
WHO SHOULD ACCESS ELECTRONIC PATIENT RECORDS
A. Ferreira
1,2
, L. Antunes
2
, C. Pinho
3
, C. Sá
3
, E. Mendes
3
, E. Santos
3
, F. Silva
3
, F. Sousa
3
F. Gomes
3
, F. Abreu
3
, F. Mota
3
, F. Aguiar
3
, F. Faria
3
, F. Macedo
3
S. Martins
3
and R. Cruz-Correia
3
1
Computing Laboratory, University of Kent, Canterbury, Kent, CT2 7NF, UK
2
Department of Computer Science, Faculty of Science, University of Porto, Portugal, partially supported by KCrypt
(POSC/EIA/60819/2004) and funds granted to LIACC through Programa de Financiamento Plurianual, FCT and
Programa POSI.
3
Faculty of Medicine, University of Porto and CINTESIS, Portugal
Keywords: Electronic Patient Record, access control, attitudes.
Abstract: Access control to Electronic Patient Records (EPR) may greatly depend on users’ objectives and needs. The
purpose of this study is to assess the opinions of medical doctors within a university hospital towards access
control to an EPR. We selected a randomized sample of 58 doctors from a university hospital and 45
structured interviews were applied. 42 respondents (93%) agree with the existence of access control levels
to patient information according to healthcare professionals’ category and 31 (69%) think that more
sensitive information (e.g. HIV) should be accessed only by doctors that treat those patients. As 24 doctors
(53%) feel that there is no need for them to see all information about all the patients, 41 (91%) think that
nurses should not be able to do it also. Further, 31 doctors (69%) believe that patients themselves should not
access their full medical record. These results show that it is very hard to get to a consensual policy
regarding access control to EPR by its regular users. There is therefore the need for a multidisciplinary
agreement that can include healthcare professionals’ experiences and needs in order to define the most
appropriate and efficient way to perform access control to the EPR.
1 INTRODUCTION
Good communication between health providers is an
essential component of high quality health care
(Hassol et al., 2004) Paper-based medical record is
still widely used in hospitals, where health
professionals gather patient’s clinical and
administrative information. There is however some
problems with this type of records and so computer-
based medical records are being implemented and
used in a more regular basis (Bakker et al., 2004).
The evolution of technology allows health
providers to communicate electronically and to obtain
information which includes patient’s health story,
examination findings, diagnosis and treatment over a
period of time (Hassol et al., 2004) (Day, 2001).
This enabling technology that constitutes the
informational basis for communication and
cooperation in and between healthcare organizations
is called Electronic Patient Records (EPR) (Ab et al.,
2004).
However, this wide use of information systems
and technologies shows the need for healthcare
organizations to integrate and manage information
from various sources, types and formats. This
reflects the careful scrutiny that electronic access to
medical information requires (Rogerson, 2000).
Information security is then essential, moreover
when people accessing the EPR can have varied
objectives, different types of access and several
processes to execute. Therefore, access control is
essential to provide because it manages one of the
first contacts between users of a system and its
functionalities and features (Ferreira et al., 2005)
(Ferreira et al., 2006).
According to a recent report, more than 1000
accidental deaths have been attributed to computer
system failure (Gritzalis, 1997). Such occurrences
must be present when considering the different
interests and objectives that users want to achieve
when using the EPR.
The Biostatistics and Medical Informatics
Department of Porto’s Faculty of Medicine
182
Ferreira A., Antunes L., Pinho C., S
´
a C., Mendes E., Santos E., Silva F., Sousa F., Gomes F., Abreu F., Mota F., Mota F., Aguiar F., Faria F., Macedo F.,
Martins S. and Cruz-Correia R. (2008).
WHO SHOULD ACCESS ELECTRONIC PATIENT RECORDS.
In Proceedings of the First International Conference on Health Informatics, pages 182-185
Copyright
c
SciTePress

implemented a centralized EPR system (VEPR –
Virtual EPR) between May 2003 and May 2004 in
Hospital S. João (HSJ), Porto, Portugal. This
hospital has more than 1300 beds and 5000 workers
from 56 departments, where about 1000 are medical
doctors, so any access to information needs to be
properly defined, controlled and monitored. A generic
but strong access control policy that reflects people’s
processes and interactions with the system, without
incapacitating its use, is the basis for the VEPR
success and, more importantly, acceptance, trust and
use (Ferreira et al., 2005) (Ferreira et al., 2006). More
than 900 doctors access this system on a daily basis,
and this number is increasing, as healthcare
professionals can feel the benefit from its use.
Even patient’s access to their health records is
now common in many places (Tracyl et al., 2004)
(Pyper et al., 2004). How is access control going to
be modelled in all these cases?
In this article we aim to get a small glimpse of
what are the opinions of doctors working in HSJ
towards who should access Electronic Patient
Records, how should it be done and for whom this
information should be (or not) restricted.
2 METHODS
2.1 Type of Study
This is an observational, descriptive, transversal
study, in which the analysis unit is the individual.
2.2 Participants’ Selection
Initially, we performed a bibliographic search of
publications concerning access control to Electronic
Patient Records. The next step was the selection of
participants. Our target population was medical
doctors. The available representative population was
the medical doctors of the HSJ from a list available
from the department of human resources at HSJ.
From that list the medical doctors, department
directors and pre-career doctors were selected. As a
sampling method, from the filtered list, we selected
a simple randomized sample of 92 elements.
2.3 Data Collection
The instrument used for data collection was a
questionnaire with the characteristics of a structured
interview, which was absolutely anonymous. The
first steps in the questionnaire design were the
research of questionnaires previously tested and the
elaboration of a variable list.
The questionnaire was then pre-tested, in order
to evaluate its validity and reproducibility. The pre-
test’s participant selection was made by a non-
random accidental sampling process. The
interviewer asked 10 HSJ doctors, who were at the
hospital at that moment, to fill it in. Then, the final
version of the questionnaire was elaborated with the
pre-coded variables.
The questionnaire comprises 8 questions, some
of them subdivided (see Apendix). The first 2
questions are global questions where doctors
indicate the frequency they use the EPR and if there
should be several access levels to records depending
on the health professional’s category (a Yes or No
response).
Question 3 refers to doctors’ access
control and question 4 refers to the access to more
sensitive information about patients (like HIV tests).
Question 5 demanded doctors’ opinions about
nurses’ access to EPR. Questions 6, 7 and 8 describe
other situations such as emergency situations, other
uses of EPR and patient’s access to their EPR.
The independent variables potentially relevant
for the statistical analysis are: age, gender,
professional category and department. This
information was used to compare answers to the
different questions (dependent variables) between
these distinct groups in the statistical analysis.
The following step was the recruitment.
Different departments were visited in order to find
the doctors that were part of the sample. Those who
did not work in HSJ anymore (29 people) or were
already retired (5 doctors) were excluded, and the
sample was reduced to 58 people. Then, the
questionnaire was applied. If the doctors were not
available at their department after three attempts,
refused to answer the questionnaire or left it
incomplete, they were eliminated from the study.
2.4 Statistical Analysis
In what concerns statistical analysis, we used SPSS
to insert the collected data in a preformatted table
.
We started to analyse our sample using absolute
and relative frequency tables as well as pie graphs.
Chi-Square tests were also performed in order to
evaluate the significance of the differences found
between ages, genders, professional categories and
departments, regarding the most relevant questions.
As there are cases that do not respect the qui-square
test’s assumption (that require all expected values to
be equal or superior to 5), some values are
calculated using Fisher’s exact test.
All the independent variables used in this study
are categorical variables, except the age. In order to
facilitate the data analysis, we transformed this
numerical variable in a categorical one.
WHO SHOULD ACCESS ELECTRONIC PATIENT RECORDS
183
Furthermore, some independent variables were
attached in categories so that we could perform a
chi-square test. The variable age was separated in
two categories: under 35 and over 35. We chose 35
as the dividing age because most doctors become
specialists at that age. Professional categories were
also divided in two categories: pre-career doctors
and medical doctors. Departments were categorized
in medical departments or medical – surgical. The
significance level used in this study was 0.05.
3 RESULTS
Of the 58 applied questionnaires, 45 were fully
answered, so the response rate was 78%. 10 doctors
were not available in the department for three
consecutive times and 3 refused to answer.
Participants’ characteristics are listed in Table 1.
Most doctors were over 35 years old and there were
more female doctors than male doctors.
Table 1: Respondents’ demographics (N=45).
Age <35
>35
22%
78%
Gender Male
Female
58%
42%
Department Chirurgic
Medical
38%
62%
Professional
Category
General Intern
Specialist Intern
Specialist
Graduated Specialist
Service Director
7%
9%
38%
36%
11%
All doctors confirmed that they have already
used EPR. Most of them said that they use this kind
of records daily and that they agree with the
existence of different access levels of information
depending on the healthcare professional’s category.
93% (3) of the doctors said they agree and 7% (42)
answered they do not agree or have no opinion
regarding this issue.
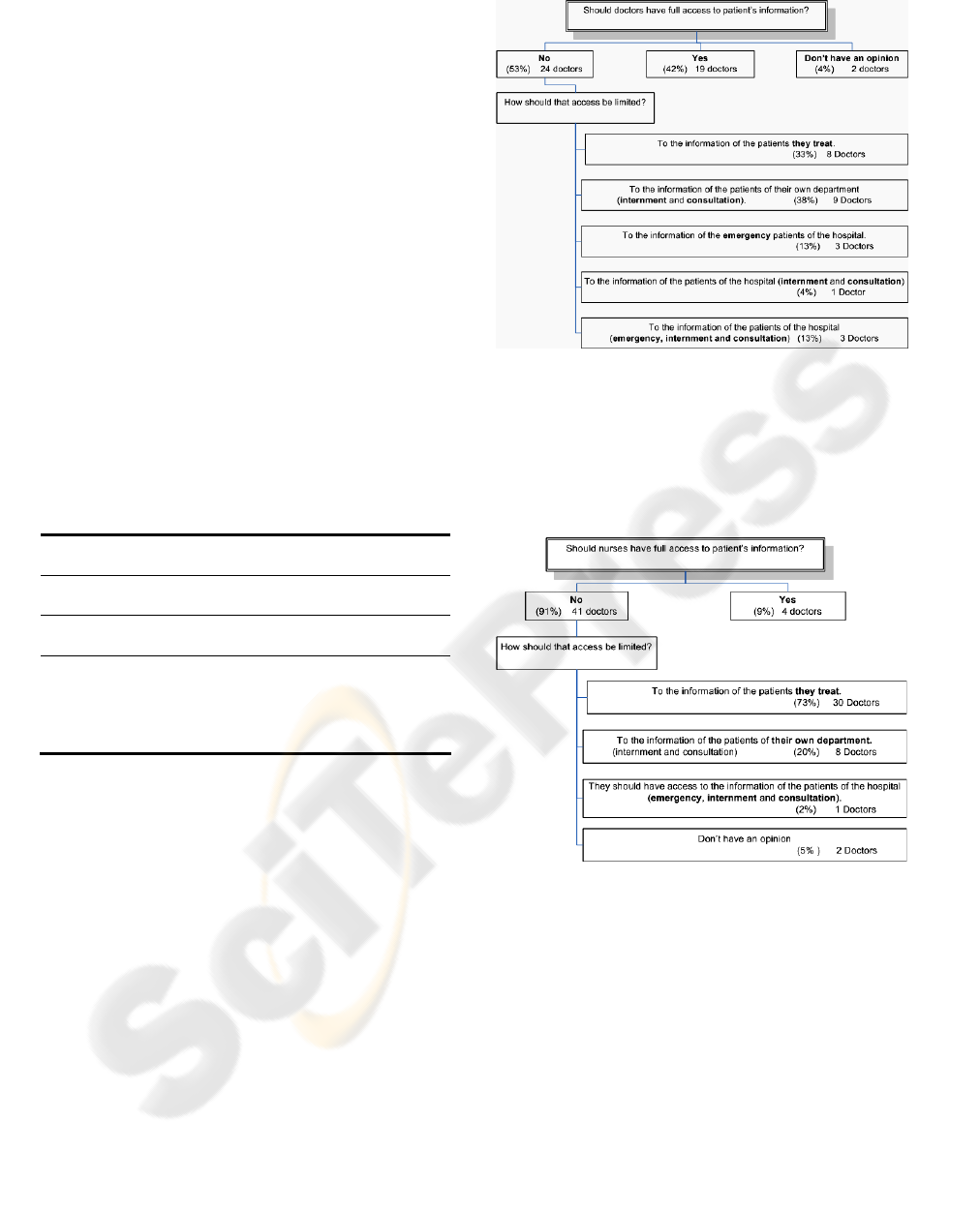
In what concerns doctors’ access to information,
the answers are summarized in Figure 1. More than
a half of the respondents thought that doctors should
not have full access to patients’ information. While
some thought that doctors should only have access
to the information of the patients they treat, others
considered that they should have access to all the
information of their department.
Further, 31 (69%) respondents thought that
sensitive information such as HIV tests, venereal or
cancer diseases should only be accessed by doctors
who treat those patients.
Figure 1: Answers for doctors’ access to a full EPR.
In what concerns nurses (Figure 2), a vast
majority of doctors (41 - 91%) thought that they
should not have full access to patients’ information.
The majority believe that nurses should only have
access to the information of the patients they treat.
Figure 2: Answers for nurses’ access to a full EPR.
Most doctors also agreed that, in emergency
situations, non authorized doctors and nurses must
have access to patients’ information, but that access
must be registered and controlled (Ferreira et al.,
2006). The majority of respondents found pertinent
to use the patients’ records to other purposes such as
clinical or epidemiologic investigation.
Regarding now patients, most doctors thought
that patients should not have full access to their
clinical information, 69% (31) thought that they
should not be able to access it while 31% (14) said
that they should.
HEALTHINF 2008 - International Conference on Health Informatics
184

4 CONCLUSIONS
From these results we can see that EPR are intensely
used by doctors. We can also discuss that doctors are
mostly concerned with situations regarding sensitive
information (e.g. HIV tests), and patients’ access to
these type of records. This is why they see access
control as an essential part of the EPR.
Also, doctors do not agree with the fact that
patients should be able to access the whole of their
healthcare record, thinking probably some of the
notes they make should be for they own use only.
This opinion is also demonstrated in another study
where they seem to be worried about the information
accessed by their patients.
Further, doctors were reluctant in what concerns
nurses’ access to patients’ information. They think
they should only access the information of the
patients they treat. This can be problematic as nurses
spend more time dealing and treating patients than
the doctors themselves and may need all the
information about the patient relating to other types
of treatment they can had been undergoing. It should
be noted that all doctors had an opinion regarding
this matter.
Our study also shows a tendency between some
variables. It is interesting to note that, within the 4
doctors who think that nurses should have total
access to information, 3 were male doctors and 3
were specialists.
Finally, doctors’ attitudes towards the use of
information for other purposes such as research were
mostly positive. They also vastly agreed with the
existence of different levels of access to EPR.
In conclusion, these results show that it is very
hard to get to a consensual policy regarding access
control to EPR by its regular users.
There is therefore the need for a
multidisciplinary agreement that can include
healthcare professionals’ experiences and needs in
order to define the most appropriate and efficient
way to perform access control to the EPR. Several
issues concerning the type of information, location,
type of user and other situations (e.g. emergency or
other unanticipated) may influence the way access
control should be made.
We believe that this is a very important issue to
be pursued and further studied. There is the need to
evaluate more healthcare professionals and patients’
attitudes and needs in order to define a better way to
perform access control to EPR (Ferreira, Cruz-
Correia et al., 2006).
ACKNOWLEDGEMENTS
We would like to thank class 8 of the 1
st
year
medical students from the 2005/2006 academic year
at the Biostatistics and Medical Informatics
Department of the Faculty of Medicine of Porto for
their work and enthusiasm in the development of
this project.
REFERENCES
Ab, B., Addabit, B.V., 2004. Access to EHR and access
control at a moment in the past: a discussion of the
need and an exploration of the consequences.
International Journal of Medical Informatics, 73, 267-
270.
Blobel, B., 2004. Authorisation and access control for
electronic health record systems. International Journal of
Medical Informatics, 73(3): 251-257.
Day, J., 2001. Privacy and Personal Health Data in
Cyberspace: the Role and Responsibility of Healthcare
Professionals. The journal of contemporary Dental
Practice, 2(1).
Ferreira, A, Cruz-Correia, R., Antunes, L., Chadwick,
D.W., 2007. Access Control: how can it improve
patients' healthcare? Studies in Health Technology and
Informatics. IOS Press, 127:65-76.
Ferreira, A., Correia, R., Antunes, L., Palhares, E.,
Farinha, P., Costa-Pereira, A., 2005. How to start
moddeling Access Control in a Healthcare
Organization. Proceedings of the 10th International
Symposium on Health Information Management
Research.
Ferreira, A., Cruz-Correia, R., Antunes, L., Farinha, P.,
Oliveira-Palhares, E., Chadwick, D. W., Costa-Pereira,
A., 2006. How to break access control in a controlled
manner? Proceedings of the 19th IEEE Symposium on
Computer-Based Medical Systems, 847-851.
Gritzalis, D., 1997. A Baseline Security Policy for
Distributed Healthcare Information Systems. Computers
and security, 16(8):709-719.
Hassol, A., Walker, J., Kidder, D., Rokita, K., Young, D.,
Pierdon, S., Deitz, D., Kuck, S., Ortiz, E., 2004. Patient
Experiences and Attitudes About Access to Patient
Electronic Healthcare Record and Linked Web
Messaging. J Am Med Inform Assoc, 11, 505-513
Pyper, C., Amery, J., Watson, M., Crook, C., 2004.
Access to electronic health records in primary care- a
survey of patients’ views. Med Sci Monit,
10(11):SR17-22.
Rogerson, S., 2000. Electronic Patient Records.
IMIS, 10(5).
Tracyl, S., Dantas, C., Upshur, R., 2004. Feasibility of a
patient decision aid regarding disclosure of personal
health information: qualitative evaluation of the Health
Care. BMC Medical Informatics and Decision Making.
WHO SHOULD ACCESS ELECTRONIC PATIENT RECORDS
185
