
CHANGING PERSPECTIVES ON INFORMATICS?
A Comparison of Three National Electronic Health Records
Bettine Pluut
Utrecht School of Governance, Utrecht University, Bijlhouwerstraat 6, Utrecht, The Netherlands
Zenc consultancy, Alexanderstraat 18, The Hague, The Netherlands
Arre Zuurmond
Faculty of Technology, Policy and management, Technical University, Jaffalaan 5, Delft, The Netherlands
Zenc Consultancy, Alexanderstraat 18, The Hague, The Netherlands
Keywords: Electronic Health Records, Health informatics, Relational Responsibility, Doctor-patient relationship.
Abstract: Participatory approaches to health care are getting increasingly popular in Western countries. But are the
perspectives on informatics changing as well? Because not every patient (always) can or wants to actively
participate in his health care process, differentiation in medical encounters is needed. We use the term
‘relational responsibility’ to refer to a process in which doctor and patient are responsive to each other’s
norms, values and ideas, especially with respect to their role division. Health informatics can support or
restrict this differentiation by giving patients access to Electronic Health Records (EHRs) and/or converging
those records with Personal Health Records (consumer oriented informatics). When we look at the policies
on the national EHRs in Canada, Denmark, and The Netherlands we find that the orientation towards
informatics is still mainly provider-oriented. Even when policy makers emphasize the importance of patient
participation and are aware of the potential of health informatics in this context, they have not given priority
to translating this into the design of their EHR. This means that for the upcoming years EHRs will support
one traditional role division: the one in which the health care professional is in the lead and is the better-
informed party.
1 INTRODUCTION
There appears to be a worldwide trend towards the
development of Electronic Health Records (EHRs).
On all continents nationwide generic Electronic
Health Records are being introduced (see e.g.
EHTEL, 2008). In addition, there is a trend towards
health records that are more directed towards use by
patients – the so-called Personal Health Records
(Tang et al., 2006).
Electronic Health Records are not ‘just’ a
technical matter. On the contrary, they can be seen
as the ‘stabilization’ (Chia, 1996) of norms, values
and conceptions of ‘good health care’. Ideas of a
‘good’ division of roles between doctor and patient
are automated and thus stabilized in EHRs.
Analyzing the stabilization of such norms and
values in EHRs is timely because of the increasing
popularity of participatory approaches to health care
(Todres et al, 2007). An explanation for this
popularity is that patient participation is considered
‘ethical’ (see e.g. Stilgoe and Farook, 2008). Patients
tend to be more satisfied when they have an active
role in considering and deciding about possible
treatments. Sometimes this also leads to better health
results (Jahng et al., 2005). The second argument for
patient participation lies in the demographic and
labour market developments in many western
countries (see e.g., Commission of the European
Communities, 2000). Because of an ageing
population it is argued that a significant amount of
health care tasks need to be carried out by patients
and/or their family members (Van den Eerenbeemt
and Mulder, 2005).
Still patient participation can also be ‘unethical’.
For instance, patients can be emotionally and
mentally unable or unwilling to decide about their
treatments (Bensing et al., 2004). Moreover, the
extent to which patients appreciate an egalitarian
416
Pluut B. and Zuurmond A. (2009).
CHANGING PERSPECTIVES ON INFORMATICS? - A Comparison of Three National Electronic Health Records.
In Proceedings of the International Conference on Health Informatics, pages 416-420
DOI: 10.5220/0001431004160420
Copyright
c
SciTePress
relationship with a health care professional varies
from patient to patient and from context to context
(Bensing et al, 2004).
This implies that within every medical encounter
doctor and patient face the challenge of distributing
roles and responsibilities, depending on the specific
context. We use the term ‘Relational Responsibility’
to refer to a process by which doctor and patient are
responsive to each other’s ideas, norms and values
and thus try to create an optimal role division,
depending on the specific context of their
interactions (McNamee and Gergen, 1999). So for
instance, sometimes patient and doctor both agree to
a subject-object understanding of their relationship,
in which the patient has a passive role. At other
times, the patient will appreciate an active
participant in his health care situation. This asks of
the participants in doctor-patient communication to
be open to each other’s preferences. In this way a so-
called ‘soft’ self-other differentiation can emerge
(Hosking, 2007).
2 CHANGING INFORMATICS
So far we have emphasized the importance of
differentiation in doctor-patient relationships. The
next question is: Can developments in health care
informatics support relational responsibility in the
doctor-patient relationship? To answer this question
it is useful to distinguish between two forms of
health care informatics: consumer health informatics
(PHRs) and provider-oriented medical informatics
i
(EHRs) (Eysenbach, 2000).
Personal Health Records (PHRs) can be seen as a
form of consumer health informatics, because they
are designed to empower patients by giving patients
more access to health care information and in this
way bridging the knowledge gap between health
care professional (Eysenbach, 2000, Tang et al.,
2006). EHRs are manifold in appearance and
traditionally support the health care professional, or
its institution, to manage information about (not
from) patients.
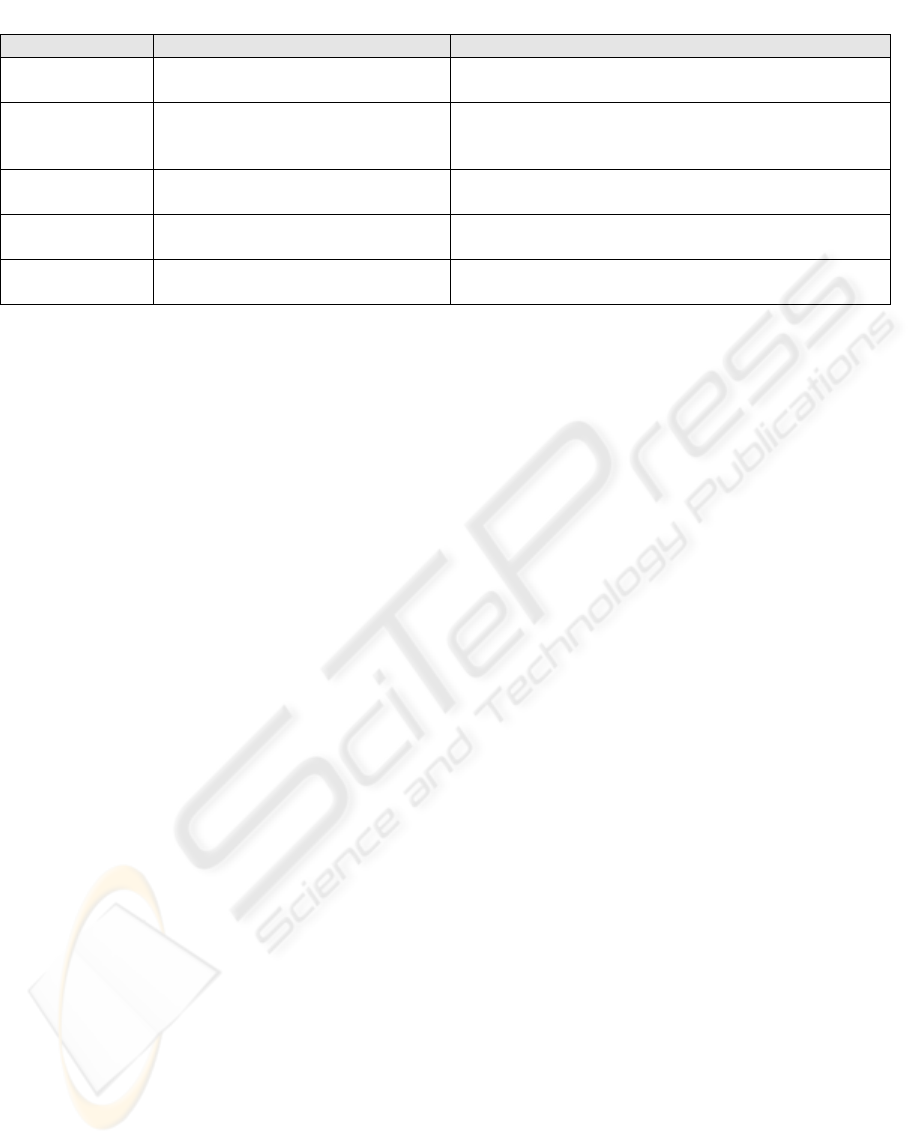
Table 1 shows the different development stages
of medical records
ii
. In more recent stages of
information technology the interoperability, i.e. the
degree in which it is possible to exchange
information, has increased significantly. This means
the fifth development stage, in which EHR and PHR
converge, has become technically possible. Due to
standardization and higher levels of interoperability,
both information written by the patient and
information written by the professional can be
exchanged
iii
. Such a convergence of EHR and PHR
would support relational responsibility because
patient and doctor can, depending on the particular
context of their communication, choose who adds
information to the health record, at what times this
information is read - and by whom.
Given this (theoretical) possibility of
convergence it is interesting to empirically study
whether countries are planning on realizing this
convergence and for what reasons. Do policy
makers acknowledge the need for differentiation in
doctor-patient relationships (relational
responsibility) and what is their perspective on
health informatics?
3 EMPIRICAL APPROACH
The empirical work concerns a qualitative,
explorative and comparative study, involving three
countries. For each country we studied:
- the institutional context: How is the EHR
implemented?
- EHR policy: What are the primary objectives of
the national EHR?
- functionalities of EHRs: What are the most im-
Table 1: development stages of EHRs and PHRs.
Stage Electronic Health records Personal health records
1. Computerizing Computerized records
Hand written notes; personal written annotations, personal
knowledge
2. Automating Automated systems
Manual entry into pc applications (word, excel, electronic
agenda). Stand-alone medical devices with computerized
records
3. Connecting
Digital organizational infrastructure
(e.g. hospital information systems)
Using medical devices and putting output of these devices
into journal / ehr-application
4. Networking Networked, distributed EHR
Automatic connections between devices and personal
EHR, synchronizing EHR with EPR by hand
5. Converging
Virtual, multidimensional records on
shared infrastructure
Automatic, multidirectional synchronization of PHR and
EHR
CHANGING PERSPECTIVES ON INFORMATICS? - A Comparison of Three National Electronic Health Records
417

portant design features of the EHR and who can
use them (professionals and/or patients)?
- data: What data are exchanged through the EHR
and are these created by professionals and/or
patients?
The answers to these questions are based on the
study of policy and implementation documents.
4 EHR POLICY & DESIGN
4.1 Countries & Institutional Contexts
We have chosen to study the policy and design of
EHRs in Canada, Denmark and The Netherlands,
because these countries are actively working on a
national, generic EHR, and because they have a high
penetration of pc and Internet use. After all,
convergence is difficult if only a few people use
Internet. All three countries are in the top ten of the
United Nations E-government Readiness Index
(United Nations, 2008).
In Canada each province is creating its own
EHR, which in time should become interoperable.
Denmark and The Netherlands are working on one
nation-wide, generic EHR.
All three countries have founded and/or
appointed an implementation organization. In
Canada the federally funded organization ‘Health
Infoway’ is mandated to accelerate the development
and adoption of EHR’s (Canada Health Infoway,
2005). Infoway tries to create the basic infrastructure
that makes it possible to connect EHR systems and
in addition tries to distribute successful EHR
practices nationwide. In Denmark ‘Medcom’ is
responsible for the creation of an interoperable ICT-
network and communication standards (Medcom,
2007). In The Netherlands the Ministry of Health,
Welfare and Sport has appointed ‘NICTIZ’, the
national ICT institute for health care. NICTIZ has
developed a national ICT infrastructure for the
health care sector (NICTIZ, 2005).
4.2 EHR Policy: Primary Objectives
The table below gives on overview of the primary
objectives that follow from EHR policy documents
iv
.
Canadian policy makers directly link the EHR to
patient involvement, participation, education
(empowerment) and self-care, which are considered
important objectives. Danish government also makes
a direct link between patient access to EHRs and
their ability to actively participate in their healthcare
process. In The Netherlands the formal EHR
objectives are all oriented towards supporting
providers in the delivery of health care. However,
NICTIZ states in its brochure that it sees the EHR as
a way to increase patient’s autonomy, to take work
off health care professionals’ shoulders and to
increase the level of responsibility and involvement
(NICTIZ, 2005).
4.3 Functionalities of EHRs
Documentation (registration of health information)
and collection (retrieval of health information) are
the first functionalities that all three countries hope
to realize. In addition to this, Canada hopes that in
2015 other functionalities like order entry, public
visibility into wait times, Clinical Information
Systems and chronic disease management will be
available (Canada Health Infoway, 2005). Denmark
connects the EHR to various telemedicine projects in
Table 2: EHR policy: objectives of EHRS.
Canada Denmark The Netherlands
- Increasing quality of care
- Timely access to accurate information and
improved decision-making support
- Enhancing ongoing disease management
and longer-term care
- A higher level of patient involvement and
education
1
- Enabling patient self care/remote care
- Controlling system risks from pandemics or
other health issues
- More guideline-compliant treatment
- Manage wait times and improve patient
access
- Enhanced performance management of cost,
quality and access
(Canada Health Infoway, 2005)
- Enable the individual citizen to have safe
access to personal health-related
information
- Increased efficiency
- Quality assurance of health care
delivery, e.g. by fewer errors in
medication
- Improved quality of clinical decision-
making
- Shorter waiting times
- Supporting the citizens freedom of
choice
(Ministry of the Interior and Health, 2003)
- Continuity and quality of care
- Decrease in number of avoidable
medication errors
- Increasing safety of patients
- Increase in the efficiency of health
care
- More demand-driven health care, i.e.
preventing patients from
unnecessarily having to tell the same
story over and over again
(Ministry of Health, Welfare and
Sport, CIBG and NICTIZ, 2005 and
2008; Website of Ministry, 2008)
HEALTHINF 2009 - International Conference on Health Informatics
418

which the local nurse can perform certain activities
that in the past only specialists were allowed to
perform. In this way patients can be treated closer to
home.
In both Canada and The Netherlands health care
professionals first gain access to the EHR. The
Dutch NICTIZ is exploring the possibility of giving
patients access to their record through a patient
portal, but in the first year(s) patient access is only
possible by a paper print of the EHR (NICTIZ,
2005). The same applies to Canada: a patient portal
with self-help tools and basic EHR information
should be in place around 2015 (Canada Health
Infoway, 2005). In Denmark there is already a
patient portal in use, which is linked to the EHR
infrastructure. At “sundhed.dk” patients can find a
directory of names and addresses, make
appointments, get prescription renewals, contact
their GP through e-mail, compare prices, quality and
accessibility of care, by drugs online, receive
information about prevention and treatment, view
information on waiting lists, preventive medicine,
health laws and regulations and access their own
personal health data, i.e. their EHR (Ministry of
Interior and Health, 2003).
4.4 Data that are Exchanged
All data that are exchanged by the EHR
infrastructure in the three countries are created and
provided by the community of health care
professionals. Patients do not have the possibility to
add health related information to their EHR.
Within the basic Canadian infrastructure data
that will be exchanged are: a) client and provider
registries; b) Public Health Surveillance data (PHS);
c) drug data; d) laboratory data and e) Diagnostic
Imaging (DI).
For the most important data products in
Denmark, almost all paper forms have been replaced
by electronic forms. Hospital information and
treatment plans are now sent electronically to
municipal care centers (62%)
1
. GP’s receive
discharge letters (88%) and send prescriptions
(83%). Laboratories send lab results to GP’s and
hospitals (96%), after receiving lab requests (75%).
Reimbursement is almost entirely done
electronically (96%).
The first version of the Dutch EHR exchanges
medication data and a GP’s summary file that is to
be used by the local GP. Within a couple of years
NICTIZ also hopes to realize an emergency record, a
diabetes record and it hopes to integrate laboratory
data (NICTIZ, 2005).
5 CONCLUSIONS
In the first part of this paper we concluded that
differentiation in medical encounters is needed.
There are important ethical and practical reasons for
patient participation, but sometimes a more
traditional role division, in which patients have a
more passive role, can be preferable. Depending on
the relational context, patient and doctor need to
look for an optimal role division. Health informatics
can support such Relational Responsibility in
doctor-patient relationships, given that increasing
interoperability makes convergence of EHRs and
PHRs technically possible.
We empirically explored what norms and values
with respect to the role division between doctors and
patients are being stabilized in nation-wide EHRs –
both in policy and design. When we look at Canada,
Denmark and The Netherlands we can first conclude
that policy makers all to a greater or lesser extent
emphasize the importance of patient participation.
Canada has the most extensive vision on the EHR as
a means of empowering patients and promoting self-
care. When we look at the ways in which the EHRs
are implemented, we must conclude that we can only
find few traces of these visions on patient
participation in the current designs of EHRs.
Denmark and The Netherlands are ahead in realizing
an infrastructure for the national exchange of
medical information between professionals. In
Denmark the possibility of patient participation is
most developed through a patient portal that enables
patients to access information written by
professionals. However, in none of the countries
patients can add medical information that is written
by themselves to the record.
In none of the policy visions we find an explicit
recognition of the need to facilitate a differentiation
of role division in doctor-patient relationships. In
addition, the integration of EHR and PHR is in no
policy document, although Canada does plan on
creating self-help tools for patients and the
implementation organization in The Netherlands
values the idea of patients adding information to the
EHR.
In sum, for the upcoming years Electronic Health
Records will mainly support one traditional role
division: the one in which the health care
professional is in the lead and is the better-informed
party. Although the perspective on the doctor-patient
relationship seems to be changing towards more
patient participation, the current use of informatics
still seems to be provider-oriented.
Future research could explore how these policies
CHANGING PERSPECTIVES ON INFORMATICS? - A Comparison of Three National Electronic Health Records
419

and designs of national EHRs work out in practice
and to what extent they restrict or support patient
participation.
REFERENCES
Bensing, J.M., Verhaak, P.F.M., Van Dulmen, A.M. and
Van den Brink-Muinen, A. (2004). Communication in
GP consultations. In: Van den Brink-Muinen, A., Van
Dulmen, A.M., Schellekens, F.G. and Bensing, J.M.
(eds.), Second national study into illnesses and
activities in the GP-practice, p. 14-35. Utrecht:
NIVEL.
Beun, J.G. (2003). Electronic Health Record: a way to
empower the patient. In: International Journal of
Medical Informatics, 69, p. 191-196.
Commission of the European Communities (2000). e-
Health - making healthcare better for European
citizens: An action plan for a European e-Health Area.
Brussels.
Canada Health Infoway (2005). Vision 2015: advancing
Canada’s next generation of health care.
Chia, R. (1996). The problem of reflexivity in or-
ganizational research. In: Organization, 3, 1, p.31-59.
EHTEL (2008). Sustainable Telemedicine: paradigms for
future-proof healtcare. Brussels: EHTEL.
Eysenbach, H. (2000). Consumer health informatics. In:
BMJ, 320, p.1713-16.
Hosking, D.M. (2007). Can constructionism be critical? In
J. Holstein & J. Gubrium (Eds.), Handbook of
Constructionist Research. New York: Guilford
Publications.
Jahng, K.H., Martin, L.R., Golin, C.E., DiMatteo. M.R.
(2005). Preferences for Medical Collaboration: Patient-
Physician Congruence and Its Associations with
Outcomes. In: Patient Education and Counseling, 57:
308-14.
McNamee, S., & Gergen, K.J. (Eds.). (1999). Relational
responsibility: resources for sustainable dialogue.
Thousands Oaks, California: Sage Publications.
Medcom (2003). Medcom IV: status, plans and projects.
Copenhagen: Medcom.
Medcom (2007). On the threshold of a healthcare IT
system for a new era. Copenhagen: Medcom.
Ministry of Health, Welfare and Sport (2005). ICT in
healthcare: from Electronic Medical Record to
Electronic Patient Record.
Ministry of Health, Welfare and Sport, CBIG, NICTIZ
(2005). Implementation of Electronic Medical Record
and Observation Record GP’s.
Ministry of Health, Welfare and Sport (2008).
Implementation Electronic Health Record.
Ministry of the interior and health (2002). Health care in
Denmark. Copenhagen: Ministry of the interior and
health.
Ministry of the interior and health (2003). National IT
strategy for health, 2003-2007. Copenhagen: Ministry
of the interior and health.
NICTIZ (2005). Corporate brochure. Leidschendam:
NICTIZ.
Stilgoe, F. and Farook, F. (2008). The talking cure: why
conversation is the future of healthcare. London:
Demos.
Tang, P.C., Ash, J.S., Bates, D.W., Overhage, J.M. and
Sands, D.Z. (2006). Personal Health Records:
Definitions, Benefits, and Strategies for Overcoming
Barriers to Adoption. In: Jamai, 13, p. 121–126.
Todres, L., Galvin, K. and Dahlberg, K. (2007).
Lifeworld-led healthcare: revisiting a humanising
philosophy that integrates emerging trends. In:
Medicine, Healthcare and Philosophy, 10, pp. 53–63.
United Nations (2008). United Nations e-Government
survey 2008. New York: United Nations.
Van den Eerenbeemt, F. and Mulder, B. (2004). Samen
zorgen voor jezelf (Taking care of yourself together).
Den Haag: De Informatiewerkplaats.
i
The word ‘provider’ refers to the health care professional.
ii
The development of EHRs is patchy. Thinking in terms of
configurations can therefore be useful, in which certain
aspects of an EHR still belong to one of the former stages,
whereas certain other aspects are already congruent with later
stages.
iii
The choice for exchange and use of information depends on
contextual factors such as quality, privacy and relevance.
iv
In Canada and Denmark one integrated vision document with
both long-term and short-term objectives have been written.
In The Netherlands we had to study different information
sources to create an overview of objectives as formulated in
formal documents.
HEALTHINF 2009 - International Conference on Health Informatics
420
