
COMPARISON OF ANALYTIC APPROACHES FOR
DETERMINING VARIABLES
A Case Study in Predicting the Likelihood of Sepsis
Femida Gwadry-Sridhar, Benoit Lewden, Selam Mequanint
Lawson Health Research Institute, I-THINK Research Lab, London, ON, Canada
Michael Bauer
Department of Computer Science, University of Western Ontario, London, ON, Canada
Keywords: Sepsis, Decision support, Decision trees.
Abstract: Sepsis is a significant cause of mortality and morbidity and is often associated with increased hospital
resource utilization, prolonged intensive care unit (ICU) and hospital stay. The economic burden associated
with sepsis is severe. With advances in medicine, there are now aggressive goal oriented treatments that can
be used to help these patients. If we were able to predict which patients may be at risk for sepsis we could
start treatment early and potentially reduce the risk of mortality and morbidity. Analytic methods currently
used in clinical research to determine the risk of a patient developing sepsis may be further enhanced by
using multi-modal analytic methods that together could be used to provide greater precision. Researchers
commonly use univariate and multivariate regressions to develop predictive models. We hypothesized that
such models could be enhanced by using multi-modal analytic methods that together could be used to
provide greater precision. In this paper, we analyze data about patients with and without sepsis using a
decision tree approach. A comparison with a regression approach shows strong similarity among variables
identified, though not an exact match. We compare the variables identified by the different approaches and
draw conclusions about the respective predictive capabilities.
1 INTRODUCTION
Sepsis is defined as infection plus systematic
manifestations of infection (Dellinger et al., 2008).
Severe sepsis is considered present when sepsis co-
exists with sepsis-induced organ dysfunction or
tissue hypo-perfusion (Dellinger et al., 2008). Sepsis
can result in mortality and morbidity, especially
when associated with shock and/or organ
dysfunction (Angus et al., 2001). Sepsis can be
associated with increased hospital resource
utilization, prolonged intensive care unit (ICU) and
hospital stay, decreased long-term health related
quality of life and an economic burden estimated at
US $17 billion each year in the United States alone
(Brun-Buisson et al., 1995; Salvo et al, 1995; Pittet
et al., 1995; Angus et al., 2001). In Canada, there are
limited data on the burden of severe sepsis; however,
costs in Quebec may be as high as $73M per year
(Letarte, Longo, Pelletier, Nabonne & Fisher, 2002),
which contribute to estimates of total Canadian cost
of approximately $325 M per year.
Patients with severe sepsis generally receive their
care in the ICU. A multicentre study of sepsis in
teaching hospitals found that severe sepsis or septic
shock is present or develops in 15% of ICU patients
(Alberti et al., 2002). However, diagnosing sepsis is
difficult because there is no “typical” presentation
despite published definitions for sepsis (American
College of Chest Physicians/Society of Critical Care
Medicine Consensus Conference 1992; Levy et al.,
2003).
In the Canadian Sepsis Treatment And Response
(STAR) registry (mix of teaching and community
hospitals across Canada), the total rate for severe
sepsis was 19.0%. Of these, 63% occurred after
hospitalization.
With advances in medicine there are now
aggressive goal oriented treatments that can be used
90
Gwadry-Sridhar F., Lewden B., Mequanint S. and Bauer M. (2009).
COMPARISON OF ANALYTIC APPROACHES FOR DETERMINING VARIABLES - A Case Study in Predicting the Likelihood of Sepsis .
In Proceedings of the International Conference on Health Informatics, pages 90-96
DOI: 10.5220/0001554100900096
Copyright
c
SciTePress

to help these patients (Rivers et al., 2001; Minneci,
Deans, Banks, Eichacker, & Natanson, 2004;
Bernard et al., 2001). If researchers were able to
predict which patients may be at risk for sepsis we
could start treatment early and potentially reduce the
risk of mortality and morbidity. Therefore, methods
that can be developed to help with the early
diagnosis of patients who either present with sepsis
or develop sepsis in hospital are needed.
A variety of analysis techniques can be used to
identify relationships among a set of measured
variables or quantities. We hypothesized that
analytic methods currently used in clinical research
to determine the risk of a patient developing sepsis
may be further enhanced by using multi-modal
analytic methods that together could be used to
provide greater precision. Researchers commonly
use univariate and multivariate regressions to gather
information about variables that are associated with
the dependent variable, which in this case is whether
the patient contracted sepsis or not. However,
sometimes these models are constrained as we either
use univariate analysis to guide our decision on
which variable to include or rely on the literature to
guide the variable selection. Earlier work had looked
at the use of regression techniques to develop a
linear predictive model or mortality and length of
stay, but not sepsis (Martin et al., 2008).
In this paper, we consider the use of decision tree
analysis and cluster analysis. Decision trees are
interesting since they provide a prescriptive
approach for arriving at a decision with an
associated probability. In contrast, cluster analysis
takes a holistic approach to partition the data into
similar but disjointed sets. We were interested in
using these approaches to identify the key variables
or variable sets that can be used to predict the
likelihood of sepsis or not having sepsis in patients.
2 DATA IN STUDY
We obtained data that was collected from 12
Canadian intensive care units that were
geographically distributed and included a mix of
medical and surgical patients (Martin et al., 2008).
Data were collected on all patients admitted to the
ICU who had an ICU stay greater than 24 hours or
who had severe sepsis at the time of ICU admission.
Patients who were not anticipated to obtain to
receive active treatment were excluded.
Hospitals collected a minimum data set on all
eligible patients admitted to the ICU. This included
demographic information and data about their
admission, source of admission, diagnosis, illness
severity, outcome and length of ICU and hospital
stay. Illness severity scores were calculated using
data obtained during the first 24 hours in the ICU
(Knaus, Draper, Wagner, & Zimmerman, 1985;
Knaus et al., 1991). All patients were subsequently
assessed on a daily basis for the presence of
infection and severe sepsis.
The management of severe sepsis requires
prompt treatment within the first six hours of
resuscitation (Dellinger et al., 2008b). Experts in
critical care agree that the literature supports early
goal-directed resuscitation which has been shown to
improve survival in patients presenting to
emergency rooms with septic shock (Dellinger et al.,
2008a).
2.1 Ethical Review, Funding and Data
Ownership
The study was approved by the University of
Western Ontario Research Ethics Board and the
need for informed consent was waived. Participating
institutions submitted the study to their review
process if local approval was required. All activities
were compliant with the privacy and confidentiality
practices of the participating institutions and the
Federal and Provincial governments of Canada. Eli
Lilly Canada provided a research grant to London
Health Sciences Centre to support trial coordination,
data collection, data management and data analysis.
The investigators and sites retained control and
responsibility for data collection, analysis and
interpretation. Data is owned by and resides with
London Health Sciences Centre.
3 DECISION TREE APPROACH
In data mining and machine learning, a decision tree
is a predictive model, that is, a mapping from
observations about an item to conclusions about its
target value. In these tree structures, leaves represent
classifications and branches represent conjunctions
of features that lead to those classifications. The
machine learning technique for inducing a decision
tree from data is called decision tree learning, or
(colloquially) decision trees.
A decision tree is made from a succession of
nodes, each splitting the dataset into branches.
Generally, the algorithm begins by treating the entire
dataset as a single large set and then proceeds to
recursively split the set. Three popular rules are
typically applied in the automatic creation of
COMPARISON OF ANALYTIC APPROACHES FOR DETERMINING VARIABLES - A Case Study in Predicting the
Likelihood of Sepsis
91

classification trees. The Gini rule splits off a single
group of as large a size as possible, whereas the
entropy and twoing rules find multiple groups
comprising as close to half the samples as possible.
The algorithms construct the tree from the “top”
down until some stopping criteria is met. In our
current approach, we have used the gain in entropy
in order to determine how to best create each node
of the tree.
3.1 Entropy
In order to define information gain precisely, we
used a measure commonly used in information
theory, called entropy, that characterizes the “purity”
(or, conversely, “impurity”) of an arbitrary
collection of examples. Generally, given a set S,
containing only positive and negative examples of
some target concept (a so-called two-class problem),
the entropy of set S relative to this simple, binary
classification is defined as:
Entropy(S) = - p
p
log
2
p
p
– p
n
log
2
p
n
(1)
where p
p
is the proportion of positive examples in S
and p
n
is the proportion of negative examples in S. In
all calculations involving entropy we define 0log0 to
be 0.
One interpretation of entropy from information
theory is that it specifies the minimum number of
bits of information needed to encode the
classification of an arbitrary member of S (i.e., a
member of S drawn at random with uniform
probability).
If the target attribute takes on c different values,
then the entropy of S relative to this c-wise
classification is defined as
(2)
where p
i
is the proportion of S belonging to class i.
Note that if the target attribute can take on c possible
values, the maximum possible entropy is log
2
c.
3.2 Information Gain
Given entropy as a measure of the impurity in a
collection of training examples, we can now define a
measure of the effectiveness of an attribute in
classifying the data. The measure we will use, called
information gain, is simply the expected reduction in
entropy caused by partitioning the examples
according to this attribute. More precisely, the
information gain, Gain (S, A) of an attribute A,
relative to a collection of examples S, is defined as
(3)
where Values(A) is the set of all possible values for
attribute A, and S
v
is the subset of S for which
attribute A has value v (i.e., S
v
= {s ∈ S | A(s) = v}).
Note the first term in the equation for Gain is just
the entropy of the original collection S and the
second term is the expected value of the entropy
after S is partitioned using attribute A. The expected
entropy described by this second term is simply the
sum of the entropies of each subset S
v
, weighted by
the fraction of examples |S
v
|/|S| that belong to S
v
.
Gain (S,A) is therefore the expected reduction in
entropy caused by knowing the value of attribute A.
Put another way, Gain(S,A) is the information
provided about the target attribute value, given the
value of some other attribute. The value of
Gain(S,A) is the number of bits saved when
encoding the target value of an arbitrary member of
S, by knowing the value of attribute A.
The process of selecting a new attribute and
partitioning the training examples is now repeated
for each non-terminal descendant node in the tree,
this time using only the training examples associated
with that node. Attributes that have been
incorporated higher in the tree are excluded, so that
any given attribute can appear at most once along
any path through the tree. This process continues for
each new leaf node until either of two conditions is
met:
1. Every attribute has already been included
along this path through the tree, or
2. The training examples associated with this
leaf node all have the same target attribute
value (i.e., their entropy is zero).
Some of the variables in the data set are
continuous variables, such as temperature. These
require a somewhat special approach. This is
accomplished by dynamically defining new discrete-
valued attributes that partition the continuous
attribute value into a discrete set of intervals. In
particular, for an attribute A that is continuous-
valued, the algorithm can dynamically create a new
Boolean attribute A
c
that is true if A < c and false
otherwise. The only question is how to select the
best value for the threshold c. This is done by
selecting values for the threshold based on the
existing values of the attribute A and computing the
HEALTHINF 2009 - International Conference on Health Informatics
92
gain. The threshold c that produces the greatest
information gain is then chosen.
4 COMPARISON
In this section we compare the results of the decision
tree analysis to the results obtained using regression
techniques. In particular, we were interested in
which variables were identified as key in
determining sepsis in the two approaches.
4.1 Regression Analysis
Previous work had focused on the analysis of the
data using regression techniques. From a
multivariate logistic regression a number of
variables emerged as significant in the model
(computed using SAS 8.2). The model was very
accurate in being able to classify patients not likely
to get sepsis (99%) and reasonably accurate at
predicting patients that were likely to get sepsis
(66%). The variables in the model are summarized
in Table 1.
As indicated, we were interested in exploring
whether a decision tree analysis technique could
provide additional or at least complementary insight
into the regression model.
4.2 Decision Tree Analysis
The decision tree analysis yielded 9 distinct paths
that led to a determination of sepsis with high
probability. The four most frequent of the variables
associated with sepsis are shaded in Table 2 along
with all variables that appeared in one of these 9
paths.
We tested the accuracy of the tree by randomly
removing 30 patients, for whom outcomes were
known, regenerating the tree and then tested the
accuracy of the tree in predicting whether those 30
patients would develop sepsis or not. Of the 30
patients, 6 had developed sepsis. Using the decision
tree to predict the likelihood of developing sepsis for
these 6 patients, the tree predicted that 5 would
develop sepsis with a likelihood of 100% and the 6
th
would develop sepsis with a likelihood of 97%. Of
the 24 patients that did not develop sepsis, the tree
predicted their likelihood with values between 0%
and 1.7%, i.e., that it was very unlikely that these
patients would develop sepsis. Essentially, the
decision tree correctly predicted all 30 of the
patients.
Table 1: Logistic Regression Model.
Variables P value Exp(B)
Anaerobea culture
.122 .317
Abdominal diagnosis
.000 15.027
Blood diagnosis
.000 3.574
Lung diagnosis
.000 10.360
Other diagnosis
.000 8.492
Urine diagnosis
.000 7.280
Chest X-ray and purulent
sputum
.000 2.756
Gram negative culture
.047 .679
Gram positive culture
.001 .533
Heart rate >90bpm
.000 16.933
No culture growth
.000 .103
PaO2/FiO2 <250
.000 12.305
pH <7.30 or lactate >1.5
upper normal with base
deficit >5
.141 1.242
Platelets <80 or 50%
decrease in past 3 days
.000 5.665
Respiratory rate >19,
PaCO2 <32 or Mechanical
ventilation
.000 8.866
SBP <90 or MAP <70 or
Pressure for one hr
.000 9.963
Abdominal culture
.259 1.872
Blood culture
.000 2.311
Lung culture
.724 .932
Other site culture
.614 .869
Urine culture
.100 1.450
Temperature <36 or >38
.000 8.246
Urinary output <0.5
mL/kg/hr
.000 3.166
WBC > 12 or <4 or >10%
bands
.000 6.281
Yeast culture
.011 .492
Constant
.000 .000
Details on the variables and their decision points
in paths 1, 3, 4 and 9 are provided in Tables 3-6. The
variables which appear in these 9 paths of the
decision tree are highlighted in the Table 1 of the
regression model.
COMPARISON OF ANALYTIC APPROACHES FOR DETERMINING VARIABLES - A Case Study in Predicting the
Likelihood of Sepsis
93

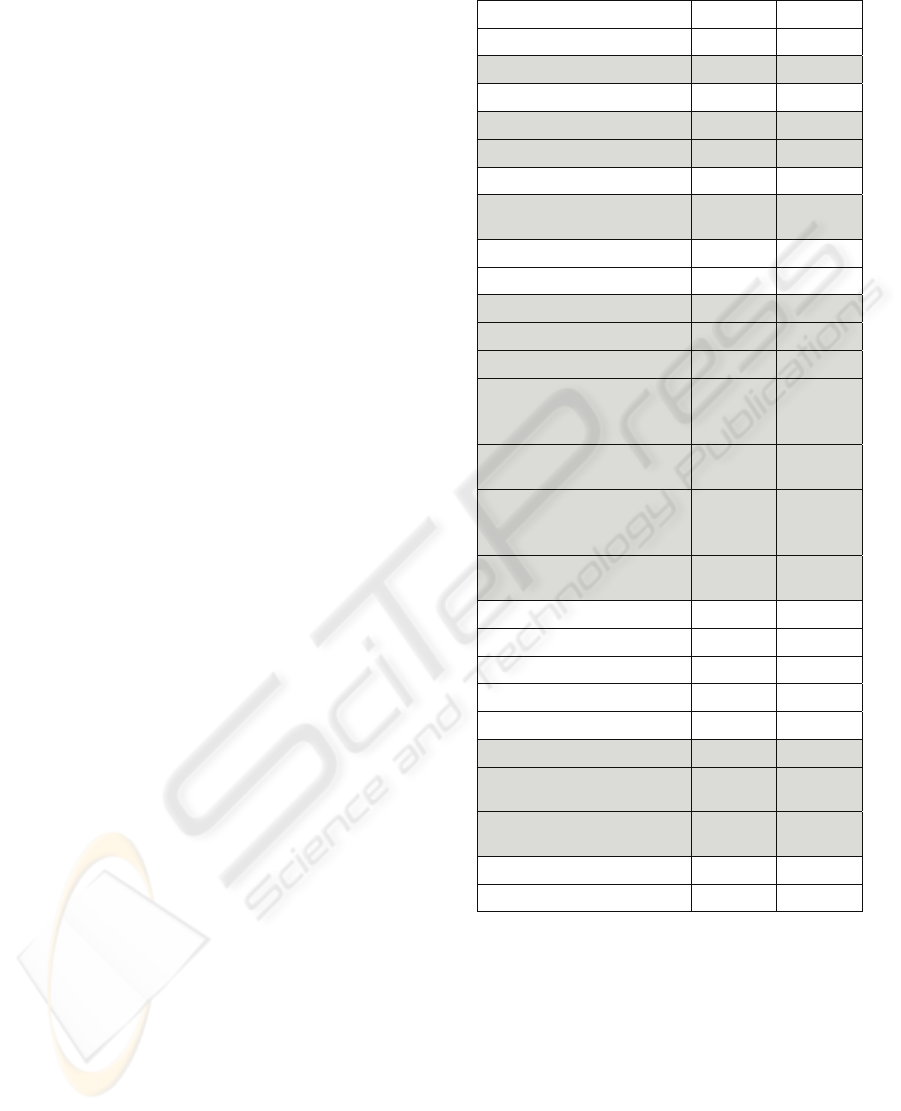
Table 2: Decision Tree Analysis.
Variables
Path1
Path2
Path3
Path4
Path5
Path6
Path7
Path8
Path9
Lung diagnosis √ √ √ √ √ √
Chest X-ray and purulent sputum √
Temperature <36 or >38 √ √ √ √ √ √ √
WBC > 12 or <4 or >10% bands √ √ √ √
No culture growth √ √ √ √ √ √
Heart rate >90bpm √ √ √ √ √ √ √ √ √
SBP <90 or MAP < 70 or pressors for one hour √ √ √ √ √ √ √ √ √
PaO2/FiO2 <250 √ √ √ √
Urinary output <0.5 mL/kg/hr √ √
pH <7.30 or lactate >1.5 upper normal with base
deficit >5
√ √
Respiratory rate >19, PaCO2 <32 or Mechanical
ventilation
√
√ √
Other diagnosis √ √
Abdominal diagnosis √ √ √
Platelets <80 or 50% decrease in past 3 days √ √
Note: Underlined check marks are for ‘Yes’
Table 3: Decision Tree Analysis Path-1.
Variables in the path
Platelets <80 or 50% decrease in past 3 days Yes
pH <7.30 or lactate >1.5 upper normal with base
deficit >5
No
Urinary output <0.5 mL/kg/hr No
SBP <90 or MAP < 70 or pressors for one hour No
PaO2/FiO2 <250 No
WBC > 12 or <4 or >10% bands Yes
Temperature <36 or >38 Yes
Heart rate >90bpm No
Table 4: Decision Tree Analysis Path-3.
Variables in the path
Temperature <36 or >38 Yes
Chest X-ray and purulent sputum Yes
No culture growth Yes
Lung diagnosis No
PaO2/FiO2 <250 Yes
SBP <90 or MAP < 70 or pressors for one hour No
Heart rate >90bpm Yes
Table 5: Decision Tree Analysis Path-4.
Variables in the path
Temperature <36 or >38 No
WBC > 12 or <4 or >10% bands Yes
Lung diagnosis Yes
PaO2/FiO2 <250 Yes
SBP <90 or MAP < 70 or pressors for one hour No
Heart rate >90bpm Yes
Table 6: Decision Tree Analysis Path-9.
Variables in the path
Respiratory rate >19, PaCO2 <32 or Mechanical
ventilation
Yes
WBC > 12 or <4 or >10% bands Yes
Lung diagnosis Yes
No culture growth Yes
SBP <90 or MAP < 70 or pressors for one hour Yes
Heart rate >90bpm Yes
5 DISCUSSION
First, all variables appearing in the 9 paths also did
appear in the regression model. This provides good
support for both the regression model and decision
tree result. Interestingly, urine diagnosis had
HEALTHINF 2009 - International Conference on Health Informatics
94

relatively high beta coefficient in the regression, but
did not appear in any of these paths of the decision
tree. However, other variables with higher beta
coefficients in the regression, such as abdominal
diagnosis, lung diagnosis, SBP and temperature,
were also important in the tree.
This has implications for practice since clinicians
want to apply models of risk at the bedside. Often it
is not feasible to collect data on 20 variables, such as
those we found in the regression or cluster and
models that are easy to use to either rule out patients
who are not at risk of sepsis or those who are at risk
would be more useful. To test any model we have to
ensure that it is reliable and valid. Here we have
shown with the 30 patient accuracy test that our tree
is reliable and it approaches 100% validity. Our
analysis also illustrates the value of multiple
methods: 1) in our analysis, regressions can be used
to provide a broad estimate of risk, and 2) a more
precise estimate in this case can be made using a
decision tree. In a separate paper, we will compare a
cluster analysis approach to a decision tree. This is
outside the scope of this paper. A valid approach for
future research is the comparison of cluster analysis,
decision trees and regression analysis.
6 CONCLUSIONS
Multiple methods of analysing clinical data provide
different perspectives on models of risk of disease.
To develop robust models researchers may want to
consider regression to get a broad perspective on the
risk and utilize decision trees to provide more
parsimonious models.
This study has several strengths. This was a
prospective observational cohort and the
determination of sepsis used standard criteria. The
large sample size provided a large number of
variables that we could use for our analyses.
Future research will now entail testing the
decision tree paths in practice to determine which
path is most reliable and valid as well as completing
a more in depth measure of the accuracy of the
regression and decision tree models. We did not
have an opportunity to test other methods such as
cluster analysis, Bayesian methods or neural
networks, which we hope to do in the future.
ACKNOWLEDGEMENTS
We would like to thank Corey Hilliard for assisting
with manuscript preparation.
REFERENCES
American College of Chest Physicians/Society of Critical
Care Medicine Consensus Conference: definitions for
sepsis and organ failure and guidelines for the use of
innovative therapies in sepsis. (1992). Crit Care Med,
20, 864-874.
Alberti, C., Brun-Buisson, C., Burchardi, H., Martin, C.,
Goodman, S., Artigas, A. Sicignano, A., Palazzo, M.,
Moreno, R., Boulme, R., Lepage, E., & Le Gall, R.,
(2002). Epidemiology of sepsis and infection in ICU
patients from an international multicentre cohort study.
Intensive Care Med, 28, 108-121.
Angus, D.C., Linde-Zwirble, W.T., Lidicker, J., Clermont,
G., Carcillo, J., & Pinsky, M.R. (2001). Epidemiology
of severe sepsis in the United States: analysis of
incidence, outcome, and associated costs of care. Crit
Care Med, 29, 1303-1310.
Bernard, G.R., Vincent, J.L., Laterre, P.F., LaRosa, S.P.,
Dhainaut, J.F., Lopez-Rodriguez, A. Steingrub, J.S.,
Garber, G.E., Helterbrand, J.D., Ely, E.W. & Fisher,
C.J.Jr. (2001). Efficacy and safety of recombinant
human activated protein C for severe sepsis. N Engl J
Med, 344, 699-709.
Brun-Buisson, C., Doyon, F., Carlet, J., Dellamonica, P.,
Gouin, F., Lepoutre, A. Mercier, J.C., Offenstadt, G.
& Regnier, B. (1995). Incidence, risk factors, and
outcome of severe sepsis and septic shock in adults. A
multicenter prospective study in intensive care units.
French ICU Group for Severe Sepsis. JAMA, 274,
968-974.
Dellinger, R.P., Levy, M.M., Carlet, J.M., Bion, J., Parker,
M.M., Jaeschke, R., Reinhart, K., Angus, D.C., Brun-
Buisson, C., Beale, R., Calandra,T., Dhainaut, J.F.,
Gerlach, H., Harvey, M., Marini, J. J., Marshall, J.,
Ranieri, M., Ramsay, G., Sevransky, J., Thompson,
B.T., Townsend, S., Vender, J.S., Zimmerman, J.L. &
Vincent, J. L. (2008). Surviving Sepsis Campaign:
international guidelines for management of severe
sepsis and septic shock: 2008. Crit Care Med, 36, 296-
327.
Knaus, W.A., Draper, E.A., Wagner, D.P., & Zimmerman,
J.E. (1985). APACHE II: a severity of disease
classification system. Crit Care Med, 13, 818-829.
Knaus, W. A., Wagner, D. P., Draper, E. A., Zimmerman,
J. E., Bergner, M., Bastos, P. G., Sirio, C.A., Murphy,
D.J., Lotring, T. & Damiano, A. (1991). The
APACHE III prognostic system. Risk prediction of
hospital mortality for critically ill hospitalized adults.
Chest, 100, 1619-1636.
Letarte, J., Longo, C. J., Pelletier, J., Nabonne, B., &
Fisher, H. N. (2002). Patient characteristics and costs
COMPARISON OF ANALYTIC APPROACHES FOR DETERMINING VARIABLES - A Case Study in Predicting the
Likelihood of Sepsis
95

of severe sepsis and septic shock in Quebec. J Crit
Care, 17, 39-49.
Levy, M. M., Fink, M. P., Marshall, J. C., Abraham, E.,
Angus, D., Cook, D. Cohen, J., Opal, S.M., Vincent,
J.L. & Ramsay, G (2003). 2001
SCCM/ESICM/ACCP/ATS/SIS International Sepsis
Definitions Conference. Crit Care Med, 31, 1250-
1256.
Martin, C., Priestap, F., Fisher, H. , Fowler R.A., Heyland,
D.K., Keenan, S.P., Longo, C.J., Morrison, T.,
Bentley, D. & Antman, N.(In Press)A prospective,
observational registry of patients with severe sepsis:
The Canadian Sepsis Treatment And Response
(STAR) Registry. Crit Care Med, (in press).
Minneci, P. C., Deans, K. J., Banks, S. M., Eichacker, P.
Q., & Natanson, C. (2004). Meta-analysis: the effect of
steroids on survival and shock during sepsis depends
on the dose. Ann Intern Med, 141, 47-56.
Pittet, D., Rangel-Frausto, S., Li, N., Tarara, D., Costigan,
M., Rempe, L., Jebson, P. & Wenzel, R.P. (1995).
Systemic inflammatory response syndrome, sepsis,
severe sepsis and septic shock: incidence, morbidities
and outcomes in surgical ICU patients. Intensive Care
Med, 21, 302-309.
Rivers, E., Nguyen, B., Havstad, S., Ressler, J., Muzzin,
A., Knoblich, B., Peterson, E. & Tomlanovich, M.
(2001). Early goal-directed therapy in the treatment of
severe sepsis and septic shock. N Engl J Med, 345,
1368-1377.
Salvo, I., de, C. W., Musicco, M., Langer, M., Piadena, R.,
Wolfler, A., Montani, C. & Magni, E. (1995). The
Italian SEPSIS study: preliminary results on the
incidence and evolution of SIRS, sepsis, severe sepsis
and septic shock. Intensive Care Med, 21 Suppl 2,
S244-S249.
HEALTHINF 2009 - International Conference on Health Informatics
96
