
SMART TRANSPLANTATION
Fever of Unknown Origin after Stem Cell Transplantation as a Model for a
Knowledge-Based Decision Support System in Medicine
Gerrit Meixner
1
, Nancy Thiels
2
1
University of Kaiserslautern, Gottlieb-Daimler-Strasse, Kaiserslautern, Germany
²German Research Center for Artificial Intelligence (DFKI), Trippstadter Strasse, Kaiserslautern, Germany
Ingo Haschler
3
, Andreas Wicht
4
and Ulrike Klein
5
University of Heidelberg, Im Neuenheimer Feld, Heidelberg, Germany
Keywords: Human-Computer Interaction in Health Care, Usability of Medical Information Systems, Human Aspects of
Future Technologies in Health Care, Cognitive Task Analysis, Usability Engineering, Stem cell
transplantation, Decision support system.
Abstract: Public health care has to make use of the potentials of IT to meet the enormous demands on patient
management in the future. Embedding artificial intelligence in medicine may lead to an increase in health
care quality and patient safety. One possibility in this respect is the use of knowledge-based decision
support systems which facilitate the practice of evidence-based medicine. Conditions for such a system are
structured data sources to extract relevant data for the proposed decision. Therefore, the demonstrator “allo-
tool” was designed. To develop the allo-tool a user-orientated process was applied and future users of the
later software were integrated in each step of the development process. The concept of introducing a
"Medical decision support system based on the model of Stem Cell Transplantation" was developed
afterwards. The global objectives of the planned system are (1) to improve patient safety (2) to support
patient autonomy and (3) to optimize the work flow of medical personnel.
1 INTRODUCTION
In many areas of human life, computer-based
Information Technology (IT) has prevailed and has
become essential for the coordinated and efficient
organization of work flow. This offers numerous
advantages for the future, but will also lead to
problems for the people confronted with it.
Especially in the field of health care, interaction
between human beings and information technology
is a sensitive subject. Physicians have immense
reservations and apprehensions of being made the
slaves of information scientists and of their
programmed computer system. Nevertheless,
medicine has to become more scientific in patient
management. The importance of interdisciplinary
advice and discussion which is a prerequisite for the
best possible decision on a treatment strategy has to
be reflected in the application of new information
technologies.
Embedding artificial intelligence in medicine
may lead to an increase in quality and safety and to a
decrease in costs significantly. In the future, IT-
systems are supposed to have the ability to extract
the relevant knowledge to filter irrelevant
information and focus on significant information and
to present it available to the user. Inevitably, people
working in health care will have to make use of the
potentials of IT in order to meet the enormous
demands on patient management in the future.
One possibility in this respect is a knowledge
based decision support system which facilitates the
practice of evidence-based medicine. The idea of
medical decision support systems is not new. In the
past, however, these systems have not become
popular and utilized. The reason was not that the
technology had failed, but that the implementation
was inadequate. A prerequisite for success is that we
understand "how medicine thinks" in order to be
298
Meixner G., Thiels N., Haschler I., Wicht A. and Klein U. (2008).
SMART TRANSPLANTATION - Fever of Unknown Origin after Stem Cell Transplantation as a Model for a Knowledge-Based Decision Support System
in Medicine.
In Proceedings of the First International Conference on Health Informatics, pages 298-304
Copyright
c
SciTePress

able to create a "decision-supporting", and not a
"decision-making" system.
Decision support systems need an evaluation of
their applicability and of their cost-benefit
relationship as well as the evaluation of precision,
quality, and effects of their recommendations.
Against the background of the challenges mentioned
above, the concept of introducing a "Medical
decision support system based on the model of Stem
Cell Transplantation", named allo-tool, was
developed.
Whenever bringing a decision support system
into clinical practice, one has to consider the
possible harms caused by the system. Concretely
this means to consider what happens if the system
recommends a wrong decision or presents
incomplete or inadequate information at the point of
care to the physician. We therefore plan to integrate
a feedback mechanism. In the case that a physician
has the opinion that the system could recommend
something wrong, he will submit an incident report
to the maintenance team. In that way, the users (i.e.
mainly the physicians) will retain control over the
system and possible harm to the patients caused by
the system will be minimized.
The global objectives of the planned system are
(1) to improve patient safety (2) to support patient
autonomy and (3) to optimize the work flow of
medical personnel. It might lead to more efficient
use of resources without detrimental effects on the
relationship between physician and patient or on the
physician's autonomy to decide. The allogeneic
haematopoietic stem cell transplantation is
extremely well suited as a model for this type of
system because of repeating standard procedures, the
well defined span of time required and the
predictable recovery period as well as recurrent side
effects after transplantation.
2 STEM CELL
TRANSPLANTATION
Hematopoietic stem cell transplantation (HSCT) or
bone marrow transplantation (BMT) is a medical
procedure in the field of hematology and oncology
(Korbling, 1986). It is most often performed for
people with diseases of blood or bone marrow
(Gratwohl, 2007; Goldschmidt, 2000). HSCT
remains a risky procedure and has always been
reserved for patients with life threatening diseases.
Since the availability of stem cell growth factors,
most hematopoietic stem cell transplantation
procedures have been performed with stem cells
collected from the peripheral blood (Montgomery,
2007). Most recipients of HSCTs are patients with
leukemia or aggressive hematological tumors who
would benefit from treatment with high doses of
chemotherapy or total body irradiation. Other
patients who receive bone marrow transplants
include pediatric cases where patients have an
inborn defect and were born with defective stem
cells. Other conditions that bone marrow transplants
are considered for include inherently diseases of the
bone marrow. More recently non-myeloablative, or
so-called "mini transplant," procedures have been
developed which do not require such large doses of
chemotherapy and radiation (Djulbegovic, 2003).
This has allowed HSCT to be conducted in older
patients and as a matter of principle without the need
for hospitalization. There are two major types of
stem cell transplantation maneuvers: Autologous
HSCT involves isolation of HSC from a patient,
storage of the stem cells in a freezer, high-dose
chemotherapy to eradicate the malignant cell
population at the cost of also eliminating the
patient's bone marrow stem cells, then return of the
patient's own stored stem cells to their body.
Autologous transplants have the advantage of a
lower risk of graft rejection, infection and graft-
versus-host disease. Allogeneic HSCT, as the second
type, involves two people, one is the healthy donor
and one is the recipient. Allogeneic HSC donors
must have a tissue type that matches the recipient
and, in addition, the recipient requires
immunosuppressive medications. Allogeneic
transplant donors may be related or unrelated
volunteers.
The number of performed HSCT, autologous and
allogeneic, is increasing. Due to better anti-infective
medication the life-threatening side effects of
infectious complications are decreasing but they still
remain as the main risk factor for life threatening
side effects (Walker, 2007; Afessa, 2006).
Therefore one intention of the allo-tool is the
improvement of patient safety through a decision
support system for choosing an anti-infective
therapy based on evidence based advices.
Bacterial, viral or fungal infections are severe
side effects of high dose chemotherapy and stem cell
transplantation and can result in life threatening
complications. Infections are the most important
causes of morbidity and mortality in patients
undergoing allogeneic stem cell transplantation.
That is why immediate anti-infective therapy in case
of fever is mandatory (Afessa, 2006). Because of the
resistance to widely used antibiotics and a shift of
SMART TRANSPLANTATION - Fever of Unknown Origin after Stem Cell Transplantation as a Model for a
Knowledge-Based Decision Support System in Medicine
299

Figure 1: Risk chart graphic.
causative pathogens towards multi-resistant bacteria,
anti-infective therapy remains to be a challenge.
Beside this drug-interaction, kidney function, known
allergies, the cause of fever and former anti-infective
therapies needs to be included into the decision of
the treatment of choice. Therefore the model of a
decision support system was developed. The idea of
programming and implementing such a system is not
new. Attempts of this type had already been initiated
in the Eighties (then called medical expert systems)
(Shortliffe, 1975). In the past, however, these
medical expert systems have not become popular
and utilized. The reason was not that the technology
had failed, but that the implementation was
inadequate.
Beside this the support of patient autonomy
through modern forms of communications like web-
based access to specific patient data and the
optimization of the work flow in the complex
process of an allogeneic transplantation is the goal
of the allogeneic tool “smartTransplantation”.
3 USEWARE ENGINEERING
PROCESS
The level of acceptance and efficiency of a modern
user interface are determined by the ease of use of
the interface. Primary considerations in this
evolutionary development process are always the
requirements and needs of the user, for whom the
user interface is being developed. The process
consists of analysis, structural design, rough and
detailed design, implementation, and evaluation
(Zühlke, 2004). As a continuation of the analysis,
evaluation occurs concomitantly to the development.
A risk chart (see Fig. 1) has been developed to
get an understanding of the transplantation
procedure. It explains the work flow of the stem cell
transplantation in detail. The preparation of the
analysis phase derived five different user groups.
From these user groups ten different persons were
chosen to be questioned to find out the tasks and
needs of users for the later user interface.
After the questioning and characterizing, the
collected data were compiled (Bödcher, 2007).
Additional results included an analysis of
weaknesses identified in the existing user interfaces
and documentation of the “wish list” expressed by
the users. Problems to be found within the analysis
of the clinical situation for the stem cell
transplantation were published.
Based on the task models of the different user
groups, the use structure for the future user interface
was developed. The modeling language useML
(Reuther, 2003) was used in structural design. The
result of the structural design phase is a platform-
independent model and it provides the foundation
for the later design phase. This model formed the
base for the development of the prototype.
4 PROTOTYPE: ALLO-TOOL
The intention of the allo-tool is not only the
optimization of the work flow in the complex
process of an allogeneic transplantation, but also the
provision of a structured platform for relevant data.
This aim is reached by data integration from
different existing information sources: clinical
information system, drug information system and
paper patient files as well as domain knowledge
formalized in knowledge bases (described in more
detail in chapter 5). The digitized aggregated data is
displayed in a clearly structured way.
The tool shall be able to extract medical
information from different sources, structure the
HEALTHINF 2008 - International Conference on Health Informatics
300
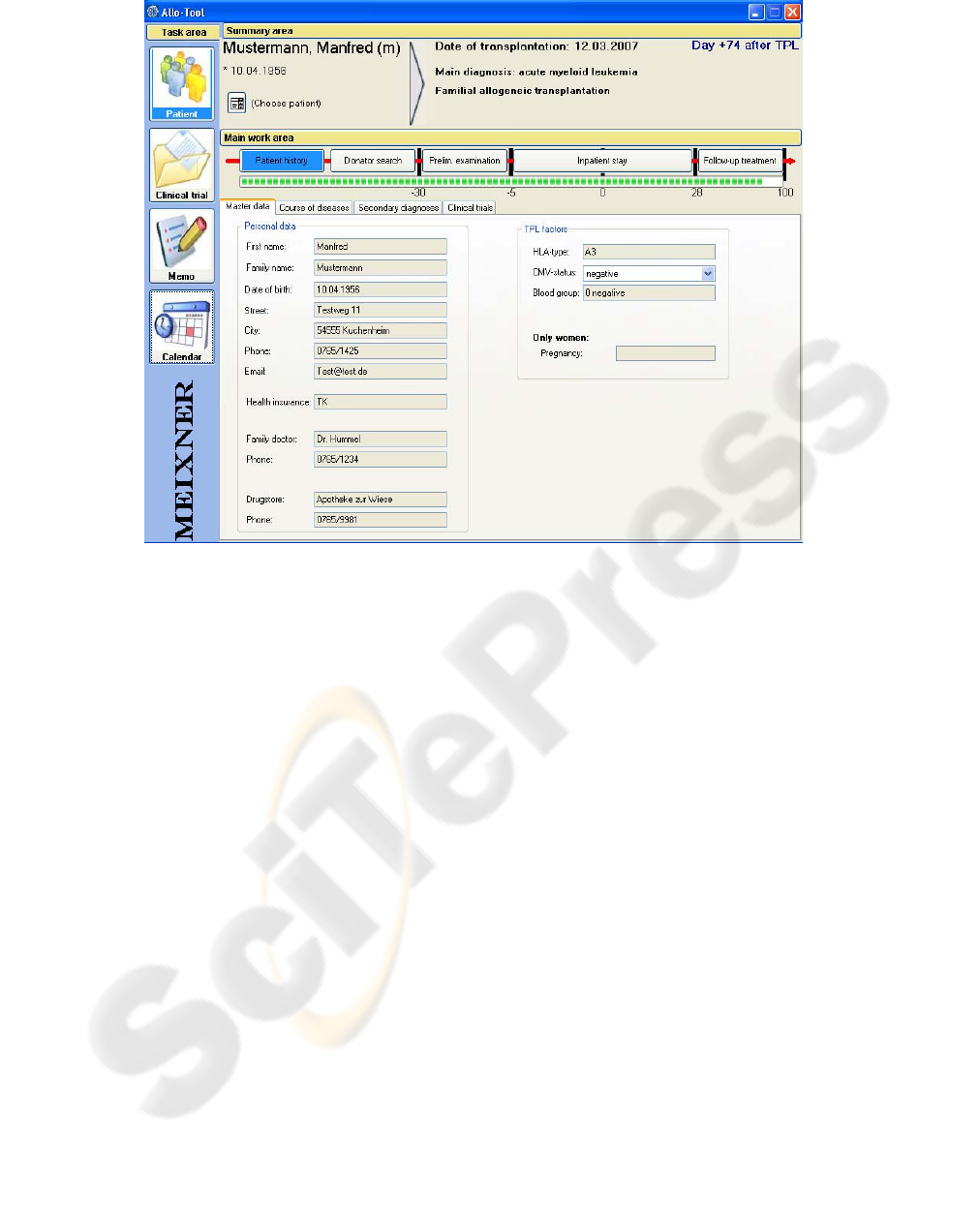
Figure 2: Patient history screen in the detailed view.
information and automatically generate discharge
letters and further documents, e.g. drug plans.
Each user group is able to work consistently with
the allo-tool. The tool consists of four main views:
calendar, memos, clinical trials and patients. The
memo view consists of a text field, where the user
has the possibility to take notes. In the clinical trial
view the user is able to administrate information
about current clinical trials.
For allogeneic transplantations information about
conditioning, transplantation, immunosuppression,
GVHD prevention (graft versus host disease) and
donor lymphocyte transfusions are stated within
these clinical trials.
According to the work flow of an allogeneic
transplantation, the detailed patients view consists of
five different chronological parts in the main work
area of the tool: patient history, donator-search,
preliminary examinations, inpatient stay and follow-
up treatment. These five parts are clearly separated
phases in the time line of an allogeneic
transplantation (see Fig. 1). The graphical
representation of a time line (see Fig. 2) enables
physicians to have a better understanding (Norman,
1990) of the current date according to the complex
process of an allogeneic transplantation. The tool
supports physicians in keeping deadlines according
to a physical examination time schedule.
The patient’s history phase (see Fig. 2) consists
of a structured overview of the patient’s master data.
In the course of diseases previous examinations and
medical results are displayed in a table view.
Secondary diagnoses are an important part of the
decision supporting system and help to minimize
adverse effects.
The preliminary examination phase contains
information about the accomplished examinations
according to the physical examination time schedule.
The results of external examinations are entered into
the clinical information system. The allo-tool shall
be able to extract the results of external
examinations.
In the phase of hospitalization, the patient
receives high dose chemotherapy and some patients
a whole body irradiation. After that the allogeneic
stem cell transplantation is performed. During the
whole phase patient data (e.g. vital signs, blood
counts or organ functions) are monitored very
closely. Beside others, one important task of the
attending physician is to administrate drug plans.
Via an implemented interface, physicians are
able to use an existing drug information system
(Kaltschmidt, 2004;
Pruszydlo, 2006).
SMART TRANSPLANTATION - Fever of Unknown Origin after Stem Cell Transplantation as a Model for a
Knowledge-Based Decision Support System in Medicine
301

In the follow-up phase the physician is reminded to
accomplish examinations according to the physical
examination time schedule. The time schedule
consists of a large number of physical examinations
and complex execution logic. The prototype
transfers the execution logic from the physicians to
the software.
Patients in the follow-up phase have the
possibility to access test results via internet and can
directly communicate with their allocated physician
via email. This will be reached by developing a web-
based access for patients. Patients will have the
possibility to view their own data (e.g. blood test
results, X-ray photographs). Test results, which can
be viewed by patients over internet are evaluated
and released by their allocated physician. Patients in
the follow-up phase have to control e.g. blood
pressure values. They can measure blood pressure
on their own and email the results over the web-
based access directly to their allocated physician. So
patients don’t have to call the hospital via telephone
or have to visit the hospital on their own.
5 KNOWLEDGE-BASED
SUPPORT
In the future, physicians will be supported by a
knowledge-based system with data mining
capabilities. The detailed functionality is explained
in the following.
Monitoring and interpretation of several
parameters such as vital signs or laboratory results
will be one main function of the knowledge-based
system component. The system thus detects specific
clinical situations and pushes unsolicited warnings
or reminder and starts the according work flow.
In everyday clinical practice physicians are often
faced with an information overflow rather than a
lack of information, they have to spend valuable
time in looking for relevant findings. To reduce this
time a “Semantic Information Extraction” is
provided. The system looks for findings in the
patient’s history which could fit into the context of
the current clinical picture. Furthermore, it
visualizes the classification of the findings, which
has previously to be provided by a physician:
“abnormal”, “no abnormality”, “unclear”. So the
physician gets a clearly arranged listing of relevant
findings matching the current issue.
For a defined amount of clinical pictures,
therapy and diagnostic recommendations are
provided. These recommendations are on the one
hand based on so-called domain knowledge which is
patient-independent knowledge on e.g. diseases or
processes. Domain knowledge will mainly derived
from clinical practice guidelines (CPG) or in-house
standard operating procedures (SOP). On the other
hand they are based on available patient data such as
current parameters as well as the patient’s general
data (if any parameters are missing or out of date,
the system will ask the user to enter these), the
system should give exact medication and dosing
recommendations. Once the system has generated a
recommendation, it will also provide the user with a
reasonable explanation. In this context it may also be
helpful that the user is guided to external knowledge
resources, which match the current clinical picture,
such as local SOP-documents, relevant study
protocols or other medical knowledge bases, if
further information is requested.
Recommending a (drug) therapy at first requires
a knowledge base which encapsulates the SOPs and
the guidelines’ knowledge. The process of
formalizing guidelines and SOPs is a challenging
and time-consuming task (Kaiser, 2007). We will try
to build a semi-automatic, peer-reviewed process,
i.e. the system will try to import the unstructured
material and recognize as much structure as
possible. In the next step a specially trained medical
professional will then review and complete
structural or semantic issues. Afterwards, another
medical professional will review the work of the
first one to ensure high quality of the formalized
knowledge.
Once the therapy decision was accepted and
started, the system supports the medical staff by
monitoring not only the over-all treatment work
flow, but also the flow of the specific therapy.
Concerning the over-all treatment work flow, the
system should give reminders or warnings if
scheduled diagnostic procedures (e.g. ECG) are not
done or assigned yet or scheduled medications (e.g.
antibiotic prophylaxis) are not ordered. Regarding
the therapy monitoring, the system should detect if a
patient does not respond to the treatment (e.g.
patient remains febrile) and recommend necessary
steps and/or alternative therapies as well as indicated
diagnostic procedures. On the other hand, the system
should detect if a therapy was apparently successful
and recommend further steps (e.g. to stop antibiotics
and to start a prophylaxis again). In this context the
system presents - as already mentioned before -
reasonable explanations and guides the user to
external knowledge resources if requested.
As medical knowledge is subject to ongoing
changes, the knowledge base has to be maintained
regularly. Changes can be triggered either by
external factors (e.g. update of a guideline) or by
internal factors. We therefore need a user feedback
mechanism which enables a physician to mark a
system’s decision as potentially wrong. The user
HEALTHINF 2008 - International Conference on Health Informatics
302

feedback has to be analyzed and the need to change
the knowledge base has to be assessed. All changes
to the knowledge base must be carried out within a
“bullet-proof” process like the one described above.
A critical issue when it comes to the
implementation of decision support systems is user
compliance. In our environment we face mainly
physicians as users, but also patients in an advanced
state of the software (e.g. test results via web-based
access). We have to ensure usability of the tool (as
described earlier) and ensure that physicians get a
benefit from it. The patients are most likely to do
everything to improve their therapy outcome
because of their severe illness.
One reason why decision support systems often
do not prevail in clinical practice is poor work flow
integration (Bates, 2003). Since our software will
cover the SCT-treatment process as a whole we can
map the practical work flow. Physicians will more
likely use a decision support system if they see a
clear benefit from it. This means mainly time-saving
as well as convenient access to all relevant
information.
Because the decision support system will be
seamlessly embedded as a component into the allo-
tool, we can reach an optimal solution to this
obstacle. All of the knowledge-based features we
presented above will appear within the current work
flow context. We provide the medical user with only
the information he or she needs at a given clinical
situation. Therefore we can expect a reasonable time
saving for the users. By ensuring that we do not miss
relevant information on the other side, we may raise
quality of treatment and patient safety.
6 CONCLUSIONS
It is incontestable that people working in health care
will have to make use of the potentials of IT in order
to meet the enormous demands on patient
management in the future. Beside this the quality of
work can be supported by intelligent software which
is able to extract, rate and provide the user with
relevant data. Not least patients require more
autonomy of their own health information data. To
meet this challenges the demonstrator of the allo-
tool was developed.
Time consuming data search, redundant
information and vast numbers of needed software
applications are reduced by displaying all data in
one tool. User interfaces, which are designed in
close relationship to known software products,
developed with the support of different users during
the whole process and consulting of usability experts
facilitate an easy-to-use application. Time schedules,
reminder of deadlines and coherent information
about study procedures enable medical staff to work
efficiently. Taking these analysis results as a basis,
conditions for a medical decision support system are
accomplished. In order to meet the exploding
number of scientific perception, decision support
systems are needed in the future to maintain the
quality of medical decisions.
Through web-based access to selected health
information, patients obtain more autonomy and
responsibility. Summarizing the potentialities of the
planned allo-tool, the goals mentioned at the
beginning, (1) improvement of patient safety (2)
support of patient autonomy and (3) optimizing the
work flow of medical personnel are illustrated.
Studies to evaluate these potentialities are needed to
prove these advantages of the allo-tool.
ACKNOWLEDGEMENTS
This work was supported by the Gottlieb Daimler-
and Karl Benz-Foundation.
REFERENCES
Afessa, B.; Peters, S.G., 2006. Major complications
following hematopoietic stem cell transplantation,
Semin Respir Crit Care Med, 2006, 27(3), 297-309.
Bates, D. W.; Kuperman, G. J.; Wang, S.; Gandhi, T.;
Kittler, A.; Volk, L.; Spurr, C.; Khorasani, R.;
Tanasijevic, M.; Middleton, B., 2003. Ten
commandments for effective clinical decision support:
making the practice of evidence-based medicine a
reality, J Am Med Inform Assoc, 2003, 10, 523-30.
Bödcher, A., 2007. Methodische Nutzungskontext-Analyse
als Grundlage eines strukturierten USEWARE-
Engineering-Prozesses, Fortschritt-Berichte pak, no.
14, Kaiserslautern: University of Kaiserslautern.
Djulbegovic, B.; Seidenfeld, J.; Bonnell, C.; Kumar, A.,
2003. Nonmyeloablative allogeneic stem-cell
transplantation for hematologic malignancies: a
systematic review, Cancer Control, 2003, 10(1), 17-41.
Goldschmidt, H.; Egerer, G.; Ho, A.D., 2000. Autologous
and allogeneic stem cell transplantation in multiple
myeloma, Bone Marrow Transplant, 2000; 25, Suppl.
2, 25-26.
Gratwohl, A.; Baldomero, H.; Frauendorfer, K.; Urbano-
Ispizua, A.; Niederwieser, D., 2007. Results of the
EBMT activity survey 2005 on haematopoietic stem
cell transplantation: focus on increasing use of
unrelated donors, Bone Marrow Transplant, 2007,
39(2), 71-87.
SMART TRANSPLANTATION - Fever of Unknown Origin after Stem Cell Transplantation as a Model for a
Knowledge-Based Decision Support System in Medicine
303

Kaiser, K.; Akkaya, C.; Miksch, S., 2007. How can
information extraction ease formalizing treatment
processes in clinical practice guidelines? A method
and its evaluation, Artif Intell Med, 2007, 39, 151-
163.
Kaltschmidt J.; Gallin S.; Haefeli W.E., 2004. Essential
functional requirements for an effective electronic
drug information system in a hospital, Int J Clin
Pharmacol Ther, 2004, 42:615.
Korbling, M.; Dorken, B.; Ho A.D.; Pezzutto, A.;
Hunstein, W.; Fliedner, T.M., 1986. Autologous
transplantation of blood-derived hemopoietic stem
cells after myeloablative therapy in a patient with
Burkitt's lymphoma blood, J AM Society of
Hematology, 1986, 67(2), 529-532.
Montgomery, M.; Cottler-Fox, M., 2007. Mobilization and
collection of autologous hematopoietic
progenitor/stem cells, Clin Adv Hematol Oncol, 2007,
5(2), 127-136.
Norman, D., 1990. The Design of Everyday Things,
Currency.
Pruszydlo, M.G.; Kaltschmidt, J.; Schmitt, S.P.W.;
Markmann, A.; Bertsche, T.; Haefeli W.E., 2004.
Successful implementation of computer-aided
prescribing in a hospital providing tertiary care, Int J
Clin Pharmacol Ther, 2006, 44:529.
Reuther, A., 2003. useML – Systematische Entwicklung
von Maschinenbediensystemen mit XML, Fortschritt-
Berichte pak, no. 8, Kaiserslautern: University of
Kaiserslautern.
Shortliffe, E. H.; Davis, R.; Axline, S. G.; Buchanan, B.
G.; Green, C. C.; Cohen, S. N., 1975. Computer based
consultations in clinical therapeutics: explanation and
rule acquisition capabilities of the MYCIN system,
Comput Biomed Res, 1975, Aug, 8(4), 303-320.
Walker, C.M.; van Burik, J.A.; De For, T.E.; Weisdorf,
D.J., 2007. Cytomegalovirus infection after allogeneic
transplantation: comparison of cord blood with
peripheral blood and marrow graft sources, Biol
Blood Marrow Transplant, 2007, 13(9), 1106-1115.
Zühlke, D., 2004. Useware-Engineering für technische
Systeme, Springer.
HEALTHINF 2008 - International Conference on Health Informatics
304
