
SPOKEN LANGUAGE INPUT FOR A PATIENT NOTE SYSTEM
Sasha Caskey*, Kathleen McKeown*, Desmond Jordan† and Julia Hirschberg*
*Department of Computer Science, Columbia University, New York, NY 10027 U.S.A.
†Departments of Anesthesiology and Medical Informatics, Columbia University College of Physicians and Surgeons
New York, NY 10032 U.S.A.
Keywords: Speech recognition, Mobile devices, Electronic medical records, Natural language processing.
Abstract: In developing a system to help CTICU physicians write patient notes, we hypothesized that a spoken
language interface for entering observations after physical examination would be more convenient for a
physician than a more traditional menu-based system. We developed a prototype spoken language interface,
allowing input of one type of information, with which we could experiment with factors impacting use of
speech. In this paper, we report on a sequence of experiments where we asked physicians to use different
interfaces, testing how such a system could be used as part of their workflow as well as its accuracy in
different locations, with different levels of domain information. Our study shows that we can significantly
improve accuracy with integration of patient specific and high coverage domain grammars.
1 INTRODUCTION
Our long term goal is the development of a system
to help physicians create progress notes for patients
in the Cardio-Thoracic Intensive Care Unit
(CTICU). In the CTICU, a physician writes one to
two notes daily recording objective and subjective
findings for each of the approximately 28 patients
under their care. When tending to a patient, a
physician reviews the notes written by other
physicians and thus, note writing is an important
form of communication between physicians caring
for the same patient, increasing continuity of care.
At the same time, note writing is a time consuming
process and takes away from time spent on patient
care.
We are developing I
3
(Intelligent, Interactive,
Multimodal Information Ecosystem for Healthcare),
an interactive system that will reduce the time it
takes to generate progress notes. I
3
will draw
relevant information from the voluminous patient
record where appropriate, will generate inferences
from raw patient data identifying clinical problems
and highlighting acute medical care issues, and will
generate a skeletal note. Some information from the
note is not available in the online patient record,
however, and can only be provided by the physician
based on physical observations during rounds. We
hypothesize that a mobile, spoken language interface
would make it easy for a physician to enter
information about a patient at the point at which they
have available time, regardless of where they were.
We note that physicians have ready access to cell
phones, which could provide an easy-to-use method
for calling in information.
There are many unresolved issues, about the
feasibility of using a spoken language interface
within the hospital setting. Is there a point in time at
which physicians could naturally incorporate a
phone call into their workflow? Does the noisy
environment of the CTICU make it too difficult to
obtain acceptable accuracy for spoken language
input? While speech has been successfully used in
medical domains before (see Wang et. al. 99 and
Owens 05), the CTICU is a more difficult
environment. Domain-specific, telephony-based,
spoken language interfaces have proven useful when
the range of spoken inputs in response to a prompt is
sufficiently limited by the domain; spoken language
interfaces have gained in commercial use in car
direction systems, in airline reservation systems, and
in directory and weather information systems (Zue
et. al 00). Can we use the constraints of the medical
domain to adequately restrict expectations for input,
increasing accuracy? Finally, even if we can encode
sufficient domain restrictions on expected responses
to prompts, will physicians provide only the
323
Caskey S., McKeown K., Jordan D. and Hirschberg J. (2009).
SPOKEN LANGUAGE INPUT FOR A PATIENT NOTE SYSTEM.
In Proceedings of the International Conference on Health Informatics, pages 323-328
DOI: 10.5220/0001554603230328
Copyright
c
SciTePress

information requested, or will their utterances be
lengthier than required, straying off topic?
In order to investigate these issues, we developed
a prototype telephony-based spoken language dialog
system. To determine when, where, and how to elicit
restricted responses, we deliberately focused our
system to gather one type of information, the
identification of a patient problem, and
experimented with factors that would impact its use.
In this paper, we describe preliminary studies, the
system we developed, and our evaluation to assess
the feasibility of using spoken language to gather
input. Our studies show that we can significantly
improve recognition accuracy using a dialog system
that integrates patient-specific grammars with high
domain coverage. Our user study shows physician
satisfaction with a dialog strategy giving them
control over how information is entered.
2 PRELIMINARY STUDIES
Before developing the spoken language system we
describe here, we carried out several preliminary
studies and user interviews to try to understand how
the system would best fit within physician workflow
and how physicians would interact with such a
system.
We hypothesized that the best time to gather
information based on patient observations would be
during formal medical rounds. At this time most of
the content for note creation is readily available. We
used an off-the-shelf commercial recognizer from
ScanSoft, allowing the physicians to say whatever
they wanted during rounds. While this should have
worked well to obtain note content, we found that
having to record their observations while teaching
residents was too much of a cognitive load, rounds
took twice as long as usual, and accuracy was very
poor, as input was given during conversation with
interruptions. We also experimented with an
approach where physicians provided a two minute
briefing about the patient following rounds, again
using the ScanSoft system, but accuracy was much
too low to be usable. These approaches both
indicated the need for dialog with restricted input
outside of rounds.
3 OVERVIEW OF THE SPOKEN
LANGUAGE SYSTEM
We designed a spoken language system to collect
the current problems of a patient in the CTICU.
These problems are objectively defined ICD-9 codes
(International Classification of Diseases and Related
Health Problems)(ICD9), published by the World
Health Organization, which provides codes to
classify diseases, signs, symptoms, abnormal
findings, complaints, social circumstances and
external causes of injury/disease. Thus, we could
experiment with different dialog strategies for
collecting this well-defined, objective type of
information and try different methods to increase
system accuracy.
The system was deployed on the commercial
grade Genesys VoiceBrowser Platform, using IBM‘s
Websphere Voice Server (WVS) 5.1.3 for
Automatic Speech Recognition (ASR) and Text-to-
Speech (TTS)(VoiceServer). The application was
developed in VoiceXML and grammars were written
in SRGS format. Figure 1 shows how the different
components in the I
3
application interact. I
3
was built
as a web application and hosted from a Tomcat web
server. It was responsible for generating the
dynamic VoiceXML content, creating patient-
specific grammars on the fly. Patient-specific
information was supplied by an inference engine
applied to the CTICU Electronic Medical Record
(EMR - Eclipsys). This engine was designed to
generate real-time ICD-9 problem codes for the
patients being evaluated by the system.
Users access the system by calling from any
telephone including landlines and cell phones. Once
connected, the system asks the physician for the
patient’s reference number (RefN). The reference
number was used to associate the information
collected by telephone with a unique set of patient
specific clinical problems inferred over the
EMR(PIS). For development we used an
anonymized dataset. If the system cannot match the
spoken RefN against the PIS, it proceeds to collect
patient problems without access to information from
PIS. The system explains to the user that s/he must
speak one problem at a time and listens for input.
HEALTHINF 2009 - International Conference on Health Informatics
324
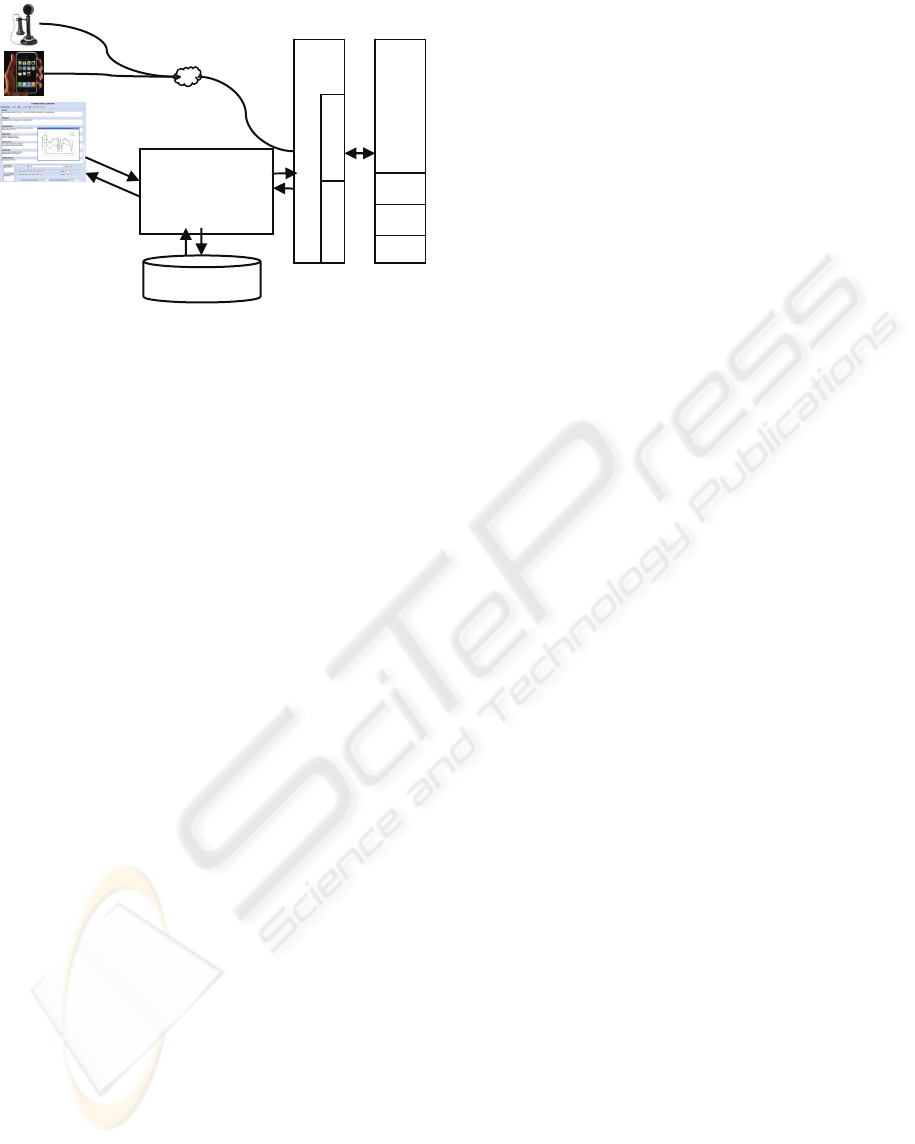
Figure 1: I
3
Architecture Description.
The user can stop the system at any time by
saying “I’m done.” The system supports collecting
information for multiple patients in one call and also
allows users to interrupt the system when they
become familiar with it and need not listen to
prompts. Once the session ends, the system records
each of the current problems collected and their
equivalent ICD-9 codes in the patient database.
Below is a sample interaction of a user with I
3
.
System I'm here to collect information about your
patients. What is the patient's 7 digit Ref N?
User 7432516
System Ok, now let's collect the current problems for this
patient. Please speak one problem at a time. When you are
done, just say “done.” What's the next problem?
User acute respiratory failure
System Ok got it! What’s the next problem?
User hyperglycemia
User done
System Given this patient's profile I would like to suggest
3 other possibilities, would you be willing to confirm them
for me? Please say yes or no.
User yes
System Does the patient have pulmonary edema?
The main challenges in the system from a speech
recognition perspective are: number recognition, for
the RefN; Yes/No recognition for confirmations and
patient problem recognition, which is unique to this
task. Number recognition is a well studied problem
in the field of speech recognition and commercial
recognizers claim to do quite well (recognition
accuracy in the 90th percentile) under normal
operating conditions.
Because we had domain knowledge but not
much spoken data, we chose to model the problems
using a grammar. We use domain knowledge to
generate a Context Free Grammar (CFG) that
represents the possible inputs for this specific
domain. The grammar was constructed by encoding
each of the 109 ICD-9 problems which are
chargeable in the CTICU as a rule in the grammar.
Note that an individual problem could consist of a
single word (e.g., “hypertension”) or a multi-word
phrase (e.g., “systolic heart failure”). We then
modified the grammar to account for variations in
how these terms were spoken, allowing for optional
words in the descriptions. For example: the rule
[acute] systolic heart failure, where brackets denote
an optional parameter, would cover both systolic
heart failure and acute systolic heart failure.
Paraphrases (e.g., abbreviations vs. full phrases)
were added as additional rules. The resulting
grammar contained 122 rules.
Our spoken language application was connected
to a database containing patient information (the PIS
in Figure 1) supplied by the inference engine,
developed by physicians at Columbia Presbyterian
Medical Center, which infers the current status of a
patient by correlating perturbations in the patient
parameters (e.g. lab results, vital statistics, and so
on) with possible diagnoses; it produces a list of
possible problems the patient could have. This list of
ICD9 problems was designed to be a superset of all
possible problems and tended to range from 10 to 30
entries. We used the problem list produced by the
inference system to generate on-the-fly a patient-
specific grammar which we hypothesized could
increase accuracy.
4 METHODS
We structured our experiments in such way as to
gain a better understanding into the following
questions
• Is speech recognition accurate enough for the
hospital environment?
• Can domain knowledge improve recognition
accuracy?
• Will physicians provide expected answers from
a short list versus unconstrained spoken input?
• How can we balance user and system initiative
for efficient interaction?
4.1 Study Design
For the experiment, the I
3
application was
configured so that it had access to information on the
current patients within the CTICU. After IRB
approval, only physicians who had patients in the
CTICU used the system during the experiments.
This allowed us to collect information about patients
during the normal course of the physician’s daily
Voice Browser
(Genesys)
WVS
(IBM)
MRCP
MRCP Client Telephony
STT
TTS
SV
I3 Application
-Survey
-Patient DB
-Data exchange
with Patient Information System
-Dynamic grammar generation
-Current problem list
patient id
problem list
+
billing codes
http
vxml
Patient Information System
(Columbia Presbyterian)
Inferred problem list
SPOKEN LANGUAGE INPUT FOR A PATIENT NOTE SYSTEM
325

routine. The experiments were conducted over
multiple days, usually right after morning rounds.
Physicians called from the operating room, after
the patient had been anesthetized, and from various
locations in the ICU, including hallways, meeting
rooms, patient rooms and nurses’ stations; calls
usually shortly after physicians examined their
patients.
We compared two different modes of interaction
with the physician users. The first was system-
driven; the system provided the list of patient
problems using inference engine output and the
physician simply confirmed problems that s/he
believed were associated with a patient. The second
one was user-driven and allowed physicians to
identify the problems they thought were relevant to
the patient. Our system-driven approach requires the
user to pay close attention to what the system
proposes. In our user-driven system the user is free
to enter information as s/he pleases. (Ackermann
and Libosse) observed that systems which require
more usage of human memory were more prone to
errors and took longer to complete.
In the system-driven mode, once the physician
had entered the patient’s RefN, s/he was presented
with a list of problems associated with that patient
and asked to say yes to any that should be included
in the note. At the end of this process, the physician
was asked if s/he would like to augment the list with
additional problems which may not have been
deduced by the inference engine.
The user-driven mode allowed the caller to first
speak all the problems for a given patient. The
system would then compare the collected problems
with those produced by the inference engine (usually
a larger set) and would ask the caller if she would
like the system to present the remaining inferred
problems for inclusion in the patient’s profile. If the
caller responded with yes, the system would then list
the remaining problems one at a time; the caller
would say yes to include a problem in the profile. It
was possible to skip this process by saying done at
any point during the listing.
Since it relies on yes-no recognition, the system-
driven mode should have the advantage of high
accuracy in recognizing problems and should expose
users to problems they might not have thought of.
The user-driven mode should give users more
control over the direction of the dialog, allowing
them to enter the problems they felt were more
important first, and hopefully reducing the cognitive
overhead.
After collecting the speech, we also
experimented with using different combinations of
grammars and language models to recognize the
input. We experimented with the ICD9 grammar and
the ICD9 plus patient-specific grammar. When used
alone the patient specific grammar yielded poor
results. This is because physicians would often
express problems using a more varied vocabulary
and order than encoded in the grammar. UMLS has
been shown to provide useful strings for natural
language processing when properly selected
(McCray, et al.) We experimented with a larger
grammar constructed from the UMLS (16391
Entries) comparing recognition accuracy with the
UMLS grammar alone, the UMLS plus the ICD9
grammar and the UMLS plus both the ICD9 and the
patient specific grammar. We also experimented
with various combinations of language models. Our
language models were trained on data from various
sources including: the UMLS database of disease
descriptions; anonymized discharge notes and
transcriptions of medical interviews. The model
trained on all the data sets combined gave the best
performance in terms of WER. See Table 1
LM+ICD9+Patient Specific for more details. There
were 389k sentences and 49k words used to train our
tri-gram language model.
After using one of the versions of the system, the
users were asked to complete a survey about their
experience with the system. They were asked to
answer four questions, using a scale from one to
five, where one generally meant a negative response
and five a very positive one. They were allowed to
speak or type their answers using the telephone’s
touchpad. The questions were:
Q1 Would you find this system helpful for collecting
patient information?
Q2 Does the system ask questions efficiently?
Q3 Was the system knowledgeable about your patient?
Q4 Would you want to use this system to retrieve
information about your patients?
5 RESULTS
During our experiment we received 44 calls from
both physicians and students. The students were
given a script with made-up patient information. The
physicians called in from the CTICU and were asked
to enter information about their current patients. The
average number of turns per call was 18, where each
turn is an interaction between the system and the
user. The average call duration was 3 minutes and
42 seconds, and the longest call lasted almost 24
minutes.
HEALTHINF 2009 - International Conference on Health Informatics
326
The overall Word Error Rate (WER), which is a
ratio of errors (measured by substitutions, insertions
and deletions of words compared to a reference
transcription) over the total number of words, was
23.39%. (Bangalore and Johnston) reported similar
rates for a multimodal conversational system with
36% WER, when trained on out-of domain data.
When they trained on in domain data they achieved
WER of 25% in offline testing. For most spoken
dialog applications Semantic Accuracy (SA) is more
relevant then WER, though there is usually a
correlation between the two. The SA for the overall
application was 79.31%. To understand the
difference between the two, consider a recognition
output of yes that’s it where the user actually said uh
yes. This would increase the WER by three but since
both have the same semantic tag (e.g. yes) the
semantic result would be correct. In our grammars
for patient problems we used the ICD-9 codes as the
semantic annotation.
Table 1: WER/SA report broken down by grammar.
Categories WER SA SentErr
RefN 7.71 74.19 -
Yes/No 20.78 94.91 -
Done 0 100 -
ICD9 62.42 50.64 50.64
ICD9 + patient specific 59.70 53.20 48.72
LM 56.67 55.76* 53.85
LM+ICD9+patient specific
43.94 61.53* 39.10
Overall (base) 32.55 76.93 27.80
Overall (LM)
23.39 79.31* 24.56
We calculated semantic accuracy for the
grammars by comparing the semantic results to the
semantic transcriptions. For the language model, we
computed semantic accuracy using a unigram
classifier
.
We break these numbers down by answer
category for WER and SA in Table 1. The most
interesting category, is the one where patient
problems are collected, handled by our ICD9 and
patient-specific grammars. While we see WER rates
of over 40%, SA is over the 60th percentile at
61.53%. To understand whether the patient-specific
grammars are helping us, we ran the same data
through a recognizer configured only with the ICD9
grammar (
ICD9 only in Table 1.) We achieved a WER
of 62.42% and a SA of 50.64% for the current
problems section, which show that combining the
patient-specific information improves the grammar
by 5%. The best results were achieved by running
both grammars and language model in parallel
which improved recognition accuracy by 15% for
SA and 26% for WER in the current problems
section. If we look at our overall numbers (
Overall
(LM)
in Table 1) we see our changes improved the
system in all three categories (WER, SA, SentErr)
when compared to the base system (e.g.
Overall (base)
in Table 1).
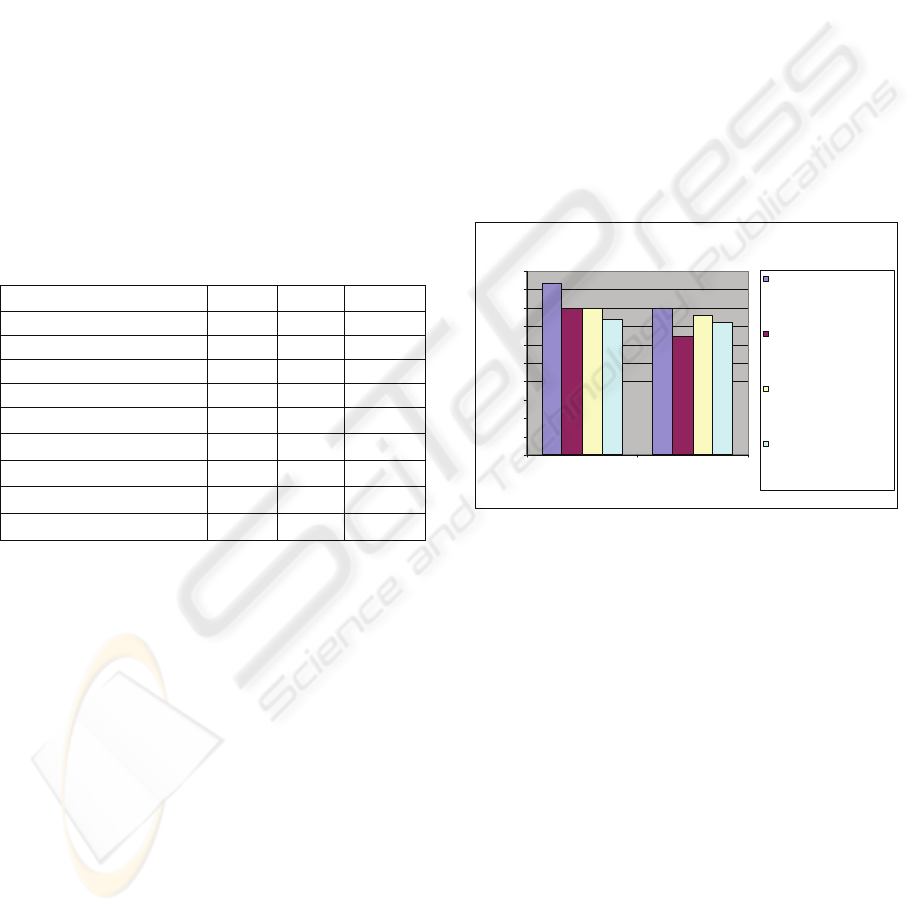
5.1 Survey Analysis
Each user was randomly routed to one of the two
systems (user- or system-driven.) Once the user was
finished with a patient s/he would be asked to
answer four questions over the phone. We collected
responses from eight physicians. Results are shown
in Figure 2.
Figure 2 shows that users preferred the system
that allowed them to say the problems first (e.g.
user-driven,) as it scored higher in all questions.
Survey Results
0
0.5
1
1.5
2
2.5
3
3.5
4
4.5
5
User Driven System Driven
I
3
Syste m
Average
Would you find this system
helpful for collecting patient
information?
Does the system ask
questions ef ficiently?
Was the system
know ledgeable about your
patient?
Would you w ant to use this
system to retrieve
information about your
patients?
Figure 2: Survey results of questions for each system.
6 DISCUSSION
From the survey responses, it was clear that
physicians found this system helpful for collecting
patient information (avg. 4.5). While they found the
user-driven method more efficient than the system-
driven approach, they mentioned that they were at
times frustrated by the speed and performance of the
system, indicating that there is still room for
improvement. One of the most populated areas, the
nurse’s station, provided the worst acoustic
environment for speech recognition. We found that
other areas such as patient rooms, O.R. and hallways
had less effect on performance.
By analyzing the anonymized transcriptions we
noted that physicians provided expected answers in
over 60% of the inputs for patient problems,
especially those problems which were common in
SPOKEN LANGUAGE INPUT FOR A PATIENT NOTE SYSTEM
327

the CTICU. However, in other cases they tended to
combine problems or modify their descriptions of
them slightly. We plan to develop models that would
allow some provision of multiple problems in one
input.
Our recognition results were clearly affected by
the adverse environment, though we plan to
investigate methods to overcome these barriers,
including building recognizers robust to machine
noises (beeps.) and further smart dialog strategies.
6.1 Related Work
Other researchers have investigated the use of
speech recognition for translation of physician
diagnostic questions to the patient language using a
linguistically based constrained domain grammar
and achieve accuracy results of 69% (Bouillan et al).
Strzalkowski et al experiment with the use of post-
processing correction on a speaker-dependent
system for recognition of dictated radiology reports.
They first observe that recognition accuracy is far
below the advertised 5% and averages 14.3%. Their
linguistically based correction model reduced the
rate to 11.3%. Thus, even in a quiet environment,
with trained, speaker dependent models and close-
talking microphones, error rate is just 10% above
what we achieved. Bangalore & Johnston
experiment with mixing grammar and rule based
models in their MATCH application. MATCH is a
multimodal application that enables mobile users to
access subway and restaurant information for New
York City. In their best results they report 25% for
WER and 59.5% for SentErr. Our numbers for the
overall application are in line with those and in fact
show a slight improvement.
7 CONCLUSIONS
Our research shows that by using patient specific
inferences, we can increase the semantic accuracy of
clinical problem recognition by 5% and by
augmenting our patient specific grammars with a
large coverage language model, we can further
increase semantic accuracy by 15% and WER by
26%. Thus, an approach which is tightly integrated
with underlying patient-specific systems shows
promise for providing a usable spoken language
interface. Our survey shows that physicians find this
to be a helpful method for providing patient
information. Analysis of input shows that physicians
provide short responses that directly answer the
given questions.
REFERENCES
Wang SS, Starren JB. A Java speech implementation of
the mini-mental status exam. Proceedings of the
AMIA Annual Fall Symposium; Hanley&Belfus,
Philadelphia, 1999: 435-439.
Owens, S.. New Operations in Speech. Speechteg
Magazine, August 2005
Zue, V., S. Seneff, J. Glass, J. Polifroni, C. Pao, T. Hazen
and L. Hetherington, Jupiter: A Telephone-based
Conversational Interface for Weather Information,
IEEE Trans. on Speech and Audio Processing, 8(1),
2000.
International Classification of Diseases, Ninth Revision,
Clinical Modification, NCHS, 2007.
National Library of Medicine. Documentation, UMLS
Knowledge Sources. 2007AC Edition, May 2007.
McCray AT, Bodenreider O, Malley J and Browne AC.
Evaluating UMLS Strings for Natural Language
Processing. Proc AMIA Symp 2001.
Ackermann, Chantal and Libossek, Marion (2006):
System-versus user-initiative dialog strategy for driver
information systems, In INTERSPEECH-2006, paper
1172-Mon2FoP.3.
Bouillon, P. and Halimi, S. and Rayner, M. and
Hockey, B. A. Adapting a Medical speech to speech
translation system (MedSLT) to Arabic. Proceedings
of the 2007 Workshop on Computational Approaches
to Semitic Languages: Common Issues and Resources
Strzalkowski, T. and Brandow, R. A Natural Language
Correction Model for Continuous Speech Recognition.
5
th
Workshop on Very Large Corpora, EMNLP 1997
Bangalore, S. and Johnston, M. Balancing data-driven
and rule-based approaches in the context of a
Multimodal Conversational System. HLT-NAACL
2004: Main Proceedings
IBM Websphere Voice Server
http://www.ibm.com/software/pervasive/voice_server/
HEALTHINF 2009 - International Conference on Health Informatics
328
