
USING A CLASSIFICATION SCHEME TO FACILITATE
OUTSOURCING OF RADIOLOGY SERVICES
Ulrik Schønnemann
MedWare
Blåbærvej 108, 5260 Odense S, Denmark
Uffe Kock Wiil
The Maersk Mc-Kinney Moller Institute, University of Southern Denmark
Campusvej 55, 5230 Odense M, Denmark
Keywords: Support for clinical decision-making, Knowledge management, Design and development of methodologies
for Healthcare IT, Classification scheme, Articulation work, Common information space.
Abstract: This paper deals with the issues involved in outsourcing radiology services. Based upon a field study of the
work practices at the radiology department at Svendborg Hospital in Denmark, a novel solution (including a
prototype of a computer supported reporting tool) that enables outsourcing of radiology services is
introduced. The solution is based upon development of a classification scheme of possible radiology
findings. Using predefined clinical findings for the radiology reports assure a high quality and enable
automatic translation of radiology reports.
1 INTRODUCTION
Many countries in Western Europe suffer from a
lack of radiologists, while some Eastern European
countries have available radiology resources.
According to the Danish National Board of Health
(www.sst.dk), Denmark had 102 unfilled radiology
positions in November 2007. Outsourcing of
radiology services is a potential solution to the
problem. However, important issues have to be
addressed before this solution becomes viable.
Outsourcing of radiology services demands a great
deal of trust to the providing organization. The
customer must trust that the provider delivers a
product which is at least as good as their own both
with regards to radiologic competence and linguistic
quality. The quality of the radiology service is
crucial, since patient treatment will be based upon
the radiologist’s report. The linguistic quality is an
issue when outsourcing, since a radiology report in
Denmark must be written in Danish. Having an
interpreter translate each report is very time
consuming and there are potential problems related
to decreased comprehensibility of the reports as well
as legal problems in case of mistreatment of a
patient due to a wrong translation of a correct
radiology report.
Based upon a field study of the work practices in
the radiology department at Svendborg Hospital in
Denmark, a novel solution (including a prototype of
a computer supported reporting tool) that enables
outsourcing of radiology services is introduced. The
solution is based upon development of a
classification scheme of possible radiology findings.
Using predefined clinical findings for the radiology
reports assure a high quality and enable automatic
translation of radiology reports.
2 FIELD STUDY AT SVENDBORG
HOSPITAL
The field study presents the current work practices
of the radiology department at Svendborg Hospital
in Denmark focusing on the lifecycle of an
examination.
149
Schønnemann U. and Kock Wiil U. (2009).
USING A CLASSIFICATION SCHEME TO FACILITATE OUTSOURCING OF RADIOLOGY SERVICES.
In Proceedings of the International Conference on Health Informatics, pages 149-154
DOI: 10.5220/0001510101490154
Copyright
c
SciTePress

2.1 The Radiology Department
An examination starts with a referral from either a
general practitioner or from another department
within the hospital. The referral contains the identity
of the patient and some text explaining what the
radiology department should investigate. The
referral is either received in paper or electronic form.
In both cases the referral is added to the Radiology
Information System (RIS), which is used for
governing the workflow around examinations within
the radiology department.
At a daily conference, the radiologists prioritize
the new examinations based on how crucial the
referral is and they decide which images to take. If a
patient complains about pain in the knee and the
general practitioner expects osteoarthritis, which is a
very slow progressing disease, the patient will
receive a low priority. On the other hand, if cancer is
expected, the patient will get a high priority. After
the examinations have been prioritized, a secretary
will send notification letters to the patients. Acute
patients are of course handled as fast as possible.
When the patient arrives at the department, a
secretary guides the patient to the relevant x-ray
room, where a radiographer takes the images
requested by the radiologists. Images are stored in
the Picture Archiving and Communication System
(PACS). The patient is done and leaves the
department again. The RIS is updated, enabling the
radiologists to see that the images have been taken.
A radiologist can now describe the images. If the
images contain findings that the radiologist is unsure
about, a second opinion from a colleague will be
requested. The description is entered into the RIS
and then electronically transmitted back to the
doctor who requested it in the first place.
2.2 The Radiologist
When describing an examination, the radiologist
typically follows a workflow that contains five steps:
(1) investigate the patient’s medical background, (2)
investigate what is requested to be examined, (3)
examine the images and create a mental diagnosis,
(4) report what is actually examined, and (5) report
what is found starting with most critical and finish
with a conclusion. Some of the steps (1, 2 and 4) in
the workflow can be omitted, but the quality of the
report will as a consequence be lowered. The
radiologist can obviously in some cases iterate back
and forth over the steps. The above approach of
reporting is problem oriented, meaning that the
radiologist searches for an answer to a specific
problem. This approach is optimal for swiftly
finding the source for the given problem, but there is
a risk that the radiologist will not discover secondary
findings.
When reporting, the radiologist compiles a more
or less complete mental overview of the diagnosis
before writing the report. Compilation of the mental
overview is based upon a search for findings in the
images and then concluding with a diagnosis. Thus,
the radiologist knows both the diagnosis and the
findings before the report is written.
2.3 Relevant Observations
A radiology department (fully digitalized or not)
with multiple collaborating actors requires
articulation work “to manage the distributed nature
of cooperative work” (Schmidt and Bannon 1992).
The cooperative work arrangement is supported by a
common information space (CIS) (Bannon and
Bødker 1997), which in this case encompass daily
conferences among actors and a powerful shared
artifact (the RIS). Bossen’s framework for analyzing
CIS is used to briefly characterize the CIS of the
radiology department through its parameters (Bossen
2002).
The CIS is characterized by being distributed
both in time and space – but mainly in time. There is
a high need for precision – primarily in the
descriptions made by the radiologists. There is a
high degree of common knowledge – the
descriptions are distributed among doctors who have
a very long identical education. The multiplicity of
the CIS is limited to speech and reading/writing and
the intensity is quite low due to the RIS. The
diversity of artifacts is low since it is mainly the RIS
which is used. Articulation work is also limited since
the department has very well defined work patterns.
There are three main states in the lifecycle of an
examination that requires articulation work:
prioritizing the examination, selecting the
radiographer, and selecting the radiologist. This
coordination of the actors is carried out in
conferences and is based on factors like: who is at
work, what are their qualifications, and are there
other tasks they must attend to.
There is one primary artifact used at the
radiology department (the RIS) which helps the
actors keep track of the progress of examinations
and provides the information at decentralized
locations. A radiographer does not have to leave the
x-ray room in order to know which patient is coming
and what image should be taken. The RIS also helps
to assure that patients’ data are not mixed up.
HEALTHINF 2009 - International Conference on Health Informatics
150

Finally, the RIS enforces a workflow that eases the
cooperation.
A radiology department also uses classification
schemes (Simone 2000) – some are formal and some
arises through daily practice. The most formal is
perhaps the classification of examination types,
which is a unified classification in Denmark. A less
formal classification scheme is the findings
described by the radiologists. A single radiologist
will tend to use standard terms and phrases for the
findings. The radiologists as a group will in time
develop a common set of terms and phrases. The
standardization helps the interpretation of the
descriptions. Currently, there exists no single
classification scheme for radiologic findings.
3 ISSUES IN OUTSOURCING
RADIOLOGY SERVICES
The above field study focus on the current work
practice where radiology services are handled in-
house. Outsourcing requires changes to the
cooperative work arrangement.
The articulation work will change significantly.
The management in a traditional radiology
department has to deal with quality of services,
coordination, motivation, and so on. In a department
which utilizes outsourcing, business also becomes an
important issue. The articulation work suddenly also
constitutes price determination, creation of business
relations, and negotiation with the providers.
The CIS is primarily affected in two ways. The
CIS will become distributed in space also, since part
of the workflow will be handled at a different
hospital. The CIS will also become multilingual,
since outsourcing is expected to take place in
different countries with different native languages.
The language issue changes the daily workflow.
Translation will introduce a new task. Both the
referrals and the reports must be translated.
One of the basic criteria that must be met in
order for outsourcing to be successful is that the
impact on the workflow when outsourcing should
not be much different from the impact of hiring
more radiologists. The achievement of that criterion
relies heavily on computer support and therefore
new artifacts. A number of new artifacts can be
introduced to minimize the overhead of outsourcing
radiology services:
Business relations. A new artifact can be
introduced enabling the management to set up
business relations with providers of radiology
services.
CIS distribution in space. A new artifact can
be introduced enabling the RIS to send images
and referrals to and receive reports from the
providers.
CIS language issues. A new artifact can be
introduced enabling automatic translation of
referrals and reports.
In the following, we will primarily focus on
addressing the language issues, which we believe is
by far the most complex of the issues involved in
outsourcing radiology services.
4 TOWARDS A SOLUTION
The approach taken aims at “expanding” the CIS
that currently encompass the work in the radiology
department at Svendborg Hospital to also include the
radiologists at the outsourced locations. More
precisely, we wish to develop a “common language”
shared by radiologists at Svendborg together with
radiologists at the outsourced locations. As
mentioned in the field study, a group of radiologists
that work together will over time develop a common
set of terms and phrases used for the description of
findings. This can be viewed as an informal
classification scheme.
The work to turn the informal classification
scheme into a formal one shared across distributed
locations involves radiologists at Svendborg
Hospital as well as East Tallinn Central Hospital in
Estonia. The work is based on the SNOMED CT
health care terminology and involves the Danish
National Board of Health. SNOMED CT is owned
and managed by the International Health
Terminology Standards Development Organization
(IHTSDO) (http://www.ihtsdo.org/). The novel
classification scheme of clinical findings is
organized as depicted in Figure 1.
Modality
Anatomic Region
Diagnosis
Finding
Figure 1: Classification of clinical findings.
USING A CLASSIFICATION SCHEME TO FACILITATE OUTSOURCING OF RADIOLOGY SERVICES
151
Modality is one of {x-ray, CT, MRI, US},
anatomic region is a part of the human body (i.e., a
knee), diagnosis is a suspected medical problem
(i.e., osteoarthritis) and a finding is supporting
medical evidence (i.e., subchondral sclerosis of the
medial femoral condyle).
Using predefined clinical findings for creating
the radiology reports, makes it possible to once and
for all translate the findings into multiple languages.
This solution has a number of benefits and allows
for a number of features that goes way beyond the
issues of language and translation that were the
initiating problems (see next section).
5 THE COMPUTER SUPPORTED
REPORTING TOOL
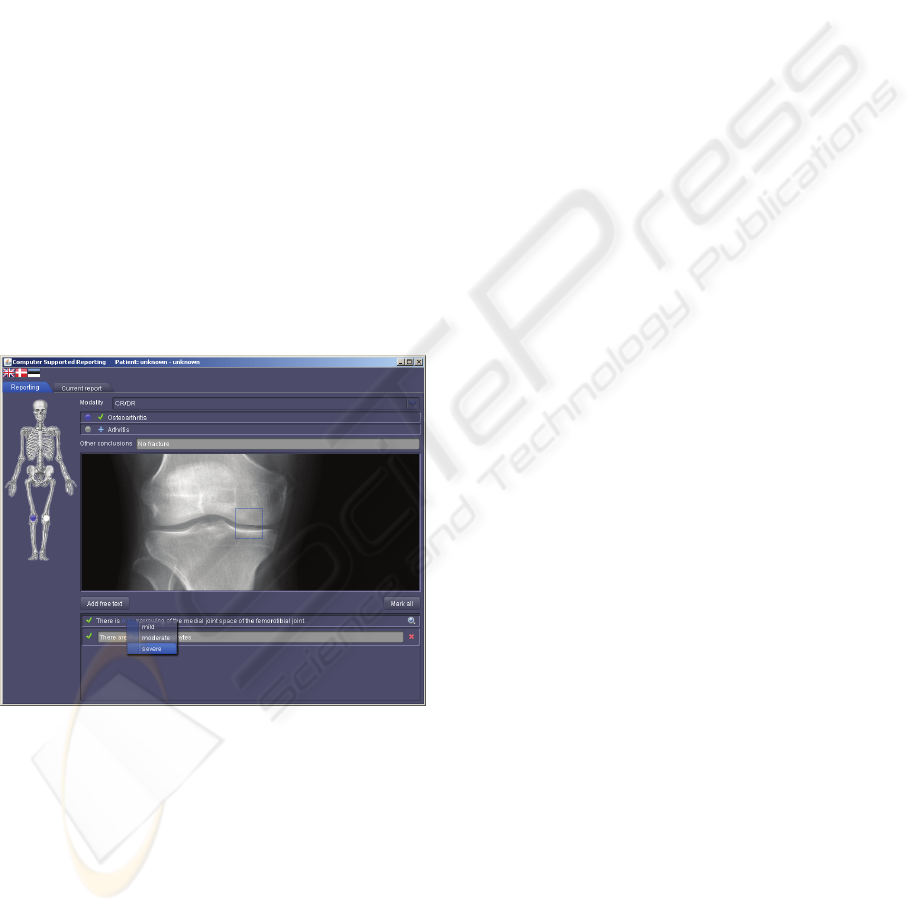
A prototype of a Computer Supported Reporting
(CSR) tool has been developed. CSR is a new
artifact in the CIS based on the novel classification
scheme of predefined clinical findings. CSR is
shown in Figure 2. The clinical finding on the screen
covers osteoarthritis in a knee.
Figure 2: The Computer Supported Reporting Tool.
The workflow for a radiologist using CSR
contains the following steps:
1. Select modality,
2. Select anatomic region,
3. Select diagnosis,
4. Add diagnosis to report conclusion, and
5. Add findings to report.
The modality and anatomical region will typically be
available from the RIS or PACS system. If they are
not, the radiologist will have to select them. As
described in the field study, the radiologist has a
mental overview of the diagnosis and the findings
that supports the diagnosis when writing the report.
Findings are typically related to a single diagnosis,
and it is therefore appropriate to have a tree structure
where the radiologist starts with selecting the desired
diagnosis and then the associated findings. If there
are enough indicators for the diagnosis, the
radiologist can choose to select this diagnosis for the
conclusion.
A diagnosis will typically have many associated
findings, which makes the list from which the
radiologist selects from very long. Therefore, CSR
provides a method for filtering the findings and a
method for compressing the findings.
1. Anatomic Filtering. For the selected
anatomic region an image of that region is
shown. Each finding is defined within an
area of that image. CSR enables the
radiologist to select an area of interest within
the shown image and thereby filter the
available findings to only those defined
within the area of interest.
2. Compressed Content. Some findings are
compressed into one statement where part of
the content is changeable, since some
findings are mutually exclusive, which
makes it appropriate only to be able to select
one of them; severity of the finding is an
example. Some findings can be found in
only two locations (A, B) which induces
three options (A, B, A and B). These options
can be made selectable instead of having
two separate findings.
The clinical findings supported by CSR can be
presented in different languages. The desired
language can be selected by clicking at an icon
depicting the nationality. Currently, Danish,
Estonian, and English are supported. Clinical
findings which are not currently predefined can be
typed in as free text. Such findings will naturally
have to be translated by an interpreter. However, the
solution supports that such findings can be assessed
later and added to the predefined set if eligible.
The use of a classification scheme for predefined
clinical findings combined with the features of the
CSR tool enables a number of advanced features:
Automated Translation between Languages. The
fact that each predefined clinical finding is translated
into numerous languages makes automated
translation of reports possible. Translation opens for
the possibility of cross border outsourcing of
radiology services. Foreign radiologists working at a
HEALTHINF 2009 - International Conference on Health Informatics
152

hospital can also benefit from automated translation
since they can report in their native language.
Clinical Guidance. CSR offers clinical guidance for
the radiologist. Each clinical finding is documented
by a reference image and some descriptive
background knowledge. The reference image aids
the radiologist in selecting the correct clinical
finding especially when the finding contains
severity.
Higher Comprehensibility of Reports. Reports
made with CSR will have a higher comprehensibility
than traditional reports due to the fact that linguistics
is independent of the radiologist who made the
report. A lot of effort is put into making good
descriptions and translations of the predefined
clinical findings. The receiver of a report can benefit
from the descriptive background knowledge for each
clinical finding in case of uncertainties.
Faster Reporting. Efficiency for the radiologists is
one of the primary objectives for CSR. The goal is to
have the radiologist use less time for reporting and
more time for using their radiologic knowledge.
Faster reporting is achieved by organizing the
clinical findings in a way which enables the
radiologist to rapidly find it.
Automated Translation to Patients. Countries
where patients are granted access to their own
medical records will suffer from the problem that
reports are almost impossible to understand due to
the difficult medical terminology. The automated
translation feature of CSR can remedy this by
translating the findings into an understandable
terminology.
Easy and Automatic Testing. CSR can assists in
testing radiologists. A group of experts describes a
number of examinations and thereby making the
“correct” answer for the test. When a radiologist has
described the examinations, the reports and the
correct answers are compared in an objective and
automated manner. The radiologist can either be
aware or unaware of the testing depending on the
purpose of the test.
6 SYSTEM OVERVIEW
The system architecture is optimized to support the
CSR tool, which is the central component used for
the actual reporting by the radiologists as described
in Section 5. The clinical content will continuously
be under development and undergo a lot changes.
The CSR tool will be used by numerous radiologists.
The overall architecture should insure efficient
updating of the clinical content. It is therefore
desirable to separate the clinical content and the
CSR tool as depicted in Figure 3.
Clinical
Content
Database
Clinical
Content
Server
Examination
Server
Administration
Tool
CSR
Tool
RIS
SOAP
HTML
Examination
Tool
HTML
Figure 3: The overall system architecture.
The clinical content is stored in the clinical
content database, which is accessible via the clinical
content server. The roles of the clinical content
server are to protect the database by validating the
data before it is stored in the database and to publish
an easy accessible SOAP interface for fetching the
clinical content. The clinical content server also
provides a web interface for the administration tool,
which is used to create and manage the clinical
content. The reports created with the CSR tool are
stored in the examination server, which in a real
world scenario needs to be connected to the RIS.
The examination tool is used by the local hospital to
manage users (radiologists) at the remote hospitals
and to add new tasks to be handled by the remote
hospitals. The examination tool is used by the
radiologist at the remote hospitals to login into the
system, to find their tasks, and to create radiology
reports (by opening and using the CSR tool).
Additional details about the CSR tool and the
overall system can be found in (Schønnemann
2008).
7 RELATED WORK
The presented work is inspired by previous work on
the structured reporting tool developed as part of the
Baltic eHealth project (www.baltic-ehealth.org).
Dixon and Fitzgerald (2008) discuss potential
benefits and risks of outsourcing radiology services.
They outline language, terminology, and accuracy
issues as risks. They propose that outsourced reports
should be in the same style as the usual reports from
the outsourcing hospital. CSR and the radiology
classification scheme handle these issues by
USING A CLASSIFICATION SCHEME TO FACILITATE OUTSOURCING OF RADIOLOGY SERVICES
153

introducing a common language used for radiology
reports.
Some hospitals already have experiences with
outsourcing of radiology services (i.e., Esbjerg
Hospital in Denmark (Rasmussen 2007)). They use a
Danish radiologist who was formerly employed at
Esbjerg Hospital. Therefore, they do not have to deal
with language, terminology, and accuracy issues.
To our knowledge, this work is the first attempt
to develop a classification scheme of radiology
findings with the degree of precision and structure
needed to allow computer tools to automatically
manipulate the clinical content.
8 CURRENT STATUS
The classification scheme currently only provides
clinical findings regarding one anatomical region
(the knee) and using one modality (x-ray). Future
work will focus on expanding the classification
scheme with additional modalities, anatomical
regions, and languages.
The CSR (with its limited clinical content added
using the administration tool) has been used in a test
scenario involving radiologists in Denmark and
Estonia. A senior radiologist at Svendborg Hospital
in Denmark provided images for the tests. The tasks
were added to the examination server using the
examination tool. The images were examined by a
senior radiologist and three medical students from
East Tallinn Central Hospital in Estonia using the
examination tool and the CSR tool.
The users found the system quite easy to use and
clinically relevant. They concluded that the system
could be useful to structure reporting methods inside
their own radiology department. More importantly,
they also concluded that the system would have even
more value for outsourcing radiology reports.
The users also commented on a few minor issues
relating to the layout of the features in the main
window of the CSR tool. These issues are relatively
easy to fix and did not hinder the use of the CSR
tool.
9 CONCLUSIONS
The primary contribution of this work is the
development of a classification scheme of clinical
findings and a set of tools for computer supported
reporting. Together, they provide a novel solution
allowing radiology services to be outsourced. We
have demonstrated that is it possible to introduce
classification into a limited medical domain and that
doing so enable automation of many tasks.
The tests of our solution were very promising
and encouraging. We envision that such systems for
outsourcing medical services will find their way into
hospitals within few years.
One could imagine that an internet based world
wide market place for outsourcing medical services
would appear some time in the future to fulfill the
needs of hospitals that find it difficult to recruit
certain medical specialist.
The approach of outsourcing medical services is
appealing compared to the alternative of enticing
medical specialist from less resourceful countries to
move to more resourceful countries. Such an
approach would, of course, eliminate the problems
in Denmark, but it would create new problems in
other less resourceful countries.
ACKNOWLEDGEMENTS
We wish to thank Dr. Leslie Christensen, Svendborg
Hospital, Denmark and Dr. Peeter Ross, East Tallinn
Central Hospital, Estonia for their collaboration and
participation in this project.
REFERENCES
Bannon, L., Bødker, S. 1997. Constructing Common
Information Spaces. In Proc. of ECSCW 1997.
Kluwer, pp. 81-96
Bossen, C. 2002. The Parameters of Common Information
Spaces: the Heterogeneity of Cooperative Work at a
Hospital Ward. In Proc. of CSCW 2002. (Nov., New
Orleans, LA). ACM Press, pp. 176-185.
Dixon, A. K., Fitzgerald, R. 2008. Outsourcing and
Teleradiology: Potential Benefits, Risks and Solutions
From a UK/European Perspective. Journal of the
American College of Radiology, 5, 1, 12-18.
Rasmussen, J. 2007. Barcelona hjælper sygehus
(Barcelona helps hospital). JydskeVestkysten (Danish
newspaper), November 29, 2007.
Schmidt, K., Bannon, L. 1992. Taking CSCW Seriously:
Supporting Articulation Work. Computer Supported
Cooperative Work, 1, 1-2, 7-40.
Schønnemann, U. 2008. IT Support of Radiology
Outsourcing. Master’s Thesis, The Maersk Mc-Kinney
Moller Institute, University of Southern Denmark.
Simone, C. 2000. Making Classification Schemes a first
class notion in CSCW. 1st CISCPH workshop on
Cooperative Organization of Common Information
Spaces. http://www.itu.dk/~schmidt/ciscph.html.
(Aug., Copenhagen, Denmark).
HEALTHINF 2009 - International Conference on Health Informatics
154
