong socio-territorial impact based on real data. In particular, we are interested in the understanding of the
selection process in which staff discriminate cases of interest for the service. We describe here our method-
ological framework combining data and event log analysis, modeling with standard language and business
process simulation with scenario analysis.
1 INTRODUCTION
Demographic and economic modifications occurred
in last decades, together with the availability of new
technologies, pushed the research of continuous im-
provements in healthcare. In Medicine, the most
part of actual applications of artificial intelligence and
computer science concerns diagnostic processes and
performance analysis, mostly focusing on the appli-
cation of new algorithms (e.g. machine learning).
Nevertheless, an equally important aspect to investi-
gate is the organization of health processes, by con-
sidering an holistic and systemic approach. In this
direction, computer science gained a relevant role not
only for computational reasons, but also for techni-
cal hardware and information systems improvements
(Dumas et al., 2005). This is the case of Business
Process Management (BPM) (Dumas et al., 2018;
Van der Aalst, 2013), a discipline combining stud-
ies of management with data science to perform busi-
ness process improvement and computational sim-
ulation as a management instrument for decision-
making (Van der Aalst et al., 2010). A large number
of modeling techniques investigates the actual process
(As-Is) in order to propose a restructured one (To-Be)
(Di Leva and Sulis, 2017). Modeling and simula-
tion includes computer-based Discrete Event Simula-
tion (DES) (Johnson et al., 2008), probably the most
used approach to investigate the outcomes of simu-
lated scenarios, as well as to estimate the performance
of the system after introducing changes in the process
model. Moreover, modeling the actual situation easily
allows to detect the actual functioning of the work-
flow by facilitating the detecting inefficiencies, bot-
tlenecks, constraints, and risks (Suriadi et al., 2014;
Amantea et al., 2018).
We focus on a specific department in healthcare,
one of the most relevant public service in developed
countries (Vincent et al., 2016). Our interest here is
the Hospital-at-Home Service (HHS) in Turin, one of
the largest city of Italy, within a EU co-funded project
by Regione Piemonte to investigate healthcare pro-
cesses and telemedicine (Grosso et al., 2018). This
service has a great tradition with more than thirty
years of experience. As one of the main issue con-
cerns the selection of patients, we focused the atten-
tion on the first part of the HHS process by mod-
eling the functioning of admissions. Similar works
about business process analysis in healthcare focused
on process mining (Mans et al., 2015; Rojas et al.,
2016), also addressing the specific task to model in-
tegrated home-care services (Russo et al., 2015). Our
goal here is to investigate the organisation of HHS to
create a repeatable model, as well as to propose the
extension to other areas.
The scientific literature and the practical experi-
ences within the domiciliary cares have underlined
the particular utility and effectiveness of this type of
Amantea, I., Arnone, M., Di Leva, A., Sulis, E., Bianca, D., Brunetti, E. and Marinello, R.
Modeling and Simulation of the Hospital-at-Home Service Admission Process.
DOI: 10.5220/0007928602930300
In Proceedings of the 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications (SIMULTECH 2019), pages 293-300
ISBN: 978-989-758-381-0
Copyright
c
2019 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
293

sanitary intervention in geriatric and oncology’s ar-
eas, recognizing the function of the hospital structure
to make more flexible integration between hospital
and territory. In northern Italy, the Regione Piemonte
defined in 2010 the hospitalization at home as a form
of Sanitary Assistance characterized by the whole tak-
ing in charge of the patient from an hospital struc-
ture (Aimonino Ricauda et al., 2011). Such a service
relies on own personnel, formed and with expressly
and documented experience in the management of pa-
tients in acute phase directly at home.
The paper includes the following sections: we
introduce our methodological framework and data
about the admission process in section 2. Section 3
describes the model of the service, while the follow-
ing section includes simulation results. We conclude
the paper with future works in Section 5.
2 METHODOLOGY
Our methodological framework consists of three
phases:
• Context Analysis - this phase aims to fix the over-
all strategic scenario of the enterprise and to de-
termine the organizational components that are re-
lated to the process under analysis.
• Process Engineering - the initial purpose of this
phase is the determination of the activities per-
formed in the functions involved in the pro-
cess and the causal relationships existing between
them. The process is then reconstructed from
facts external to the system, events and objects
in input/output: this provides the Process dia-
gram (sometimes referred to as process map or
flowchart) that will be specified by adopting a
standard language.
• Data analysis - this phase aims to analyze the real
data of the past years to understand and better rep-
resent the process the most truthful and and the
more next to the reality as possible. The whole
process model must be validated with the stake-
holders involved in the process, using animation
and simulation of specification, obtaining the so
called As-is model.
2.1 Business Process Modeling Notation
We adopt Business Process Modeling and Notation
(BPMN) (Allweyer, 2016), which is a standard mod-
eling language developed to reduce the fragmenta-
tion that was witnessed between the existing model-
ing languages. We prefer such notation as it is suffi-
ciently generic to be easily extended, as well as easily
understand by stakeholders. The actual version 2.0 is
a “de facto” standard for process modeling (Allweyer,
2016). Our diagram includes the following figures:
activities, delays, exclusive gateways, start and end
events.
2.2 Business Process Simulation
Once modeled the process, we aim to simulate the
arrival of patients in the workflow of resources. We
adopt iGrafxProcess tool (iGrafx, 2015), used to
implement the main phases of our methodological
framework, as well as process simulation. The sim-
ulation model is driven by the arrival of patients, as
detailed in the simulation section, following the flow
of activities and events.
2.3 Data Analysis
We analysed data about the arrival of patients in pre-
vious year to identify patterns and define the work-
flow in the business process. As already mentioned,
new patients are admitted to the service following a
standard procedure which involves several qualitative
information. The exploration of existing file about
event and activities facilitates the preparation of the
model and the analysis of the output results. We pro-
cessed information about the arrival of patients by
using python programming language and specific li-
braries for scientific computing numpy, statistics
1
.
3 THE HOSPITAL AT HOME
SERVICE
The Hospital at Home Service is operating in the City
of Health in Turin. This is a service that provides
diagnostic and therapeutic treatments by healthcare
professionals at patient’s home, in a condition that
normally would require acute hospital in-patient care.
Transport and acceptance are free for these patients,
as part of the HHS service. In case of necessity, a
quick admission to hospital is possible for examina-
tions or interventions that cannot be carried out at
home.
The service normally operates 12 hours a day
(from 8 am to 8 pm), each day of the week. For some
patients medical staff is available 24 hours a day.
Caregivers are instructed in the emergency plan and
encouraged to telephone if any problem arise. The
multidisciplinary staff includes four geriatricians, 13
1
Cfr. https://www.python.org/
SIMULTECH 2019 - 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
294

nurses, one nurse coordinator, two physiotherapists,
one social worker, one counsellor. One of the main
features of the service is that physicians and nurses
work together as a team with daily meeting to discuss
the needs of each patient and to organize individual-
ized medical care plans and day-to-day work.
The three most important aspects of the nurs-
ing activity are: home visits to outpatients to give
medical care as agreed with the doctors; daily team
meeting; secretarial work, receiving applications for
hospitalization, stocking pharmaceuticals and sani-
tary material, sending and collecting laboratory anal-
ysis, transporting patients for particular consultations
or exams which can be done only in hospital.
Services and Treatment Provided: physician and
nursing visits; standard blood tests; pulse oximetry;
electrocardiogram; spirometry; echocardiogram; in-
ternistic ecographies and Doppler ultrasonographies;
oral and intravenous medication administration, in-
cluding antimicrobials and cytotoxic drugs; oxygen
therapy; blood product transfusion; central venous ac-
cess (PICC, Midline); surgical treatment of pressure
sores; X-rays; telemonitoring; physical therapy; oc-
cupational therapy; counselling
The daily activities at home of patients are defined
on the basis of different clinical necessities of the pa-
tients. The team of care (physicians and nurses) guar-
antees an answer in 20-30 minutes in case of emer-
gency. Hospital-at-home patients are considered hos-
pital patients, and all services are provided by the
hospital, which retains legal and financial responsi-
bility for care. If the patient needs instrumental ex-
aminations or consultations that are not practicable to
the domicile the performance as hospitalized patient.
Hospital team booked and organized the move in the
hospital with the ambulances service for the necessary
time, then the patient returns to his/her own domicile.
All the medical equipment (e.g. the medicines) are
brought to the patient’s domicile during the daily vis-
its and furnished from the hospital. A documentation
exists for each patient always available at the patient’s
home, with an updated report available in the HHS of-
fice.
The professional experience of the staff and im-
portant clinical studies described the advantages in
terms of clinical improvement, reduction of the com-
plications, reduction of the re-entry in the hospital,
the impact on the quality of patient’s life, as well as a
reduction of the costs (i.e., from 400 Euro/day to 155
Euro/ day on average).
3.1 The Admission Process: The
Challenge to Balance Qualitative
and Quantitative Variables in a
Diagram
The admission process have only one human re-
source, that is the Case Manager (CM), who have to
evaluate all the requests and each one case according
to some guideline to understand if the patient have
some characteristics to allow him to take in charge to
this type of hospitalization. It seams a simple process
but is full of qualitative variables, over the quantita-
tive once, which make the process very more com-
plex of that it seems. At the end of this evaluation,
for the taken in charge of a patient, a real contract of
collaboration is created. It sees on one side the hospi-
tal, and in specific the staff of the department of HHS,
and from the other side the patient with the caregiver
and the possible family, which can be coincide or not
with the figure of the caregiver in itself. Besides it
is important that this type of collaboration remains
as established to the beginning for the whole time of
the duration of the service. Otherwise, for instance
in case of caregiver missing or family exhaustion, the
patient is immediately moves to hospital and hospital-
ize classically inside the hospital wall.
Firstly, every morning the Case Manager (CM)
have to evaluate the available numbers of possible
posts (Evaluation n
◦
places available, that corre-
spond to the maximum numbers of patients that she
could accept in this day. In this evaluation the CM
spent about 45 minutes because she have to evaluate:
• The number of patient that during the day will be
probably release.
• The number of staff available: for example if we
are near Christmas or summer holiday sorely staff
are fewer, so patients must be proportionate.
• How long each patients, they already have in
charge, been: some patients have some pathology
that must imply more time then other, for exam-
ple blood transfusions are longer then bandages
that are longer then giving a medicine. First type
of patient occupy two slot, second type of patients
occupy one slot and an half and the third type oc-
cupy only one place.
This first evaluation imply both type the variables,
qualitative and quantitative, it is based on the best ex-
perience of the Case Manager made by years of expe-
rience, and it is a very important task because it deter-
minate the future workload of all the staff involve in
the service.
At the same time requests can arrive by telephone
from the emergency department as well as from any
Modeling and Simulation of the Hospital-at-Home Service Admission Process
295
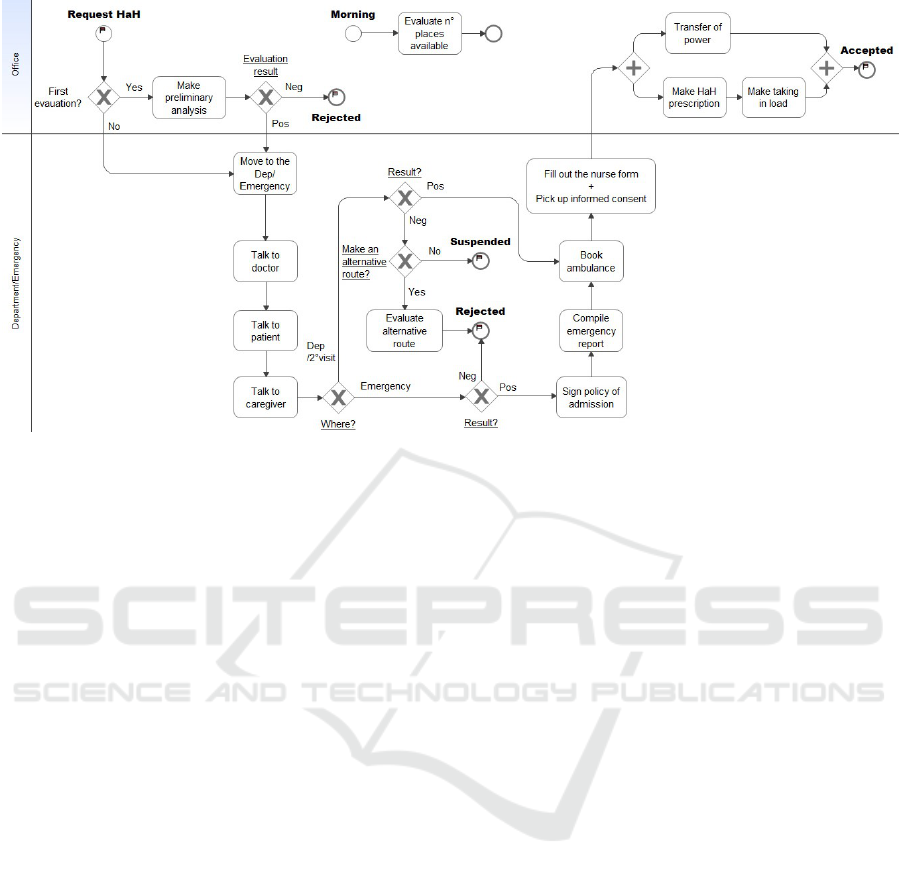
Figure 1: Process of acceptance of requests for the HHS.
other hospital departments. The requests are made by
the responsible doctors of the departments that made
a first quick evaluation.
The arrival of a request by phone at the Hospital
at Home (HaH) (generator Request HaH) implies an
initial evaluation (gateway First evaluation?) by the
doctor and the CM or the chief nursing (Make pre-
liminary analysis). If there are really features not
complying with this type of hospitalization (gateway
Evaluation’s result?) the request is immediately re-
jected (end of the process Rejected). Otherwise, CM
moves to the department to evaluate the patient (Move
to the Dep/Emergency). At first, the CM talks to the
requested doctor to evaluate clinical conditions (Talk
to doctor). All patients are in acute disease but they
must not be in state of bleeding or risk of reanimation.
Then the CM talks to the patient, if he is conscious
and capable of understanding and willing (Talk to pa-
tient), as well as to the family and the caregiver (Talk
to caregiver).
During this meeting the Case Manager explains to
the patient, if possible, and to the family:
• The characteristics of the service.
• The organization of the service.
• The necessity that a person of the family, or some-
one else, collaborates with the hospital’s team.
Already from this phase:
• Evaluation of clinical, functional and cognitive as-
pects.
• A run of diagnosis, care and assistance are estab-
lish to optimize the existing human and material
resources, that is finalized to a held result the best
possible, reducing the days of hospitalization.
• If necessary, a solution of suitable relief is evalu-
ate.
• Since the possible taking in charge of the patient
that possible problem list are analyzed for the fu-
ture resignation.
• Predispose the applications for the supply of aids
and garrisons that can be useful to the domicile
(for instance, it is possible to require with pro-
cedure of urgency the liquid oxygen that will be
delivered in a few hours to the patient’s house).
The requisite to access the service are:
• As quantitative variable:
– Patient’s residence in the Piedmont Region.
– Patient’s domicile in the geographical area cov-
erage by the service (half city of Turin).
– Clinical characteristics to be asked for hospital-
ization without an invasive or intensive moni-
toring. Are exclusion criteria the need of me-
chanical ventilation, a monitoring more fre-
quent than every 2 hours of blood pressure or
haemogasanalysis, patients with an heart attack
or with very low levels of oxygen in the blood
or with a serious acidosis or alkalosis or with a
suspect of pulmonary embolism.
• As qualitative variable:
– Signature of the informed consent of the patient
and/or of the family, that imply the consent of
and the will to access to this service.
SIMULTECH 2019 - 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
296

– Suitable family support.
Through this structured interview of mutual
knowledge, Case Manager attentively appraises the
real availability to accept the cares to house, if it is
possible to identify a caregiver, so the avaialility of
taking in charge the patient in this type of hospitaliza-
tion.
The requests could be forward both from each de-
partments of the hospital and from the emergency
department. For both of them the activities already
shown are always the same, but after having talked to
all the interested parts, the decisional trial is different
according to where they are (gateway Where?).
If they are in the emergency department there is
an urgent need to free up beds. Any bed of the emer-
gency department can be busy for more than 24 hours.
Therefore, the evaluation result must be immediately
positive or negative (gateway Result?). If it is neg-
ative the request is definitively rejected (Rejected).
Probably the patient have not the requirement and he
is transferred in a classical departments. If the parts
(CM-patient-caregiver-patient’s family) reach the ac-
cord to hospitalize at home the CM signs the policy
of admission (Sign policy of admission), the emer-
gency department’s doctor compiles the emergency
report (Compile emergency report) and then the CM
books the ambulance for the transport to the patient’s
domicile through ambulance of the service of trans-
port settled with the hospital (Book ambulance) and
finally the CM fill out the nurse form asking dates to
the patient/caregivers, collects some patient’s infor-
mation, give to the patient and to his family some in-
formation about the service including an “Informative
Card” with information on the service and about or-
ganization of the next tasks and at the end makes to
sign and pick up informed consent to the patient, or
to the caregiver if the patient is unable (Fill out the
nurse form + Pick up informed consent).
If the request came from a classical department
of the hospital the result of the evaluation (gateway
Result?) could be:
• Positive: the patient is taken in charge, so the CM
books the ambulance, give and take different in-
formation, compile the nurse form and make sign
the informed consent to the patient, like the pre-
vious process (Book ambulance and Fill out the
nurse form + Pick up informed consent).
• Really negative: CM suggest an alternative route
to the patient (gateway Make an alternative
route?) and the request for this type of hospital-
ization is definitively rejected (Rejected).
• Negative but really Suspended: often the family
need time to organize themselves or to required
medical products or it is necessary to talk also to
the ”real” caregiver that remain with the patient
or to other family members, so it is a temporary
reject (Suspended), but the CM takes another ap-
pointment.
To establish this contract of trust and collabora-
tion among patient and hospital is essential that the
CM talks to the whole family nucleus to narrow con-
tact with the patient, that must take care and divide
assignments and responsibility and finally with the
caregiver, that could be a relative or not. It is nec-
essary that all these people are informed, aware and
give the consent to the service, otherwise there could
be severe consequences in terms of collaboration that
could affect the patient’s care.
In this case, the Case Manager will have other tour
(gateway First evaluation arrow 2
◦
visit). These oth-
ers visit are in average 1, 2, 3 or at most 4 in particular
cases, maybe if there is the need to wait some medical
products that have to be order. These other visit are
not made by the different doctor with other requests,
but the Case Manager take the appointment on a case-
by-case bases directly with the patients. The activ-
ities remain the same but need to less time then the
firsts. This second evaluation could be exist only in
the department (gateway Where, 2
◦
visit), for reasons
already explained. In all these visits is possible both
taken in charge the patient, or a rejected the request
or a suspended it for another visit and the trial can be
repeated until the patient will be taken in charge, or
the service will be refused, or the patient will die or
will be discharge.
In all cases in which the patent go at home in a
different day from the request of the HHS, the Case
Manager autonomously goes to the patient before he
goes away, with the purpose to make sure that all the
information are clear. It imply the remake of the three
activities already explain but in less time.
At the end of this trial with the patient the Case
Manager came back to her department’s office and
make the administrative tasks for the patients just
taken in charge. On the hospital’s computer system
the CM has to make the prescription of the Hospital-
ization at Home (Make HaH prescription) and the
formal taking in charge in the department of the Hos-
pitalization at Home (Make taking in charge). In
the meantime, as soon as the doctors and the nurses
arrive the CM informs them about the new patients
(Transfer of power). At this time the request is also
formally accepted and the patient is definitively in the
workload of the department of the Hospital at Home
(Accepted).
Modeling and Simulation of the Hospital-at-Home Service Admission Process
297
4 SIMULATING BUSINESS
PROCESSES
4.1 Analysis of Input Requests
We analyze and simulate the real date of the hospital
in the years 2017 and 2018.
The arrival of patients follows a not uniform dis-
tribution and this is because activation of the service
can happen:
• On direct application of the physician of general
medicine in alternative to the dispatch of the pa-
tient in Emergency Department.
• On application of the physicians of the depart-
ments of hospitalization of the hospital.
• Directly from the Emergency Department for pa-
tients transferred home within few times (in av-
erage 7-8 hours), after the necessary diagnostic
checks.
Doctors makes requests for this type of hospital-
ization mainly in three occasions:
• When the patients request this service because he
already use it and the conditions of the pathology
are conform to this type of hospitalization.
• When doctor is enough convinced that the patient
would have great benefits with this type of hospi-
talization.
• When there are few department’s beds and some
patients could profit of this type of hospitalization
freeing beds, especially in the emergency depart-
ment.
Today, approximately 60% of the HHS depart-
ment’s patients are referred by the Emergency De-
partment (ED), 25% by hospital wards and 15% by
specialist or general physicians in the community.
Table 1: Daily distribution of the arrival request.
R + CM visit R rej. by phone Total
2017 468 96 558
2018 516 103 619
Total 994 199 1,193
Analyzing hospital data base, it is shown, in Table
1, the number of the requests that have wanted at least
one CM visit (R + CM visit) and the number in av-
erage of the request that are immediately rejected by
phone, without a CM visit (R rejected by phone), in
years 2017 and 2018. The number of request imme-
diately rejected are an average number because they
don’t report this call in the data base. This value has
been arranged with the CM.
4.2 Case Manager Workload: Data
Analysis
The workload of the Case Manager depend not only
by the real number or the request made by the differ-
ent doctors, but also, as shown in the process (Figure
1), by the other appointment on a case-by-case basis
that the CM autonomously take with the patient.
Starting to the Table 1 and according to the data
base analysis we can estimate about that the workload
of the Case Manager is incremented of the 57% by the
visits after the first.
Table 2: Increasing of the CM’s workload by the seconds
visits, in 2017-2018.
Tot.R+CM visits Tot.CM visits Diff.(%)
994 1,742 43%
Table 2 considers the sum (Total) of the column
R + CM visit of Table 1 comparing the results of the
Case Manager database of the HHS.
The increasing of the workload of the CM, al-
most 50%, shows how much balancing all these vari-
ables, above the qualitative once, increase the work-
load. This is made with the purpose to create a clear
collaboration, stable in time that will lead advantages
in the workload of the team that will go home and to
the patient’s care.
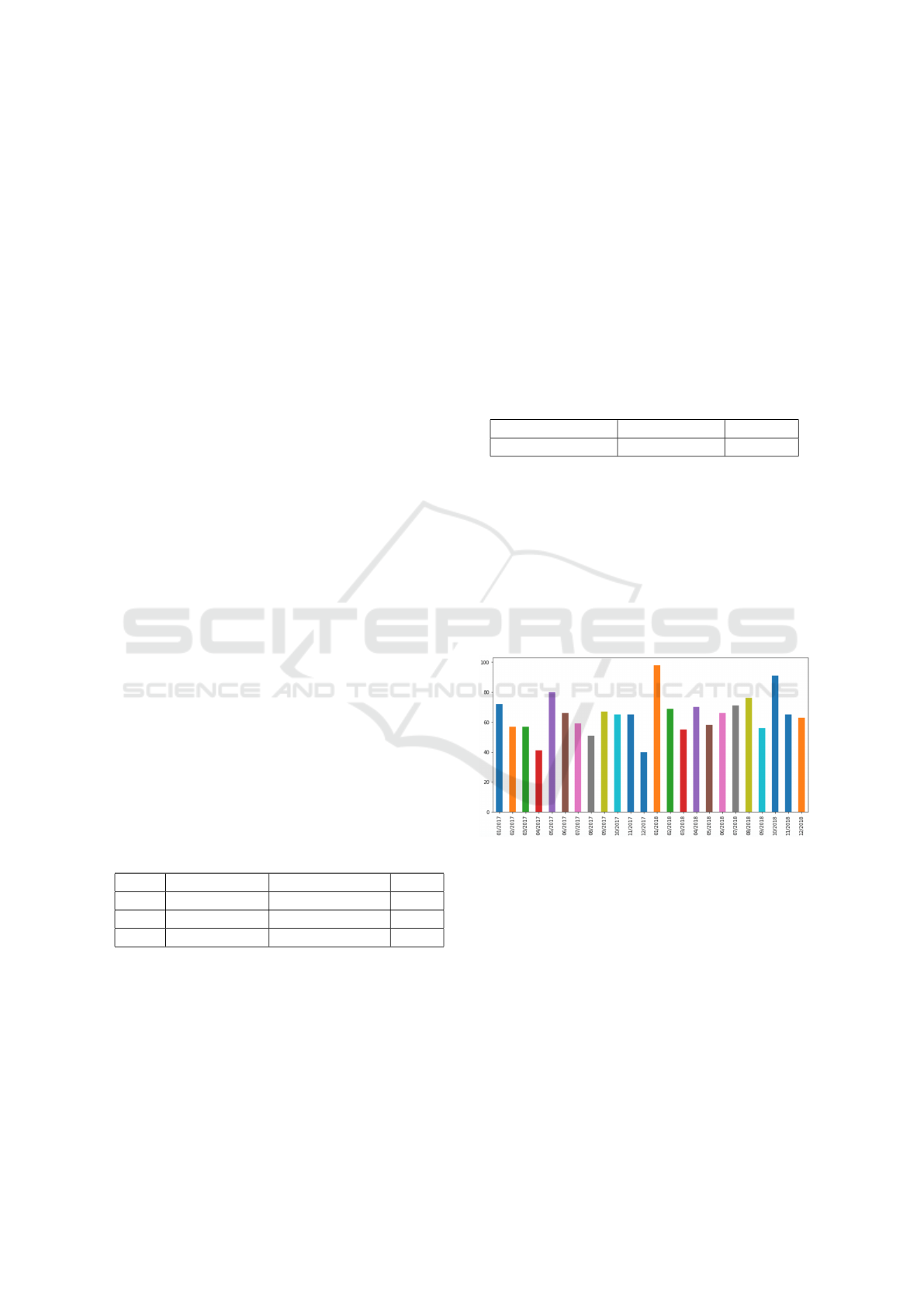
Figure 2: Arrivals of patients at the HaH service in 2017
and 2018 in the different months.
Therefore, Figure 2 describes how the CM’s work-
load changed monthly in last two years. For example,
in January or autumn there were some peaks, mostly
related to periods of flu. On the contrary, near (Ital-
ian) festivity days (i.e. April 2017) there were less
requests, maybe because people are less available to
move out from the city.
Another analysis that we made concerns the dif-
ference of the CM’s workload made by the Emer-
gency department and the other classical department.
This analysis is shown in Figure 3.
It is notable the difference as the requests by the
Emergency department imply only one visit, a more
SIMULTECH 2019 - 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
298

Figure 3: Worlkoad of the Case Manager of HHS in
2017 and 2018 from Hospital Departments (DEP) and from
Emergency Department (ED).
quickly decision and two more documents for each
patients. The request provided by the different de-
partment, in addition to the fact that the departments
are more then one, there is some more time and the
visits are frequently more then one.
We also computed the average daily arrival of pa-
tients by day, which is about 3.5 with a standard devi-
ation of about 2. Interestingly, the distribution varies
across days with a peak in the first part of the week.
Table 3 describes the average value of patients the
modal value and the standard deviation for each day
by considering the period between 2017 and 2018.
Table 3: Daily distribution of the CS’s workload: average
(Avg), modal value (Mode) and standard deviation (StDev).
Mon Tue Wed Thu Fri
Avg 4.05 4.05 4.09 3.35 2.56
Mode 4.00 4.00 3.00 3.00 2.00
StDev 2.04 2.04 2.03 1.72 1.62
The actual process has been validated by managers of
the hospital department as well as accurately verified
in actual and future simulation results. In particular,
besides changes related to the arrival of patients, we
investigate variations in the execution times of work-
ers and organizational changes.
4.3 Output with Different Arrivals
The output of the Case Manager evaluation directly
affect on the workload of the HHS department, so on
the job of the team doctor+nurse that day by day have
to go to the different patient’s home.
The team looks after 25 patients per day and 500
patients per year, on average. Figure 4 show the ac-
cepted requests, so the patients taken in charge in
2017 and 2018, from Hospital Departments (DEP)
and from Emergency Department (ED). Curiously,
the accepted requests by the Emergency Department
follow a similar trend of the provided requests. This
Figure 4: Patients taken in charge in the HHS in 2017 and
2018, from Hospital Departments (DEP) and from Emer-
gency Department (ED).
is because, if it is possible, it is easier to free a bed of
the Emergency Department avoiding simply to move
the patient to another bed of a classical department.
The number of patient in charge each day has to be
balanced with the patients that leave the service, in
order to guarantee an adequate workload for the team
and an adequate level of care, according to the first
evaluation activity explained in Figure 1 (Evaluate
n
◦
place available).
Table 4: Description of the requests accepted and rejected
in 2017 and 2018.
2017 2018
Patients taken in charge 468 489
Patient rejected from DEP 10 22
Patient rejected from ED 2 5
Request rejected by phone 96 103
Table 4 describes the number of patients taken in
charge in two last years. The fact that the rejected
patients are very few is also thanks to an adequate
information and collaboration between the doctor of
the Emergency and other classical departments and
the staff of the HHS.
4.4 Scenario Analysis
Beside scenario As-Is, we plan to modify some fea-
tures of the organisation as the introduction of dif-
ferent execution time of workers (i.e. stagiest ver-
sus expert workers) in expert-stagiest scenario, the re-
structuring of the whole process with different activi-
ties in re-engineering scenario, or the working shift of
staff in part-time scenario. The interest of managers
in considering the introduction of different execution
time of workers concerns the ability to produce more
realistic scenario including young specialist nurses
and doctors besides actual experienced workers. In
other analysis some tasks in the flow can be slightly
modified, to investigate the outcome on the whole
Modeling and Simulation of the Hospital-at-Home Service Admission Process
299

time execution of the process. Finally, by introduc-
ing part-time worker shift some considerations can be
added with respect to different organisation planning,
i.e. obeying to some special request from workers.
5 CONCLUSIONS
This research describes a methodological framework
to model and simulate an hospital admission process.
We applied the standard language modeling BPMN
to introduce a simulation effort based on real data. In
future works, we consider to investigate the remain-
der of the process, as well as the trajectories of the
operators on the territory towards the patients’ home
with social network analysis by combining geograph-
ical information systems and agent-based modeling to
improve the analysis and simulation of the HHS pro-
cess (Sulis and Di Leva, 2017). Moreover, we plan
to investigate several scenarios to provide some sug-
gestions to managers by offering insights on organ-
isational aspects, also including an increment of pa-
tients as in the case of an extension with respect to
the actual service. In addition, we aim to explore dif-
ferent options concerning the arrivals of patients by
investigating the extension of the service to another
area of the same city. As the HHS actually involves
only the southern part of Turin, we plan to investigate
the extension to the northern area: that would mean
mostly doubling the arrivals of patients. In particu-
lar, we afford this research question to manage such
increment of patients by planning different configu-
ration settings, also involving the staff dimension, in
order to produce optimal results for decision-makers.
ACKNOWLEDGEMENTS
This research was conducted in the project “CANP
- CAsa Nel Parco” of Regione Piemonte funded by
POR FESR PIEMONTE 2014-2020. We are grateful
for the collaboration of the “City of Health and Sci-
ence” of Torino (Italy).
REFERENCES
Aimonino Ricauda, N., Tibaldi, V., Bertone, P., Chiusano,
V., Piano, S., Grillo, S., Rocco, M., Marinello, R.,
and Isaia, G. (2011). L’ospedalizzazione a domicilio.
Proceedings of SIGOT - Italian society of geriatrics,
Suppl.Vol.XXIII(1):53–62.
Allweyer, T. (2016). BPMN 2.0: introduction to the stan-
dard for business process modeling. Books on De-
mand.
Amantea, I. A., Leva, A. D., and Sulis, E. (2018). A
simulation-driven approach in risk-aware business
process management: A case study in healthcare. In
Proceedings of 8th International Conference on Sim-
ulation and Modeling Methodologies, Technologies
and Applications - Volume 1: SIMULTECH,, pages
98–105. INSTICC, SciTePress.
Di Leva, A. and Sulis, E. (2017). Process analysis for a
hospital emergency department. International Journal
of Economics and Management Systems, 2(1):34–41.
Dumas, M., La Rosa, M., Mendling, J., and Reijers, H.
(2018). Fundamentals of business process manage-
ment, volume 1. Springer, 2nd edition.
Dumas, M., van der Aalst, W. M., and ter Hofstede, A. H.
(2005). Process-aware Information Systems: Bridg-
ing People and Software Through Process Technology.
John Wiley & Sons, Inc., New York, NY, USA.
Grosso, M., Scardino, M., Cerutti, S., Guida, A., Tibaldi,
S., Sardo, P., Davini, O., and Marinello, R. (2018).
Telemedicina e fragilita’ clinica: il progetto la casa nel
parco. eHealth. Innovazione e tecnologia in ospedale,
65.
iGrafx (2015). iGrafxProcess 2015. http://www.igrafx.com.
Johnson, M. W., Christensen, C. M., and Kagermann, H.
(2008). Reinventing your business model. Harvard
business review, 86(12):57–68.
Mans, R., Van der Aalst, W., and Vanwersch, R. (2015).
Process mining in healthcare: evaluating and exploit-
ing operational healthcare processes. Springer.
Rojas, E., Munoz-Gama, J., Sep
´
ulveda, M., and Capurro,
D. (2016). Process mining in healthcare: A literature
review. Journal of Biomedical Informatics, 61:224 –
236.
Russo, V., Ciampi, M., and Esposito, M. (2015). A busi-
ness process model for integrated home care. In EU-
SPN/ICTH.
Sulis, E. and Di Leva, A. (2017). An agent-based model
of a business process: The use case of a hospital
emergency department. In International Conference
on Business Process Management, pages 124–132.
Springer.
Suriadi, S., Weiß, B., Winkelmann, A., ter Hofstede, A. H.,
Adams, M., Conforti, R., Fidge, C., La Rosa, M.,
Ouyang, C., Rosemann, M., et al. (2014). Current
research in risk-aware business process management:
overview, comparison, and gap analysis. Communica-
tions of the AIS, 34(1):933–984.
Van der Aalst, W. M. (2013). Business process manage-
ment: a comprehensive survey. ISRN Software Engi-
neering, 2013.
Van der Aalst, W. M., Nakatumba, J., Rozinat, A., and Rus-
sell, N. (2010). Business process simulation. In Hand-
book on BPM 1, pages 313–338. Springer.
Vincent, C., Amalberti, R., et al. (2016). Safer healthcare.
Cham: Springer International Publishing.
SIMULTECH 2019 - 9th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
300
